Reevaluating Calf Circumference as an Indicator of Muscle Mass in Malnutrition Among Community-Dwelling Older Adults: A Cross-Sectional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Malnutrition
2.3. Health Conditions
2.3.1. Frailty
2.3.2. Disability
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
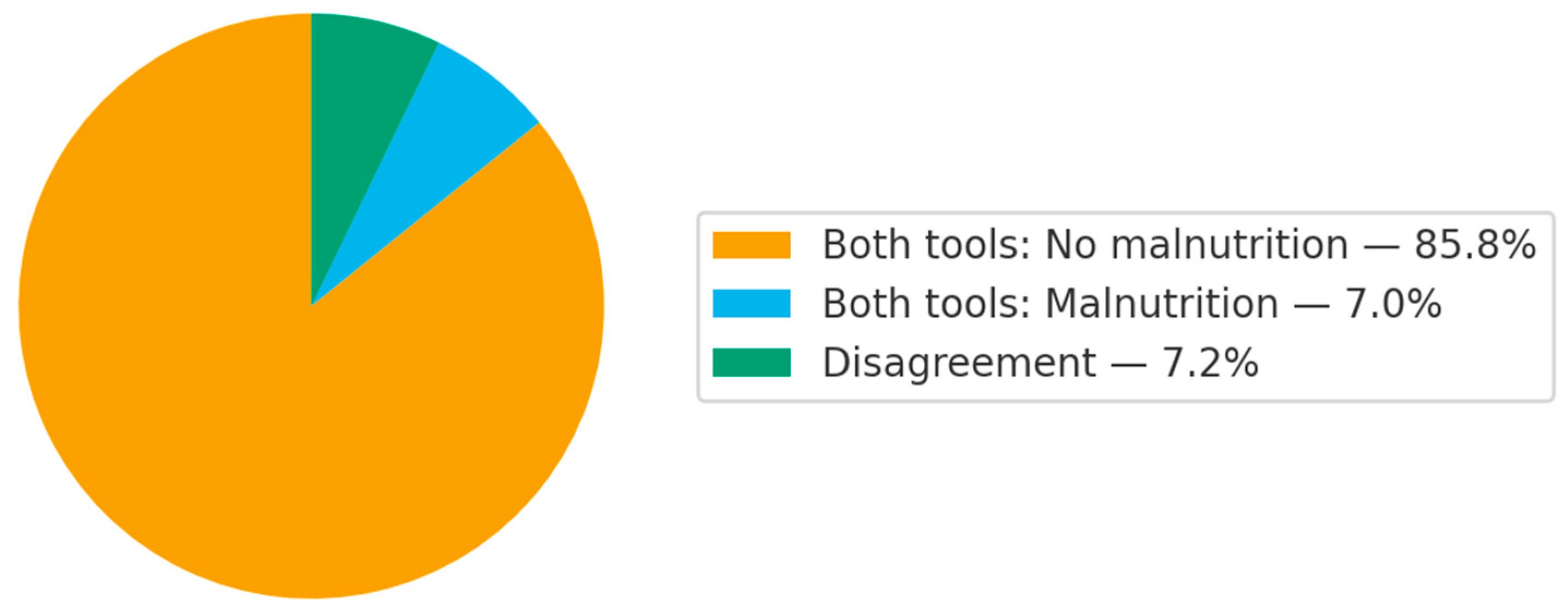
3.2. Agreement for Malnutrition Between Assessment Methods
3.3. Associations Between Assessment Methods
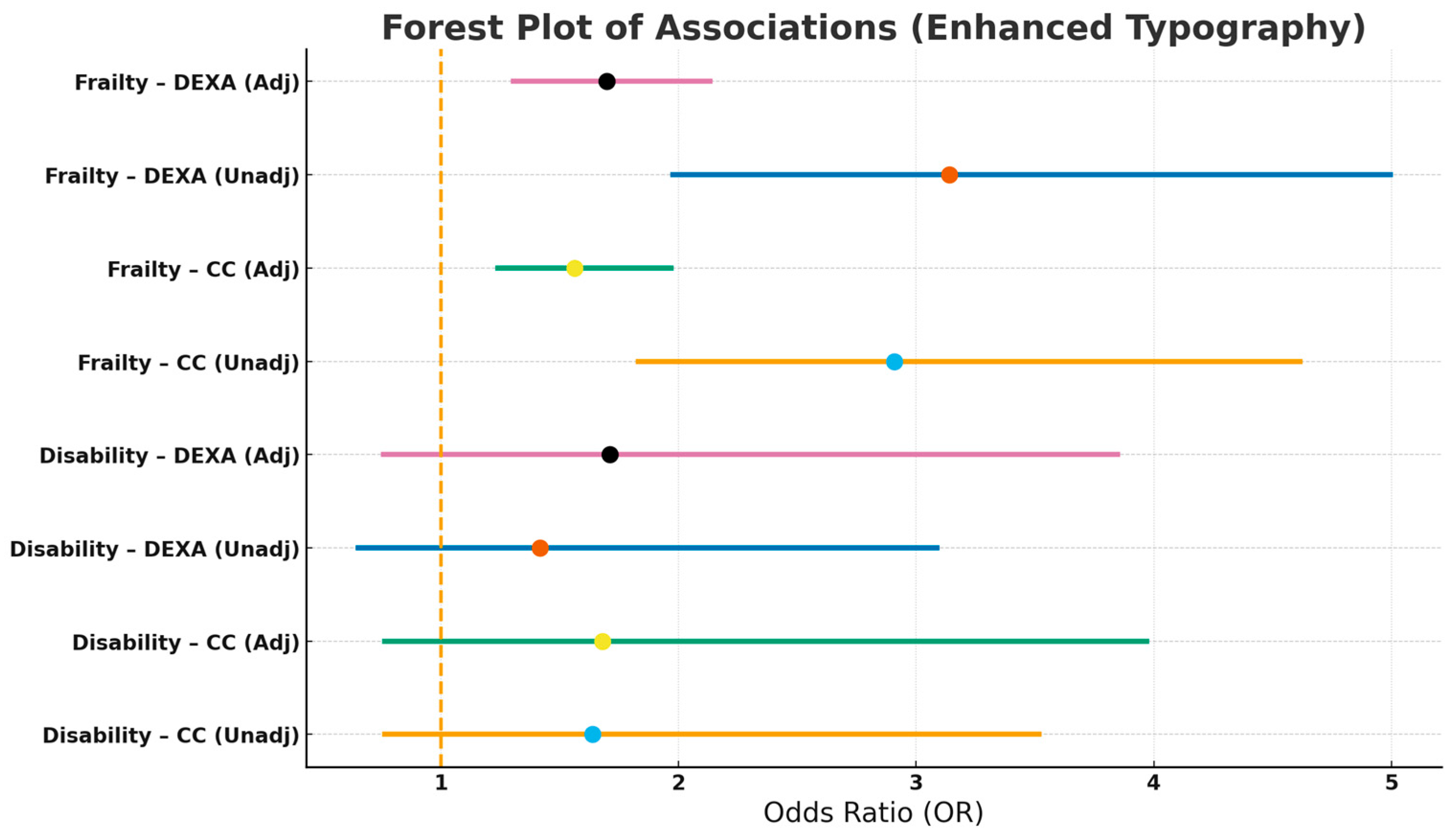
3.4. Associations Between Malnutrition with Disability and Frailty
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jensen, G.L.; Cederholm, T.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; de Baptista, G.A.; Barazzoni, R.; Blaauw, R.; Coats, A.J.S.; et al. GLIM Criteria for the Diagnosis of Malnutrition: A Consensus Report From the Global Clinical Nutrition Community. JPEN J. Parenter. Enteral Nutr. 2019, 43, 32–40. [Google Scholar] [CrossRef]
- Kupisz-Urbanska, M.; Marcinowska-Suchowierska, E. Malnutrition in Older Adults-Effect on Falls and Fractures: A Narrative Review. Nutrients 2022, 14, 3123. [Google Scholar] [CrossRef]
- Yeung, S.S.Y.; Chan, R.S.M.; Kwok, T.; Lee, J.S.W.; Woo, J. Malnutrition According to GLIM Criteria and Adverse Outcomes in Community-Dwelling Chinese Older Adults: A Prospective Analysis. J. Am. Med. Dir. Assoc. 2021, 22, 1953–1959.e4. [Google Scholar] [CrossRef] [PubMed]
- Söderström, L.; Rosenblad, A.; Thors Adolfsson, E.; Bergkvist, L. Malnutrition Is Associated with Increased Mortality in Older Adults Regardless of the Cause of Death. Br. J. Nutr. 2017, 117, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Streicher, M.; van Zwienen-Pot, J.; Bardon, L.; Nagel, G.; Teh, R.; Meisinger, C.; Colombo, M.; Torbahn, G.; Kiesswetter, E.; Flechtner-Mors, M.; et al. Determinants of Incident Malnutrition in Community-Dwelling Older Adults: A MaNuEL Multicohort Meta-Analysis. J. Am. Geriatr. Soc. 2018, 66, 2335–2343. [Google Scholar] [CrossRef]
- Correia, M.I.T.D.; Tappenden, K.A.; Malone, A.; Prado, C.M.; Evans, D.C.; Sauer, A.C.; Hegazi, R.; Gramlich, L. Utilization and Validation of the Global Leadership Initiative on Malnutrition (GLIM): A Scoping Review. Clin. Nutr. 2022, 41, 687–697. [Google Scholar] [CrossRef]
- Coelho-Júnior, H.J.; Marzetti, E. Capturing What Counts in Muscle Failure: A Critical Appraisal of the Current Operational Models of Sarcopenia. Lancet Healthy Longev. 2025, 6, 100756. [Google Scholar] [CrossRef]
- Kiss, C.M.; Bertschi, D.; Beerli, N.; Berres, M.; Kressig, R.W.; Fischer, A.M. Calf Circumference as a Surrogate Indicator for Detecting Low Muscle Mass in Hospitalized Geriatric Patients. Aging Clin. Exp. Res. 2024, 36, 25. [Google Scholar] [CrossRef]
- Rolland, Y.; Lauwers-Cances, V.; Cournot, M.; Nourhashémi, F.; Reynish, W.; Rivière, D.; Vellas, B.; Grandjean, H. Sarcopenia, Calf Circumference, and Physical Function of Elderly Women: A Cross-Sectional Study. J. Am. Geriatr. Soc. 2003, 51, 1120–1124. [Google Scholar] [CrossRef]
- Kawakami, R.; Murakami, H.; Sanada, K.; Tanaka, N.; Sawada, S.S.; Tabata, I.; Higuchi, M.; Miyachi, M. Calf Circumference as a Surrogate Marker of Muscle Mass for Diagnosing Sarcopenia in Japanese Men and Women. Geriatr. Gerontol. Int. 2015, 15, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, R.; Miyachi, M.; Sawada, S.S.; Torii, S.; Midorikawa, T.; Tanisawa, K.; Ito, T.; Usui, C.; Ishii, K.; Suzuki, K.; et al. Cut-Offs for Calf Circumference as a Screening Tool for Low Muscle Mass: WASEDA’S Health Study. Geriatr. Gerontol. Int. 2020, 20, 943–950. [Google Scholar] [CrossRef]
- Soeters, P.B.; Wolfe, R.R.; Shenkin, A. Hypoalbuminemia: Pathogenesis and Clinical Significance. JPEN J. Parenter. Enteral Nutr. 2019, 43, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Allison, S.P.; Lobo, D.N. The Clinical Significance of Hypoalbuminaemia. Clin. Nutr. 2024, 43, 909–914. [Google Scholar] [CrossRef]
- About NHANES|National Health and Nutrition Examination Survey|CDC. Available online: https://www.cdc.gov/nchs/nhanes/about/ (accessed on 23 October 2025).
- NHANES 2001-2002 Laboratory Data Overview. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/overviewlab.aspx?BeginYear=2001 (accessed on 23 October 2025).
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- NHANES Body Composition Procedures Manual 2021. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/public/2021/manuals/2021-Body-Composition-Procedures-508.pdf (accessed on 23 October 2025).
- Gonzalez, M.C.; Mehrnezhad, A.; Razaviarab, N.; Barbosa-Silva, T.G.; Heymsfield, S.B. Calf Circumference: Cutoff Values from the NHANES 1999–2006. Am. J. Clin. Nutr. 2021, 113, 1679. [Google Scholar] [CrossRef]
- Morley, J.E.; Malmstrom, T.K.; Miller, D.K. A Simple Frailty Questionnaire (FRAIL) Predicts Outcomes in Middle Aged African Americans. J. Nutr. Health Aging 2012, 16, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Gao, Y.; Gan, D. The Combined Associations of Depression and Cognitive Impairment with Functional Disability and Mortality in Older Adults: A Population-Based Study from the NHANES 2011–2014. Front. Aging Neurosci. 2023, 15, 1121190. [Google Scholar] [CrossRef]
- Mehta, R.S.; Kochar, B.D.; Kennelty, K.; Ernst, M.E.; Chan, A.T. Emerging Approaches to Polypharmacy among Older Adults. Nat. Aging 2021, 1, 347–356. [Google Scholar] [CrossRef]
- Gutiérrez-Valencia, M.; Izquierdo, M.; Cesari, M.; Casas-Herrero, Á.; Inzitari, M.; Martínez-Velilla, N. The Relationship between Frailty and Polypharmacy in Older People: A Systematic Review. Br. J. Clin. Pharmacol. 2018, 84, 1432–1444. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN Guideline on Clinical Nutrition in the Intensive Care Unit. Clin. Nutr. 2018, 38, 48–79. [Google Scholar] [CrossRef]
- Kiss, N.; Steer, B.; de van der Schueren, M.; Loeliger, J.; Alizadehsani, R.; Edbrooke, L.; Deftereos, I.; Laing, E.; Khosravi, A. Comparison of the Prevalence of 21 GLIM Phenotypic and Etiologic Criteria Combinations and Association with 30-Day Outcomes in People with Cancer: A Retrospective Observational Study. Clin. Nutr. 2022, 41, 1102–1111. [Google Scholar] [CrossRef]
- Clark, A.B.; Reijnierse, E.M.; Lim, W.K.; Maier, A.B. Prevalence of Malnutrition Comparing the GLIM Criteria, ESPEN Definition and MST Malnutrition Risk in Geriatric Rehabilitation Patients: RESORT. Clin. Nutr. 2020, 39, 3504–3511. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, C.; Li, Y.; Zhang, Y.; Zou, C.; Yang, H.; Lu, W.; Zhang, X.; Liang, T. Prevalence and Prognostic Implications of Malnutrition According to GLIM Criteria in Hospitalized Heart Failure Patients: Reduced Muscle Mass and Inflammation as Predominant Criteria Identified in a Prospective Cohort Study. Nutr. Clin. Pract. 2025. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Sánchez, I.; Carnicero-Carreño, J.A.; Álvarez-Bustos, A.; García-García, F.J.; Rodríguez-Mañas, L.; Coelho-Júnior, H.J. Effects of Malnutrition on the Incidence and Worsening of Frailty in Community-Dwelling Older Adults with Pain. Nutrients 2025, 17, 1400. [Google Scholar] [CrossRef] [PubMed]
- Kaegi-Braun, N.; Boesiger, F.; Tribolet, P.; Gomes, F.; Kutz, A.; Hoess, C.; Pavlicek, V.; Bilz, S.; Sigrist, S.; Brändle, M.; et al. Validation of Modified GLIM Criteria to Predict Adverse Clinical Outcome and Response to Nutritional Treatment: A Secondary Analysis of a Randomized Clinical Trial. Clin. Nutr. 2022, 41, 795–804. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD/n (%) |
|---|---|
| Demographics | |
| Age at Screening (years) | 74.4 ± 6.3 |
| Gender (male) | 529 (50.9%) |
| Anthropometrics and Body Composition | |
| Body Mass Index (kg/m2) | 27.6 ± 5.3 |
| Maximal Calf Circumference (cm) | 36.8 ± 3.9 |
| ALM DEXA (kg) | 19.5 ± 5.2 |
| Physical Performance | |
| 8-foot Walking Speed (m/s) | 0.9 ± 0.3 |
| Clinical and Functional Measures | |
| Multimorbidity (≥2 diseases) | 464 (51.7%) |
| Albumin (urine, mg/L) | 3.7 ± 1.8 |
| Protein intake (g/kg/day) | 0.89 ± 0.43 |
| Caloric intake (kcal/day) | 1693.6 ± 689.9 |
| Frailty (%) | 122 (11.6) |
| Frailty criteria (%) | |
| Fatigue | 115 (11.0) |
| Resistance | 37 (3.5) |
| Ambulation | 280 (26.7) |
| Illness | 70 (6.7) |
| Loss of Weight | 70 (6.7) |
| Disability (%) | 122 (11.6) |
| DEXA-Based ASM | p-Value | |
|---|---|---|
| Calf circumference | 0.592 | 0.001 |
| Calf circumference-based ASM | 0.598 | 0.001 |
| Unadjusted | Adjusted * | |||||
|---|---|---|---|---|---|---|
| Variable | OR | p-Value | 95% CI (Lower, Upper) | OR | p-Value | 95% CI (Lower, Upper) |
| Disability | ||||||
| CC-based Malnutrition | 1.638 | 0.206 | 0.763, 3.518 | 1.680 | 0.197 | 0.764, 3.969 |
| DEXA-based Malnutrition | 1.417 | 0.380 | 0.651, 3.087 | 1.711 | 0.194 | 0.760, 3.848 |
| Frailty | ||||||
| CC-based Malnutrition | 2.908 | 0.001 | 1.832, 4.615 | 1.563 | 0.001 | 1.240, 1.970 |
| DEXA-based Malnutrition | 3.141 | 0.001 | 1.976, 4.994 | 1.699 | 0.001 | 1.306, 2.133 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marzetti, E.; Coelho-Júnior, H.J. Reevaluating Calf Circumference as an Indicator of Muscle Mass in Malnutrition Among Community-Dwelling Older Adults: A Cross-Sectional Analysis. Geriatrics 2025, 10, 162. https://doi.org/10.3390/geriatrics10060162
Marzetti E, Coelho-Júnior HJ. Reevaluating Calf Circumference as an Indicator of Muscle Mass in Malnutrition Among Community-Dwelling Older Adults: A Cross-Sectional Analysis. Geriatrics. 2025; 10(6):162. https://doi.org/10.3390/geriatrics10060162
Chicago/Turabian StyleMarzetti, Emanuele, and Hélio José Coelho-Júnior. 2025. "Reevaluating Calf Circumference as an Indicator of Muscle Mass in Malnutrition Among Community-Dwelling Older Adults: A Cross-Sectional Analysis" Geriatrics 10, no. 6: 162. https://doi.org/10.3390/geriatrics10060162
APA StyleMarzetti, E., & Coelho-Júnior, H. J. (2025). Reevaluating Calf Circumference as an Indicator of Muscle Mass in Malnutrition Among Community-Dwelling Older Adults: A Cross-Sectional Analysis. Geriatrics, 10(6), 162. https://doi.org/10.3390/geriatrics10060162







