Illness Representation and Self-Care Ability in Older Adults with Chronic Disease
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Sample Characteristics
3.2. Latent Profile Analysis
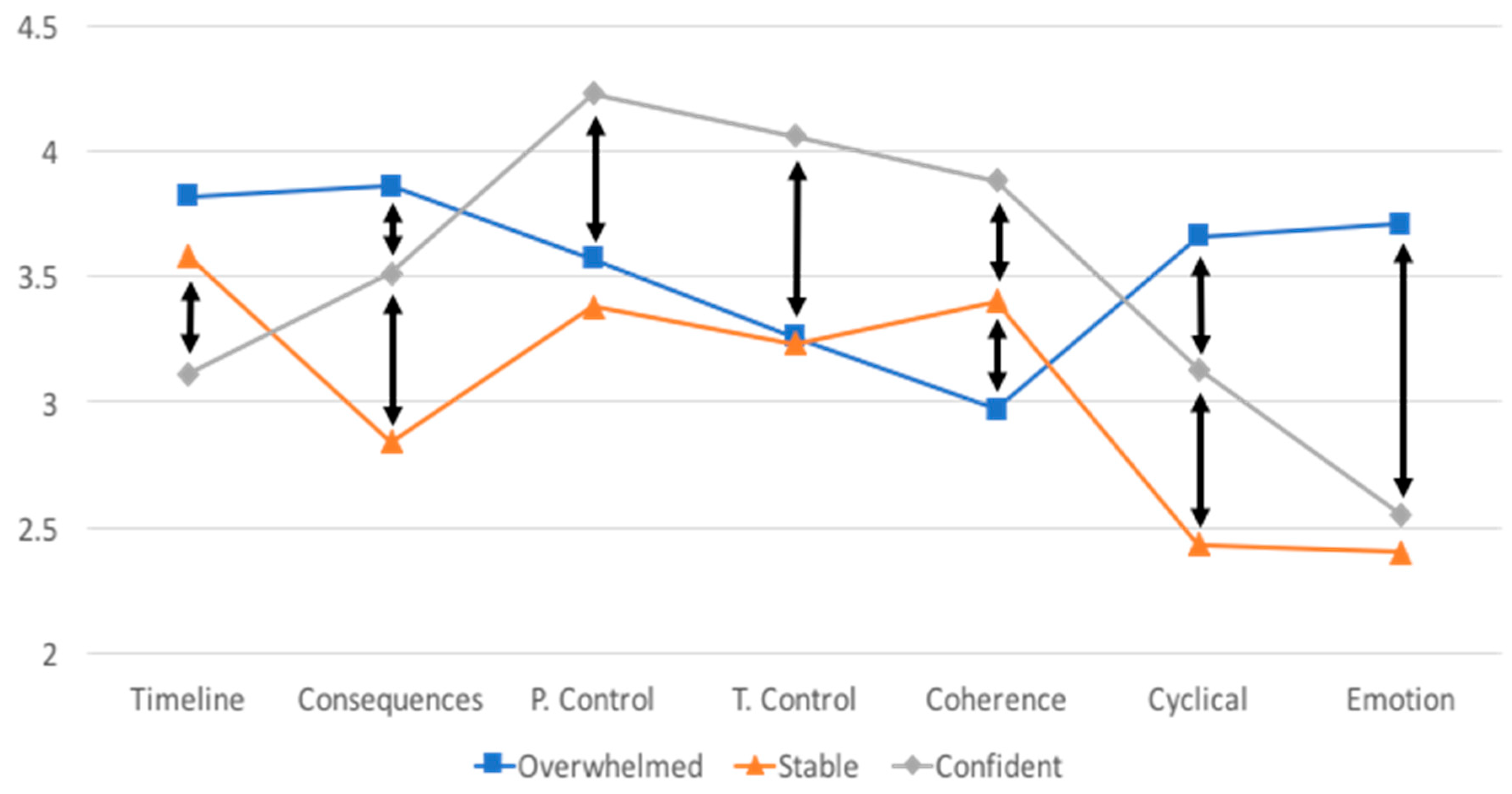
3.3. Group Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ward, B.W.; Schiller, J.S.; Goodman, R.A. Multiple chronic conditions among us adults: A 2012 update. Prev. Chronic Dis. 2014, 11, E62. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G. Chronic Care: Making the Case for Ongoing Care; Robert Wood Johnson Foundation: Princeton, NJ, USA, 2010. [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion. Chronic Disease Overview. Available online: https://www.cdc.gov/chronicdisease/overview/index.htm (accessed on 26 November 2017).
- Billings, J.; Raven, M.C. Dispelling an urban legend: Frequent emergency department users have substantial burden of disease. Health Aff. (Millwood) 2013, 32, 2099–2108. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, A.; Rogers, A.; Bower, P. Support for self care for patients with chronic disease. BMJ 2007, 335, 968–970. [Google Scholar] [CrossRef] [PubMed]
- Buck, H.G.; Dickson, V.V.; Fida, R.; Riegel, B.; D’Agostino, F.; Alvaro, R.; Vellone, E. Predictors of hospitalization and quality of life in heart failure: A model of comorbidity, self-efficacy and self-care. Int. J. Nurs. Stud. 2015, 52, 1714–1722. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.F.; Lee, M.C.; Liang, S.Y.; Lu, Y.Y.; Wang, T.J.; Tung, H.H. Effectiveness of a self-efficacy program for persons with diabetes: A randomized controlled trial. Nurs. Health Sci. 2011, 13, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Dickson, V.V.; Buck, H.; Riegel, B. Multiple comorbid conditions challenge heart failure self-care by decreasing self-efficacy. Nurs. Res. 2013, 62, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Franek, J. Self-management support interventions for persons with chronic disease: An evidence-based analysis. Ont. Health Technol. Assess. Ser. 2013, 13, 1–60. [Google Scholar] [PubMed]
- Jonkman, N.H.; Schuurmans, M.J.; Groenwold, R.H.H.; Hoes, A.W.; Trappenburg, J.C.A. Identifying components of self-management interventions that improve health-related quality of life in chronically ill patients: Systematic review and meta-regression analysis. Patient Educ. Couns. 2016, 99, 1087–1098. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Shorey, S.; Seah, B.; Chan, W.X.; Tam, W.W.S.; Wang, W. The effectiveness of psychological interventions on self-care, psychological and health outcomes in patients with chronic heart failure—A systematic review and meta-analysis. Int. J. Nurs. Stud. 2018, 78, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Jolly, K.; Majothi, S.; Sitch, A.J.; Heneghan, N.R.; Riley, R.D.; Moore, D.J.; Bates, E.J.; Turner, A.M.; Bayliss, S.E.; Price, M.J.; et al. Self-management of health care behaviors for copd: A systematic review and meta-analysis. Int. J. Chronic Obstruct. Pulm. Dis. 2016, 11, 305–326. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.C.; Wu, S.V.; Hsieh, N.C.; Tsai, J.M. Self-management programs on egfr, depression, and quality of life among patients with chronic kidney disease: A meta-analysis. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2016, 10, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Nerenz, D.R.; Steele, D.J. Illness representation and coping with health threats. In Social Psychological Aspects of Health; Baum, A., Taylor, S.E., Singer, J.E., Eds.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1984; Volume 4, pp. 219–252. [Google Scholar]
- Brandes, K.; Mullan, B. Can the common-sense model predict adherence in chronically ill patients? A meta-analysis. Health Psychol. Rev. 2014, 8, 129–153. [Google Scholar] [CrossRef] [PubMed]
- Dempster, M.; Howell, D.; McCorry, N.K. Illness perceptions and coping in physical health conditions: A meta-analysis. J. Psychosom. Res. 2015, 79, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Pickett, S.; Allen, W.; Franklin, M.; Peters, R.M. Illness beliefs in african americans with hypertension. West J. Nurs. Res. 2014, 36, 152–170. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Scharloo, M.; Abbink, J.; van’t Hul, A.; van Ranst, D.; Rudolphus, A.; Weinman, J.; Rabe, K.; Kaptein, A.A. The dynamics of illness perceptions: Testing assumptions of leventhal’s common-sense model in a pulmonary rehabilitation setting. Br. J. Health Psychol. 2010, 15, 887–903. [Google Scholar] [CrossRef] [PubMed]
- Wilski, M.; Tasiemski, T. Illness perception, treatment beliefs, self-esteem, and self-efficacy as correlates of self-management in multiple sclerosis. Acta Neurol. Scand. 2016, 133, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Kunschitz, E.; Friedrich, O.; Schoppl, C.; Maitz, J.; Sipotz, J. Illness perception patterns in patients with coronary artery disease. Psychol. Health Med. 2017, 22, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Frostholm, L.; Hornemann, C.; Ornbol, E.; Fink, P.; Mehlsen, M. Using illness perceptions to cluster chronic pain patients: Results from a trial on the chronic pain self-management program. Clin. J. Pain 2018. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.L.; Robertson, N.; Graham, C.D.; Williams, J.; Steiner, M.C.; Morgan, M.D.; Singh, S.J. Can we identify patients with different illness schema following an acute exacerbation of copd: A cluster analysis. Respir. Med. 2014, 108, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Lopes, A.C.; Xavier, R.F.; Ac Pereira, A.C.; Stelmach, R.; Fernandes, F.; Harrison, S.L.; Carvalho, C.R. Identifying copd patients at risk for worse symptoms, hrqol, and self-efficacy: A cluster analysis. Chronic Illn. 2018. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.A.; Posner, S.F.; Huang, E.S.; Parekh, A.K.; Koh, H.K. Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice. Prev. Chronic Dis. 2013, 10, E66. [Google Scholar] [CrossRef] [PubMed]
- Moss-Morris, R.; Weinman, J.; Petrie, K.J.; Horne, R.; Cameron, L.D.; Buick, D. The revised illness perception questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Weinman, J.; Petrie, K.J.; Moss-Morris, R.; Horne, R. The illness perception questionnaire: A new method for assessing the cognitive representation of illness. Psychol. Health 1996, 11, 431–435. [Google Scholar] [CrossRef]
- Cherrington, C.C.; Lawson, T.N.; Clark, K.B. Illness representation of patients with systolic heart failure. Prog. Cardiovasc. Nurs. 2006, 21, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Fowler, C.; Baas, L.S. Illness representations in patients with chronic kidney disease on maintenance hemodialysis. Nephrol. Nurs. J. 2006, 33, 173–174, 179–186. [Google Scholar] [PubMed]
- Chilcot, J.; Wellsted, D.; Farrington, K. Illness representations are associated with fluid nonadherence among hemodialysis patients. J. Psychosom. Res. 2010, 68, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the patient activation measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef] [PubMed]
- Zimbudzi, E.; Lo, C.; Ranasinha, S.; Fulcher, G.R.; Jan, S.; Kerr, P.G.; Polkinghorne, K.R.; Russell, G.; Walker, R.G.; Zoungas, S. Factors associated with patient activation in an australian population with comorbid diabetes and chronic kidney disease: A cross-sectional study. BMJ Open 2017, 7, e017695. [Google Scholar] [CrossRef] [PubMed]
- Aung, E.; Donald, M.; Williams, G.M.; Coll, J.R.; Doi, S.A. Joint influence of patient-assessed chronic illness care and patient activation on glycaemic control in type 2 diabetes. Int. J. Qual Health Care 2015, 27, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef] [PubMed]
- Bos-Touwen, I.; Schuurmans, M.; Monninkhof, E.M.; Korpershoek, Y.; Spruit-Bentvelzen, L.; Ertugrul-van der Graaf, I.; de Wit, N.; Trappenburg, J. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: A cross-sectional survey study. PLoS ONE 2015, 10, e0126400. [Google Scholar] [CrossRef] [PubMed]
- Watson, R.D.; Gibbs, C.R.; Lip, G.Y. Abc of heart failure. Clinical features and complications. BMJ 2000, 320, 236–239. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Kanso, A.; Sedor, J.R. Chronic kidney disease and its complications. Prim. Care 2008, 35, 329–344. [Google Scholar] [CrossRef] [PubMed]
- Simon, H.; Zieve, D. Chronic Obstructive Pulmonary Disease. Available online: http://www.umm.edu/health/medical/reports/articles/chronic-obstructive-pulmonary-disease (accessed on 26 November 2017).
- Gupta, S.; Goren, A.; Phillips, A.L.; Dangond, F.; Stewart, M. Self-reported severity among patients with multiple sclerosis in the U.S. And its association with health outcomes. Mult. Scler. Relat. Disord. 2014, 3, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Muthen, B.; Muthen, L.K. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcohol. Clin. Exp. Res. 2000, 24, 882–891. [Google Scholar] [CrossRef] [PubMed]
- Morgan, K.; Villiers-Tuthill, A.; Barker, M.; McGee, H. The contribution of illness perception to psychological distress in heart failure patients. BMC Psychol. 2014, 2, 50. [Google Scholar] [CrossRef] [PubMed]
- Meuleman, Y.; Chilcot, J.; Dekker, F.W.; Halbesma, N.; van Dijk, S. Health-related quality of life trajectories during predialysis care and associated illness perceptions. Health Psychol. 2017, 36, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Halding, A.G.; Grov, E.K. Self-rated health aspects among persons living with chronic obstructive pulmonary disease. Int. J. Chronic Obstruct. Pulmon. Dis. 2017, 12, 1163–1172. [Google Scholar] [CrossRef] [PubMed]
- Shively, M.J.; Gardetto, N.J.; Kodiath, M.F.; Kelly, A.; Smith, T.L.; Stepnowsky, C.; Maynard, C.; Larson, C.B. Effect of patient activation on self-management in patients with heart failure. J. Cardiovasc. Nurs. 2013, 28, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Porter, A.; Snooks, H.; Button, L.; Evans, B.A. The association between illness representation profiles and use of unscheduled urgent and emergency health care services. Br. J. Health Psychol. 2011, 16, 862–879. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Chang, C.; Chen, C.D. An investigation on illness perception and adherence among hypertensive patients. Kaohsiung J. Med. Sci. 2012, 28, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Rivera, E.; Corte, C. Person-centered analysis of illness representations: A systematic review of the literature. In Proceedings of the Midwest Nursing Research Society Conference, Minneapolis, MN, USA, 6–9 April 2017. [Google Scholar]
- Korpershoek, Y.; Bos-Touwen, I.D.; de Man-van Ginkel, J.M.; Lammers, J.W.; Schuurmans, M.J.; Trappenburg, J. Determinants of activation for self-management in patients with copd. Int. J. Chronic Obstruct. Pulmon. Dis. 2016, 11, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Shifren, K. Individual differences in the perception of optimism and disease severity: A study among individuals with parkinson’s disease. J. Behav. Med. 1996, 19, 241–271. [Google Scholar] [CrossRef] [PubMed]
- Flora, P.K.; Anderson, T.J.; Brawley, L.R. Illness perceptions and adherence to exercise therapy in cardiac rehabilitation participants. Rehabil. Psychol. 2015, 60, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Skinner, T.C.; Carey, M.E.; Cradock, S.; Dallosso, H.M.; Daly, H.; Davies, M.J.; Doherty, Y.; Heller, S.; Khunti, K.; Oliver, L.; et al. Comparison of illness representations dimensions and illness representation clusters in predicting outcomes in the first year following diagnosis of type 2 diabetes: Results from the desmond trial. Psychol. Health 2011, 26, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Fry, M.; Fitzpatrick, L.; Considine, J.; Shaban, R.Z.; Curtis, K. Emergency department utilisation among older people with acute and/or chronic conditions: A multi-centre retrospective study. Int. Emerg. Nurs. 2018, 37, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Powell, E.S.; Khare, R.K.; Courtney, D.M.; Feinglass, J. Lower mortality in sepsis patients admitted through the ed vs direct admission. Am. J. Emerg. Med. 2012, 30, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Berk, M.; Berk, L.; Dodd, S.; Jacka, F.N.; Fitzgerald, P.B.; de Castella, A.R.; Filia, S.; Filia, K.; Kulkarni, J.; Jackson, H.J.; et al. Psychometric properties of a scale to measure investment in the sick role: The illness cognitions scale. J. Eval. Clin. Pract. 2012, 18, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, A.A.; Bijsterbosch, J.; Scharloo, M.; Hampson, S.E.; Kroon, H.M.; Kloppenburg, M. Using the common sense model of illness perceptions to examine osteoarthritis change: A 6-year longitudinal study. Health Psychol. 2010, 29, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The brief illness perception questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. What Is Precision Medicine? Available online: https://ghr.nlm.nih.gov/primer/precisionmedicine/definition (accessed on 20 December 2017).
| Subscale | Definition | High Score Indicates | Number of Items |
|---|---|---|---|
| Timeline | Whether an individual perceives their disease to be acute or chronic in nature | A more chronic disease perception | 6 |
| Consequences | The extent of perceived consequences of the disease | More disease consequences | 6 |
| Personal Control | The amount of perceived control a person has over their disease | More control | 6 |
| Treatment Control | The amount of perceived control the medical treatments have over the disease | More control | 5 |
| Coherence | The perceived level of understanding of their disease | More understanding | 5 |
| Cyclical Timeline | Whether an individual perceives their disease to have a stable or unstable pattern from day today | More unstable disease pattern | 4 |
| Emotion | Amount of negative emotion an individual attribute to their disease | More negative emotion | 6 |
| Variables | Entire Sample n = 187 | Groups Derived from Latent Profile Analysis | Chi-Square or ANOVA | ||
|---|---|---|---|---|---|
| Overwhelmed n = 80 | Stable n = 61 | Confident n = 46 | |||
| Chronic Disease | 5.228 | ||||
| HF | 63 (33.7%) | 29 (36.3%) | 16 (26.2%) | 18 (39.1%) | |
| CKD | 65 (34.8%) | 24 (30.0%) | 28 (45.9%) | 13 (28.3%) | |
| COPD | 59 (31.6%) | 27 (33.8%) | 17 (27.9%) | 15 (32.6%) | |
| Age | 64.9 (SD = 8.9) | 64.5 (8.5) | 66.8 (8.8) | 63.1 (9.6) | 2.468 |
| Range: 50–88 | |||||
| Gender | 1.704 | ||||
| Female | 100 (53.8%) | 46 (57.5%) | 33 (55.0%) | 21 (45.7%) | |
| Male | 86 (46.2%) | 34 (42.5%) | 27 (45.0%) | 25 (54.3%) | |
| Race/ethnicity | 9.201 | ||||
| Black | 137 (73.7%) | 53 (66.3%) | 45 (75.0%) | 39 (84.8%) | |
| Hispanic | 15 (8.1%) | 7 (8.8%) | 5 (8.3%) | 3 (6.5%) | |
| White | 30 (16.1%) | 16 (20.0%) | 10 (16.7%) | 4 (8.7%) | |
| Asian | 4 (2.2%) | 4 (5.0%) | 0 (0.0%) | 0 (0.0%) | |
| Education | 0.798 | ||||
| ≤High school | 96 (51.9%) | 38 (48.1%) | 33 (55.0%) | 25 (54.3%) | |
| >High school | 89 (48.1%) | 41 (51.9%) | 27 (45.0%) | 21 (45.7%) | |
| Severity variables | |||||
| Years with disease | 6.9 (SD = 8.6) | 5.3 (5.2) a | 10.3 (12.0) b | 5.3 (6.9) a | 6.550 ** |
| Range: 1–55 | |||||
| Complications | 1.68 (SD = 1.0) | 1.84 (1.0) a | 1.38 (1.0) b | 1.80 (1.1) ab | 3.965 * |
| Range: 0–4 | |||||
| Comorbid conditions | 3.2 (SD = 1.7) | 1.32 | |||
| Range: 0–8 | 3.3 (1.8) | 2.9 (1.4) | 3.3 (1.6) | ||
| Severity | 8.713 | ||||
| Mild | 56 (31.3%) | 19 (24.7%) | 24 (42.1%) | 13 (28.9%) | |
| Moderate | 82 (45.8%) | 34 (44.2%) | 23 (40.4%) | 25 (55.6%) | |
| Severe | 41 (22.9%) | 24 (31.2%) | 10 (17.5%) | 7 (15.6%) | |
| Illness representation variables | |||||
| Timeline | 3.57 (SD = 0.87) | 3.82 (0.76) a | 3.58 (0.81) a | 3.11 (0.98) b | 10.750 *** |
| Range: 1.2–5 | |||||
| Consequences | 3.44 (SD = 0.76) | 3.86 (0.61) a | 2.84 (0.60) b | 3.51 (0.65) c | 48.49 *** |
| Range: 1.2–5 | |||||
| Personal Control | 3.67 (SD = 0.65) | 3.57 (0.57) a | 3.38 (0.62) a | 4.23 (0.47) b | 32.49 *** |
| Range: 2–5 | |||||
| Treatment Control | 3.45 (SD = 0.64) | 3.26 (0.58) a | 3.23 (0.54) a | 4.06 (0.45) b | 39.12 *** |
| Range: 1.8–5 | |||||
| Coherence | 3.33 (SD = 0.85) | 2.97 (0.85) a | 3.40 (0.77) b | 3.88 (0.61) c | 20.80 *** |
| Range: 1–5 | |||||
| Cyclical | 3.13 (SD = 0.87) | 3.66 (0.67) a | 2.43 (0.63) b | 3.13 (0.80) c | 54.37 *** |
| Range: 1–5 | |||||
| Emotion | 3.00 (SD = 0.93) | 3.71 (0.72) a | 2.40 (0.62) b | 2.55 (0.74) b | 73.75 *** |
| Range: 1–5 | |||||
| Outcome variables | |||||
| ED visits | 3.976 | ||||
| 0 | 83 (44.4%) | 29 (36.3%) | 32 (52.5%) | 22 (47.8%) | |
| ≥1 | 104 (55.6%) | 51 (63.8%) | 29 (47.5%) | 24 (52.2%) | |
| Hospitalizations | 7.842 * | ||||
| 0 | 86 (46.0%) | 31 (38.8%) | 37 (60.7%) | 18 (39.1%) | |
| ≥1 | 101 (54.0%) | 49 (61.3%) a | 24 (39.3%) b | 28 (60.9%) a | |
| PAM score | 5.783 | ||||
| Low activation | 84 (44.9%) | 42 (52.5%) | 28 (45.9%) | 14 (30.4%) | |
| High activation | 103 (55.1%) | 38 (47.5%) a | 33 (54.1%) ab | 32 (69.6%) b | |
| Variables | ED Visits (≥1) | Hospitalizations (≥1) | Self-Care Activation (High) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | Z | p | OR | Z | p | OR | Z | p | |
| Model 1: Groups only (n = 187) | |||||||||
| Stable = 0 Overwhelmed = 1 | 1.942 | −1.92 | 0.055 | 2.439 | −2.56 | 0.011 | 0.768 | 0.78 | 0.438 |
| Confident = 0 Overwhelmed = 1 | 1.613 | −1.27 | 0.204 | 1.016 | −0.04 | 0.966 | 0.387 | 2.37 | 0.018 |
| Stable = 0 Confident = 1 | 1.204 | 0.47 | 0.635 | 2.437 | 2.19 | 0.029 | 1.939 | 1.61 | 0.107 |
| Model 2: Groups plus disease years and complications (n = 171) | |||||||||
| Stable = 0 Overwhelmed = 1 | 1.848 | −1.56 | 0.118 | 1.701 | −1.37 | 0.171 | 0.938 | 0.17 | 0.866 |
| Confident = 0 Overwhelmed = 1 | 1.730 | −1.38 | 0.169 | 0.975 | −0.06 | 0.949 | 0.352 | 2.52 | 0.012 |
| Stable = 0 Confident = 1 | 1.068 | 0.15 | 0.879 | 1.751 | 1.28 | 0.200 | 2.662 | 2.15 | 0.031 |
| Years since diagnosis | 1.016 | 0.78 | 0.437 | 0.995 | −0.27 | 0.786 | 1.030 | 1.41 | 0.159 |
| Complications | 1.460 | 2.32 | 0.020 | 1.524 | 2.57 | 0.010 | 0.915 | −0.56 | 0.573 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rivera, E.; Corte, C.; Steffen, A.; DeVon, H.A.; Collins, E.G.; McCabe, P.J. Illness Representation and Self-Care Ability in Older Adults with Chronic Disease. Geriatrics 2018, 3, 45. https://doi.org/10.3390/geriatrics3030045
Rivera E, Corte C, Steffen A, DeVon HA, Collins EG, McCabe PJ. Illness Representation and Self-Care Ability in Older Adults with Chronic Disease. Geriatrics. 2018; 3(3):45. https://doi.org/10.3390/geriatrics3030045
Chicago/Turabian StyleRivera, Eleanor, Colleen Corte, Alana Steffen, Holli A. DeVon, Eileen G. Collins, and Pamela J. McCabe. 2018. "Illness Representation and Self-Care Ability in Older Adults with Chronic Disease" Geriatrics 3, no. 3: 45. https://doi.org/10.3390/geriatrics3030045
APA StyleRivera, E., Corte, C., Steffen, A., DeVon, H. A., Collins, E. G., & McCabe, P. J. (2018). Illness Representation and Self-Care Ability in Older Adults with Chronic Disease. Geriatrics, 3(3), 45. https://doi.org/10.3390/geriatrics3030045





