Short- and Long-Term Effects on Physical Fitness in Older Adults: Results from an 8-Week Exercise Program Repeated in Two Consecutive Years
Abstract
1. Introduction
2. Materials and Methods
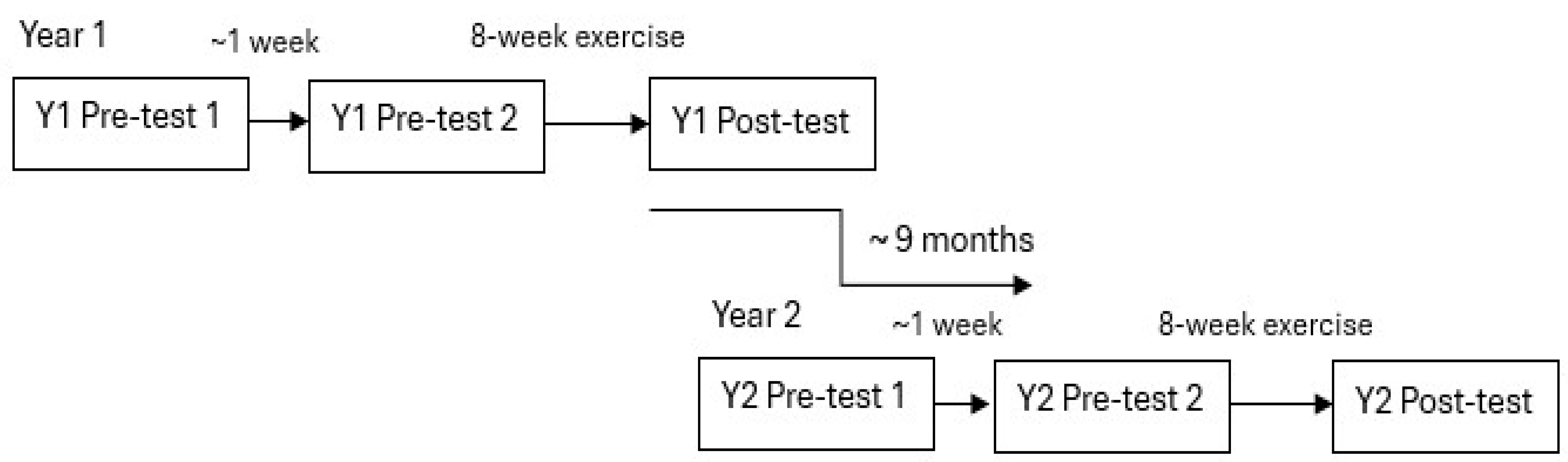
2.1. Study Design
2.2. Participants
2.3. Exercise Period
2.4. Test Procedures
2.4.1. Muscular Endurance Tests
- Isometric trunk flexion at 45° was assessed in seconds and performed for as long as possible while seated on the floor, with the trunk held statically backward at 45° (arms crossed over the chest, knees bent 90°) with the ankles supported by the test leader. A wooden 45° frame was positioned just behind the participant as a reference angle [21].
- Isometric trunk extension (Sorensen’s test, assessed in seconds) was performed prone for as long as possible while holding the trunk horizontally (crossed arms on the chest) and the lower body on a bench (iliac crest at the bench edge, with the test leader supporting the ankles). Timing started, in these two endurance tests, when the correct trunk position was reached and was stopped at exhaustion [22].
- 30 s sit-to-stand (n out of 50): The participants went from sitting to standing 50 times as fast as possible, being instructed to only touch the chair seat if possible. Otherwise, a complete sit-down was performed between each rise (46 cm chair height). Time and speed/frequency (number of sit-to-stands/second) were noted. In case 50 sit-to-stands were not completed, the number of completed sit-to-stands was used to calculate the speed. Furthermore, all completed sit-to-stands during the first 30 s were noted in the test (for 30 s sit-to-stand, see also [23]). The number of sit-to-stands (n of 50) where the chair seat was briefly bounced on was also noted [21].
- Shoulder press: Hand weights (5 kg for men and 3 kg for women) were alternately pressed from shoulder height to straight arm (cadence 1/s) until exhaustion. When the participant could not perform another press or keep cadence rhythm, the test was stopped. The number of shoulder presses was noted [21].
2.4.2. Muscular Strength Tests
- 5.
- Five sit-to-stands: Time in seconds was measured while performing five sit-to-stands as fast as possible and sitting down fully on the 46-cm high chair between each raise, with start and stop in a seated position [23].
- 6.
- Maximal step height test (MST): On either leg, a standardized MST was performed in 3-cm increments on a specially designed step-up box until the highest height was reached. Correct body posture was required, without support from hands or the other leg [24].
- 7.
- Grip strength: A hand-grip dynamometer (Sagitta, Sagitta Pedagog AB, Mariestad, Sweden) was squeezed as hard as possible for 4–5 s while standing, with arms and hands hanging. Three measurements were performed on each hand alternately with a short rest between trials. The highest grip strength from the three trials was noted (Nm) [25].
2.4.3. Cardiorespiratory Fitness Tests
- 8.
- Six-minute walk test (6MWT): Participants walked as fast as possible around a horizontal/flat course (in ~50 m-laps) indoors for 6 min, after which the distance was noted [23].
- 9.
- Submaximal cycling test: Participants cycled with a cadence of 60 rpm (revolutions per minute) during two 4-min periods (according to the Ekblom-Bak cycling protocol [26]), first at a standardized work rate of 32 watts and second at an individually determined rate of work (yielding a perceived-exertion rate (RPE) of ~14, based on sex and training background). Generally, men had higher workloads, although, to enable comparisons between tests, the same individual workload was used on all three test occasions. Mean HR was calculated for the last minute (with time marks of 3.15, 3.30, 3.45, and 4.0 min) at both work rates. HR was measured with a Polar 400 (Electro Oy, Kempele, Finland) as heartbeats per minute (bpm).
2.4.4. Motor Fitness Tests
- 10.
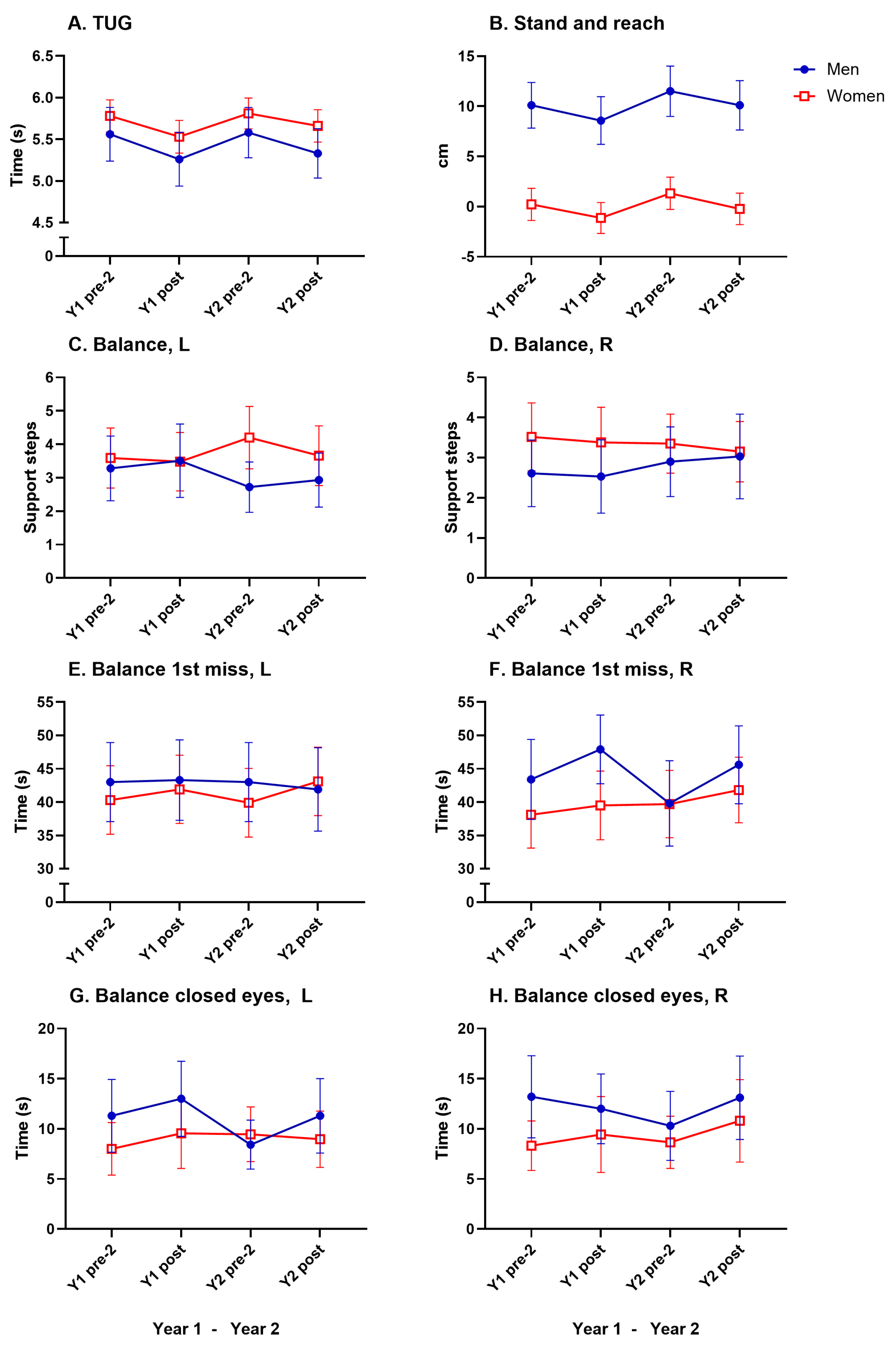
- Timed up-and-go (TUG): From a sitting position (46-cm chair height), participants walked as fast as they found comfortable 3 m around a floor mark and returned to sitting [23].
- 11.
- Stand-and-reach: Participants, standing with straight legs on a step, reached down toward their toes. The distance from their fingertips to their feet was recorded as ± cm, above/below feet [21].
- 12.
- One-leg balance test: With open eyes, on either leg, a balance test was conducted for 60 s. The amount of support needed with the non-balancing foot or arm (n/60 s) and the time to first use support (1st miss) was noted. One-leg balance tests with closed eyes were timed until the first support was needed (s) [21].
2.5. Survey Questions
2.6. Statistics
3. Results
3.1. Participants
3.2. Intervention Results
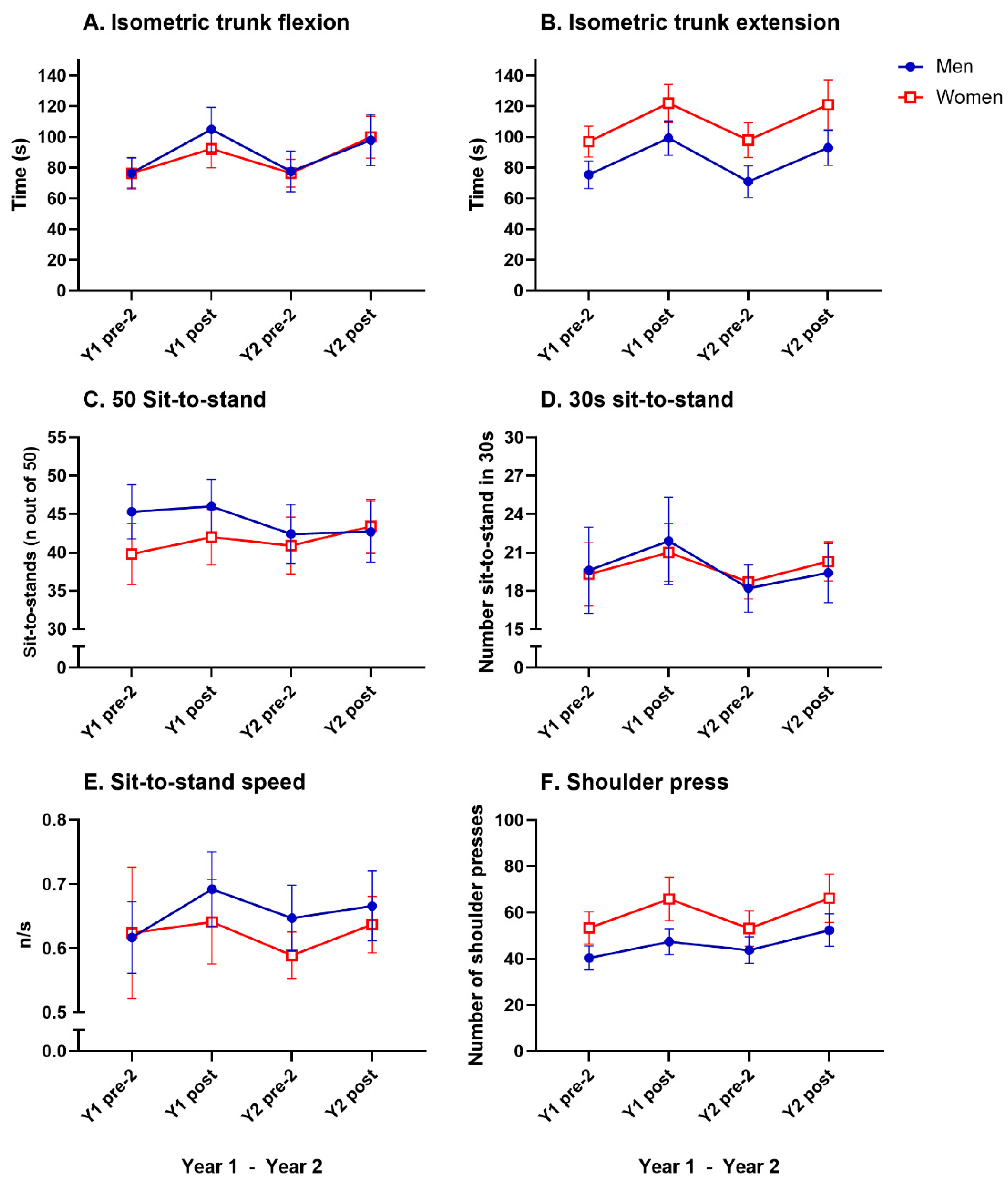
3.3. Muscular Endurance
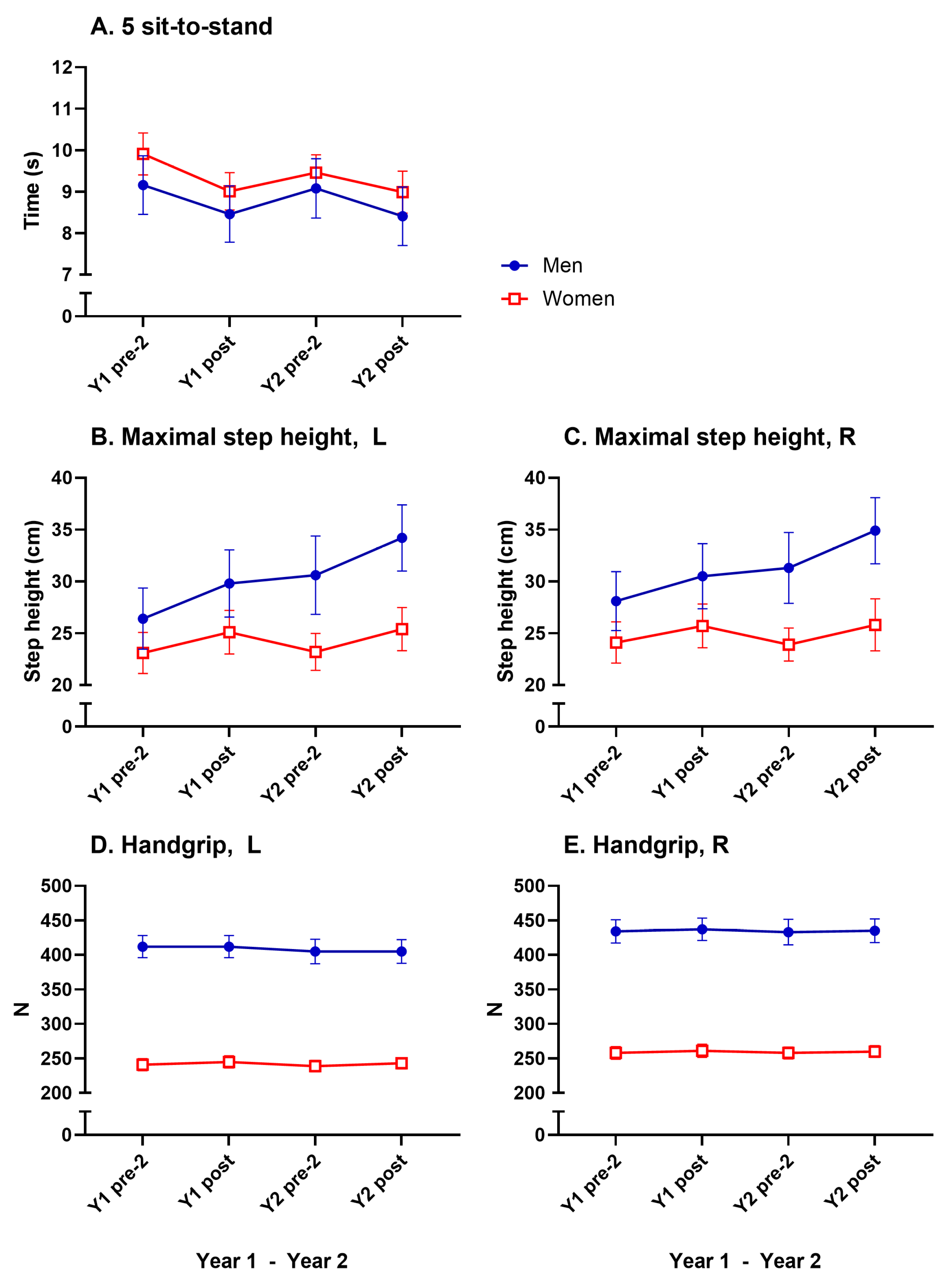
3.4. Muscular Strength
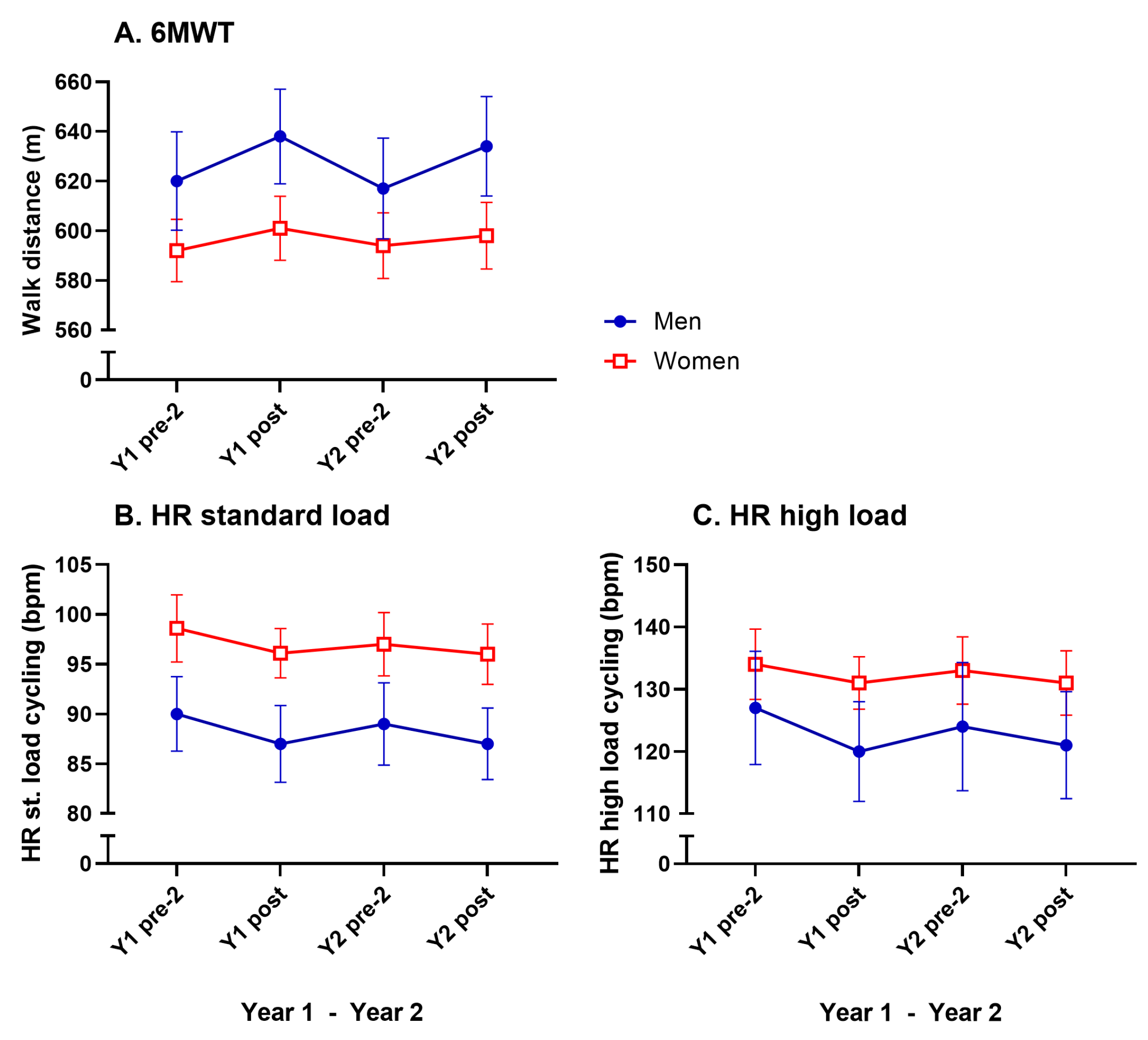
3.5. Cardiorespiratory Fitness
3.6. Motor Fitness
3.7. Survey Question About Exercise Habits
4. Discussion
4.1. Intervention Results
4.1.1. Muscular Endurance and Strength
4.1.2. Cardiorespiratory Fitness
4.1.3. Motor Fitness
4.1.4. Sex Differences
4.1.5. Long-Term Maintenance of Benefits
4.2. Physical Activity and Physical Fitness Levels in the Participants
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ageing and Health. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 18 July 2024).
- Chodzko-Zajko, W.J.; Proctor, D.N.; Singh, M.A.F.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA 2014, 311, 2387–2396. [Google Scholar] [CrossRef]
- Hagberg, L.A.; Lindholm, L. Cost-effectiveness of healthcare-based interventions aimed at improving physical activity. Scand. J. Public Health 2006, 34, 641–653. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Cavero-Redondo, I.; Ramírez-Vélez, R.; Ruiz, J.R.; Ortega, F.B.; Lee, D.C.; Martínez-Vizcaíno, V. Muscular strength as a predictor of all-cause mortality in an apparently healthy population: A systematic review and meta-analysis of data from approximately 2 million men and women. Arch. Phys. Med. Rehabil. 2018, 99, 2100–2113.e5. [Google Scholar] [CrossRef] [PubMed]
- Molari, M.; Fernandes, K.B.P.; de Souza Marquez, A.; Probst, V.S.; Bignardi, P.R.; de Castro Teixeira, D. Impact of physical and functional fitness on mortality from all causes of physically independent older adults. Arch. Gerontol. Geriatr. 2021, 97, 104524. [Google Scholar] [CrossRef]
- da Costa Pereira, J.P.; Freire, Y.A.; da Silva, A.M.B.; de Lucena Alves, C.P.; de Melo Silva, R.; Câmara, M.; Browne, R.A.V.; Costa, E.C.; Fayh, A.P.T. Associations of upper-and lower-limb muscle strength, mass, and quality with health-related quality of life in community-dwelling older adults. Geriatr. Gerontol. Int. 2024, 24, 683–692. [Google Scholar] [CrossRef] [PubMed]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance training for older adults: Position statement from the national strength and conditioning association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef] [PubMed]
- Falck, R.S.; Davis, J.C.; Best, J.R.; Crockett, R.A.; Liu-Ambrose, T. Impact of exercise training on physical and cognitive function among older adults: A systematic review and meta-analysis. Neurobiol. Aging 2019, 79, 119–130. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094. [Google Scholar] [CrossRef]
- Liguori, G.; American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Hurst, C.; Weston, K.L.; McLaren, S.J.; Weston, M. The effects of same-session combined exercise training on cardiorespiratory and functional fitness in older adults: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2019, 31, 1701–1717. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Cadore, E.L.; Casas-Herrero, A.; Zambom-Ferraresi, F.; Idoate, F.; Millor, N.; Gómez, M.; Rodriguez-Mañas, L.; Izquierdo, M. Multicomponent exercises including muscle power training enhance muscle mass, power output, and functional outcomes in institutionalized frail nonagenarians. Age 2014, 36, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Flores-Bello, C.; Correa-Muñoz, E.; Sánchez-Rodríguez, M.A.; Mendoza-Núñez, V.M. Effect of Exercise Programs on Physical Performance in Community-Dwelling Older Adults with and without Frailty: Systematic Review and Meta-Analysis. Geriatrics 2024, 9, 8. [Google Scholar] [CrossRef]
- Opdenacker, J.; Boen, F.; Coorevits, N.; Delecluse, C. Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Prev. Med. 2008, 46, 518–524. [Google Scholar] [CrossRef]
- Gudlaugsson, J.; Gudnason, V.; Aspelund, T.; Siggeirsdottir, K.; Olafsdottir, A.S.; Jonsson, P.V.; Arngrimsson, S.A.; Harris, T.B.; Johannsson, E. Effects of a 6-month multimodal training intervention on retention of functional fitness in older adults: A randomized-controlled cross-over design. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 107. [Google Scholar] [CrossRef] [PubMed]
- Fielding, R.A.; Rejeski, W.J.; Blair, S.; Church, T.; Espeland, M.A.; Gill, T.M.; Guralnik, J.M.; Hsu, F.-C.; Katula, J.; King, A.C.; et al. The lifestyle interventions and independence for elders study: Design and methods. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 1226–1237. [Google Scholar] [CrossRef]
- Bauman, A.; Merom, D.; Bull, F.C.; Buchner, D.M.; Fiatarone Singh, M.A. Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. Gerontologist 2016, 56, S268–S280. [Google Scholar] [CrossRef] [PubMed]
- Langhammer, B.; Bergland, A.; Rydwik, E. The importance of physical activity exercise among older people. Biomed. Res. Int. 2018, 2018, 7856823. [Google Scholar] [CrossRef] [PubMed]
- Godhe, M.; Rönquist, G.; Nilsson, J.; Ekblom, Ö.; Nyberg, L.; Edman, G.; Andersson, E. Reliability in Novel Field-Based Fitness Measurements and Postexercise Scores from a Physical Fitness Test Battery in Older Adults. Gerontology 2024, 70, 639–660. [Google Scholar] [CrossRef]
- Biering-Sørensen, F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine 1984, 9, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, C.J. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Nyberg, L.A.; Hellénius, M.L.; Kowalski, J.; Wändell, P.; Andersson, P.; Sundberg, C.J. Repeatability and validity of a standardised maximal step-up test for leg function-a diagnostic accuracy study. BMC Musculoskelet. BMC Musculoskelet. Disord. 2011, 12, 191. [Google Scholar] [CrossRef] [PubMed]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Kuh, D.; Cooper, C.; Sayer, A.A. Global variation in grip strength: A systematic review and meta-analysis of normative data. Age Ageing 2016, 45, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Björkman, F.; Ekblom-Bak, E.; Ekblom, Ö.; Ekblom, B. Validity of the revised Ekblom Bak cycle ergometer test in adults. Eur. J. Appl. Physiol. 2016, 116, 1627–1638. [Google Scholar] [CrossRef]
- Granacher, U.; Lacroix, A.; Muehlbauer, T.; Roettger, K.; Gollhofer, A. Effects of core instability strength training on trunk muscle strength, spinal mobility, dynamic balance and functional mobility in older adults. Gerontology 2013, 59, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Granacher, U.; Gollhofer, A.; Hortobágyi, T.; Kressig, R.W.; Muehlbauer, T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: A systematic review. Sports Med. 2013, 43, 627–641. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, A.K.; Griebler, E.M.; da Silva, W.A.; Sant, D.P.; da Silva, P.C.; Possamai, V.D.; Martins, V.F. Does a multicomponent exercise program improve physical fitness in older adults? Findings from a 5-year longitudinal study. J. Aging Phys. Act. 2021, 29, 814–821. [Google Scholar] [CrossRef]
- Andersson, E.A.; Lundahl, G.; Wecke, L.; Lindblom, I.; Nilsson, J. Maximal aerobic power versus performance in two aerobic endurance tests among young and old adults. Gerontology 2011, 57, 502–512. [Google Scholar] [CrossRef]
- Chase, J.A.D.; Phillips, L.J.; Brown, M. Physical activity intervention effects on physical function among community-dwelling older adults: A systematic review and meta-analysis. J. Aging Phys. Act. 2017, 25, 149–170. [Google Scholar] [CrossRef] [PubMed]
- Leitão, L.; Campos, Y.; Louro, H.; Figueira, A.C.C.; Figueiredo, T.; Pereira, A.; Conceição, A.; Marinho, D.A.; Neiva, H.P. Detraining and Retraining Effects from a Multicomponent Training Program on the Functional Capacity and Health Profile of Physically Active Prehypertensive Older Women. Healthcare 2024, 12, 271. [Google Scholar] [CrossRef]
- Timmons, J.F.; Griffin, C.; Cogan, K.E.; Matthews, J.; Egan, B. Exercise maintenance in older adults 1 year after completion of a supervised training intervention. J. Am. Geriatr. Soc. 2020, 68, 163–169. [Google Scholar] [CrossRef]
- Fernández Rodríguez, R.; Martínez Vizcaíno, V.; Reina Gutiérrez, S.; Bizzozero Peroni, B.; Torres Costoso, A.; Rodríguez Gutiérrez, E.; Díaz-Goñi, V.; Cadenas-Sánchez, C. Sex Differences in Effects of Exercise on Physical Function in Aging: A Systematic Review with Meta-Analysis. World J. Men’s Health 2024, 42, 694. [Google Scholar] [CrossRef]
- Eggenberger, P.; Schumacher, V.; Angst, M.; Theill, N.; de Bruin, E.D. Does multicomponent physical exercise with simultaneous cognitive training boost cognitive performance in older adults? A 6-month randomized controlled trial with a 1-year follow-up. Clin. Interv. Aging 2015, 10, 1335–1349. [Google Scholar]
- Fisher, K.L.; Reeder, B.A.; Harrison, E.L.; Bruner, B.G.; Ashworth, N.L.; Pahwa, P.; Sari, N.; Sheppard, M.S.; Shields, C.A.; Chad, K.E. Comparing class-based and home-based exercise for older adults with chronic health conditions: 12-month follow-up of a randomized clinical trial. J. Aging Phys. Act. 2018, 26, 471–485. [Google Scholar] [CrossRef]
- Huang, L.Y.; Lim, A.Y.; Hsu, C.C.; Tsai, Y.F.; Fu, T.C.; Shyu, Y.C.; Peng, S.-C.; Wang, J.-S. Sustainability of exercise-induced benefits on circulating MicroRNAs and physical fitness in community-dwelling older adults: A randomized controlled trial with follow up. BMC Geriatr. 2024, 24, 473. [Google Scholar] [CrossRef]
- Stanghelle, B.; Bentzen, H.; Giangregorio, L.; Pripp, A.H.; Skelton, D.A.; Bergland, A. Physical fitness in older women with osteoporosis and vertebral fracture after a resistance and balance exercise programme: 3-month post-intervention follow-up of a randomised controlled trial. BMC Musculoskelet. BMC Musculoskelet. Disord. 2020, 21, 471. [Google Scholar] [CrossRef]
- Gomez-Bruton, A.; Navarrete-Villanueva, D.; Pérez-Gómez, J.; Vila-Maldonado, S.; Gesteiro, E.; Gusi, N.; Villa-Vicente, J.G.; Espino, L.; Gonzalez-Gross, M.; Casajus, J.A.; et al. The effects of age, organized physical activity and sedentarism on fitness in older adults: An 8-year longitudinal study. Int. J. Environ. Res. Public Health 2020, 17, 4312. [Google Scholar] [CrossRef] [PubMed]
- Gylling, A.T.; Bloch-Ibenfeldt, M.; Eriksen, C.S.; Ziegler, A.K.; Wimmelmann, C.L.; Baekgaard, M.; Boraxbekk, C.-J.; Siebner, H.R.; Mortensen, E.L.; Kjaer, M. Maintenance of muscle strength following a one-year resistance training program in older adults. Exp. Gerontol. 2020, 139, 111049. [Google Scholar] [CrossRef] [PubMed]
- Godhe, M.; Pontén, M.; Nilsson, J.; Kallings, L.V.; Andersson, E.A. Reliability of the accelerometer to control the effects of physical activity in older adults. PLoS ONE 2022, 17, e0274442. [Google Scholar] [CrossRef]
- Oh, S.J.; Lee, S.H. Comparing durability of water-and land-based exercise benefits among older adults in South Korea: A randomized controlled trial with 1-year follow-up. J. Back Musculoskelet. Rehabil. 2021, 34, 745–755. [Google Scholar] [CrossRef]

| Year 1 | Year 2 | |||
|---|---|---|---|---|
| Sex | Men (n = 102) | Women (n = 163) | Men (n = 102) | Women (n = 163) |
| Age (yrs) | 71.6 ± 4.64 | 71.3 ± 4.80 | 72.6 ± 4.64 | 72.3 ± 4.80 |
| Height (m) | 1.78 ± 0.07 | 1.64 ± 0.05 | 1.78 ± 0.07 | 1.64 ± 0.06 |
| Weight (kg) | 82.1 ± 11.5 | 67.1 ± 9.7 | 81.6 ± 11.2 | 66.9 ± 9.9 |
| BMI (kg/m2) | 26.0 ± 3.2 | 25.0 ± 3.5 | 25.9 ± 3.1 | 25.0 ± 3.5 |
| Waist circumf. (cm) | 96.8 ± 13.1 | 86.6 ± 10.9 | 97.5 ± 9.4 | 85.4 ± 11.2 |
| Bodyfat (%) | 24.6 ± 6.6 | 34.6 ± 6.1 | 24.0 ± 7.1 | 34.3 ± 6.2 |
| Physical Fitness Test | Sex | n | Y1 Pre-Test 2 | Y1 Post-Test | Y1 Post-Test–Y1 Pre-Test 2 (%) | sign. | Partial Eta Squared (ES) Y1 Post-Test–Y1 Pre-Test 2 | Y2 Pre-Test 2 | Y2 Post-Test | Y2 Post-Test –Y2 Pre-Test 2 (%) | Sign. | Partial Eta Squared (ES) Y2 Post-Test–Y2 Pre-Test 2 | Y2 Pre-Test 2–Y1 Post-Test (%) | Sign. | Partial Eta Squared (ES) Y 2 Pre-Test 2– Y1 Post-Test |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Isometric trunk flexion | Men | 94 | 76.7 ± 47.5 | 105 ± 70.6 | 28.3 (36.9%) | <0.001 | 0.270 | 77.7 ± 64.6 | 98.1 ± 81.4 | 20.4 (26.3%) | 0.007 | 0.159 | −27.3 (−26.0%) | 0.002 | 0.160 |
| Women | 143 | 76.4 ± 62.6 | 92.4 ± 74.3 | 16.0 (20.9%) | 0.002 | 0.118 | 76.6 ± 54.3 | 100 ± 82.8 | 23.4 (30.5%) | <0.001 | 0.168 | −15.8 (−17.1%) | 0.122 | 0.059 | |
| Isometric trunk extension | Men | 84 | 75.5 ± 41.1 | 99.3 ± 50.5 | 23.8 (31.5%) | <0.001 | 0.300 | 71.0 ± 47.1 | 93.0 ± 52.2 | 22.0 (31.0%) | 0.002 | 0.330 | −28.3 (−28.5%) | <0.001 | 0.300 |
| Women | 128 | 97.1 ± 58.0 | 122 ± 71.6 | 24.9 (25.6%) | <0.001 | 0.361 | 98.1 ± 65.6 | 121 ± 93.2 | 22.9 (23.3%) | <0.001 | 0.142 | −23.9 (−19.6%) | <0.001 | 0.176 | |
| Sit to stand out of 50 | Men | 49 | 45.3 ± 12.4 | 46.0 ± 12.3 | 0.7 (1.5%) | 1.000 | 0.024 | 42.4 ± 14.8 | 42.7 ± 15.4 | 0.3 (0.7%) | 1.000 | 0.000 | −3.6 (−7.8%) | 1.000 | 0.036 |
| Women | 66 | 39.8 ± 16.3 | 42.0 ± 14.7 | 2.2 (5.5%) | 1.000 | 0.097 | 40.9 ± 16.3 | 43.4 ± 15.4 | 2.5 (6.1%) | 1.000 | 0.117 | −1.1 (−2.6%) | 1.000 | 0.005 | |
| 30 s sit-to-stand | Men | 26 | 19.6 ± 8.7 | 21.9 ± 8.6 | 2.3 (11.7%) | 0.007 | 0.348 | 18.2 ± 4.8 | 19.4 ± 6.0 | 1.2 (6.6%) | 0.678 | 0.197 | −3.7 (−16.9%) | 0.568 | 0.206 |
| Women | 44 | 19.3 ± 8.2 | 21.0 ± 7.8 | 1.7 (8.8%) | 0.007 | 0.342 | 18.7 ± 4.6 | 20.3 ± 5.2 | 1.6 (8.6%) | 1.000 | 0.283 | −2.3 (−0.11) | 1.000 | 0.113 | |
| Sit-to-stand speed | Men | 53 | 0.62 ± 0.20 | 0.69 ± 0.21 | 0.08 (12.2%) | 0.167 | 0.319 | 0.65 ± 0.19 | 0.67 ± 0.20 | 0.02 (2.9%) | 0.967 | 0.047 | −0.05 (−6.5%) | 0.957 | 0.108 |
| Women | 79 | 0.62 ± 0.46 | 0.64 ± 0.29 | 0.02 (2.7%) | 1.000 | 0.006 | 0.59 ± 0.16 | 0.64 ± 0.20 | 0.05 (8.1%) | 0.002 | 0.161 | −0.05 (−8.1%) | 0.667 | 0.035 | |
| Shoulder Press | Men | 87 | 40.4 ± 24.0 | 47.4 ± 26.2 | 7.0 (17.3%) | 0.088 | 0.279 | 43.7 ± 26.9 | 52.4 ± 33.1 | 8.7 (19.9%) | 0.038 | 0.259 | −3.7 (−7.8%) | 1.000 | 0.018 |
| Women | 134 | 53.4 ± 40.9 | 65.9 ± 54.8 | 12.5 (23.4%) | <0.001 | 0.200 | 53.1 ± 45.0 | 66.2 ± 61.6 | 13.1 (24.7%) | 0.001 | 0.177 | −12.8 (−19.4%) | 0.029 | 0.062 | |
| Five sit-to-stands | Men | 75 | 9.2 ± 3.1 | 8.5 ± 3.0 | −0.7 (−7.6%) | 0.010 | 0.203 | 9.1 ± 3.1 | 8.4 ± 3.0 | −0.7 (−7.4%) | 0.083 | 0.124 | 0.6 (7.3%) | 0.500 | 0.054 |
| Women | 114 | 9.9 ± 2.7 | 9.0 ± 2.4 | −0.9 (−9.1%) | <0.001 | 0.214 | 9.5 ± 2.3 | 9.0 ± 2.73 | −0.5 ( −5.2%) | 1.000 | 0.063 | 0.5 (0.05) | 0.850 | 0.029 | |
| Step height L | Men | 24 | 26.4 ± 7.0 | 29.8 ± 7.7 | 3.4 (12.9%) | <0.001 | 0.478 | 30.6 ± 8.96 | 34.2 ± 7.56 | 3.6 (11.8%) | 0.003 | 0.399 | 0.8 (2.7%) | 1.000 | 0.006 |
| Women | 37 | 23.1 ± 5.9 | 25.1 ± 6.3 | 2.0 (8.7%) | 0.040 | 0.277 | 23.2 ± 5.35 | 25.4 ± 6.26 | 2.2 (9.5%) | 0.048 | 0.282 | −1.9 (−7.6%) | 0.970 | 0.058 | |
| Step height R | Men | 24 | 28.1 ± 6.7 | 30.5 ± 7.5 | 2.4 (8.5%) | 0.043 | 0.317 | 31.3 ± 8.10 | 34.9 ± 7.56 | 3.6 (11.5%) | 0.015 | 0.520 | 0.8 (2.6%) | 1.000 | 0.007 |
| Women | 37 | 24.1 ± 6.0 | 25.7 ± 6.3 | 1.6 (6.6%) | 0.124 | 0.217 | 23.9 ± 4.77 | 25.8 ± 7.54 | 1.9 (7.9%) | 0.370 | 0.120 | −1.8 (−0.07) | 0.971 | 0.062 | |
| Handgrip L | Men | 92 | 412 ± 77.6 | 412 ± 77.4 | 0.0 (0.0%) | 1.000 | 0.000 | 405 ± 86.0 | 405 ± 82.5 | 0.0 (0.0%) | 1.000 | 0.000 | −7.0 (−1.7%) | 1.000 | 0.023 |
| Women | 146 | 241 ± 54.1 | 245 ± 54.5 | 4.0 (1.7%) | 1.000 | 0.020 | 239 ± 50.5 | 243 ± 49.7 | 4.0 (1.7%) | 1.000 | 0.029 | −6.0 (−2.4%) | 1.000 | 0.029 | |
| Handgrip R | Men | 92 | 434 ± 81.3 | 437 ± 78.5 | 3.0 (0.7%) | 1.000 | 0.004 | 433 ± 89.0 | 435 ± 82.5 | 2.0 (0.5%) | 1.000 | 0.005 | −4.0 (−0.9%) | 1.000 | 0.006 |
| Women | 148 | 258 ± 56.2 | 261 ± 58.6 | 3.0 (1.2%) | 0.998 | 0.007 | 258 ± 52.3 | 260 ± 52.2 | 2.0 (0.8%) | 1.000 | 0.006 | −3.0 (−1.1%) | 1.000 | 0.004 | |
| 6MWT | Men | 94 | 620 ± 96 | 638 ± 93 | 18 (2.9%) | <0.001 | 0.170 | 617 ± 99 | 634 ± 98 | 17 (2.8%) | <0.001 | 0.174 | −21.0 (−3.3%) | 0.002 | 0.126 |
| Women | 127 | 592 ± 77 | 601 ± 79 | 9 (1.5%) | 0.047 | 0.072 | 594 ± 81 | 598 ± 83 | 4 (0.7%) | 0.966 | 0.013 | −7.0 (−1.2%) | 0.731 | 0.031 | |
| HR st.load | Men | 46 | 90.7 ± 12.6 | 87.7 ± 13.0 | −3.0 (−3.3%) | 0.413 | 0.189 | 89.8 ± 13.9 | 87.8 ± 12.1 | −2.0 (−2.2%) | 0.929 | 0.051 | 2.1 (2.4%) | 0.976 | 0.034 |
| Women | 72 | 98.6 ± 14.3 | 96.1 ± 10.6 | −2.5 (−2.5%) | 0.399 | 0.060 | 97.0 ± 13.7 | 96.0 ± 13.1 | −1.0 (−1.0%) | 0.929 | 0.011 | 0.9 (0.9%) | 1.000 | 0.011 | |
| HR High load | Men | 10 | 127 ± 12.7 | 120 ± 11.2 | −7.0 (−5.5%) | 0.546 | 0.338 | 124 ± 14.4 | 121 ± 12.0 | −3.0 (−2.4%) | 0.952 | 0.270 | 4 (3.3%) | 0.996 | 0.152 |
| Women | 27 | 134 ± 15.3 | 131 ± 12.6 | −3.0 (−2.2%) | 0.702 | 0.134 | 133 ± 18.2 | 131 ± 17.4 | −2.0 (−1.5%) | 0.966 | 0.058 | 2 (1.5%) | 0.996 | 0.034 | |
| TUG | Men | 74 | 5.6 ± 1.4 | 5.3 ± 1.4 | −0.3 (−5.4%) | 0.049 | 0.125 | 5.6 ± 1.3 | 5.3 ± 1.3 | −0.3 (−4.5%) | 0.032 | 0.137 | 0.3 (6.1%) | 0.262 | 0.074 |
| Women | 118 | 5.8 ± 1.1 | 5.5 ± 1.1 | −0.3 (−4.3%) | 0.028 | 0.107 | 5.8 ± 1.0 | 5.7 ± 1.1 | −0.1 (−2.6%) | 0.006 | 0.048 | 0.3 (5.1%) | 0.101 | 0.110 | |
| Stand and reach | Men | 96 | 10.1 ± 11.3 | 8.6 ± 11.7 | −1.5 ( − ) | 0.043 | 0.085 | 11.5 ± 12.4 | 10.1 ± 12.1 | −1.4 ( − ) | 0.004 | 0.083 | 2.9 ( − ) | 0.065 | 0.185 |
| Women | 157 | 0.2 ± 10.1 | −1.1 ± 9.8 | −1.3 ( − ) | 0.030 | 0.093 | 1.3 ± 10.2 | −0.1 ± 10.0 | −1.4 ( − ) | <0.001 | 0.183 | 2.4 ( − ) | 0.023 | 0.063 | |
| Balance L | Men | 68 | 3.3 ± 4.0 | 3.5 ± 4.5 | 0.2 (7.0%) | 1.000 | 0.005 | 2.7 ± 3.6 | 2.9 ± 3.8 | 0.2 (7.7%) | 1.000 | 0.008 | −0.8 (−22.5%) | 1.000 | 0.017 |
| Women | 113 | 3.6 ± 4.8 | 3.5 ± 4.7 | −0.1 (−3.1%) | 1.000 | 0.003 | 4.2 ± 5.5 | 3.7 ± 5.3 | −0.5(−12.9%) | 0.610 | 0.059 | 0.7 (20.7%) | 1.000 | 0.075 | |
| Balance R | Men | 59 | 2.6 ± 3.2 | 2.5 ± 3.5 | −0.1 (−3.1%) | 1.000 | 0.001 | 2.9 ± 3.6 | 3.0 ± 4.34 | 0.1 (4.5%) | 1.000 | 0.004 | 0.4 (14.6%) | 1.000 | 0.005 |
| Women | 102 | 3.5 ± 4.3 | 3.4 ± 4.5 | −0.1 (−4.0%) | 1.000 | 0.004 | 3.4 ± 3.9 | 3.2 ± 4.1 | −0.2 (−6.0%) | 1.000 | 0.010 | 0 (−0.9%) | 1.000 | 0.017 | |
| Balance 1Miss L | Men | 54 | 43.0 ± 21.7 | 43.3 ± 22.1 | 0.3 (0.7%) | 1.000 | 0.000 | 43.0 ± 21.7 | 41.9 ± 22.9 | −1.1 (−2.6%) | 1.000 | 0.004 | −0.3 (−0.7%) | 1.000 | 0.000 |
| Women | 78 | 40.3 ± 22.8 | 41.9 ± 22.7 | 1.6 (4.0%) | 1.000 | 0.001 | 39.9 ± 23.0 | 43.1 ± 22.9 | 3.2 (8.0%) | 1.000 | 0.045 | −2.0 (−4.8%) | 1.000 | 0.011 | |
| Balance 1Miss R | Men | 54 | 43.4 ± 22.0 | 47.9 ± 18.9 | 4.5 (10.4%) | 1.000 | 0.060 | 39.8 ± 23.5 | 45.6 ± 21.4 | 5.8 (14.6%) | 1.000 | 0.108 | −8.1 (−16.9%) | 1.000 | 0.168 |
| Women | 79 | 38.1 ± 22.4 | 39.5 ± 23.0 | 1.4 (3.7%) | 1.000 | 0.004 | 39.7 ± 22.6 | 41.8 ± 22.1 | 2.1 (5.3%) | 1.000 | 0.017 | 0.2 (0.5%) | 1.000 | 0.000 | |
| Balance closed Eyes L | Men | 54 | 11.3 ± 13.3 | 13.0 ± 13.7 | 1.7 (15.0%) | 1.000 | 0.024 | 8.4 ± 8.9 | 11.3 ± 13.6 | 2.9 (34.0%) | 1.000 | 0.087 | −4.6 (−35.2%) | 1.000 | 0.143 |
| Women | 82 | 8.01 ± 11.9 | 9.55 ± 15.9 | 1.5 (19.2%) | 1.000 | 0.033 | 9.5 ± 12.4 | 9.0 ± 12.8 | −0.5 (−5.2%) | 1.000 | 0.002 | −0.1 (−0.9%) | 1.000 | 0.000 | |
| Balance closed Eyes R | Men | 56 | 13.2 ± 15.4 | 12.0 ± 13.1 | −1.2 (−9.1%) | 1.000 | 0.013 | 10.3 ± 13.0 | 13.1 ± 15.5 | 2.8 (27.2%) | 1.000 | 0.070 | −1.7 (−14.2%) | 1.000 | 0.021 |
| Women | 83 | 8.32 ± 11.3 | 9.44 ± 17.3 | 1.1 (13.5%) | 1.000 | 0.002 | 8.7 ± 11.9 | 10.8 ± 18.8 | 2.1 (24.7%) | 1.000 | 0.020 | −0.7 (−8.3%) | 1.000 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Godhe, M.; Nilsson, J.; Andersson, E.A. Short- and Long-Term Effects on Physical Fitness in Older Adults: Results from an 8-Week Exercise Program Repeated in Two Consecutive Years. Geriatrics 2025, 10, 15. https://doi.org/10.3390/geriatrics10010015
Godhe M, Nilsson J, Andersson EA. Short- and Long-Term Effects on Physical Fitness in Older Adults: Results from an 8-Week Exercise Program Repeated in Two Consecutive Years. Geriatrics. 2025; 10(1):15. https://doi.org/10.3390/geriatrics10010015
Chicago/Turabian StyleGodhe, Manne, Johnny Nilsson, and Eva A. Andersson. 2025. "Short- and Long-Term Effects on Physical Fitness in Older Adults: Results from an 8-Week Exercise Program Repeated in Two Consecutive Years" Geriatrics 10, no. 1: 15. https://doi.org/10.3390/geriatrics10010015
APA StyleGodhe, M., Nilsson, J., & Andersson, E. A. (2025). Short- and Long-Term Effects on Physical Fitness in Older Adults: Results from an 8-Week Exercise Program Repeated in Two Consecutive Years. Geriatrics, 10(1), 15. https://doi.org/10.3390/geriatrics10010015






