UnderstandingDelirium.ca: A Mixed-Methods Observational Evaluation of an Internet-Based Educational Intervention for the Public and Care Partners
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Recruitment
2.3. Outcomes
2.4. Data Analysis
2.4.1. Quantitative Data Analysis
2.4.2. Qualitative Data Analysis
2.5. Data Integration
2.6. Ethics Approval
3. Results
3.1. e-Learning Lesson Uptake
3.2. Demographics
3.3. Quantitative Analysis
3.4. Qualitative Analysis
“It was helpful to understand how it is different from dementia. Dementia is such a well-discussed topic, and I’m sure so many lay people are not very familiar with delirium and simply assume their loved one is experiencing dementia.”(ID 629)
“My husband died of pancreatic cancer a year ago. I wish I’d known more about delirium then, because that knowledge would’ve helped me understand what he was going through in the weeks before his death. Now, in retrospect and with the information presented in these lessons, it all makes so much more sense. Thank you.”(ID 529)
“Almost 18 months ago I experienced delirium while in hospital. I am just now coming to terms with all the pieces this was complicated by system becoming septic twice ….actually did almost die twice. Still feel fearful…..cannot remember much of 1st year of recovery. Finally understanding what happened…and be less fearful.”(ID 103)
“I will share this lesson with family members and friends who have parents experiencing delirium.”(ID 313)
“My father experienced delirium after surgery to remove stomach cancer 10 yrs ago...No one on the team explained what was happening. The amount of stress we suffered trying to figure out what was happening was immense.”(ID 62)
3.5. Integration of Quantitative and Qualitative Findings
4. Discussion
4.1. Comparison with Previous Research
4.2. Alignment with Clinical Guidelines and Implications for Practice
4.3. Limitations
4.4. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IAM4all-SF | Information Assessment Method for patients and consumers short form version |
| IAM4all | Information Assessment Method for patients and consumers |
| NPS | Net Promoter Score |
References
- De Lange, E.; Verhaak, P.F.M.; Van Der Meer, K. Prevalence, Presentation and Prognosis of Delirium in Older People in the Population, at Home and in Long Term Care: A Review. Int. J. Geriatr. Psychiatry 2013, 28, 127–134. [Google Scholar] [CrossRef]
- Chen, F.; Liu, L.; Wang, Y.; Liu, Y.; Fan, L.; Chi, J. Delirium Prevalence in Geriatric Emergency Department Patients: A Systematic Review and Meta-Analysis. Am. J. Emerg. Med. 2022, 59, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Tong, T.; Chignell, M.; Tierney, M.C.; Goldstein, J.; Eagles, D.; Perry, J.J.; McRae, A.; Lang, E.; Hefferon, D.; et al. Prevalence, Management and Outcomes of Unrecognized Delirium in a National Sample of 1493 Older Emergency Department Patients: How Many Were Sent Home and What Happened to Them? Age Ageing 2022, 51, 16. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.; e Silva, L.; Berning, M.J.; Stanich, J.A.; Gerberi, D.J.; Murad, M.H.; Han, J.H.; Bellolio, F. Risk Factors for Delirium in Older Adults in the Emergency Department: A Systematic Review and Meta-Analysis. Ann. Emerg. Med. 2021, 78, 549–565. [Google Scholar] [CrossRef] [PubMed]
- O’Regan, N.A.; Fitzgerald, J.; Adamis, D.; Molloy, D.W.; Meagher, D.; Timmons, S. Predictors of Delirium Development in Older Medical Inpatients: Readily Identifiable Factors at Admission. J. Alzheimers. Dis. 2018, 64, 775–785. [Google Scholar] [CrossRef] [PubMed]
- Vasilevskis, E.E.; Han, J.H.; Hughes, C.G.; Ely, E.W. Epidemiology and Risk Factors for Delirium across Hospital Settings. Best Pr. Res. Clin. Anaesthesiol. 2012, 26, 277–287. [Google Scholar] [CrossRef] [PubMed]
- Gibb, K.; Seeley, A.; Quinn, T.; Siddiqi, N.; Shenkin, S.; Rockwood, K.; Davis, D. The Consistent Burden in Published Estimates of Delirium Occurrence in Medical Inpatients over Four Decades: A Systematic Review and Meta-Analysis Study. Age Ageing 2020, 49, 352–360. [Google Scholar] [CrossRef]
- Meyer, G.; Mauch, M.; Seeger, Y.; Burckhardt, M. Experiences of Relatives of Patients with Delirium Due to an Acute Health Event—A Systematic Review of Qualitative Studies. Appl. Nurs. Res. 2023, 73, 151722. [Google Scholar] [CrossRef]
- Shrestha, P.; Fick, D.M. Family Caregiver’s Experience of Caring for an Older Adult with Delirium: A Systematic Review. Int. J. Older People Nurs. 2020, 15, e12321. [Google Scholar] [CrossRef]
- Chuen, V.L.; Chan, A.C.H.; Ma, J.; Alibhai, S.M.H.; Chau, V. The Frequency and Quality of Delirium Documentation in Discharge Summaries. BMC Geriatr. 2021, 21, 307. [Google Scholar] [CrossRef]
- Martinez, F.T.; Tobar, C.; Beddings, C.I.; Vallejo, G.; Fuentes, P. Preventing Delirium in an Acute Hospital Using a Non-Pharmacological Intervention. Age Ageing 2012, 41, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Rosgen, B.K.; Krewulak, K.D.; Davidson, J.E.; Ely, E.W.; Stelfox, H.T.; Fiest, K.M. Associations between Caregiver-Detected Delirium and Symptoms of Depression and Anxiety in Family Caregivers of Critically Ill Patients: A Cross-Sectional Study. BMC Psychiatry 2021, 21, 187. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.T.; Dhesi, J.K.; Partridge, J.S.L. Distress in Delirium: Causes, Assessment and Management. Eur. Geriatr. Med. 2020, 11, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Carbone, M.K.; Gugliucci, M.R. Delirium and the Family Caregiver: The Need for Evidence-Based Education Interventions. Gerontologist 2015, 55, 345–352. [Google Scholar] [CrossRef]
- Barbara, A.M.; Dobbins, M.; Haynes, R.B.; Iorio, A.; Lavis, J.N.; Raina, P.; Levinson, A.J. The McMaster Optimal Aging Portal: Usability Evaluation of a Unique Evidence-Based Health Information Website. JMIR Hum. Factors 2016, 3, e14. [Google Scholar] [CrossRef]
- Barbara, A.; Dobbins, M.; Haynes, R.; Iorio, A.; Lavis, J.; Levinson, A.J. User Experiences of the McMaster Optimal Aging Portal’s Evidence Summaries and Blog Posts: Usability Study. JMIR Hum. Factors 2016, 3, e22. [Google Scholar] [CrossRef]
- Reichheld, F.F. The One Number You Need to Grow. Harv. Bus Rev. 2003, 81, 46–54. [Google Scholar]
- Pluye, P.; Granikov, V.; Bartlett, G.; Grad, R.M.; Tang, D.L.; Johnson-Lafleur, J.; Shulha, M.; Galvão, M.C.B.; Ricarte, I.L.M.; Stephenson, R.; et al. Development and Content Validation of the Information Assessment Method for Patients and Consumers. JMIR Res. Protoc. 2014, 3, e2908. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Creswell, J.W.; Fetters, M.D.; Ivankova, N.V. Designing A Mixed Methods Study In Primary Care. Ann. Fam. Med. 2004, 2, 7–12. [Google Scholar] [CrossRef]
- Neil-Sztramko, S.E.; Farran, R.; Watson, S.; Levinson, A.J.; Lavis, J.N.; Iorio, A.; Dobbins, M. If You Build It, Who Will Come? A Description of User Characteristics and Experiences With the McMaster Optimal Aging Portal. Gerontol. Geriatr. Med. 2017, 3, 2333721417737681. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.F.; Ayers, S.; Pluye, P.; Grad, R.; Sztramko, R.; Marr, S.; Papaioannou, A.; Clark, S.; Gerantonis, P.; Levinson, A.J. Impact and Perceived Value of IGeriCare E-Learning Among Dementia Care Partners and Others: Pilot Evaluation Using the IAM4all Questionnaire. JMIR Aging 2022, 5, e40357. [Google Scholar] [CrossRef] [PubMed]
- Bull, M.J.; Boaz, L.; Jermé, M. Educating Family Caregivers for Older Adults About Delirium: A Systematic Review. Worldviews Evid Based Nurs. 2016, 13, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Bull, M.J.; Avery, J.S.; Boaz, L.; Oswald, D. Psychometric Properties of the Family Caregiver Delirium Knowledge Questionnaire. Res. Gerontol. Nurs. 2015, 8, 198–207. [Google Scholar] [CrossRef]
- Wong, S.P.; Tu, J.; Downie, S.; Heflin, M.T.; McDonald, S.R.; Yanamadala, M. Delirium Education for Geriatric Patients and Their Families: A Quality Improvement Initiative✰. Aging Health Res. 2023, 3, 100123. [Google Scholar] [CrossRef]
- Alaujan, R.; Alhinti, S.; Alharbi, M.; Basakran, F.; Ahmed, M.; Almodaimegh, H. Delirium Knowledge, Risk Factors, and Attitude among General Public in Riyadh, Saudi Arabia, a Cross-Sectional Study. Int. J. Med. Dev. Ctries. 2022, 6, 957. [Google Scholar] [CrossRef]
- Alshurtan, K.; Ali Alshammari, F.; Alshammari, A.B.; Alreheili, S.H.; Aljassar, S.; Alessa, J.A.; Al Yateem, H.A.; Almutairi, M.; Altamimi, A.F.; Altisan, H.A. Delirium Knowledge, Risk Factors, and Attitude Among the General Public in Saudi Arabia: A Cross-Sectional Study. Cureus 2024, 16, e59263. [Google Scholar] [CrossRef]
- Zhai, S.; Chu, F.; Tan, M.; Chi, N.C.; Ward, T.; Yuwen, W. Digital Health Interventions to Support Family Caregivers: An Updated Systematic Review. Digit. Health 2023, 9, 20552076231171967. [Google Scholar] [CrossRef]
- Crone, C.; Fochtmann, L.J.; Ahmed, I.; Balas, M.C.; Boland, R.; Escobar, J.I.; Heinrich, T.; Jackson-Triche, M.; Levenson, J.L.; Mattison, M.; et al. The American Psychiatric Association Practice Guideline for the Prevention and Treatment of Delirium. Am. J. Psychiatry 2025, 182, 880–884. [Google Scholar] [CrossRef]
| Variables | Responses, n (%) |
|---|---|
| Arrived at lesson through (n = 621) | |
| McMaster Optimal Aging Portal e-newsletter | 496 (79.8) |
| links from friends | 36 (5.8) |
| healthcare professional recommendation | 35 (5.6) |
| other websites | 14 (2.3) |
| search engine | 12 (1.9) |
| links on social media | 8 (1.3) |
| Gender (n = 619) | |
| Female | 528 (85.4) |
| Male | 85 (13.8) |
| Prefer not to say | 4 (0.7) |
| Other | 1 (0.2) |
| Age (n = 610) | |
| ≥75 years old | 216 (35.4) |
| 65–74 years old | 222 (36.4) |
| 55–64 years old | 99 (16.2) |
| 45–54 years old | 35 (5.7) |
| 35–44 years old | 22 (3.6) |
| 25–34 years old | 12 (2.0) |
| 18–24 years old | 4 (0.7) |
| Responses, n (%) | ||||||
|---|---|---|---|---|---|---|
| Strongly Disagree | Somewhat Disagree | Neither Agree nor Disagree | Somewhat Agree | Strongly Agree | Total | |
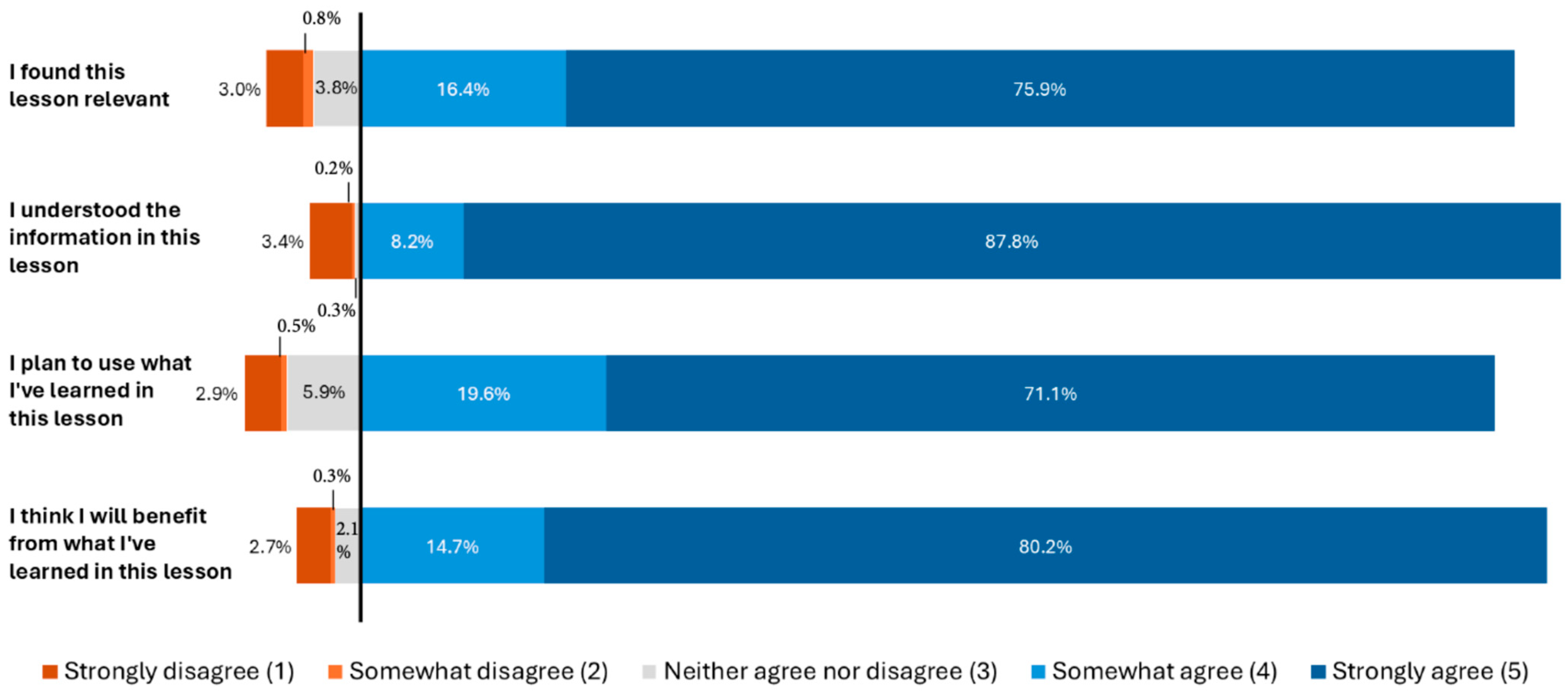
| I found this lesson relevant. | 19 (3.0) | 5 (0.8) | 24 (3.8) | 103 (16.4) | 476 (75.9) | 627 (100) |
| I understood the information in this lesson. | 21 (3.4) | 1 (0.2) | 3 (0.5) | 51 (8.2) | 548 (87.8) | 624 (100) |
| I plan to use what I’ve learned in this lesson. | 18 (2.9) | 3 (0.5) | 37 (5.9) | 123 (19.6) | 446 (71.1) | 627 (100) |
| I think I will benefit from what I’ve learned in this lesson. | 17 (2.7) | 2 (0.3) | 13 (2.1) | 92 (14.7) | 502 (80.2) | 626 (100) |
| Mean (SD) | Median | Mode | Frequency of the Mode (%) | Interquartile Range | |
|---|---|---|---|---|---|
| I found this lesson relevant. | 4.61 (0.85) | 5.0 | 5 | 476 (63.2) | 0 |
| I understood the information in this lesson. | 4.77 (0.78) | 5.0 | 5 | 548 (72.8) | 0 |
| I plan to use what I’ve learned in this lesson. | 4.56 (0.86) | 5.0 | 5 | 446 (59.2) | 1 |
| I think I will benefit from what I’ve learned in this lesson. | 4.69 (0.78) | 5.0 | 5 | 501 (66.5) | 0 |
| Themes | Subthemes |
|---|---|
| 1. Educational value of the lesson | a. Informative and educational b. Better understanding of delirium vs. dementia c. Useful to better understanding of prior experiences with delirium d. Refresher/reinforcement of knowledge e. Clarity and organization of content |
| 2. Personal and professional relevance | a. Personal use: Intend to share lesson/knowledge dissemination b. Personal use: Awareness and proactive health management for others c. Personal use: Awareness and proactive health management for themselves d. Professional use: Awareness and proactive health management for patients/clients |
| 3. Suggestions for improvements | a. Technical issues/suggestions b. Formatting issues/suggestions c. Content expansion/suggestions |
| 4. Emotional and psychological impact | a. Relief, clarification and gratitude b. Anxiety, fear and sadness-induced by lesson content c. Anxiety, fear and sadness-induced by experience/recollection |
| 5. Healthcare system and professional support | a. Need for better professional support: General b. Lack of information in the healthcare and professional support system c. Lack of communication in the healthcare and professional support system d. Missed diagnosis/ignored brought up concerns e. This lesson as candidate for training professionals and patients |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, R.; Hadid, D.; Ayers, S.; Clark, S.; Woodburn, R.; Grad, R.; Levinson, A.J. UnderstandingDelirium.ca: A Mixed-Methods Observational Evaluation of an Internet-Based Educational Intervention for the Public and Care Partners. Geriatrics 2025, 10, 168. https://doi.org/10.3390/geriatrics10060168
Shen R, Hadid D, Ayers S, Clark S, Woodburn R, Grad R, Levinson AJ. UnderstandingDelirium.ca: A Mixed-Methods Observational Evaluation of an Internet-Based Educational Intervention for the Public and Care Partners. Geriatrics. 2025; 10(6):168. https://doi.org/10.3390/geriatrics10060168
Chicago/Turabian StyleShen, Randi, Dima Hadid, Stephanie Ayers, Sandra Clark, Rebekah Woodburn, Roland Grad, and Anthony J. Levinson. 2025. "UnderstandingDelirium.ca: A Mixed-Methods Observational Evaluation of an Internet-Based Educational Intervention for the Public and Care Partners" Geriatrics 10, no. 6: 168. https://doi.org/10.3390/geriatrics10060168
APA StyleShen, R., Hadid, D., Ayers, S., Clark, S., Woodburn, R., Grad, R., & Levinson, A. J. (2025). UnderstandingDelirium.ca: A Mixed-Methods Observational Evaluation of an Internet-Based Educational Intervention for the Public and Care Partners. Geriatrics, 10(6), 168. https://doi.org/10.3390/geriatrics10060168







