Impact of Mattress Use on Sacral Interface Pressure in Community-Dwelling Older Adults
Abstract
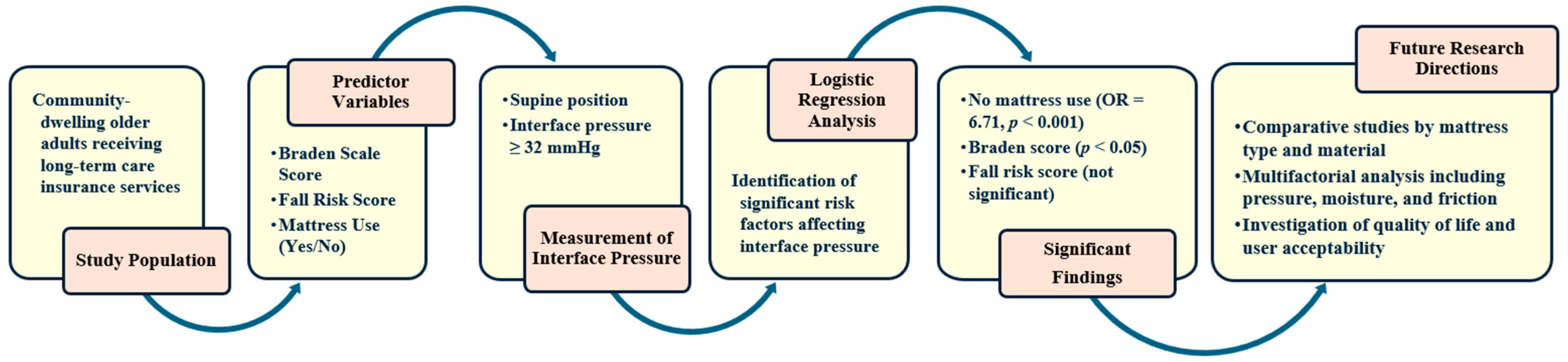
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection and Measurement Instruments
2.4. Sacral Interface Pressure Measurement
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
3.1. General Characteristics of the Participants
3.2. Differences in Sacral Interface Pressure According to General Characteristics
3.3. Factors Influencing Sacral Interface Pressure
4. Discussion
4.1. Summary of Main Findings
4.2. Interpretation in the Context of Prior Research
4.3. Methodological Considerations
4.4. Practical and Technological Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects; United Nations: New York, NY, USA, 2024. [Google Scholar]
- Statistics Korea. Data on the Proportion of the Elderly [Internet]; Statistics Korea: Daejeon, Republic of Korea, 2021.
- National Health Insurance Service. Long Term Care Insurance Statistical Yearbook; National Health Insurance Service: Wonju, Republic of Korea, 2021. [Google Scholar]
- Gould, L.; Stuntz, M.; Giovannelli, M.; Ahmad, A.; Aslam, R.; Mullen-Fortino, M.; Whitney, J.D.; Calhoun, J.; Kirsner, R.S.; Gordillo, G.M. Wound Healing Society 2015 update on guidelines for pressure ulcers. Wound Repair Regen. 2016, 24, 145–162. [Google Scholar] [CrossRef] [PubMed]
- Eom, J.Y.; Jung, D.Y. Systematic review for the pressure ulcer preventive interventions. J. Korean Gerontol. Nurs. 2013, 33, 21–37. [Google Scholar]
- National Pressure Ulcer Advisory Panel. NPUAP Announces a Change in Terminology From Pressure Ulcer to Pressure Injury and Updates the Stages of Pressure Injury; National Pressure Ulcer Advisory Panel: Washington, DC, USA, 2016. [Google Scholar]
- Moon, I.; Kang, S.J.; Kim, G.S.; Mun, M.S. Control of air-cell mattress for preventing pressure ulcer based on approximate anthropometric model. In Proceedings of the 9th International Conference on Rehabilitation Robotics, Chicago, IL, USA, 28 June–1 July 2005; IEEE: Piscataway, NJ, USA, 2005; pp. 164–167. [Google Scholar]
- Baumgarten, M.; Margolis, D.J.; Localio, A.R.; Kagan, S.H.; Lowe, R.A.; Kinosian, B.; Abbuhl, S.B.; Kavesh, W.; Holmes, J.H.; Ruffin, A.; et al. Extrinsic risk factors for pressure ulcers early in the hospital stay: A nested case-control study. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 408–413. [Google Scholar] [CrossRef]
- Kawabata, T.; Sugama, J. Relationship between mattress internal air pressure and interface pressure distribution in the lateral position. Int. Wound J. 2022, 19, 2115–2123. [Google Scholar] [CrossRef]
- Primiano, M.; Friend, M.; McClure, C.; Nardi, S.; Fix, L.; Schafer, M.; Savochka, K.; McNett, M. Pressure ulcer prevalence and risk factors during prolonged surgical procedures. AORN J. 2011, 94, 555–566. [Google Scholar] [CrossRef]
- Capon, A.; Pavoni, N.; Mastromattei, A.; Di Lallo, D. Pressure ulcer risk in long-term units: Prevalence and associated factors. J. Adv. Nurs. 2007, 58, 263–272. [Google Scholar] [CrossRef]
- Finnie, A. Interface pressure measurements in leg ulcer management. Br. J. Nurs. 2000, 9 (Suppl. 1), S8–S18. [Google Scholar] [CrossRef]
- Matsuo, J.; Sugama, J.; Sanada, H.; Okuwa, M.; Nakatani, T.; Konya, C.; Sakamoto, J. Development and validity of a new model for assessing pressure redistribution properties of support surfaces. J. Tissue Viability 2011, 20, 55–66. [Google Scholar] [CrossRef]
- Kim, K.; Kang, S. Intelligent Pressure Ulcer Prevention Mattress for Interventional Nursing in an Aged Society. J. Inst. Electron. Eng. Korea 2017, 44, 32–37. [Google Scholar]
- Ministry of Health and Welfare. Plan for Improving the Welfare Equipment System; Ministry of Health and Welfare: Sejong, Republic of Korea, 2024.
- Kim, Y. A Study on the Long-Term Care Insurance Welfare Equipment Rental System: Focus Group Interview with Service Users and Providers. Health Soc. Welf. Rev. 2017, 37, 230–259. [Google Scholar]
- McInnes, E.; Jammali-Blasi, A.; Bell-Syer, S.; Dumville, J.C.; Middleton, V.; Cullum, N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst. Rev. 2015, 2015, CD001735. [Google Scholar] [CrossRef]
- Moon, Y. Empirical Analysis of Use Support for Long-Term Care Management Establishment. J. Korea Acad.-Ind. Coop. Soc. 2022, 23, 348–357. [Google Scholar]
- Walia, G.S.; Wong, A.L.; Lo, A.Y.; Zhou, A.Y.; Ko, J.N.; Huang, R.; Lee, G.K.; Hara, H.; Wong, M.S. Effectiveness of pressure-redistributing support surfaces in preventing pressure ulcers: A systematic review. J. Tissue Viability 2020, 29, 220–228. [Google Scholar]
- Tao, L.; Tang, C.; Chen, J.; Jiang, Y. Comparison of the predictive validity of the Braden and Waterlow scales in preventing pressure injuries among surgical patients: A meta-analysis. J. Clin. Nurs. 2023, 32, 892–903. [Google Scholar] [CrossRef]
- Shang, Y.; Wang, F.; Cai, Y.; Zhu, Q.; Li, X.; Wang, R.; Tung, T.-H. The accuracy of the risk assessment scale for pressure ulcers in adult surgical patients: A network meta-analysis. BMC Surg. 2025, 25, 104. [Google Scholar] [CrossRef]
- Yu, M.; Park, K.H.; Shin, J.; Lee, J.H. Predicting the cut-off point for interface pressure in pressure injury according to the standard hospital mattress and polyurethane foam mattress as support surfaces. Int. Wound J. 2022, 19, 1509–1517. [Google Scholar] [CrossRef]
- Ho, C.; Ocampo, W.; Southern, D.A.; Sola, D.; Baylis, B.; Conly, J.M.; Hogan, D.B.; Kaufman, J.; Stelfox, H.T.; Ghali, W.A. Effect of a continuous bedside pressure mapping system for reducing interface pressures: A randomized clinical trial. JAMA Netw. Open 2023, 6, e2316480. [Google Scholar] [CrossRef]
- Sari, S.P.; Everink, I.H.; Lohrmann, C.; Amir, Y.; Sari, E.A.; Halfens, R.J.; Schols, J.M. Knowledge, Attitude and Practice of Family Caregivers on Pressure Injury Prevention for Community-Dwelling Older Adults: A Cross-Sectional Study in an Indonesia City. BMC Nurs. 2025, 24, 24. [Google Scholar] [CrossRef]
- Zhang, Y.; Zou, X.; Zhang, B.; Han, Y.; Wang, S.; Liu, T.; Zhang, X. A flexible turning and sensing system for pressure ulcers prevention. Electronics 2021, 10, 2971. [Google Scholar] [CrossRef]
- Lee, K.H.; Kwon, Y.-E.; Lee, H.; Lee, Y.; Seo, J.; Kwon, O.; Kang, S.-W.; Lee, D. Active body pressure relief system with time-of-flight optical pressure sensors for pressure ulcer prevention. Sensors 2019, 19, 3862. [Google Scholar] [CrossRef]
- Blackburn, J.; Britton, S.; Pearson, A. Pressure Redistribution Support Surfaces in the Community Setting: An American Perspective. World Union. Wound Heal. Soc. J. 2020, 20, 12–18. [Google Scholar]
- National Pressure Injury Advisory Panel; European Pressure Ulcer Advisory Panel; Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. 2019. Available online: https://internationalguideline.com/ (accessed on 1 May 2025).

| Variables | Categories | n | % | Mean ± SD | |
|---|---|---|---|---|---|
| Gender | Male | 137 | 65.2 | ||
| Female | 73 | 34.8 | |||
| Age | ≤70 | 14 | 6.8 | 82.30 ± 7.56 | |
| 71–80 | 69 | 33.5 | |||
| ≥81 | 123 | 59.7 | |||
| Bedridden status | Fully | 50 | 23.8 | ||
| Partially | 51 | 24.3 | |||
| Not bedridden | 109 | 51.9 | |||
| BMI (kg/m2) | <18.5 | 34 | 16.4 | 21.59 ± 3.48 | |
| 18.5–25.5 | 150 | 72.5 | |||
| ≥25.5 | 23 | 11.1 | |||
| Defecation | No diaper | 156 | 74.3 | ||
| With diaper | 54 | 25.7 | |||
| Urination | No diaper | 160 | 76.2 | ||
| With diaper | 50 | 23.8 | |||
| Urinary catheter | None | 172 | 81.9 | ||
| Present | 38 | 18.1 | |||
| Nutritional status | Good | 128 | 62.1 | ||
| Poor | 71 | 34.5 | |||
| Very poor | 7 | 3.4 | |||
| Hemoglobin (Hb,g/dL) | ≥10 | 10 | 4.8 | 12.32 ± 1.61 | |
| <10 | 198 | 95.2 | |||
| SpO2 (%) | ≥97 | 90 | 60.4 | 96.43 ± 2.48 | |
| <97 | 59 | 39.6 | |||
| Pressure injury | No | 159 | 75.7 | ||
| Yes | Stage 1 | 23 | 11 | ||
| Stage 2 | 18 | 8.6 | |||
| Stage 3 | 7 | 3.3 | |||
| Stage 4 | 2 | 1 | |||
| Unstageable | 1 | 0.5 | |||
| Huhn Scale score for fall risk | Low (≤4) | 61 | 29 | 11.98 ± 8.66 | |
| Moderate (5–10) | 14 | 6.7 | |||
| High (≥11) | 135 | 64.3 | |||
| Braden Scale score | Normal (≥18) | 98 | 46.7 | 16.55 ± 4.81 | |
| Moderate risk (10–17) | 92 | 43.8 | |||
| High risk (≤9) | 20 | 9.5 | |||
| Mattress use | No | 73 | 34.8 | ||
| Yes | 137 | 65.2 | |||
| Variables | Categories | Interface Pressure n (%) | χ2/t/Z | p | ||
|---|---|---|---|---|---|---|
| <32 mmHg | ≥32 mmHg | |||||
| Gender | Male | 37 (27.0) | 100 (73.0) | 0.65 | 0.419 | |
| Female | 16 (21.9) | 57 (78.1) | ||||
| Age | ≤70 | 2 (14.3) | 12 (85.7) | 0.96 | 0.620 | |
| 71–80 | 18 (26.1) | 51 (73.9) | ||||
| ≥81 | 32 (26.0) | 91 (74.0) | ||||
| Bedridden status | Fully | 15 (30.0) | 35 (70.0) | 4.78 | 0.092 | |
| Partially | 7 (13.7) | 44 (86.3) | ||||
| Not bedridden | 31 (28.4) | 78 (71.6) | ||||
| BMI | <18.5 | 10 (29.4) | 24 (70.6) | 0.49 | 0.783 | |
| 18.5–25.5 | 37 (24.7) | 113 (75.3) | ||||
| ≥25.5 | 5 (21.7) | 18 (78.3) | ||||
| Defecation | No diaper | 41 (26.3) | 115 (73.7) | 0.35 | 0.554 | |
| With diaper | 12 (22.2) | 42 (77.8) | ||||
| Urination | No diaper | 42 (26.3) | 118 (73.8) | 0.37 | 0.546 | |
| With diaper | 11 (22.0) | 39 (78.0) | ||||
| Indwelling catheter | No | 44 (25.6) | 128 (74.4) | 0.06 | 0.807 | |
| Yes | 9 (23.7) | 29 (76.3) | ||||
| Nutritional status | Good | 39 (30.5) | 89 (69.5) | 4.92 | 0.086 | |
| Poor | 12 (16.9) | 59 (83.1) | ||||
| Severely poor | 1 (14.3) | 6 (85.7) | ||||
| Hemoglobin (Hb,g/dL) | ≥10 g/dL | 5 (50.0) | 5 (50.0) | 3.50 | 0.061 | |
| <10 g/dL | 47 (23.7) | 151 (76.3) | ||||
| SpO2 (%) | ≥97% | 21 (23.3) | 69 (76.7) | 1.45 | 0.229 | |
| <97% | 9 (15.3) | 50 (84.7) | ||||
| Pressure injury | No | 40 (25.2) | 119 (74.8) | 4.27 | 0.511 | |
| Yes | Stage 1 | 5 (21.7) | 18 (78.3) | |||
| Stage 2 | 5 (27.8) | 13 (72.2) | ||||
| Stage 3 | 1 (14.3) | 6 (85.7) | ||||
| Stage 4 | 1 (50.0) | 1 (50.0) | ||||
| Unstageable | 1 (100.0) | 0 (0.0) | ||||
| Fall risk score | Low (≤4) | 24 (39.3) | 37 (60.7) | 9.29 | 0.010 | |
| Moderate (5–10) | 2 (14.3) | 12 (85.7) | ||||
| High (≥11) | 27 (20.0) | 108 (80.0) | ||||
| Huhn Scale score for fall risk | Normal (≥18) | 32 (32.7) | 66 (67.3) | 11.18 | 0.004 | |
| Moderate risk (10–17) | 13 (14.1) | 79 (85.9) | ||||
| High risk (≤9) | 8 (40.0) | 12 (60.0) | ||||
| Mattress use | No | 9 (13.4) | 58 (86.6) | 8.17 | 0.004 | |
| Yes | 44 (32.1) | 93 (67.9) | ||||
| Variable | Categories | B | SE | p | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Fall risk score | Low risk (≤4 points, reference) | ||||||
| Moderate risk (5–10 points) | 1.15 | 0.87 | 0.184 | 3.16 | 0.58 | 17.27 | |
| High risk (≥11 points) | 0.47 | 0.54 | 0.381 | 1.6 | 0.56 | 4.57 | |
| Braden Scale score | Normal (≥18, reference) | ||||||
| Moderate risk (10–17) | 1.57 | 0.57 | 0.006 | 4.8 | 1.57 | 14.7 | |
| High risk (≤9) | 0.27 | 0.67 | 0.692 | 1.31 | 0.35 | 4.9 | |
| Mattress use | Yes (reference) | ||||||
| No | 1.9 | 0.46 | <0.001 | 6.71 | 2.7 | 16.67 | |
| Nagelkerke R2 = 0.23; Cox and Snell R2 = 0.16; χ2/p-value = 35.70/<0.001 | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.Y.; Jang, I.S.; Hong, J.E.; Kim, J.H.; Park, S. Impact of Mattress Use on Sacral Interface Pressure in Community-Dwelling Older Adults. Geriatrics 2025, 10, 107. https://doi.org/10.3390/geriatrics10040107
Lee HY, Jang IS, Hong JE, Kim JH, Park S. Impact of Mattress Use on Sacral Interface Pressure in Community-Dwelling Older Adults. Geriatrics. 2025; 10(4):107. https://doi.org/10.3390/geriatrics10040107
Chicago/Turabian StyleLee, Hye Young, In Sun Jang, Jung Eun Hong, Je Hyun Kim, and Seungmi Park. 2025. "Impact of Mattress Use on Sacral Interface Pressure in Community-Dwelling Older Adults" Geriatrics 10, no. 4: 107. https://doi.org/10.3390/geriatrics10040107
APA StyleLee, H. Y., Jang, I. S., Hong, J. E., Kim, J. H., & Park, S. (2025). Impact of Mattress Use on Sacral Interface Pressure in Community-Dwelling Older Adults. Geriatrics, 10(4), 107. https://doi.org/10.3390/geriatrics10040107





