Doctors Are Inconsistent in Estimating Survival after CPR and Are Not Using Such Predictions Consistently in Determining DNACPR Decisions
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection and Analysis
2.2. Ethical Approval
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Aarons, E.; Beeching, N. Survey of “Do not resuscitate” orders in a district general hospital. BMJ 1991, 30, 1504–1506. [Google Scholar] [CrossRef]
- Schneider, A.P.; Nelson, D.J.; Brown, D.D. In-hospital cardiopulmonary resuscitation: A 30-year review. J. Am. Board Fam. Pract. 1993, 6, 91–101. [Google Scholar]
- Tunstall-Pedoe, H.; Bailey, L.; Chamberlain, D.; Marsden, A.; Ward, M.; Zideman, D. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): Methods and overall results. BMJ 1992, 304, 1347. [Google Scholar] [CrossRef][Green Version]
- Peberdy, M.; Kaye, W.; Ornato, J.; Larkin, G.; Nadkarni, V.; Mancini, M.E.; Berg, R.; Nichol, G.; Lane-Trultt, T. Cardiopulmonary resuscitation of adults in the hospital: A report of 14,720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation 2003, 58, 297–308. [Google Scholar] [CrossRef]
- Sandroni, C.; Sandroni, C.; Nolan, J.; Cavallaro, F.; Antonelliet, M. In-hospital cardiac arrest: Incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007, 33, 237–245. [Google Scholar] [CrossRef]
- Hilberman, M.; Kutner, J.; Parsons, D.; Murphy, D. Marginally effective medical care: Ethical analysis of issues in cardiopulmonary resuscitation (CPR). J. Med. Ethics 1997, 23, 361–367. [Google Scholar] [CrossRef]
- Guidance from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. In Decisions Relating to Cardiopulmonary Resuscitation (Previously Known as the ‘Joint Statement’), 3rd ed.; British Medical Association; Resuscitation Council (UK); Royal College of Nursing: London, UK, 2016.
- Williams, R. The do-not-resuscitate decision: Guidelines for policy in the adult. J. Royal Coll. Phys. Lond. 1993, 27, 139–146. [Google Scholar]
- Ardagh, M. Futility has no utility in resuscitation medicine. J. Med. Ethics 2000, 26, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Jecker, N. Medical futility: A paradigm analysis. HEC Forum 2007, 19, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Weijer, C.; Elliott, C. Pulling the plug on futility. BMJ 1995, 310, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Bruce-Jones, P. Resuscitation decisions in the elderly: A discussion of current thinking. J. Med. Ethics 1996, 22, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Glance, L.G.; Osler, T.; Shinozaki, T. Intensive care scoring systems to predict death: A cost effective analysis. Crit. Care Med. 1998, 26, 1842–1849. [Google Scholar] [CrossRef] [PubMed]
- Rodriquez, R.M.; Wang, N.E.; Pearl, R.G. Prediction of poor outcome of intensive care unit patients admitted from the emergency department. Crit. Care Med. 1997, 25, 1801–1806. [Google Scholar] [CrossRef]
- Ebell, M.H.; Jang, W.; Shen, Y.; Geocadin, R.G.; for the Get With the Guidelines–Resuscitation Investigators. Development and Validation of the Good Outcome Following Attempted Resuscitation (GO-FAR) Score to Predict Neurologically Intact Survival After In-Hospital Cardiopulmonary Resuscitation. JAMA Intern. Med. 2013, 173, 1872–1878. [Google Scholar] [CrossRef] [PubMed]
- George, A.L., Jr.; Folk, B.P.; Crecelius, P.L.; Campbell, W.B. Pre-arrest morbidity and other correlates of survival after in-hospital cardiopulmonary arrest. Am. J. Med. 1989, 87, 28–34. [Google Scholar] [CrossRef]
- O’Keeffe, S.; Ebell, M.H. Prediction of failure to survive following in-hospital cardiopulmonary resuscitation: Comparison of two predictive instruments. Resuscitation 1994, 28, 21–25. [Google Scholar] [CrossRef]
- Rimmer, A. Ethnic diversity in NHS trusts. BMJ 2016, 355, i6406. [Google Scholar] [CrossRef]
| Mean/n | SD/% | |
|---|---|---|
| Age | 41.3 | 7.9 |
| Male | 81 | 66.4 |
| Ethnicity | ||
| White British | 82 | 67.2 |
| Asian | 26 | 21.3 |
| Other | 10 | 8.2 |
| Black | 3 | 2.5 |
| Mixed Race | 1 | 0.8 |
| Grade | ||
| Consultant | 70 | 58.3 |
| SpR | 32 | 26.7 |
| Staff Grade | 18 | 15 |
| Experience (years) | ||
| <5 | 26 | 21.9 |
| 5–10 | 5 | 4.2 |
| >10 | 88 | 74.0 |
| Specialty | ||
| Other | 26 | 21.7 |
| Care of Elderly | 21 | 17.5 |
| Orthopaedic | 15 | 12.5 |
| Cardiology | 10 | 8.3 |
| Haematology | 7 | 5.8 |
| Urology | 7 | 5.8 |
| Gastroenterology | 6 | 5 |
| Endocrinology | 5 | 4.2 |
| Palliative | 5 | 4.2 |
| Colorectal | 4 | 3.3 |
| Respiratory | 4 | 3.3 |
| Neurology | 3 | 2.5 |
| Vascular | 3 | 2.5 |
| Renal | 2 | 1.7 |
| Upper GI | 2 | 1.7 |
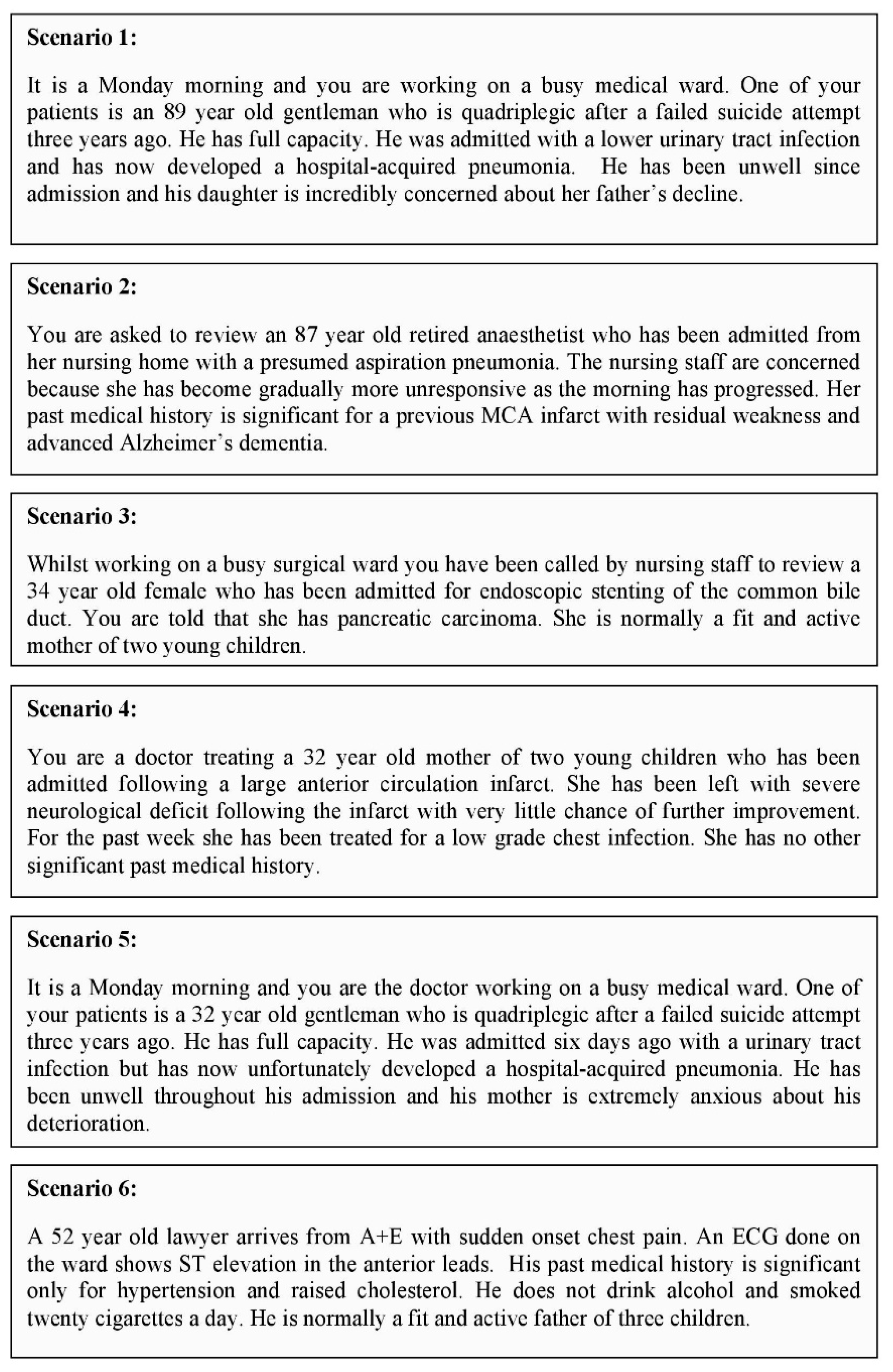
| Scenario | Respondents Who Would Not Resuscitate (%) | Respondents Who Would Resuscitate (%) | No Response (%) |
|---|---|---|---|
| 1 | 82 (59.9) | 30 (21.9) | 25 (18.2) |
| 2 | 105 (76.6) | 7 (5.2) | 25 (18.2) |
| 3 | 11 (8.1) | 100 (73.0) | 26 (18.9) |
| 4 | 54 (39.4) | 56 (40.8) | 27 (19.8) |
| 5 | 42 (30.6) | 66 (48.2) | 29 (21.2) |
| 6 | 0 (0) | 109 (79.5) | 28 (20.5) |
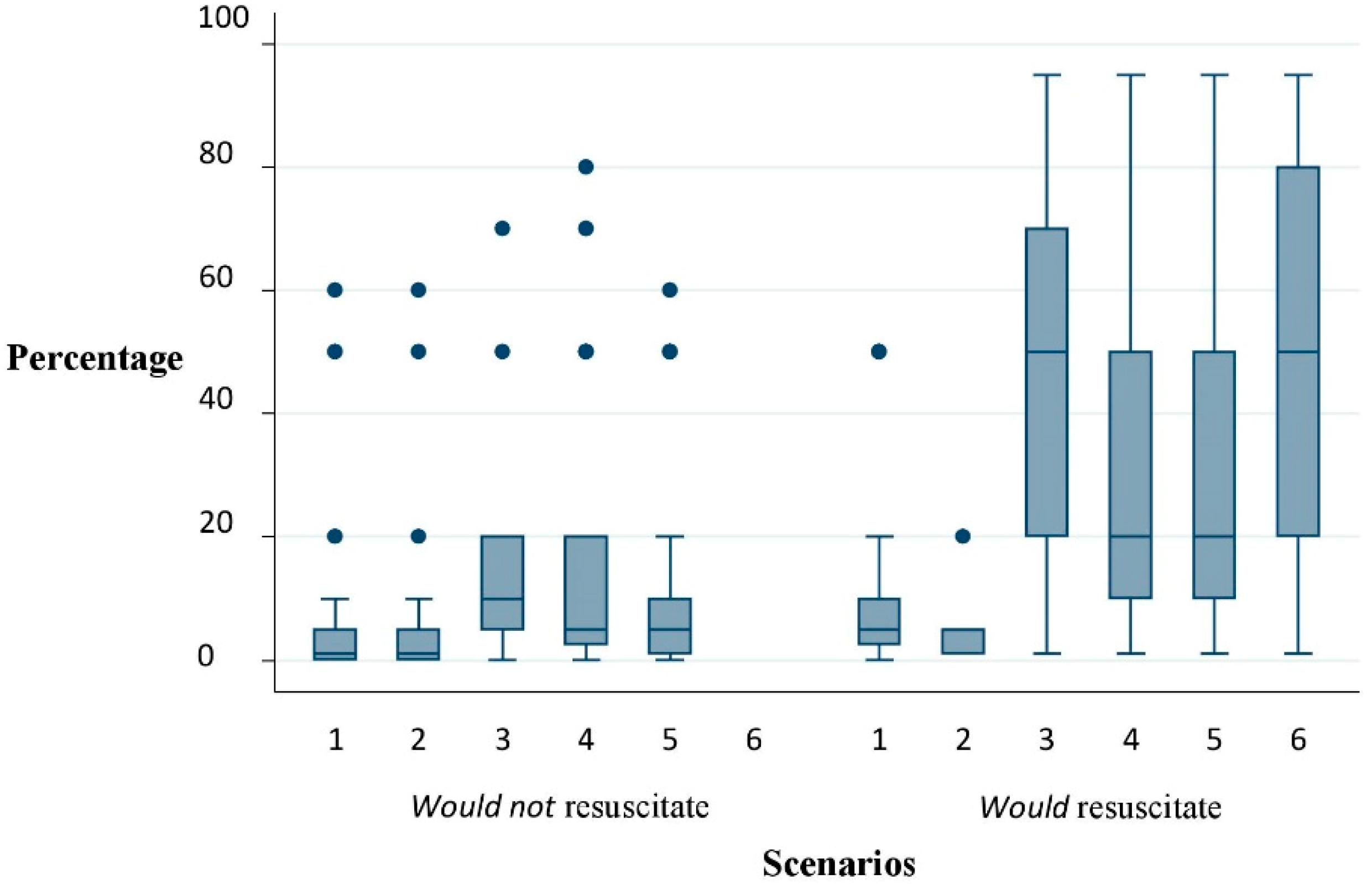
| Scenario | Respondents Who Would Not Resuscitate Estimated Percentage Survival after CPR–Median (Range) | Respondents Who Would Resuscitate Estimated Percentage Survival after CPR–Median (Range) | P-Value * |
|---|---|---|---|
| 1 | 1 (0.1–60) | 5 (0.1–50) | 0.001 |
| 2 | 1 (0.1–60) | 1 (0.1–20) | 0.130 |
| 3 | 10 (0.1–70) | 50 (1–95) | 0.005 |
| 4 | 5 (0.1–80) | 20 (1–95) | <0.001 |
| 5 | 5 (0.1–60) | 20 (1–95) | <0.001 |
| 6 | - | 50 (1–95) | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kidd, A.C.; Honney, K.; Bowker, L.K.; Clark, A.B.; Myint, P.K.; Holland, R. Doctors Are Inconsistent in Estimating Survival after CPR and Are Not Using Such Predictions Consistently in Determining DNACPR Decisions. Geriatrics 2019, 4, 33. https://doi.org/10.3390/geriatrics4020033
Kidd AC, Honney K, Bowker LK, Clark AB, Myint PK, Holland R. Doctors Are Inconsistent in Estimating Survival after CPR and Are Not Using Such Predictions Consistently in Determining DNACPR Decisions. Geriatrics. 2019; 4(2):33. https://doi.org/10.3390/geriatrics4020033
Chicago/Turabian StyleKidd, Andrew C, Katie Honney, Lesley K Bowker, Allan B Clark, Phyo K Myint, and Richard Holland. 2019. "Doctors Are Inconsistent in Estimating Survival after CPR and Are Not Using Such Predictions Consistently in Determining DNACPR Decisions" Geriatrics 4, no. 2: 33. https://doi.org/10.3390/geriatrics4020033
APA StyleKidd, A. C., Honney, K., Bowker, L. K., Clark, A. B., Myint, P. K., & Holland, R. (2019). Doctors Are Inconsistent in Estimating Survival after CPR and Are Not Using Such Predictions Consistently in Determining DNACPR Decisions. Geriatrics, 4(2), 33. https://doi.org/10.3390/geriatrics4020033






