Preliminary Validation of a Questionnaire Covering Risk Factors for Impaired Driving Skills in Elderly Patients
Abstract
:1. Introduction
1.1. Background
1.2. Legislation
1.3. How to Measure Driving Fitness?
1.4. Rationale of the Study
2. Methods
2.1. Participants
| N | 22 |
| sex (female/male) | 7/15 |
| age in years (SD) | 71.6 (8.3) |
| minimum | 56 |
| maximum | 88 |
| school education in years (SD) | 9.9 (1.9) |
| minimum | 8 |
| maximum | 13 |
| MMSE score (SD) | 27.3 (2.6) |
| minimum | 19 |
| maximum | 30 |
| Post-hoc diagnoses (n) | |
| no psychiatric diagnosis | 8 |
| AD dementia | 3 |
| Vascular dementia | 1 |
| MCI | 4 |
| Affective disorder | 6 |
2.2. Corporal A
2.3. Neuropsychological Data
2.4. Safety Advice For Elderly Drivers (SAFE)
2.5. Statistics
3. Results
3.1. Corporal A
| Unimpaired | Impaired | |
|---|---|---|
| N | 3 | 19 |
| age (SD) | 60.7 (4.7) | 73.4 (7.4) |
| sex (female/male) | 1/2 | 5/14 |
| school education in years (SD) | 10.7 (1.5) | 9.8 (1.9) |
| SAFE total risk (SD) | 0 | 1.8 (1.3) |
| Number of SAFE risk factors (SD) | 0 | 2.6 (1.3) |
| SAFE risk factor score (SD) | 0 | 4.8 (3.4) |
| MMSE score (SD) | 29.3 (0.6) | 26.9 (2.7) |
| TMT-B score (SD) | 74 (34) | 192.6 (121.6) |
| Post-hoc diagnoses | ||
| no psychiatric diagnosis | 2 | 6 |
| AD dementia | 0 | 3 |
| Vascular dementia | 0 | 1 |
| MCI | 0 | 4 |
| Affective disorder | 1 | 5 |
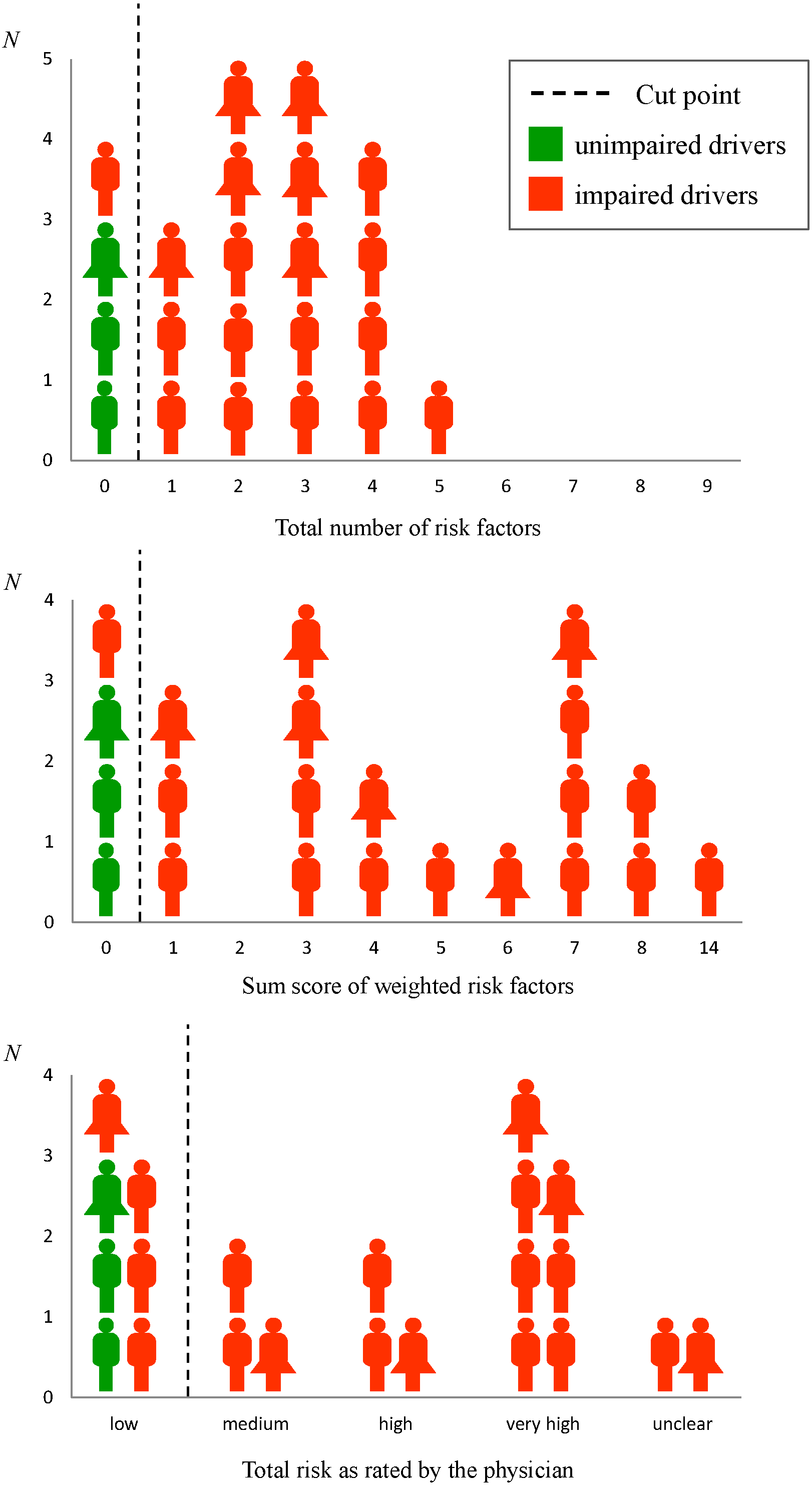
3.2. SAFE
| SAFE Subscores and Risk Factors | Descriptive Data | Correlations with Overall Corporal A Performance 1 | |||
|---|---|---|---|---|---|
| n | M | SD | Zero Order | Controlled for Age | |
| SAFE subscores | |||||
| Total risk 2 | 22 | 1.5 | 1.3 | −0.55 ** | −0.41 + |
| Number of risk factors | 22 | 2.2 | 1.5 | −0.49 ** | −0.39 + |
| Risk factor score | 22 | 4.2 | 3.6 | −0.43 ** | −0.33 |
| Frequency of SAFE risk factors | |||||
| TMT-B | 15 | ||||
| MMSE | 13 | ||||
| Avoidance behavior | 8 | ||||
| Anosognosia/thought disorder etc. | 3 | ||||
| Accidents/traffic offences/police controls due to driving behavior (last 2 years) | 2 | ||||
| Passenger feels unsafe | 2 | ||||
| Daytime sleepiness | 2 | ||||
| Impairment BADL | 1 | ||||
| Limited head rotation, but >45° | 1 | ||||
| Psychotropic substances (uptitration phase) | 1 | ||||
| Mild Alzheimer’s dementia | 1 | ||||
| SAFE Subscores | Unimpaired Drivers | Impaired Drivers | Sensitivity (%) | Specifity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| Total risk | low | ≥medium | 79 | 100 | 100 | 43 |
| Number of risk factors | 0 | ≥1 | 95 | 100 | 100 | 75 |
| Risk factor score | 0 | ≥1 | 95 | 100 | 100 | 75 |
3.3. Neuropsychological Tests
| Neuropsychological Tests | M | Md | Min | Max | SD | Correlation with Corporal A 1 |
|---|---|---|---|---|---|---|
| MMSE | 27.3 | 28 | 19 | 30 | 2.6 | 0.54 ** |
| RAVLT learning | 41.4 | 43 | 12 | 66 | 14.6 | 0.50 ** |
| RAVLT recall | 6 | 7 | 0 | 15 | 4.8 | 0.43 ** |
| RAVLT recognition | 12.3 | 14 | 3 | 15 | 3.2 | 0.42 * |
| RAVLT false positives | 6.2 | 4 | 0 | 20 | 6.3 | −0.44 ** |
| Constructional Praxis II | 5.9 | 7 | 0 | 11 | 3.4 | 0.40 * |
| BNT | 14 | 15 | 10 | 15 | 1.6 | 0.29 |
| Category Fluency Task | 19.3 | 19.5 | 9 | 33 | 6 | 0.31 * |
| TMT-A | 45.9 | 44.5 | 18 | 87 | 16.9 | −0.60 ** |
| Clock Drawing Test | 0.23 | 0 | 0 | 1 | 0.43 | −0.20 |
| Number Transcoding | 0.5 | 0 | 0 | 4 | 0.96 | −0.28 |
| TMT-B | 176.5 | 132.5 | 41 | 517 | 120.5 | −0.50 ** |
| Neuropsychological Tests | Unimpaired Drivers | Impaired Drivers | Sensitivity (%) | Specifity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|
| MMSE | ≥29 | ≤28 | 68 | 100 | 100 | 33 |
| RAVLT learning | ≥54 | ≤53 | 89 | 67 | 94 | 50 |
| RAVLT recall | ≥11 | ≤10 | 89 | 67 | 94 | 50 |
| RAVLT recognition | ≥14 | ≤13 | 56 | 100 | 100 | 27 |
| RAVLT false positives | ≤1 | ≥2 | 83 | 100 | 100 | 50 |
| Constructional Praxis II | ≥8 | ≤7 | 78 | 67 | 93 | 33 |
| BNT | 15 | ≤14 | 53 | 100 | 100 | 25 |
| Category Fluency Task | ≥24 | ≤23 | 84 | 67 | 94 | 40 |
| TMT-A | ≤37 | ≥38 | 68 | 100 | 100 | 33 |
| Clock Drawing Test | 0 | ≥1 | 21 | 67 | 80 | 12 |
| Number Transcoding | 0 | ≥1 | 32 | 67 | 86 | 13 |
| TMT-B | ≤116 | ≥117 | 79 | 100 | 100 | 43 |
4. Discussion
4.1. Corporal A and Percentile Rank 16 Criterion
4.2. SAFE
4.3. Neuropsychological Tests
4.4. Conclusions and Limitations
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hedden, T.; Gabrieli, J.D.E. Insights into the ageing mind: A view from cognitive neuroscience. Nat. Rev. Neurosci. 2004, 5, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Falkenstein, M.; Sommer, S.M. Altersbegleitende Veränderungen kognitiver und neuronaler Prozesse mit Bedeutung für das Autofahren. In Leistungsfähigkeit und Mobilität im Alter; Schlag, B., Ed.; TÜV Media GmbH: Köln, Germany, 2008; pp. 113–141. [Google Scholar]
- Kroll, G.; Kaiser, A.; Krone, M.; Mönning, M.; Griese, H.; Macek, C.; Hartje, W. Die praktische Fahrprobe im mittleren und höheren Lebensalter. Z. Neuropsychol. 2003, 14, 81–87. [Google Scholar] [CrossRef]
- Pottgiesser, S.; Kleinemas, U.; Dohmes, K.; Spiegel, L.; Schädlich, M.; Rudinger, G. Profiles of Elderly Drivers with Accidents (PROSA); Bundesanstalt für Straßenwesen: Wirtschaftsverlag NW; Verlag für neue Wissenschaft GmbH: Bremerhaven, Germany, 2012; Available online: http://trid.trb.org/view.aspx?id=1217291 (accessed on 2 November 2015).
- Langford, J.; Methorst, R.; Hakamies-Blomqvist, L. Older drivers do not have a high crash risk—A replication of low mileage bias. Accid. Anal. Prev. 2006, 38, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Bäckman, L.; Jones, S.; Berger, A.-K.; Laukka, E.J.; Small, B.J. Cognitive impairment in preclinical Alzheimer’s disease: A meta-analysis. Neuropsychology 2005, 19, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Collie, A.; Maruff, P. The neuropsychology of preclinical Alzheimer’s disease and mild cognitive impairment. Neurosci. Biobehav. Rev. 2000, 24, 365–374. [Google Scholar] [CrossRef]
- Salmon, D.P. Neuropsychological features of mild cognitive impairment and preclinical Alzheimer’s disease. Curr. Top. Behav. Neurosci. 2012, 10, 187–212. [Google Scholar] [PubMed]
- Toepper, M.; Beblo, T.; Thomas, C.; Driessen, M. Early detection of Alzheimer’s disease: A new working memory paradigm. Int. J. Geriatr. Psychiatr. 2008, 23, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Cushman, L.A.; Stein, K.; Duffy, C.J. Detecting navigational deficits in cognitive aging and Alzheimer disease using virtual reality. Neurology 2008, 71, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Iachini, T.; Iavarone, A.; Senese, V.; Ruotolo, F.; Ruggiero, G. Visuospatial Memory in Healthy Elderly, AD and MCI: A Review. Curr. Aging Sci. 2009, 2, 43–59. [Google Scholar] [CrossRef] [PubMed]
- Toepper, M.; Steuwe, C.; Beblo, T.; Bauer, E.; Boedeker, S.; Thomas, C.; Markowitsch, H.J.; Driessen, M.; Sammer, G. Deficient symbol processing in Alzheimer disease. Alzheimer Dis. Assoc. Disord. 2014, 28, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Brashear, A.; Unverzagt, F.W.; Kuhn, E.R.; Glazier, B.S.; Farlow, M.R.; Perkins, A.J.; Hui, S.L. Impaired traffic sign recognition in drivers with dementia. Am. J. Alzheimers Dis. Other Demen. 1998, 13, 131–137. [Google Scholar] [CrossRef]
- Mix, S.; Lämmler, G.; Steinhagen-Thiessen, E. Fahreignung bei Demenz: Eine Herausforderung für neuropsychologische Diagnostik und Beratung. GeroPsych 2004, 17, 97–108. [Google Scholar] [CrossRef]
- Kessler, H.; Supprian, T. Zum Problem der Krankheitseinsicht bei Patienten mit Demenz vom Alzheimer-Typ. Fortschr. Neurol. Psych. 2003, 71, 541–548. [Google Scholar]
- Hopkins, R.W.; Kilik, L.; Day, D.J.; Rows, C.; Tseng, H. Driving and dementia in Ontario: A quantitative assessment of the problem. Can. J. Psychiatr. 2004, 49, 434–438. [Google Scholar]
- Golz, D.; Huchler, S.; Jörg, A.; Küst, J. Beurteilung der Fahreignung. Z. Neuropsychol. 2004, 15, 157–167. [Google Scholar] [CrossRef]
- Spannhorst, S.; Kreisel, S.; Töpper, M.; Thomas, C. Konsensusverfahren zur Beratung von Senioren in der Gedächtnissprechstunde. NeuroTransmitter 2014, 25, 30–34. [Google Scholar] [CrossRef]
- Mosimann, U.P.; Bächli-Biétry, J.; Boll, J.; Bopp-Kistler, I.; Donati, F.; Kressig, R.W.; Martensson, B.; Monsch, A.U.; Müri, R.; Nef, T.; et al. Konsensusempfehlungen zur Beurteilung der medizinischen Mindestanforderungen für Fahreignung bei kognitiver Beeinträchtigung. Praxis 2012, 101, 451–464. [Google Scholar] [CrossRef] [PubMed]
- Berg, M.; Schubert, W. Corporal—Thematisches Testsystem zur Erfassung von Funktionen der Aufmerksamkeit: Innovation für verkehrspsychologische Diagnostik. Zeitschrift für Verkehrssicherheit 1999, 45, 74–81. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Müller, H.; Hasse-Sander, I.; Horn, R.; Helmstaedter, C.; Elger, E. Rey auditory-verbal learning test: Structure of a modified German version. J. Clin. Psychol. 1997, 53, 663–671. [Google Scholar] [CrossRef]
- Morris, J.C.; Heyman, A.; Mohs, R.C.; Hughes, J.P.; van Belle, G.; Fillenbaum, G.; Mellits, E.D.; Clark, C. The consortium to establish a registry for Alzheimer’s disease (CERAD): I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 1989, 39, 1159–1165. [Google Scholar] [PubMed]
- Thalmann, B.; Monsch, A.U. CERAD The Consortium to Establish a Registry for Alzheimer’s Disease. Neuropsychologische Testbatterie; Memory Clinic: Basel, Switzerland, 1997. [Google Scholar]
- Kaplan, E.; Goodglass, H.; Weintraub, S. Boston Naming Test; Lea & Febiger: Philadelphia, PA, USA, 1983. [Google Scholar]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W. Neuropsychological Assessment, 4th ed.; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Reitan, R.M. The relation of the Trail Making Test to organic brain damage. J. Consult. Psychol. 1955, 19, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Tombaugh, T. Trail Making Test A and B: Normative data stratified by age and education. Arch. Clin. Neuropsychol. 2004, 19, 203–214. [Google Scholar] [CrossRef]
- Shulman, K.I.; Pushkar Gold, D.; Cohen, C.A.; Zucchero, C.A. Clock-drawing and dementia in the community: A longitudinal study. Int. J. Geriatr. Psychiatr. 1993, 8, 487–496. [Google Scholar] [CrossRef]
- Schröder, M.R.; Hasse Sander, I.; Muller, H.; Horn, R.; Möller, H.J. Merkmalsanalyse von Uhrzeichnungen als Beitrag zur Diagnostik der Demenz vom Alzheimer Typ. GeroPsych 1999, 12, 55–66. [Google Scholar] [CrossRef]
- Kessler, J.; Calabrese, P.; Kalbe, E.; Berger, F. DemTect: A new screening method to support diagnosis of dementia. Psycho 2000, 26, 343–347. [Google Scholar]
- Gatterer, G. Multiprofessionelles Geriatrisches Assessment. GeroPsych 2007, 20, 125–134. [Google Scholar] [CrossRef]
- Ott, B.R.; Davis, J.D.; Papandonatos, G.D.; Hewitt, S.; Festa, E.K.; Heindel, W.C.; Snellgrove, C.A.; Carr, D.B. Assessment of Driving-Related Skills Prediction of Unsafe Driving in Older Adults in the Office Setting. J. Am. Geriatr. Soc. 2013, 61, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Bortz, J.; Lienert, G.A. Kurzgefasste Statistik für die klinische Forschung; Springer Medizin Verlag: Heidelberg, Germany, 2008. [Google Scholar]
- Fimm, B.; Blankenheim, A.; Poschadel, S. Dementia and Road Safety; Bundesanstalt für Straßenwesen: Fachverlag NW in der Carl Schünemann Verlag GmbH: Bremerhaven, Germany, 2015; Available online: http://trid.trb.org/view.aspx?id=1358429 (accessed on 2 November 2015).
- Niemann, H.; Hartje, W. Beurteilung der Fahreignung hirngeschädigter Patienten in der neurologischen Rehabilitation. Z. Neuropsychol. 2013, 24, 69–87. [Google Scholar] [CrossRef]
- Poschadel, S. Traffic Related Performance Potentials, Deficits and Compensation Possibilities of Elderly Drivers; Bundesanstalt für Straßenwesen: Wirtschaftsverlag NW; Verlag für neue Wissenschaft: Bremerhaven, Germany, 2012; Available online: http://trid.trb.org/view.aspx?id=1247406 (accessed on 2 November 2015).
- Engeln, A.; Schlag, B. Kompensationsstrategien im Alter. In Leistungsfähigkeit und Mobilität im Alter; Schlag, B., Ed.; TÜV Media GmbH: Köln, Germany, 2008; pp. 255–275. [Google Scholar]
- Ball, K.K.; Roenker, D.L.; Wadley, V.G.; Edwards, J.D.; Roth, D.L.; McGwin, G.; Raleigh, R.; Joyce, J.J.; Cissell, G.M.; Dube, T. Can high-risk older drivers be identified through performance-based measures in a Department of Motor Vehicles setting? J. Am. Geriatr. Soc. 2006, 54, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Dobbs, B.M.; Shergill, S.S. How effective is the Trail Making Test (Parts A and B) in identifying cognitively impaired drivers? Age Ageing 2013, 42, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Mathias, J.L.; Lucas, L.K. Cognitive predictors of unsafe driving in older drivers: A meta-analysis. Int. Psychoger. 2009, 21, 637–653. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schulz, P.; Spannhorst, S.; Beblo, T.; Thomas, C.; Kreisel, S.; Driessen, M.; Toepper, M. Preliminary Validation of a Questionnaire Covering Risk Factors for Impaired Driving Skills in Elderly Patients. Geriatrics 2016, 1, 5. https://doi.org/10.3390/geriatrics1010005
Schulz P, Spannhorst S, Beblo T, Thomas C, Kreisel S, Driessen M, Toepper M. Preliminary Validation of a Questionnaire Covering Risk Factors for Impaired Driving Skills in Elderly Patients. Geriatrics. 2016; 1(1):5. https://doi.org/10.3390/geriatrics1010005
Chicago/Turabian StyleSchulz, Philipp, Stefan Spannhorst, Thomas Beblo, Christine Thomas, Stefan Kreisel, Martin Driessen, and Max Toepper. 2016. "Preliminary Validation of a Questionnaire Covering Risk Factors for Impaired Driving Skills in Elderly Patients" Geriatrics 1, no. 1: 5. https://doi.org/10.3390/geriatrics1010005
APA StyleSchulz, P., Spannhorst, S., Beblo, T., Thomas, C., Kreisel, S., Driessen, M., & Toepper, M. (2016). Preliminary Validation of a Questionnaire Covering Risk Factors for Impaired Driving Skills in Elderly Patients. Geriatrics, 1(1), 5. https://doi.org/10.3390/geriatrics1010005





