Pharmacist Clinical Interventions and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A Prospective Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Site, and Setting
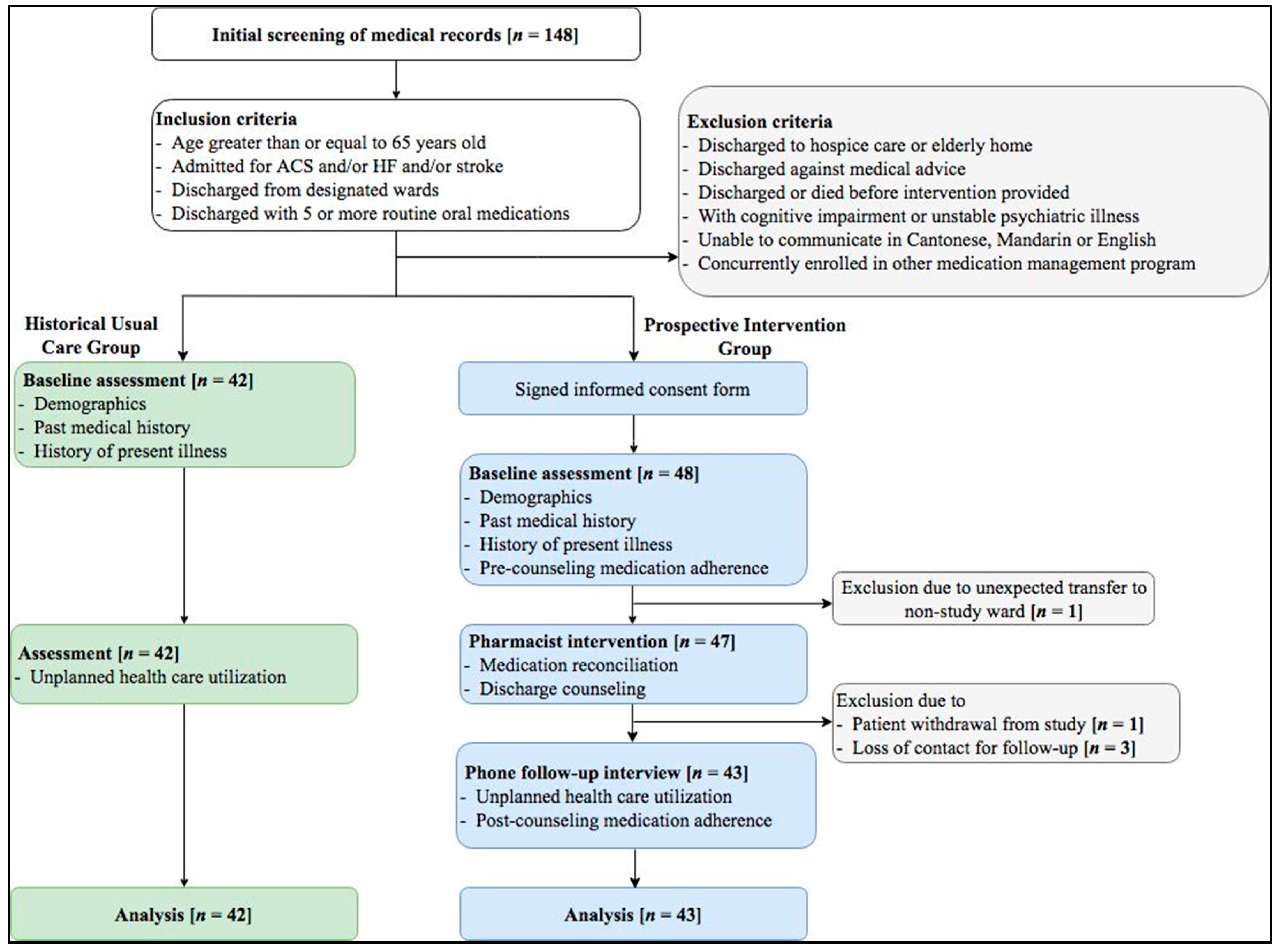
2.2. Patient Enrollment
2.3. Group Allocation
2.4. Baseline Assessment
2.5. Medication Reconciliation
2.6. Discharge Counseling
2.7. Phone Follow-Up
2.8. Outcome Measures
2.9. Data Management and Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Medication Utilization
3.2.1. Pre-Admission Medications
3.2.2. Discharge Medications
3.3. Identified DRPs and Clinical Significance
3.3.1. (Possible) Causes
3.3.2. Interventions and Acceptance
3.3.3. Medications Implicated in DRPs
3.3.4. Clinical Significance of DRPs Identified
3.4. Unplanned Health Care Utilization
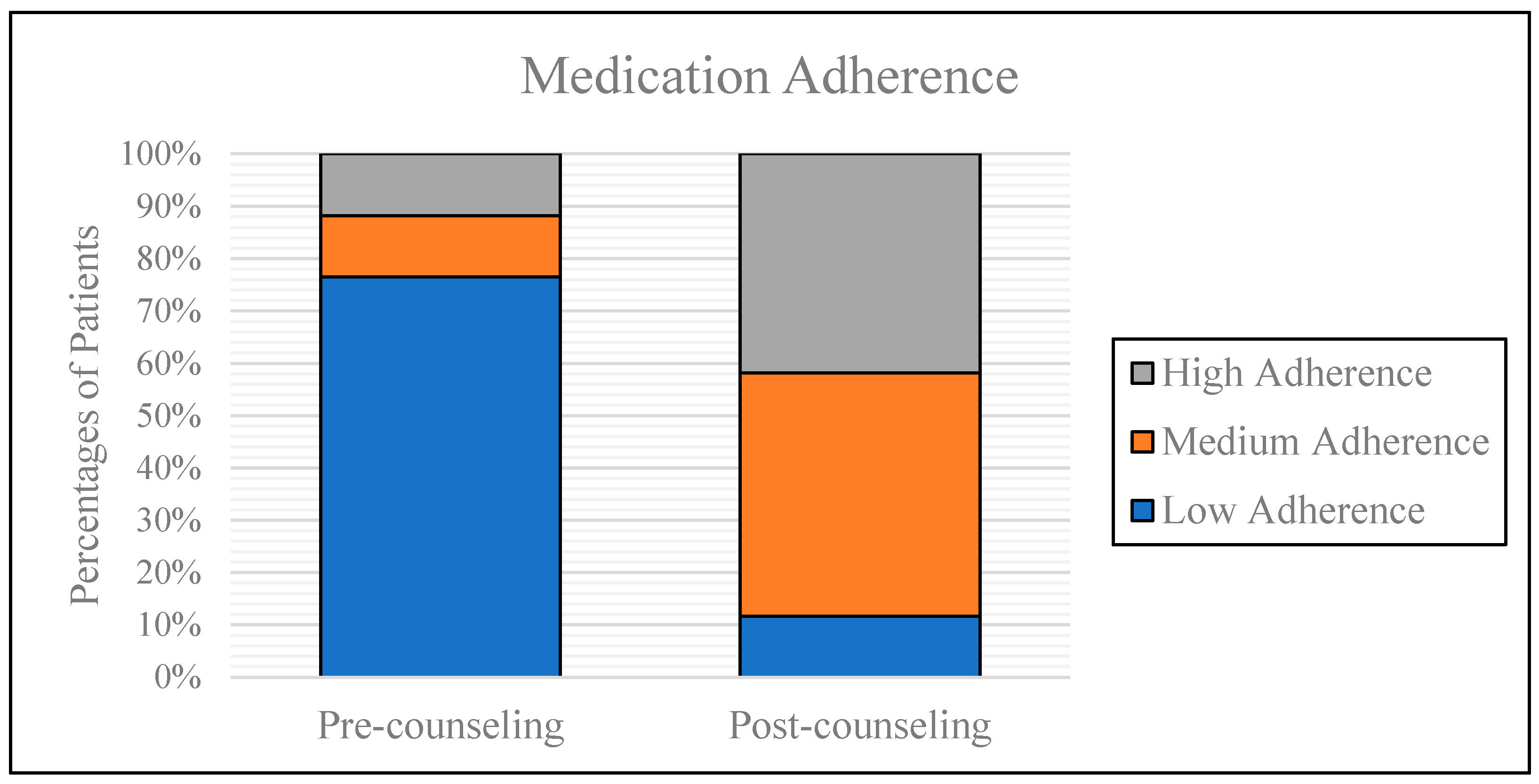
3.5. Medication Adherence
3.6. Risk Factors of Occurrence of DRPs
3.7. Risk Factors Associated with Readmissions
4. Discussion
4.1. DRPs and Associated Risk Factors
4.2. Unplanned Health Care Utilization
4.3. Medication Adherence
4.4. Limitations
4.5. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

References
- Pharmaceutical Care Network Europe. DRP-Classification V8.02. Available online: http://www.pcne.org/upload/files/230_PCNE_classification_V8-02.pdf (accessed on 21 May 2018).
- Forster, A.J.; Murff, H.J.; Peterson, J.F.; Gandhi, T.K.; Bates, D.W. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann. Intern. Med. 2003, 138, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Jencks, S.F.; Williams, M.V.; Coleman, E.A. Rehospitalizations among patients in the medicare fee-for-service program. N. Engl. J. Med. 2009, 360, 1418–1428. [Google Scholar] [CrossRef] [PubMed]
- Ho, P.M.; Spertus, J.A.; Masoudi, F.A.; Reid, K.J.; Peterson, E.D.; Magid, D.J.; Krumholz, H.M.; Rumsfeld, J.S. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch. Intern. Med. 2006, 166, 1842–1847. [Google Scholar] [CrossRef] [PubMed]
- Spertus, J.A.; Kettelkamp, R.; Vance, C.; Decker, C.; Jones, P.G.; Rumsfeld, J.S.; Messenger, J.C.; Khanal, S.; Peterson, E.D.; Bach, R.G. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement. Circulation 2006, 113, 2803–2809. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.J.; Murff, H.J.; Peterson, J.F.; Gandhi, T.K.; Bates, D.W. Adverse drug events occurring following hospital discharge. J. Gen. Intern. Med. 2005, 20, 317–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kripalani, S.; Roumie, C.L.; Dalal, A.K.; Cawthon, C.; Businger, A.; Eden, S.K.; Shintani, A.; Sponsler, K.C.; Harris, L.J.; Theobald, C. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: A randomized trial. Ann. Intern. Med. 2012, 157, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rask, K.J.; Wells, K.J.; Teitel, G.S.; Hawley, J.N.; Richards, C.; Gazmararian, J.A. Can an algorithm for appropriate prescribing predict adverse drug events? Am. J. Manag. Care 2005, 11, 145–151. [Google Scholar] [PubMed]
- Anderson, J.L.; Adams, C.D.; Antman, E.M.; Bridges, C.R.; Califf, R.M.; Casey, D.E., Jr.; Chavey, W.E., 2nd; Fesmire, F.M.; Hochman, J.S.; Levin, T.N.; et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–st elevation myocardial infarction. J. Am. Coll. Cardiol. 2007, 116, 148–304. [Google Scholar]
- Wong, Y.Y. Pharmacist Clinical Service in an Orthopedic Rehabilitation Ward in A Local Hospital. HKPJ 2017, 24, S26. [Google Scholar]
- Koshman, S.L.; Charrois, T.L.; Simpson, S.H.; McAlister, F.A.; Tsuyuki, R.T. Pharmacist care of patients with heart failure: A systematic review of randomized trials. Arch. Intern. Med. 2008, 168, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Oborne, A.; Dodds, L.J. Seamless pharmaceutical care: The needs of community pharmacists. Pharm. J. 1994, 253, 502–506. [Google Scholar]
- Modig, S.; Kristensson, J.; Ekwall, A.K.; Hallberg, I.R.; Midlöv, P. Frail elderly patients in primary care—their medication knowledge and beliefs about prescribed medicines. Eur. J. Clin. Pharmacol. 2009, 65, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Krumholz, H.M.; Merrill, A.R.; Schone, E.M.; Schreiner, G.C.; Chen, J.; Bradley, E.H.; Wang, Y.; Wang, Y.F.; Lin, Z.Q.; Straube, B.M.; et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ. Cardiovasc. Qual. Outcomes 2009, 2, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Schnipper, J.L.; Kirwin, J.L.; Cotugno, M.C.; Wahlstrom, S.A.; Brown, B.A.; Tarvin, E.; Kachalia, A.; Horng, M.; Roy, C.L.; McKean, S.C.; et al. Role of pharmacist counseling in preventing adverse drug events after hospitalization. Arch. Intern. Med. 2006, 166, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Al-Rashed, S.A.; Wright, D.J.; Roebuck, N.; Sunter, W.; Chrystyn, H. The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. Br. J. Clin. Pharmacol. 2002, 54, 657–664. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dudas, V.; Bookwalter, T.; Kerr, K.M.; Pantilat, S.Z. The impact of follow-up telephone calls to patients after hospitalization. Am. J. Med. 2001, 111, 26–30. [Google Scholar] [CrossRef] [Green Version]
- Szkiladz, A.; Carey, K.; Ackerbauer, K.; Heelon, M.; Friderici, J.; Kopcza, K. Impact of pharmacy student and resident-led discharge counseling on heart failure patients. J. Pharm. Pract. 2013, 26, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Warden, B.A.; Freels, J.P.; Furuno, J.P.; Mackay, J. Pharmacy-managed program for providing education and discharge instructions for patients with heart failure. Am. J. Health Syst. Pharm. 2014, 71, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Kaboli, P.J.; Hoth, A.B.; McClimon, B.J.; Schnipper, J.L. Clinical pharmacists and inpatient medical care: A systematic review. Arch. Intern. Med. 2006, 166, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Bian, R.; Mo, Y. Validation of the chinese version of the eight-item morisky medication adherence scale in patients with type 2 diabetes mellitus. J. Clin. Gerontol. Geriatr. 2013, 4, 119–122. [Google Scholar] [CrossRef]
- Overhage, J.M.; Lukes, A. Practical, reliable, comprehensive method for characterizing pharmacists’ clinical activities. Am. J. Health-Syst. Pharm. 1999, 56, 2444–2450. [Google Scholar] [PubMed]
- Graabaek, T.; Kjeldsen, L.J. Medication reviews by clinical pharmacists at hospitals lead to improved patient outcomes: A systematic review. Basic Clin. Pharmacol. Toxicol. 2013, 112, 359–373. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.F.; de Neto, A.C. Exploring elements of interprofessional collaboration between pharmacists and physicians in medication review. Pharm. World Sci. 2007, 29, 574–576. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.P.; van Noord, G.R. Pharmacotherapy consultation on polypharmacy patients in ambulatory care. Ann. Pharmacother. 2001, 35, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Perera, P.N.; Guy, M.C.; Sweaney, A.M.; Boesen, K.P. Evaluation of prescriber responses to pharmacist recommendations communicated by fax in a medication therapy management program (MTMP). J. Manag. Care Pharm. 2011, 17, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Doucette, W.R.; McDonough, R.P.; Klepser, D.; McCarthy, R. Comprehensive medication therapy management: Identifying and resolving drug-related issues in a community pharmacy. Clin. Ther. 2005, 27, 1104–1111. [Google Scholar] [CrossRef]
- Maheshkumar, V.P.; Dhanapal, C.K.; Ramakrishna, R.M. Outcomes of clinical pharmacist’s interventions in solving drug-related problems in geriatric patients of rural teaching hospital. Pharm. Innov. J. 2016, 5, 99–105. [Google Scholar]
- Wincent, M.M.; Potrilingam, D.; Anagha, V.; Jacob, S.C.; Andhuvan, G. Assessmet of drug related problems in patients with chronic diseases in the general medicine units of a tertiary care hospital. Int. J. Pharm. Pharm. Sci. 2017, 9, 194–200. [Google Scholar] [CrossRef]
- Ayalew, M.B.; Megersa, T.N.; Mengistu, Y.T. Drug-related problems in medical wards of tikur anbessa specialized hospital, ethiopia. J. Res. Pharm. Pract. 2015, 4, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Tigabu, B.M.; Daba, D.; Habte, B. Drug-related problems among medical ward patients in jimma university specialized hospital, southwest ethiopia. J. Res. Pharm. Pract. 2014, 3, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Koehler, B.E.; Richter, K.M.; Youngblood, L.; Cohen, B.A.; Prengler, I.D.; Cheng, D.; Masica, A.L. Reduction of 30-day post-discharge hospital readmission or emergency department (ed) visit rates in high-risk elderly medical patients through delivery of a targeted care bundle. J. Hosp. Med. 2009, 4, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.Y.; Colayco, D.; Hashimoto, J.; Komoto, K.; Gowda, C.; Wearda, B.; McCombs, J. Impact of a pharmacy-based transitional care program on hospital readmissions. Am. J. Manag. Care 2017, 23, 170–176. [Google Scholar] [PubMed]
- Haynes, R.B.; Yao, X.; Degani, A.; Kripalani, S.; Garg, A.; McDonald, H.P. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2008, 2. [Google Scholar] [CrossRef]
- DiMatteo, M.R.; Giordani, P.J.; Lepper, H.S.; Croghan, T.W. Patient adherence and medical treatment outcomes: A meta-analysis. Med. Care 2002, 40, 794–811. [Google Scholar] [CrossRef] [PubMed]
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of medication adherence on hospitalization risk and healthcare cost. Med. Care 2005, 43, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Osterberg, L.; Blaschke, T. Adherence to Medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Rosen, O.Z.; Fridman, R.; Rosen, B.T.; Shane, R.; Pevnick, J.M. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer. Adher. 2017, 11, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Taitel, M.; Jiang, J.; Rudkin, K.; Ewing, S.; Duncan, I. The impact of pharmacist face-to-face counseling to improve medication adherence among patients initiating statin therapy. Patient Prefer. Adher. 2012, 6, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Gillespie, U. Effects of Clinical Pharmacists’ Interventions: On Drug-Related Hospitalization and Appropriateness of Prescribing in Elderly Patients. Ph.D. Thesis, Uppsala University, Uppsala, Sweden, 2012. [Google Scholar]
| Patient Demographics (n and %) | Intervention (n = 43) | Usual Care (n = 42) | p-Value @ | ||
|---|---|---|---|---|---|
| DRP Identified (n = 14) | Non-DRP Identified (n = 29) | Overall (n = 43) | |||
| Age: mean ± SD | 82.1 ± 8.7 | 79.7 ± 8.0 | 80.5 ± 8.2 | 81.4 ± 8.1 | 0.597 + |
| Age: median | 82 | 83 | 82 | 81 | 0.740 # |
| Female gender | 11 (78.6%) | 17 (58.6%) | 28 (65.1%) | 25 (59.5%) | 0.595 # |
| Chinese ethnicity | 14 (100%) | 29 (100%) | 43 (100%) | 42 (100%) | / |
| With prior hospitalizations | 13 (92.9%) | 26 (89.7%) | 39 (90.7%) | 33 (78.6%) | 0.120 # |
| Length of hospital stay: mean ± SD (days) | 47.8 ± 27.8 | 27.5 ± 18.6 | 34.1 ± 23.7 | 38.2 ± 38.7 | 0.552 + |
| Principal diagnosis (n and %) | |||||
| Stroke | 8 (57.1%) | 21 (72.4%) | 29 (67.4%) | 30 (71.4%) | 0.690 # |
| ACS | 1 (7.1%) | 1 (3.4%) | 2 (4.7%) | 7 (16.7%) | 0.072 # |
| HF | 5 (35.7%) | 7 (24.1%) | 12 (27.9%) | 5 (11.9%) | 0.065 # |
| Medications Used | Intervention (n = 43) | Usual Care (n = 42) | p-Value @ | ||
|---|---|---|---|---|---|
| DRP Identified (n = 14) | Non-DRP Identified (n = 29) | Overall (n = 43) | |||
| Number of pre-admission routine medications | |||||
| Mean ± SD | 5.1 ± 2.7 | 4.5 ± 3.8 | 4.7 ± 3.5 | 5.1 ± 3.6 | 0.583 + |
| Polypharmacy (n and %) | 9 (64.3%) | 14 (48.3%) | 23 (53.5%) | 25 (59.5%) | 0.575 # |
| Total number of pre-admission medications: mean ± SD | 7.0 ± 3.4 | 5.6 ± 4.8 | 6.0 ± 4.4 | 6.8 ± 5.0 | 0.456 + |
| Number of discharge routine medications | |||||
| Mean ± SD | 7.1 ± 1.7 | 6.7 ± 2.0 | 6.8 ± 1.9 | 7.3 ± 2.9 | 0.334 + |
| Polypharmacy (n and %) | 14 (100%) | 29 (100%) | 43 (100%) | 42 (100%) | / |
| Total number of discharge medications: mean ± SD | 9.9 ± 2.8 | 8.2 ± 2.8 | 8.7 ± 2.9 | 9.3 ± 3.7 | 0.453 + |
| Primary Domain | Cause | Case (%) | Case (%) |
|---|---|---|---|
| Drug selection: related to the selection of drug | Inappropriate drug according to guidelines/formulary | 5 (17.9) | 11 (39.3) |
| No indication for drug | 3 (10.7) | ||
| No drug treatment despite existing indication | 3 (10.7) | ||
| Drug use process: related to the way patient gets the drug administered by a health professional or caregiver, despite proper dosage instructions given | Drug administered via wrong route | 9 (32.1) | 9 (32.1) |
| Dose selection: related to the selection of dose or dosage | Dosage regimen too frequent | 2 (7.1) | 4 (14.3) |
| Drug dose too low | 1 (3.6) | ||
| Dose timing instructions wrong, unclear, or missing | 1 (3.6) | ||
| Patient related: related to the patient and their behavior | Patient uses/takes more drug than prescribed | 1 (3.6) | 3 (10.7) |
| Patient takes food that interacts | 1 (3.6) | ||
| Patient stores drug inappropriately | 1 (3.6) | ||
| Other | No obvious cause | 1 (3.6) | 1 (3.6) |
| Primary Domain | Implementation | Case (%) | Case (%) |
|---|---|---|---|
| Intervention accepted | Intervention accepted and fully implemented | 47 (92.2) | 48 (94.1) |
| Intervention accepted, partially implemented | 1 (2.0) | ||
| Intervention not accepted | Intervention not accepted: unknown reason | 2 (3.9) | 3 (5.9) |
| Intervention not accepted: not feasible | 1 (2.0) |
| Adherence Category | Pre-Counseling (n = 34) | Post-Counseling (n = 43) | Changes | p-Value | OR (95% CI) |
|---|---|---|---|---|---|
| Low | 26 (76.5%) | 5 (11.6%) | −64.9% | <0.050 # | 0.04 (0.01–0.14) |
| Medium | 4 (11.8%) | 20 (46.5%) | +34.7% | 0.001 # | 6.52 (1.96–21.72) |
| High | 4 (11.8%) | 18 (41.9%) | +30.1% | 0.004 # | 5.40 (1.62–18.04) |
| Mean ± SD | 4.94 ± 1.52 | 7.08 ± 1.03 | <0.001 + |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ip, R.N.S.; Tenney, J.W.; Chu, A.C.K.; Chu, P.L.M.; Young, G.W.M. Pharmacist Clinical Interventions and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A Prospective Trial. Geriatrics 2018, 3, 53. https://doi.org/10.3390/geriatrics3030053
Ip RNS, Tenney JW, Chu ACK, Chu PLM, Young GWM. Pharmacist Clinical Interventions and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A Prospective Trial. Geriatrics. 2018; 3(3):53. https://doi.org/10.3390/geriatrics3030053
Chicago/Turabian StyleIp, Rosanna Nga Suet, Justin Wade Tenney, Angus Chun Kwok Chu, Pauline Lai Ming Chu, and Grace Wai Man Young. 2018. "Pharmacist Clinical Interventions and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A Prospective Trial" Geriatrics 3, no. 3: 53. https://doi.org/10.3390/geriatrics3030053




