Relationship Between L4/5 Lumbar Multifidus Cross-Sectional Area Ratio and Fall Risk in Older Adults with Lumbar Spinal Stenosis: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Fall Questionnaire Assessment
2.3. Clinical Evaluation
2.4. Lumbar Multifidus Cross-Sectional Area
2.5. Spine Alignment
2.6. Balance Assessment
2.7. Low Back Pain Assessment
2.8. Geriatric Depression Scale
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kreiner, D.S.; Shaffer, W.O.; Baisden, J.L.; Gilbert, T.J.; Summers, J.T.; Toton, J.F.; Hwang, S.W.; Mendel, R.C.; Reitman, C.A. North American Spine Society. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. 2013, 13, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Chun, H.J.; Han, C.D.; Moon, S.H.; Kang, K.T.; Kim, H.S.; Park, J.O.; Moon, E.S.; Kim, B.R.; Sohn, J.S.; et al. The risk assessment of a fall in individual with lumbar spinal stenosis. Spine (Phila Pa 1976) 2011, 36, E588–E592. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R. Loss of skeletal muscle mass in aging: Examining the relationship of starvation, sarcopenia and cachexia. Clin. Nutr. 2007, 26, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Liu-Ambrose, T.; Davis, J.C.; Hsu, C.L.; Gomez, C.; Vertes, K.; Marra, C.; Brasher, P.M.; Dao, E.; Khan, K.M.; Cook, W.; et al. Action Seniors!-secondary falls prevention in community-dwelling senior fallers: Study protocol for a randomized controlled trial. Trials 2015, 16, 144. [Google Scholar] [CrossRef] [PubMed]
- Mohler, M.J.; Wendel, C.S.; Taylor-Piliae, R.E.; Toosizadeh, N.; Najafi, B. Motor performance and physical activity as predictors of prospective falls in community-dwelling older adults by frailty level: Application of wearable technology. Gerontology 2016, 62, 654–664. [Google Scholar] [CrossRef] [PubMed]
- Sturnieks, D.L.; Tiedemann, A.; Chapman, K.; Munro, B.; Murray, S.M.; Lord, S.R. Physiological risk factors for falls in elderly people with lower limb arthritis. J. Rheumatol. 2004, 31, 2272–2279. [Google Scholar]
- Zhang, X.; Huang, P.; Dou, Q.; Wang, C.; Zhang, W.; Yang, Y.; Wang, J.; Xie, X.; Zhou, J.; Zeng, Y. Falls among older adults with sarcopenia dwelling in nursing home or community: A meta-analysis. Clin. Nutr. 2019. [Google Scholar] [CrossRef]
- Leveille, S.G.; Jones, R.N.; Kiely, D.K.; Hausdorff, J.M.; Shmerling, R.H.; Guralnik, J.M.; Kiel, D.P.; Lipsitz, L.A.; Bean, J.F. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 2009, 302, 2214–2221. [Google Scholar] [CrossRef]
- Morris, R. Predicting falls in elderly women. Menopause. Int. 2007, 13, 170–177. [Google Scholar] [CrossRef]
- Oleksik, A.; Lips, P.; Dawson, A.; Minshall, M.E.; Shen, W.; Cooper, C.; Kanis, J. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J. Bone. Miner. Res. 2000, 15, 1384–1392. [Google Scholar] [CrossRef]
- Miyakoshi, N.; Itoi, E.; Kobayashi, M.; Kodama, H. Impact of postural deformities and spinal mobility on quality of life in postmenopausal osteoporosis. Osteoporos. Int. 2003, 14, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, Y.; Miyakoshi, N.; Kasukawa, Y.; Hongo., M.; Shimada, Y. Spinal sagittal contour affecting falls: Cut-off value of the lumbar spine for falls. Gait Posture 2013, 38, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Hwang, J.Y.; Oh, J.K.; Park, M.S.; Kim, S.W.; Chang, H.; Kim, T.-H. The association between whole body sagittal balance and risk of falls among elderly patients seeking treatment for back pain. Bone. Joint. Res. 2017, 6, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.; Hodges, P.W.; Hides, J. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain, 2nd ed.; Churchill Livingstone: New York, NY, USA, 2004; pp. 185–219. [Google Scholar]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine (Phila Pa 1976) 2006, 31, E707–E712. [Google Scholar]
- Okochi, J.; Toba, K.; Takahashi, T.; Matsubayashi, K.; Nishinaga, M.; Takahashi, R.; Ohru, T. Simple screening test for risk of falls in the elderly. Geriatr. Gerontol. Int. 2006, 6, 223–227. [Google Scholar] [CrossRef]
- Ito, T.; Sakai, Y.; Yamazaki, K.; Igarashi, K.; Sato, N.; Yokoyama, K.; Morita, Y. Proprioceptive change impairs balance control in older patients with low back pain. J. Phys. Ther. Sci. 2017, 29, 1788–1792. [Google Scholar] [CrossRef]
- Jackson, R.P.; McManus, A.C. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and individual with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994, 19, 1611–1618. [Google Scholar] [CrossRef]
- Clark, R.A.; Bryant, A.L.; Pua, Y.; McCrory, P.; Bennell, K.; Hunt, M. Validity and reliability of the Nintendo Wii Balance Board for assessment of standing balance. Gait Posture 2010, 31, 307–310. [Google Scholar] [CrossRef]
- Young, W.; Ferguson, S.; Brault, S.; Craig, C. Assessing and training standing balance in elderly adults: A novel approach using the ‘Nintendo Wii’ Balance Board. Gait Posture 2011, 33, 303–305. [Google Scholar] [CrossRef]
- Bacciu, D.; Chessa, S.; Gallicchio, C.; Micheli, A.; Pedrelli, L.; Ferro, E.; Fortunati, L.; La Rosa, D.; Palumbo, F.; Vozzi, F.; et al. A learning system for automatic Berg Balance Scale score estimation. Eng. Appl. Artif. Intell. 2017, 66, 60–74. [Google Scholar] [CrossRef]
- Ito, T.; Sakai, Y.; Morita, Y.; Yamazaki, K.; Igarashi, K.; Nishio, R.; Sato, N. Proprioceptive weighting ratio for balance control in static standing is reduced in elderly patients with non-specific low back pain. Spine (Phila Pa 1976) 2018, 43, 1704–1709. [Google Scholar] [CrossRef] [PubMed]
- Howcroft, J.; Lemaire, E.D.; Kofman, J.; McIlroy, W.E. Elderly fall risk prediction using static posturography. PLoS ONE 2017, 12, e0172398. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.; Schiphorst Preuper, H.R.; Balk, G.A.; Stewart, R.E. Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 2014, 155, 2545–2550. [Google Scholar] [CrossRef] [PubMed]
- Sugishita, K.; Sugishita, M.; Hemmi, I.; Asada, T.; Tanigawa, T. A validity and reliability study of the Japanese version of the Geriatric Depression Scale 15 (GDS-15-J). Clin. Gerontol. 2017, 40, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.; Heisel, M.J.; Delavan, R.L. Psychometric properties of the 15-item Geriatric Depression Scale in functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J. Am. Geriatr. Soc. 2005, 53, 1570–1576. [Google Scholar] [CrossRef] [PubMed]
- Masi, A.T.; Nair, K.; Evans, T.; Ghandour, Y. Clinical, biomechanical, and physiological translational interpretations of human resting myofascial tone or tension. Int. J. Ther. Massage Bodyw. 2010, 3, 16–28. [Google Scholar] [PubMed]
- Ward, S.R.; Kim, C.W.; Eng, C.M.; Gottschalk, L.J.; Tomiya, A.; Garfin, S.R.; Lieber, R.L. Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. J. Bone. Joint. Surg. Am. 2009, 91, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Kado, D.M.; Huang, M.H.; Nguyen, C.B.; Barrett-Connor, E.; Greendale, G.A. Hyperkyphotic posture and risk of injurious falls in elderly persons: The Rancho Bernardo Study. J. Gerontol. A Biol. Sci. Med. Sci. 2007, 62, 652–657. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Miyakoshi, N.; Hongo, M.; Shimada, Y. Spinal curvature and postural balance in individual with osteoporosis. Osteoporos. Int. 2009, 20, 2049–2053. [Google Scholar] [CrossRef]
- Kasukawa, Y.; Miyakoshi, N.; Hongo, M.; Ishikawa, Y.; Noguchi, H.; Kamo, K.; Sasaki, H.; Murata, K.; Shimada, Y. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J. Bone Miner. Metab. 2010, 28, 82–87. [Google Scholar] [CrossRef]
- Choi, C.J.; Lim, H.W.; Park, M.K.; Cho, J.G.; Im, G.J.; Chae, S.W. Does the kyphotic change decrease the risk of fall? Clin. Exp. Otorhinolaryngol. 2011, 4, 118–121. [Google Scholar] [CrossRef] [PubMed]
- Imagama, S.; Ito, Z.; Wakao, N.; Seki, T.; Hirano, K.; Muramoto, A.; Sakai, Y.; Matsuyama, Y.; Hamajima, N.; Ishiguro, N.; et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur. Spine J. 2013, 22, 1346–1353. [Google Scholar] [CrossRef]
- Rosa, N.M.; Queiroz, B.Z.; Lopes, R.A.; Sampaio, N.R.; Pereira, D.S.; Pereira, L.S.M. Risk of falls in Brazilian elders with and without low back pain assessed using the Physiological Profile Assessment: BACE study. Braz. J. Phys. Ther. 2016, 20, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, Y.; Miyakoshi, N.; Hongo, M.; Kasukawa, Y.; Kudo, D.; Shimada, Y. Relationships among spinal mobility and sagittal alignment of spine and lower extremity to quality of life and risk of falls. Gait Posture 2017, 53, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Marshall, L.M.; Litwack-Harrison, S.; Makris, U.E.; Kado, D.M.; Cawthon, P.M.; Deyo, R.A.; Carlson, N.L.; Nevitt, M.C. Osteoporotic Fractures in Men Study (MrOS) Research Group. A prospective study of back pain and risk of falls among older community-dwelling men. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 72, 1264–1269. [Google Scholar]
- Masud, T.; Morris, R.O. Epidemiology of falls. Age. Ageing 2001, 30, 3–7. [Google Scholar] [CrossRef]
- Somadder, M.; Mondal, S.; Kersh, R.; Abdelhafiz, A.H. Are recurrent fallers depressed? J. Am. Geriatr. Soc. 2007, 55, 2097–2099. [Google Scholar] [CrossRef]
- Kvelde, T.; Lord, S.R.; Close, J.C.; Reppermund, S.; Kochan, N.A.; Sachdev, P.; Brodaty, H.; Delbaere, K. Depressive symptoms increase fall risk in older people, independent of antidepressant use, and reduced executive and physical functioning. Arch. Gerontol. Geriatr. 2015, 60, 190–195. [Google Scholar] [CrossRef]
- Hill, K.D.; Williams, S.B.; Chen, J.; Moran, H.; Hunt, S.; Brand, C. Balance and falls risk in women with lower limb osteoarthritis or rheumatoid arthritis. J. Clin. Gerontol. Geriatr. 2013, 4, 22–28. [Google Scholar] [CrossRef]
- Kamińska, M.; Brodowski, J.; Karakiewicz, B. Fall risk factors in community-dwelling elderly depending on their physical function, cognitive status and symptoms of depression. Int. J. Environ. Res. Public. Health 2015, 12, 3406–3416. [Google Scholar] [CrossRef]
- Stanmore, E.K.; Oldham, J.; Skelton, D.A.; O’Neill, T.; Pilling, M.; Campbell, A.J.; Todd, C. Risk factors for falls in adults with rheumatoid arthritis: A prospective study. Arthritis. Care. Res. (Hoboken) 2013, 65, 1251–1258. [Google Scholar] [CrossRef] [PubMed]
- Ikezoe, T.; Mori, N.; Nakamura, M.; Ichihashi, N. Effects of age and inactivity due to prolonged bed rest on atrophy of trunk muscles. Eur. J. Appl. Physiol. 2012, 112, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Anderson, D.E.; Quinn, E.; Parker, E.; Allaire, B.T.; Muir, J.W.; Rubin, C.T.; Magaziner, J.; Hannan, M.T.; Bouxsein, M.L.; Kiel, D.P. Associations of computed tomography-based trunk muscle size and density with balance and falls in older adults. J. Gerontol. A. Biol. Sci. Med. Sci. 2016, 71, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Habtemariam, D.; Iloputaife, I.; Lipsitz, L.A.; Manor, B. The complexity of standing postural sway associates with future falls in community-dwelling older adults: The MOBILIZE Boston Study. Sci. Rep. 2017, 7, 2924. [Google Scholar] [CrossRef] [PubMed]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Fukunaga, T. Age-related site-specific muscle wasting of upper and lower extremities and trunk in Japanese men and women. Age (Dordr) 2014, 36, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Bergmark, A. Stability of the lumbar spine: A study in mechanical engineering. Acta Orthop Scand. Suppl. 1989, 60, 1–54. [Google Scholar] [CrossRef]
- Gardner-Morse, M.; Stokes, I.A.; Liable, J.P. Role of the muscles in lumbar spine stability in maximum extension efforts. J. Orthop Res. 1995, 13, 802–808. [Google Scholar] [CrossRef]
| Variable | Fall Risk Group | Non-Fall Risk Group | p-Value |
|---|---|---|---|
| (n = 30) | (n = 69) | ||
| Age (years) | 77.0 (67.0–96.0) | 75.0 (65.0–90.0) | 0.178 |
| Height (cm) | 155.0 ± 10.1 | 158.0 ± 8.2 | 0.125 |
| Weight (kg) | 62.1 ± 10.8 | 61.2 ± 11.0 | 0.717 |
| BMI (kg/m2) | 24.7 (19.0–31.2) | 23.7 (19.5–31.5) | 0.056 |
| Sex (males, %) | 16 (53.3) | 47 (68.1) | 0.160 |
| Fall score (point) | 9.0 (8.0–13.0) | 4.0 (0–6.0) | 0.001 |
| VAS (cm) | 5.0 (0–8.0) | 4.0 (0–10.0) | 0.110 |
| GDS (point) | 5.0 (0–14) | 5.0 (0–13) | 0.643 |
| Variable | Fall Risk Group | Non-Fall Risk Group | p-Value |
|---|---|---|---|
| (n = 30) | (n = 69) | ||
| SVA (mm) | 42.9 (−2.1–116.3) | 41.3 (−16.9–162.0) | 0.493 |
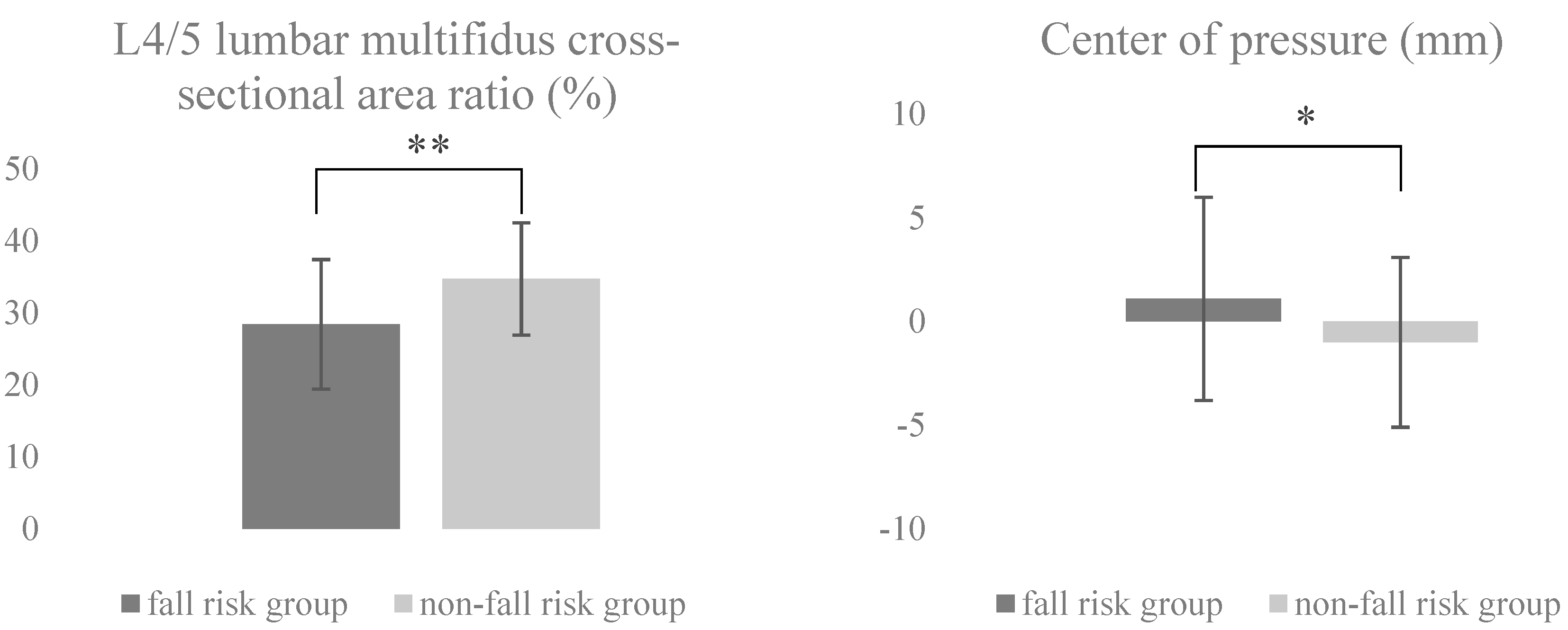
| L4/5 lumbar multifidus cross-sectional area ratio (%) | 28.4 ± 9.0 | 34.7 ± 7.8 | 0.002 |
| Center of pressure (mm) | 1.1 ± 4.9 | −1.0 ± 4.1 | 0.034 |
| Variables | OR | 95% CI | p-Value |
|---|---|---|---|
| L4/5 lumbar multifidus cross-sectional area ratio | 0.911 | 0.859–0.967 | 0.001 |
| Center of pressure | 1.144 | 1.018–1.285 | 0.024 |
| SVA (mm) | 1.010 | 0.994–1.025 | 0.227 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ito, T.; Sakai, Y.; Yamazaki, K.; Oikawa, M.; Morita, Y. Relationship Between L4/5 Lumbar Multifidus Cross-Sectional Area Ratio and Fall Risk in Older Adults with Lumbar Spinal Stenosis: A Retrospective Study. Geriatrics 2019, 4, 38. https://doi.org/10.3390/geriatrics4020038
Ito T, Sakai Y, Yamazaki K, Oikawa M, Morita Y. Relationship Between L4/5 Lumbar Multifidus Cross-Sectional Area Ratio and Fall Risk in Older Adults with Lumbar Spinal Stenosis: A Retrospective Study. Geriatrics. 2019; 4(2):38. https://doi.org/10.3390/geriatrics4020038
Chicago/Turabian StyleIto, Tadashi, Yoshihito Sakai, Kazunori Yamazaki, Makoto Oikawa, and Yoshifumi Morita. 2019. "Relationship Between L4/5 Lumbar Multifidus Cross-Sectional Area Ratio and Fall Risk in Older Adults with Lumbar Spinal Stenosis: A Retrospective Study" Geriatrics 4, no. 2: 38. https://doi.org/10.3390/geriatrics4020038
APA StyleIto, T., Sakai, Y., Yamazaki, K., Oikawa, M., & Morita, Y. (2019). Relationship Between L4/5 Lumbar Multifidus Cross-Sectional Area Ratio and Fall Risk in Older Adults with Lumbar Spinal Stenosis: A Retrospective Study. Geriatrics, 4(2), 38. https://doi.org/10.3390/geriatrics4020038







