Evidence Based Review of Fitness-to-Drive and Return-to-Driving Following Traumatic Brain Injury
Abstract
:1. Introduction
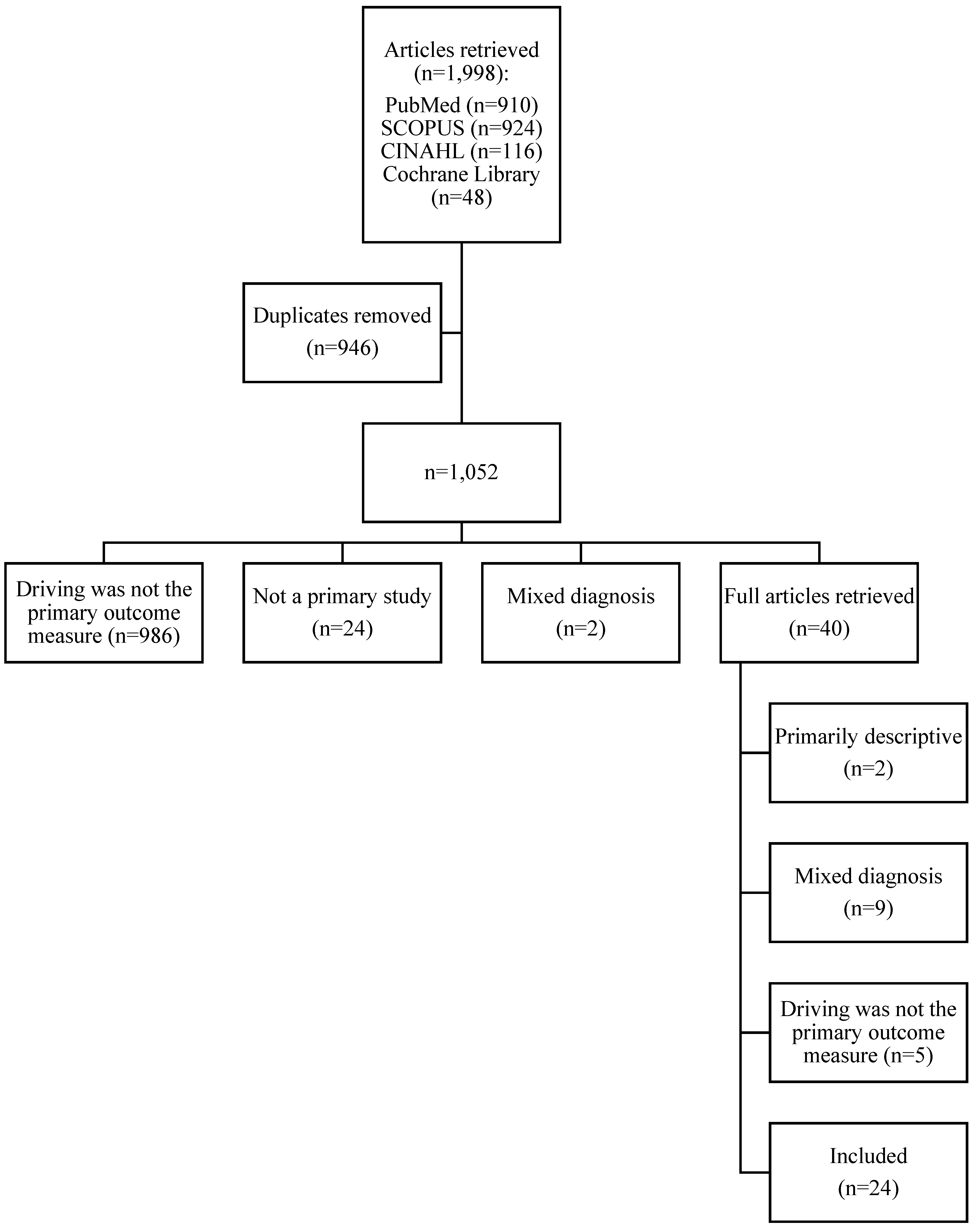
2. Methods
2.1. Procedure
2.2. Evidence-Based Ratings and Recommendations
3. Results
3.1. Description of Primary Studies
3.2. Level of Evidence, Conclusions, and Recommendations
3.2.1. On-Road Studies
3.2.2. Simulator Studies
3.2.3. Off-Road Screening Tests
3.2.4. Surveys/Self-Report
3.2.5. Return to Driving (Driving Status)
3.2.6. Driving Behaviours
3.2.7. Driving Records
4. Discussion
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Canadian Institute of Health Research. Research in Traumatic Brain Injury. 2012. Available online: http://www.cihr-irsc.gc.ca/e/45665.html (accessed on 14 January 2016).
- Faul, M.; Xu, L.; Wald, M.M.; Coronado, V.G. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006; Centers for Disease Control and Prevention, National Center for Injury Prevention and Control: Atlanta, GA, USA, 2010. [Google Scholar]
- Schneiders, A.G.; Sullivan, S.J.; Gray, A.R.; Hammond-Tooke, G.D.; McCrory, P.R. Normative values for three clinical measures of motor performance used in the neurological assessment of sports concussion. J. Sci. Med. Sport 2010, 13, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Swaine, B.R.; Sullivan, S.J. Reliability of the scores for the finger-to-nose test in adults with traumatic brain injury. Phys. Ther. 1993, 73, 71–78. [Google Scholar] [PubMed]
- Guskiewicz, K.M.; Marshall, S.W.; Bailes, J.; McCrea, M.; Harding, H.P., Jr.; Matthews, A.; Mihalik, J.R.; Cantu, R.C. Recurrent concussion and risk of depression in retired professional football players. Med. Sci. Sports Exerc. 2007, 39, 903–909. [Google Scholar] [CrossRef] [PubMed]
- Belanger, H.G.; Curtiss, G.; Demery, J.A.; Lebowitz, B.K.; Vanderploeg, R.D. Factors moderating neuropsychological outcomes following mild traumatic brain injury: A meta-analysis. J. Int. Neuropsychol. Soc. 2005, 11, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Preece, M.H.W.; Horswill, M.S.; Geffen, G.M. Driving after concussion: The acute effect of mild traumatic brain injury on drivers hazard perception. Neuropsychology 2010, 24, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Stokx, L.C.; Gaillard, A.W.K. Task and driving performance of patients with a severe concussion of the brain. J. Clin. Exp. Neuropsychol. 1986, 8, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Ilie, G.; Mann, R.E.; Ialomiteanu, A.; Adlaf, E.M.; Hamilton, H.; Wickens, C.M.; Ashbridge, M.; Rehm, J.; Cusimano, M.D. Traumatic brain injury, driver aggression and motor vehicle collisions in Canadian adults. Accid. Anal. Prev. 2015, 81, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Rike, P.; Johansen, H.J.; Ulleberg, P.; Lundqvist, A.; Schanke, A. Exploring associations between self-reported executive functions, impulsive personality traits, driving self-efficacy, and functional abilities in driver behaviour after injury. Tranp. Res. F Traffic Psychol. Behav. 2015, 29, 34–47. [Google Scholar] [CrossRef]
- Ross, P.E.; Ponsford, J.L.; di Stefano, M.; Spitz, G. Predictors of on-road driver performance following traumatic brain injury. Arch. Phys. Med. Rehabil. 2015, 96, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.; Unsworth, C.A.; Lannin, N.A. Fitness to drive after mild traumatic brain injury: Mapping the time trajectory of recovery in the acute stages post injury. Accid. Anal. Prev. 2015, 79, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Fleming, J.; Liddle, J.; Nalder, E.; Weir, N.; Cornwell, P. Return to driving in the first 6 months of community integration after acquired brain injury. NeuroRehabilitation 2014, 34, 157–166. [Google Scholar] [PubMed]
- Aslaksen, P.M.; Orbo, M.; Elvestad, R.; Schafer, C.; Anke, A. Prediction of on-road driving ability after traumatic brain injury and stroke. Eur. J. Neurol. 2013, 20, 1227–1233. [Google Scholar] [CrossRef] [PubMed]
- Hargrave, D.D.; Nupp, J.M.; Erickson, R.J. Two brief measures of executive function in the prediction of driving ability after acquired brain injury. Neuropsychol. Rehabil. 2012, 22, 489–500. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Hillary, F.; Chute, D.L. The neurocognitive driving test: Applying technology to the assessment of driving ability following brain injury. Rehabil. Psychol. 2003, 48, 275–280. [Google Scholar] [CrossRef]
- Classen, S.; Levy, C.; McCarthy, D.; Mann, W.C.; Lanford, D.; Waid-Ebbs, J.K. Traumatic brain injury and driving assessment: An evidence-based literature review. Am. J. Occup. Ther. 2009, 63, 580–591. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.; Unsworth, C.A.; Lannin, N.A. Determining fitness to drive: A systematic review of the methods and assessments used after mild traumatic brain injury. Br. J. Occup. Ther. 2015, 78, 73–84. [Google Scholar] [CrossRef]
- Edlund, W.; Gronseth, G.; So, Y.; Franklin, G. Clinical Practice Guideline Process Manual; American Academy of Neurology: St. Paul, MN, USA, 2004. [Google Scholar]
- Beaulieu-Bonneau, S.; Fortier-Brochu, E.; Ivers, H.; Morin, C.M. Attention following traumatic brain injury: Neuropsychological and driver simulator data, and association with sleep, sleepiness, and fatigue. Neuropsychol. Rehabil. 2015, 24, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Korteling, J.E.; Kaptein, N.A. Neuropsychological driving fitness tests for brain-damaged subjects. Arch. Phys. Med. Rehabil. 1996, 77, 138–146. [Google Scholar] [CrossRef]
- Lew, H.L.; Poole, J.H.; Jaffe, D.L.; Huang, H.C.; Brodd, E. Predictive validity of driving-simulator assessments following traumatic brain injury: A preliminary study. Brain Inj. 2005, 19, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Neyens, D.M.; Boyle, L.N.; Schultheis, M.T. The effects of driver distraction for individuals with traumatic brain injuries. Hum. Factors 2015, 57, 1472–1488. [Google Scholar] [CrossRef] [PubMed]
- Novack, T.A.; Banos, J.H.; Alderson, A.L.; Schneider, J.J.; Weed, W.; Blankenship, J.; Salisbury, D. UFOV performance and driving ability following traumatic brain injury. Brain Inj. 2006, 20, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Preece, M.H.W.; Horswill, M.S.; Geffen, G.M. Assessment of drivers’ ability to anticipate traffic hazards after traumatic brain injury. J. Neurol. Neurosurg. Psychiatr. 2011, 82, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Ross, P.; Ponsford, J.L.; Stefano, M.D.; Charlton, J.; Spitz, G. On the road again after traumatic brain injury: Driver safety and behaviour following on-road assessment and rehabilitation. Disabil. Rehabil. 2016, 38, 994–1005. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.J.; Gouvier, W.D. Utility of the UFOV test with mild traumatic brain injury. Appl. Neuropsychol. 2005, 12, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, M.T.; Mathis, R.J.; Nead, R.; DeLuca, J. Driving behaviors following brain injury: Self-report and motor vehicle records. J. Head Trauma Rehabil. 2002, 17, 38–47. [Google Scholar] [CrossRef] [PubMed]
- McKay, A.; Liew, C.; Schonberger, M.; Ross, P.; Ponsford, J. Predictors of the on-road driving assessment after traumatic brain injury: Comparing cognitive tests, injury factors, and demographics. J. Head Trauma Rehabil. 2015. [CrossRef] [PubMed]
- Gamache, P.L.; Lavailliere, M.; Tremblay, M.; Simoneau, M.; Teasdale, N. In-simulator training of driving abilities in a person with a traumatic brain injury. Brain Inj. 2011, 25, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Leon-Carrion, J.; Dominguez-Morales, M.R.; Martin, J.M. Driving with cognitive deficits: Neurorehabilitation and legal measures are needed for driving again after severe traumatic brain injury. Brain Inj. 2005, 19, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Novack, T.A.; Labbe, D.; Grote, M.; Carlson, N.; Sherer, M.; Arango-Lasprilla, J.C.; Bushnik, T.; Cifu, D.; Powell, J.M.; Ripley, D.; et al. Return to driving within five years of moderate-severe traumatic brain injury. Brain Inj. 2010, 24, 464–471. [Google Scholar] [CrossRef]
- Rapport, L.J.; Hanks, R.A.; Bryer, R.C. Barriers to driving and community integration after traumatic brain injury. J. Head Trauma Rehabil. 2006, 21, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Cullen, N.; Krakowski, A.; Taggart, C. Early neuropsychological tests as correlates of return to driving after traumatic brain injury. Brain Inj. 2014, 28, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Coleman, R.D.; Rapport, L.J.; Ergh, T.C.; Hanks, R.A.; Ricker, J.H.; Millis, S.R. Predictors of driving outcome after traumatic brain injury. Arch. Phys. Med. Rehabil. 2002, 83, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Hawley, C. Return to driving after head injury. J. Neurol. Neurosurg. Psychiatr. 2001, 70, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Labbe, D.R.; Vance, D.E.; Wadley, V.; Novack, T.A. Predictors of driving avoidance and exposure following traumatic brain injury. J. Head Trauma Rehabil. 2014, 29, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Pietrapiana, P.; Tamietto, M.; Torrini, G.; Mezzanato, T.; Rago, R.; Perino, C. Role of premorbid factors in predicting safe return to driving after severe TBI. Brain Inj. 2005, 19, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Casutt, G.; Martin, M.; Keller, M.; Jancke, L. The relation between performance in on-road driving, cognitive screening and driving simulator in older healthy drivers. Transp. Res. F Traffic Psychol. Behav. 2014, 22, 232–244. [Google Scholar] [CrossRef]
- Shechtman, O.; Classen, S.; Stephens, B.; Bendixen, R.; Belchior, P.; Sandhu, M.; McCarthy, D.; Mann, W.; Davis, E. The impact of intersection design on simulated driving performance of young and senior adults. Traffic Inj. Prev. 2007, 8, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Roy, M.; Molnar, F. Systematic review of the evidence for Trails B cut-off scores in assessing fitness to drive. Can. Geriatr. J. 2013, 16, 120–142. [Google Scholar] [CrossRef] [PubMed]
- Classen, S.; Wang, Y.; Crizzle, A.M.; Winter, S.M.; Lanford, D.N. Predicting older driver on-road performance by means of the useful field of view and trail making test part B. Am. J. Occup. Ther. 2013, 67, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.M.; Smith, G.A.; Cull, A.W.; Myers, A.M.; Bedard, M.; Gelinas, I.; Mazer, B.L.; Marshall, S.C.; Naglie, G.; Rapoport, M.J.; et al. Older driver estimates of driving exposure compared to in-vehicle data in the Candrive II study. Traffic Inj. Prev. 2015, 16, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Blanchard, R.A.; Myers, A.M.; Porter, M.M. Correspondence between self-reported and objective measures of driving exposure and patterns in older drivers. Accid. Anal. Prev. 2010, 42, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Crizzle, A.M.; Myers, A.M.; Almeida, Q.J. Self-regulatory practices of driving with Parkinson’s disease: Accuracy of patient reports. Parkinsonism Relat. D. 2013, 19, 176–180. [Google Scholar] [CrossRef] [PubMed]
| Class I | Class II | Class III | Class IV | |
|---|---|---|---|---|
| Rating article by class | Evidence provided by a prospective study in a broad spectrum of persons with the suspected condition, using a criterion standard for the case definition. Test should be applied in a blinded evaluation. All people undergoing the test have the presence or absence of the condition. | Evidence provided by a prospective study of a narrow spectrum of persons (n, 100) with the suspected condition, or a retrospective study of a broad spectrum of persons with an established condition by criterion standard, compared to a broad spectrum of controls. | Evidence provided by a retrospective study where either persons with the established condition or controls are of a narrow spectrum (n, 100). The reference standard, if not objective, is applied by someone other than the person performing the test. | Any design where the test is not applied in an independent evaluation or evidence provided by the expert opinion alone or in descriptive case series (without controls). |
| Level A | Level B | Level C | Level U | |
| Rating by recommendation | Recommendation: Established as effective/useful/or predictive or not. “Should be done, or should not be done.” | Recommendation: Probably effective/useful/or predictive, or not. “Should be considered, or should not be considered.” | Recommendation: Possibly effective/useful/or predictive, or not. “May be considered, or may not be considered.” | No recommendation. |
| Condition for rating by recommendation | Requires 2 consistent Class I studies, or 1 Class I study where the magnitude of the effect is large, and all criteria have been met. | Requires at least 1 Class I study, or 2 consistent Class II studies. | Requires at least 1 Class II study, or 2 consistent Class III studies. | Data inadequate or conflicting. Given the current knowledge or test, the treatment is unproven. |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palubiski, L.; Crizzle, A.M. Evidence Based Review of Fitness-to-Drive and Return-to-Driving Following Traumatic Brain Injury. Geriatrics 2016, 1, 17. https://doi.org/10.3390/geriatrics1030017
Palubiski L, Crizzle AM. Evidence Based Review of Fitness-to-Drive and Return-to-Driving Following Traumatic Brain Injury. Geriatrics. 2016; 1(3):17. https://doi.org/10.3390/geriatrics1030017
Chicago/Turabian StylePalubiski, Lisa, and Alexander M. Crizzle. 2016. "Evidence Based Review of Fitness-to-Drive and Return-to-Driving Following Traumatic Brain Injury" Geriatrics 1, no. 3: 17. https://doi.org/10.3390/geriatrics1030017
APA StylePalubiski, L., & Crizzle, A. M. (2016). Evidence Based Review of Fitness-to-Drive and Return-to-Driving Following Traumatic Brain Injury. Geriatrics, 1(3), 17. https://doi.org/10.3390/geriatrics1030017