Computer-Guided Bone Biopsy: A Technical Note with the Description of a Clinical Case
Abstract
:1. Introduction
2. Materials and Methods
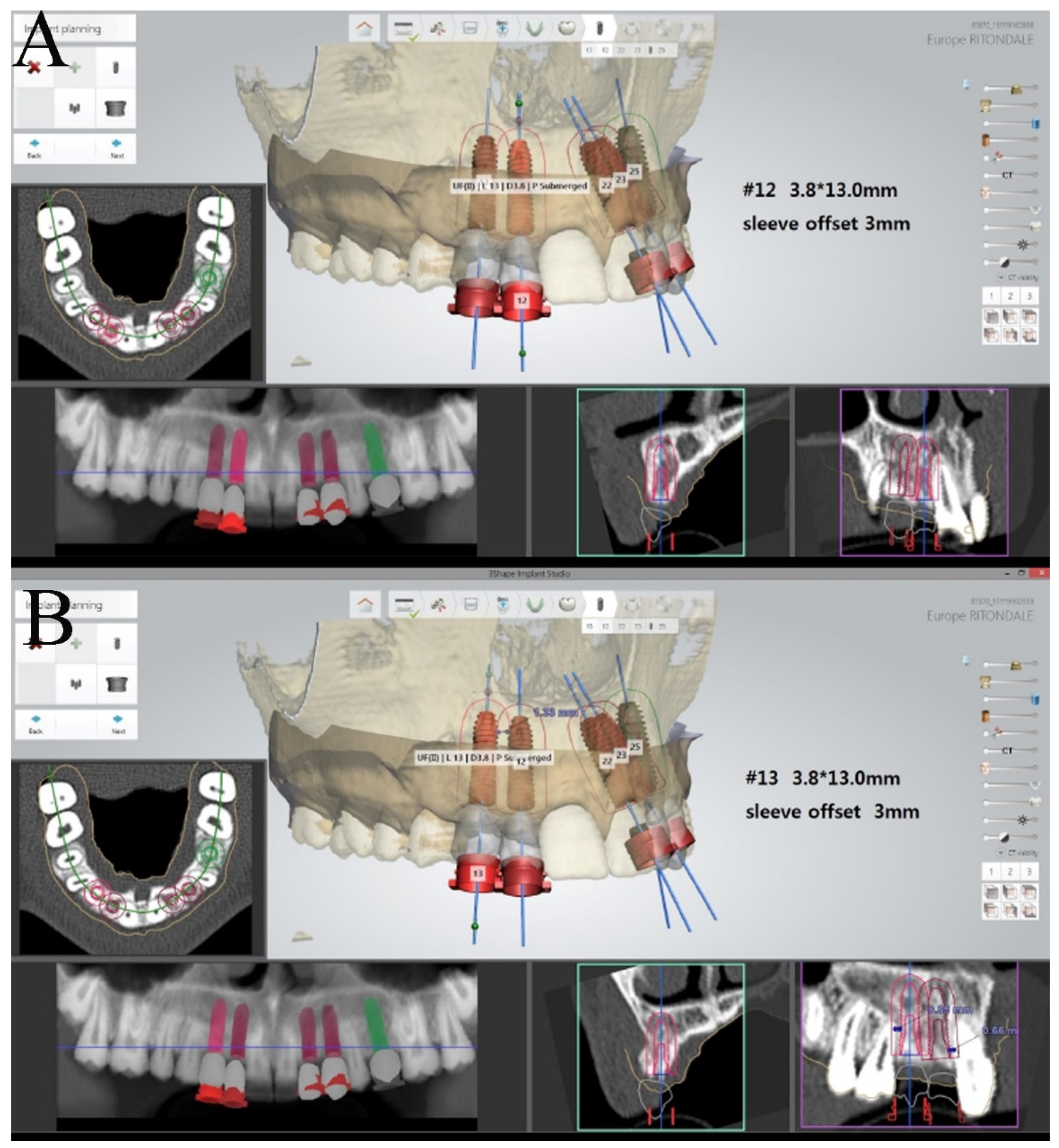
- The determining of bone sampling site and extension. For this purpose, DICOM (Digital Imaging and Communications in Medicine) files of CBCT are acquired using specific planning software and a superimposition of a 3D (three-dimensional) scan of the cast model (Easy Optical3D Scanner, Open Technologies, Rezzato, BS, Italy) is performed after uploading the corresponding STL file (stereolithography file);
- The design of a virtual surgical guide through CAD software that allows a view of the 3D guide from different perspectives and planes; the number and site of guide tubes are determined on the basis of the width and the extension of the sampling;
- The surgical guide printing, thanks to a 3D printer (Stratasys OrhoDesktop, Eden Praire, MN, USA).
3. Description of a Computer-Guided Biopsy
3.1. Manufacturing the Surgical Guide
3.2. Specimen Processing
3.3. Histological Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cassetta, M.; Altieri, F. The influence of mandibular third molar germectomy on the treatment time of impacted mandibular second molars using brass wire: A prospective clinical pilot study. Int. J. Oral Maxillofac. Surg. 2017, 46, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Rosebush, M.S.; Anderson, K.M.; Rawal, S.Y.; Mincer, H.H.; Rawal, Y.B. The oral biopsy: Indications, techniques and special considerations. J. Tenn. Dent. Assoc. 2010, 90, 17–20. [Google Scholar] [PubMed]
- Cassetta, M.; Ricci, L.; Iezzi, G.; Dell’Aquila, D.; Piattelli, A.; Perrotti, V. Resonance frequency analysis of implants inserted with a simultaneous grafting procedure: A 5-year follow-up study in man. Int. J. Periodontics Restor. Dent. 2012, 32, 581–589. [Google Scholar] [PubMed]
- Srivastava, K.C.; Shrivastava, D.; Austin, R.D. Journey towards the 3D dental imaging- the milestones in the advancement of dental imaging. Int. J. Adv. Res. 2016, 4, 377–382. [Google Scholar] [CrossRef] [Green Version]
- Jain, S.; Choudhary, K.; Nagi, R.; Shukla, S.; Kaur, N.; Grover, D. New evolution of cone-beam computed tomography in dentistry: Combining digital technologies. Imaging. Sci. Dent. 2019, 49, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Slagter, K.W.; Hartog, L.; Bakker, N.A. Immediate placement of dental implants in the esthetic zone: A systematic review and pooled analysis. J. Periodontol. 2014, 85, e241–e250. [Google Scholar] [CrossRef] [PubMed]
- Simion, M.; Baldoni, M.; Zaffe, D. Jawbone enlargement using immediate implant placement associated with a split-crest technique and guided tissue regeneration. Int. J. Periodontics Restor. Dent. 1992, 12, 462–473. [Google Scholar] [PubMed]
- Bassetti, R.; Bassetti, M.; Mericske-Stern, R.; Enkling, N. Piezoelectric alveolar ridge splitting technique with simultaneous implant placement: A cohort study with 2-year radiographic results. Int. J. Oral Maxillofac. Implant. 2013, 28, 1570–1580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agabiti, I.; Botticelli, D. Two-Stage Ridge Split at Narrow Alveolar Mandibular Bone Ridges. J. Oral Maxillofac. Surg. 2017, 75, 2115.e1–2115.e12. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Perrotti, V.; Calasso, S.; Piattelli, A.; Sinjari, B.; Iezzi, G. Bone formation in sinus augmentation procedures using autologous bone, porcine bone, and a 50:50 mixture: A human clinical and histological evaluation at 2 months. Clin. Oral Impl. 2015, 26, 1180–1184. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Altieri, F.; Di Giorgio, R.; Barbato, E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: Description of a technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Altieri, F.; Giansanti, M.; Bellardini, M.; Brandetti, G.; Piccoli, L. Is there a learning curve in static computer-assisted surgery? A prospective clinical study. Int. J. Oral Maxillofac. Surg. 2020, 49, 1335–1342. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altieri, F.; Iezzi, G.; Luzzi, V.; Di Giorgio, G.; Polimeni, A.; Cassetta, M. Computer-Guided Bone Biopsy: A Technical Note with the Description of a Clinical Case. Bioengineering 2021, 8, 214. https://doi.org/10.3390/bioengineering8120214
Altieri F, Iezzi G, Luzzi V, Di Giorgio G, Polimeni A, Cassetta M. Computer-Guided Bone Biopsy: A Technical Note with the Description of a Clinical Case. Bioengineering. 2021; 8(12):214. https://doi.org/10.3390/bioengineering8120214
Chicago/Turabian StyleAltieri, Federica, Giovanna Iezzi, Valeria Luzzi, Gianni Di Giorgio, Antonella Polimeni, and Michele Cassetta. 2021. "Computer-Guided Bone Biopsy: A Technical Note with the Description of a Clinical Case" Bioengineering 8, no. 12: 214. https://doi.org/10.3390/bioengineering8120214
APA StyleAltieri, F., Iezzi, G., Luzzi, V., Di Giorgio, G., Polimeni, A., & Cassetta, M. (2021). Computer-Guided Bone Biopsy: A Technical Note with the Description of a Clinical Case. Bioengineering, 8(12), 214. https://doi.org/10.3390/bioengineering8120214








