A Cost-Effective Reusable Tissue Mimicking Phantom for High Intensity Focused Ultrasonic Liver Surgery
Abstract
1. Introduction
2. Methods
2.1. Preparation of NP14-PASG
2.2. Measurements of Physical Properties
2.3. Measurements of Optical Property
2.4. Visualization of Thermal Lesions
3. Results
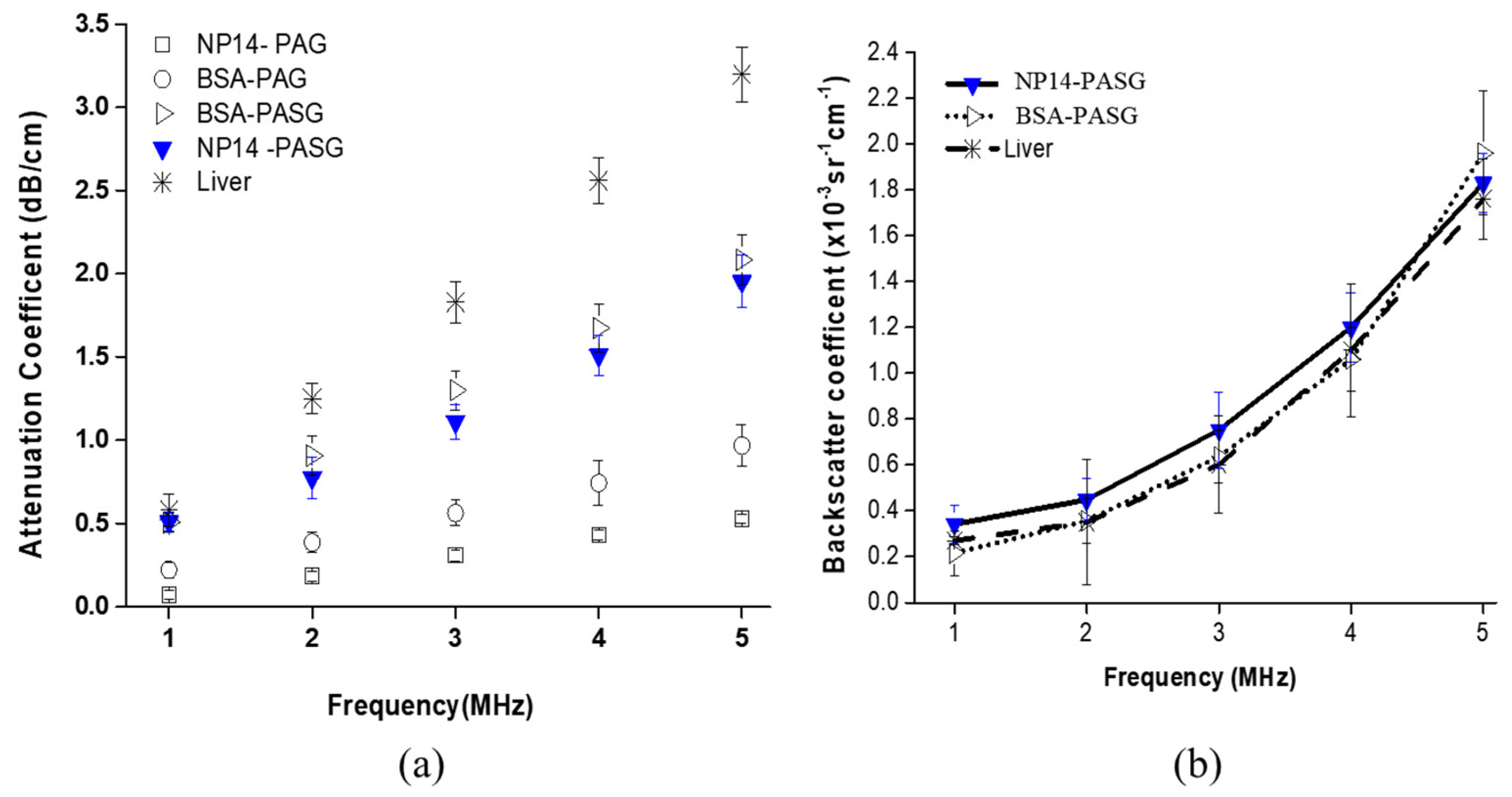
3.1. Physical Properties
| Acoustic Parameter | Units | Liver | BSA-PASG | NP14-PASG |
|---|---|---|---|---|
| Acoustic impedance | Mrays | 1.68 ± 0.02 | 1.68 ± 0.03 (1.000) | 1.70 ± 0.02 (1.012) |
| Speed of sound | m/s | 1575 ± 10 | 1588 ± 9 (1.008) | 1605 ± 8 (1.019) |
| Attenuation coefficient (at 1 MHz) | dB/cm | 0.52 ± 0.03 | 0.51 ± 0.06 (0.981) | 0.50 ± 0.09 (0.962) |
| Backscatter coefficient (at 1 MHz) | sr−1 cm−1 | 0.27 ± 0.017 × 10−3 | 0.22 ± 0.097 × 10−3 (0.815) | 0.21 ± 0.09 × 10−3 (0.778) |
| B/A | - | 6.8 ± 0.14 | 5.9 ± 0.3 (0.868) | 6.4 ± 0.2 (0.941) |
| Mechanical Parameter | Unit | Liver | BSA-PASG | NP14-PASG |
|---|---|---|---|---|
| Density | kg/m3 | 1060 ± 10 | 1057 ± 13 (0.997) | 1061 ± 10 (1.001) |
| Shear Modulus | kPa | 3.5 ± 0.55 | 4.55 ± 0.33 (1.300) | 4.29 ± 0.39 (1.226) |
| Young’s Modulus | kPa | 13 ± 0.30 | 10.63 ± 0.93 (0.818) | 9.94 ± 0.31 (0.765) |
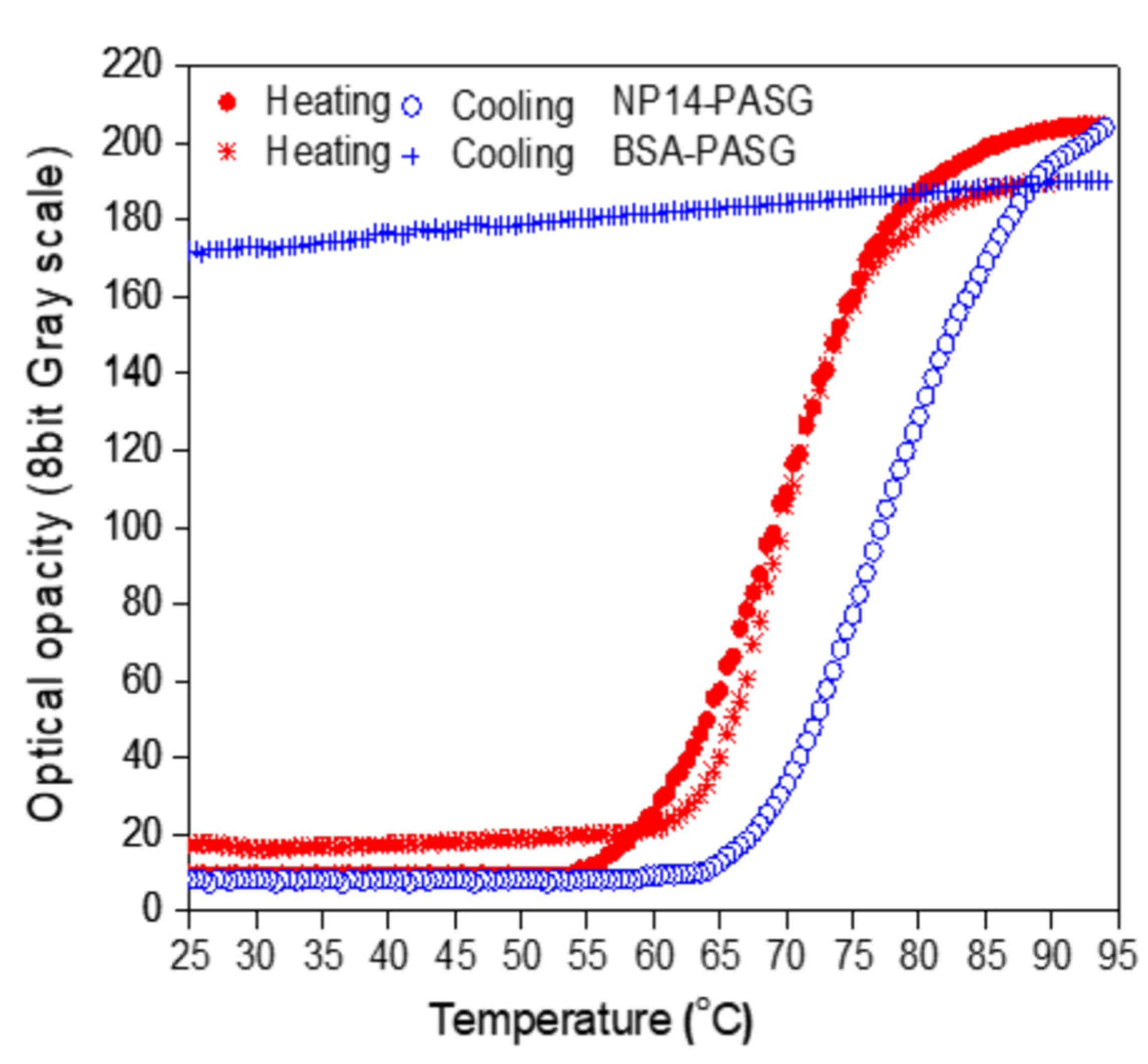
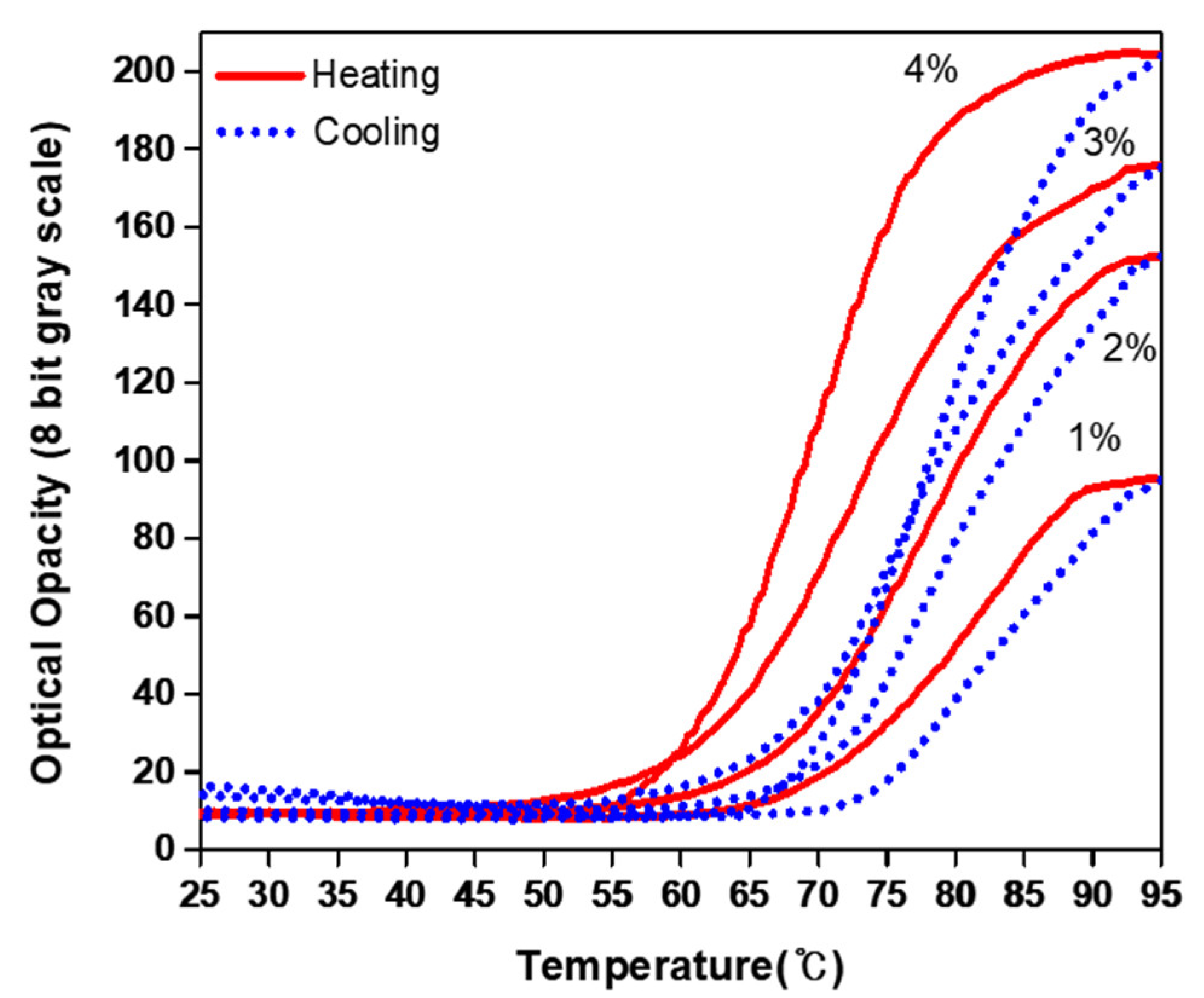
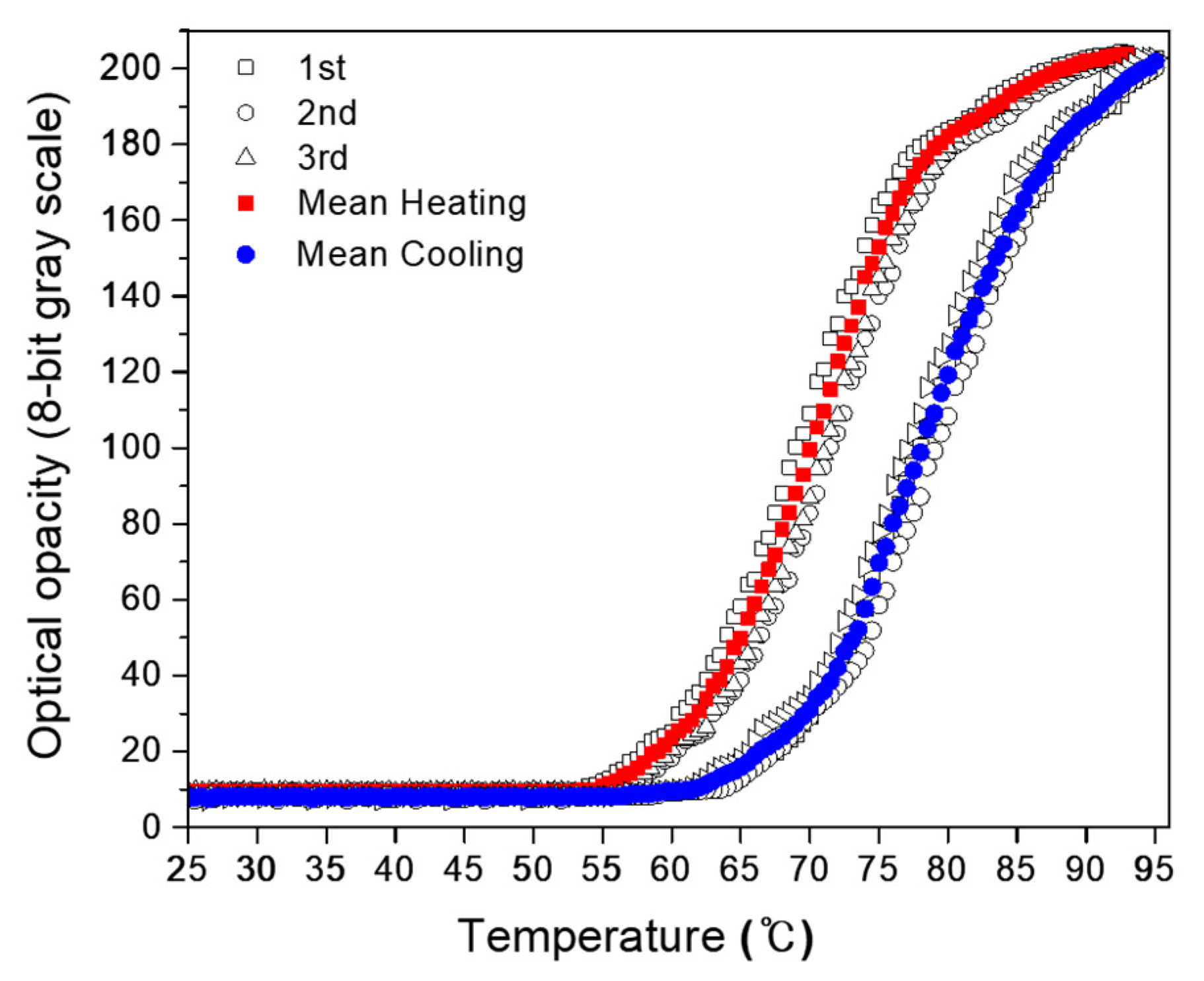
3.2. Optical Opacity against Temperature
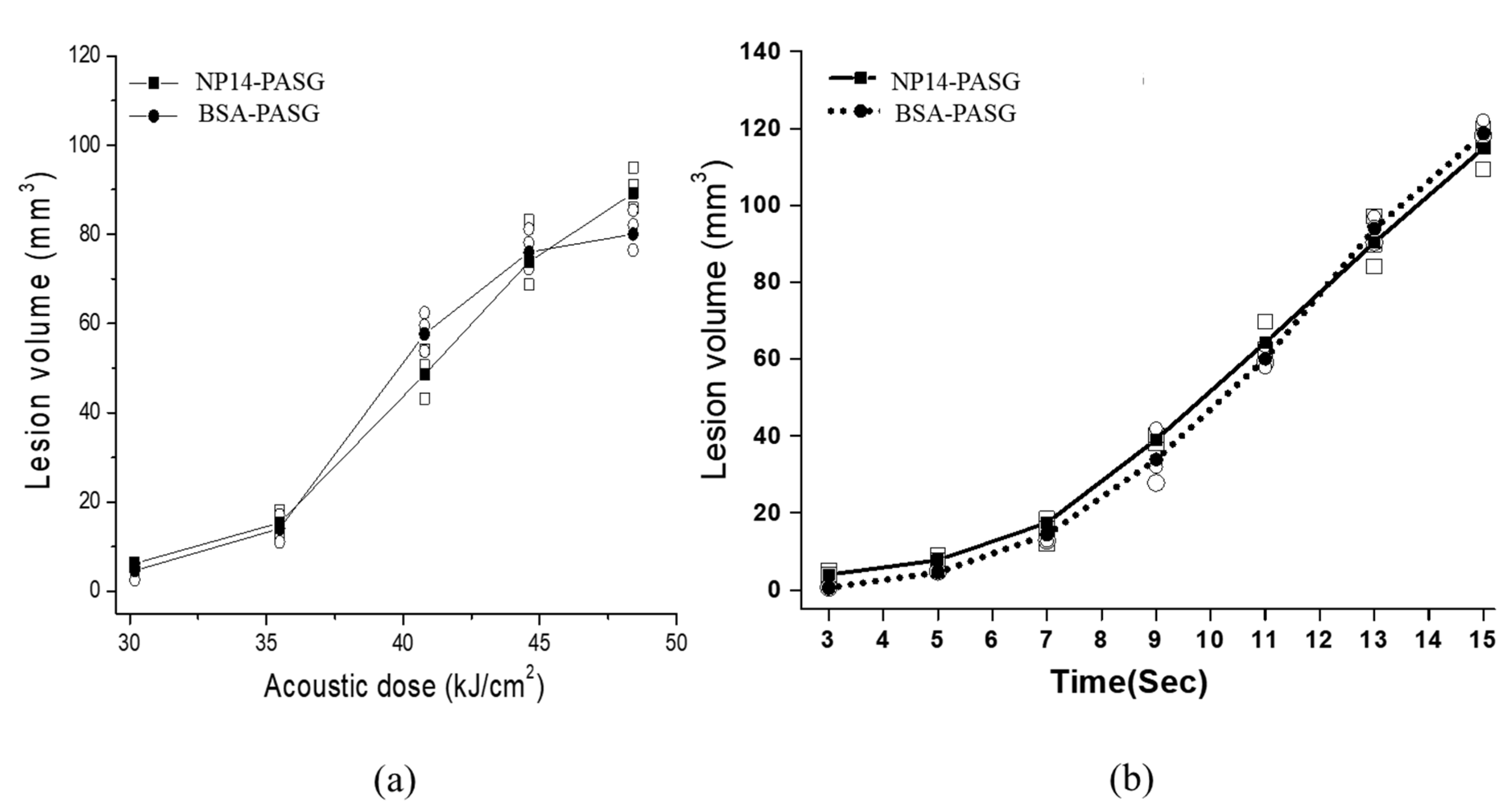
3.3. Visualization of Thermal Lesions
3.4. Size of Thermal Lesions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Agnese, D.M.; Burak, W.E., Jr. Ablative approaches to the minimally invasive treatment of breast cancer. Cancer J. 2005, 11, 77–82. [Google Scholar] [PubMed]
- Ahmed, M.; Goldberg, S.N. Thermal ablation therapy for hepatocellular carcinoma. J. Vasc. Interv. Radiol. 2002, 13, S231–S244. [Google Scholar] [CrossRef] [PubMed]
- Lafon, C.; Vesna, Z.; Noble, M.; Yuen, J.C.; Vaezy, S.J. Gel phantom for use in high intensity focused ultrasound dosimetry. Ultrasound Med. Biol. 2005, 31, 1383–1389. [Google Scholar] [CrossRef] [PubMed]
- Takegami, K.; Kaneko, Y.; Watanabe, T.; Maruyama, T.; Mastsumoto, Y.; Nagawa, H. Polyacrylamide gel containing egg white as new model for irradiation experiments using focused ultrasound. Ultrasound Med. Biol. 2004, 30, 1419–1422. [Google Scholar] [PubMed]
- Dewhirst, M.W.; Viglianti, B.L.; Michiels, M.L.; Hoopes, P.J.; Hanson, M. Thermal dose requirement for tissue effect: Experimental and clinical findings. Therm. Treat. Tissue Energy Deliv. Assess. II 2003, 4954, 37–52. [Google Scholar]
- Park, S.K.; Guntur, S.R.; Lee, K.I.; Paeng, D.G.; Choi, M.J. Reusable ultrasonic tissue mimicking hydro gels containing nonionic surface active agent for Visualizing thermal lesions. IEEE Trans. Biomed. Eng. 2010, 57, 194–202. [Google Scholar] [CrossRef]
- Miyakawa, M.; Hoshina, S.A. New Gel Phantom Used for Three-Dimensional Measurement of the Local SAR. In Proceedings of the 1996 IEEE MTT-S International Microwave Symposium Digest, San Francisco, CA, USA, 17–21 June 1996; Volume 2, pp. 1089–1092. [Google Scholar]
- Miyakawa, M.; Hoshina, S.A. Self-Supporting Gel Phantom Used for Visualization and/or Measurement of the Three-dimensional Distribution of SAR. In Proceedings of the 2002 IEEE International Symposium on Electromagnetic Compatibility, Minneapolis, MN, USA, 19–23 August 2002; Volume 2, pp. 671–676. [Google Scholar]
- Guntur, S.R.; Choi, M.J. An improved tissue mimicking polyacrylamide gel for visualization of thermal lesions produced by HIFU. Ultrasound Med. Biol. 2014, 40, 2680–2691. [Google Scholar]
- Shieh, J.; Chen, S.R.; Chen, G.S.; Lo, C.W.; Chen, C.S.; Chen, B.T.; Sun, M.K.; Huang, C.W.; Chen, W.S. Acrylic acid controlled reusable temperature-sensitive hydrogel phantoms for thermal ablation therapy. Appl. Therm. Eng. 2014, 62, 3220–3329. [Google Scholar] [CrossRef]
- Sun, M.K.; Shieh, J.; Lo, C.W.; Chen, C.S.; Chen, B.T.; Huang, C.W.; Chen, W.S. Reusable tissue-mimicking hydrogel phantoms for focused ultrasound ablation. Ultrason. Sonochem. 2015, 23, 399–405. [Google Scholar] [CrossRef]
- Guntur, S.R. Tissue Mimicking Phantoms for Visualizing Thermal Lesions by High Intensity Focused Ultrasound. Ph.D. Thesis, Jeju National University, Jeju, Republic of Korea, 2013. [Google Scholar]
- Fei, D.Y.; Shung, K.K. Ultrasonic backscatter from mammalian tissues. J. Acoust. Soc. Am. 1985, 78, 651–654. [Google Scholar]
- Kuo, I.Y.; Hete, B.; Shung, K.K. A novel method for the measurement of acoustic speed. J. Acoust. Soc. Am. 1990, 88, 1679–1682. [Google Scholar] [PubMed]
- Madsen, E.L.; Dong, F.; Frank, G.R.; Garra, B.S.; Wear, K.A.; Wilson, T.; Zagzebski, J.A.; Miller, H.L.; Shung, K.K.; Miller, J.G. Interlaboratory comparison of ultrasonic backscatter, attenuation and speed measurements. J. Ultrasound Med. 1999, 18, 615–631. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.J.; Guntur, S.R.; Lee, J.M.; Lee, K.I.; Paeng, D.G.; Coleman, A.J. Changes in ultrasonic properties of liver tissue in vitro during heating-cooling cycle concomitant with thermal coagulation. Ultrasound Med. Biol. 2011, 37, 2000–2012. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.J.; Guntur, S.R.; Lee, K.I.; Paeng, D.G.; Coleman, A.J. A tissue mimicking polyacrylamide hydrogel phantom for visualizing thermal lesions generated by high intensity focused ultrasound. Ultrasound Med. Biol. 2013, 29, 439–448. [Google Scholar]
- Lee, F.T. Influence to the Quality of Images by the Defects of Piezoelectricelements of the Probe of Medical Ultrasonic Scanners. Ph.D. Thesis, Jeju National University, Jeju, Republic of Korea, 2009. [Google Scholar]
- Takahashi, S. Illustrated Computer Tomography: A Practical Guide to CT Interpretations, 1st ed.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 1983; pp. 18–39. [Google Scholar]
- Ophir, J.; Jaeger, P.A. Ternary solution for independent acoustic impedance and speed of sound matching to biological tissues. Ultrasound Imaging 1982, 4, 163–170. [Google Scholar] [CrossRef]
- Ophir, J.; Ghouse, M.A.; Ferrari, L.A. Attenuation estimation with the zero-crossing technique: Phantom studies. Ultrasound Imaging 1985, 7, 122–132. [Google Scholar]
- Lu, Z.F.; Zagzebski, J.A.; Lee, F.T. Ultrasound backscatter and attenuation in human liver with diffuse disease. Ultrasound Med. Biol. 1999, 25, 1047–1054. [Google Scholar] [CrossRef]
- Wilson, L.S.; Robinson, D.E.; Doutst, B.D. Frequency domain processing for ultrasonic attenuation measurement in the liver. Ultrason. Imaging 1984, 6, 278–292. [Google Scholar] [CrossRef]
- Nicholas, D. Evaluation of backscattering coefficient for excised human tissues: Results, interpretation, and associated measurements. Ultrasound Med. Biol. 1982, 8, 17–28. [Google Scholar]
- Gong, X.F.; Zhu, Z.M.; Shi, X.; Huang, J.H. Determination of the acoustic nonlinearity parameter in biological media using FAIS and ITD methods. J. Acoust. Soc. Am. 1989, 86, 1–5. [Google Scholar]
- Tay, B.K.; Kim, J.; Srinivasan, M.A. In vivo mechanical behavior of intraabdominal organs. IEEE Trans. Biomed. Eng. 2006, 53, 2129–2138. [Google Scholar] [CrossRef] [PubMed]
- Kruse, S.A.; Smith, J.A.; Lawrence, A.J.; Manduca, A.; Ehman, R.L. Tissuecharacterization using magnetic resonance elastography: Preliminary results. Phys. Med. Biol. 2000, 45, 1579. [Google Scholar] [CrossRef] [PubMed]
- Duck, F.A. Physical Properties of Tissue: A Comprehensive Reference Book; Academic Press: London, UK, 1990; p. 95. [Google Scholar]
- Giering, K.; Hambrecht, I.; Minet, O.; Handke, A. Determination of the specific heat capacity of healthy and timorous human tissue. Thermochim. Acta 1995, 251, 199–205. [Google Scholar] [CrossRef]
- George, C.; Yuan, B.O.; Stevens, H.J.; Weekley, B.S.; Rajagopalan, N. Clouding point of nonionic surfactants: Modulation with pharmaceutical excipients. Pharm. Res. 1999, 16, 562–568. [Google Scholar]
- Kuroda, M.; Kato, H.; Hanamoto, K.; Shimamura, K.; Uchida, T.; Wang, Y.; Akaki, S.; Asaumi, J.; Himei, K.; Takemoto, M.; et al. Development of a new hybrid gel phantomusing carrageenan and gellan gum for visualizing three-dimensional temperature distribution during hyperthermia and radiofrequency ablation. Int. J. Oncol. 2005, 27, 175–184. [Google Scholar]
- Madsen, E.L.; Frank, G.R.; Dong, F. Liquid or solid ultrasonically tissue-mimicking materials with very low scatter. Ultrasound Med. Biol. 1998, 24, 535–542. [Google Scholar]
- Kim, Y.S.; Rhim, H.; Choi, M.J.; Lim, H.K.; Choi, D. High intensity focused ultrasound therapy: An overview for radiologists. Korean J. Radiol. 2008, 9, 291–302. [Google Scholar] [CrossRef]




| Components | Quantity (mL, g) | Proportion (% in v/v or w/v) |
|---|---|---|
| Distilled Water | 27.80 mL | 55.60 %(v/v) |
| Polysaccharide * | 20 g | 40 %(w/v) |
| NP-14 ** | 2 g | 4 %(w/v) |
| 40 %(w/v) Acrylamide | 8.75 mL | 17.50 %(v/v) |
| Sodium Azid | 0.1 g | 0.20 %(w/v) |
| Potassium Iodide(KI) | 0.5 g | 1 %(w/v) |
| Glass Bead (40~80 µm) | 0.01 × 10−1 g | 0.02 × 10−2 %(w/v) |
| 10 %(w/v) APS | 0.250 mL | 0.50 %(v/v) |
| TEMED | 0.10 mL | 0.20 %(v/v) |
| Thermal Parameters | Unit | Liver | BSA PASG | NP14-PASG |
|---|---|---|---|---|
| Specific heat capacity | mJ m−3 C−1 | 3.628 ± 0.078 | 3.933 ± 0.028 (1.084) | 3.910 ± 0.033 (1.078) |
| Thermal conductivity | W/m/°C | 0.572 ± 0.009 | 0.562 ± 0.009 (0.983) | 0.558 ± 0.01 (0.976) |
| Thermal resistivity | m/W/°C | 1.748 ± 0.090 | 1.77 ± 0.027 (1.013) | 1.79 ± 0.04 (1.024) |
| Thermal diffusivity | mm s−2 | 0.128 ± 0.030 | 0.151 ± 0.004 (1.180) | 0.15 ± 0.003 (1.172) |
| Parameter | Unit | BSA-PASG | NP14-PASG | |
|---|---|---|---|---|
| Heating (clouding) | hTs | °C | 62 | 57 |
| hTe | °C | 83 | 84 | |
| hTR | °C | 21 | 27 | |
| hS | gs/°C | 8.0 | 6.9 | |
| Cooling (clearing) | cTs | °C | 90 | 87 |
| cTe | °C | - | 66 | |
| cTR | °C | - | 21 | |
| cS | gs/°C | - | 8.4 | |
| Optical transparency | Xmin | gs | 17 | 10 |
| Xmax | gs | 190 | 203 | |
| XR | gs | 173 | 193 | |
| C | % | 72.7 | 78.8 |
| Parameter | Unit | 1 % | 2 % | 3 % | 4 % | 5 % | |
|---|---|---|---|---|---|---|---|
| Clouding (heating) | hTs | °C | 67 | 63 | 61 | 57 | 54 |
| hTe | °C | 90 | 88 | 87 | 84 | 82 | |
| hTR | °C | 22 | 25 | 26 | 27 | 28 | |
| hS | gs/ °C | 6.0 | 6.2 | 6.6 | 6.9 | 6.5 | |
| Optical transparency | Xmin | gs | 3 | 5 | 8 | 10 | 12 |
| Xmax | gs | 140 | 165 | 185 | 203 | 201 | |
| XR | gs | 137 | 160 | 177 | 193 | 189 | |
| C | % | 54.4 | 64.0 | 71.7 | 78.8 | 77.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guntur, S.R.; Kim, S.-C.; Choi, M.-J. A Cost-Effective Reusable Tissue Mimicking Phantom for High Intensity Focused Ultrasonic Liver Surgery. Bioengineering 2022, 9, 786. https://doi.org/10.3390/bioengineering9120786
Guntur SR, Kim S-C, Choi M-J. A Cost-Effective Reusable Tissue Mimicking Phantom for High Intensity Focused Ultrasonic Liver Surgery. Bioengineering. 2022; 9(12):786. https://doi.org/10.3390/bioengineering9120786
Chicago/Turabian StyleGuntur, Sitaramanjaneya Reddy, Seong-Chan Kim, and Min-Joo Choi. 2022. "A Cost-Effective Reusable Tissue Mimicking Phantom for High Intensity Focused Ultrasonic Liver Surgery" Bioengineering 9, no. 12: 786. https://doi.org/10.3390/bioengineering9120786
APA StyleGuntur, S. R., Kim, S.-C., & Choi, M.-J. (2022). A Cost-Effective Reusable Tissue Mimicking Phantom for High Intensity Focused Ultrasonic Liver Surgery. Bioengineering, 9(12), 786. https://doi.org/10.3390/bioengineering9120786





