Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Post Placement
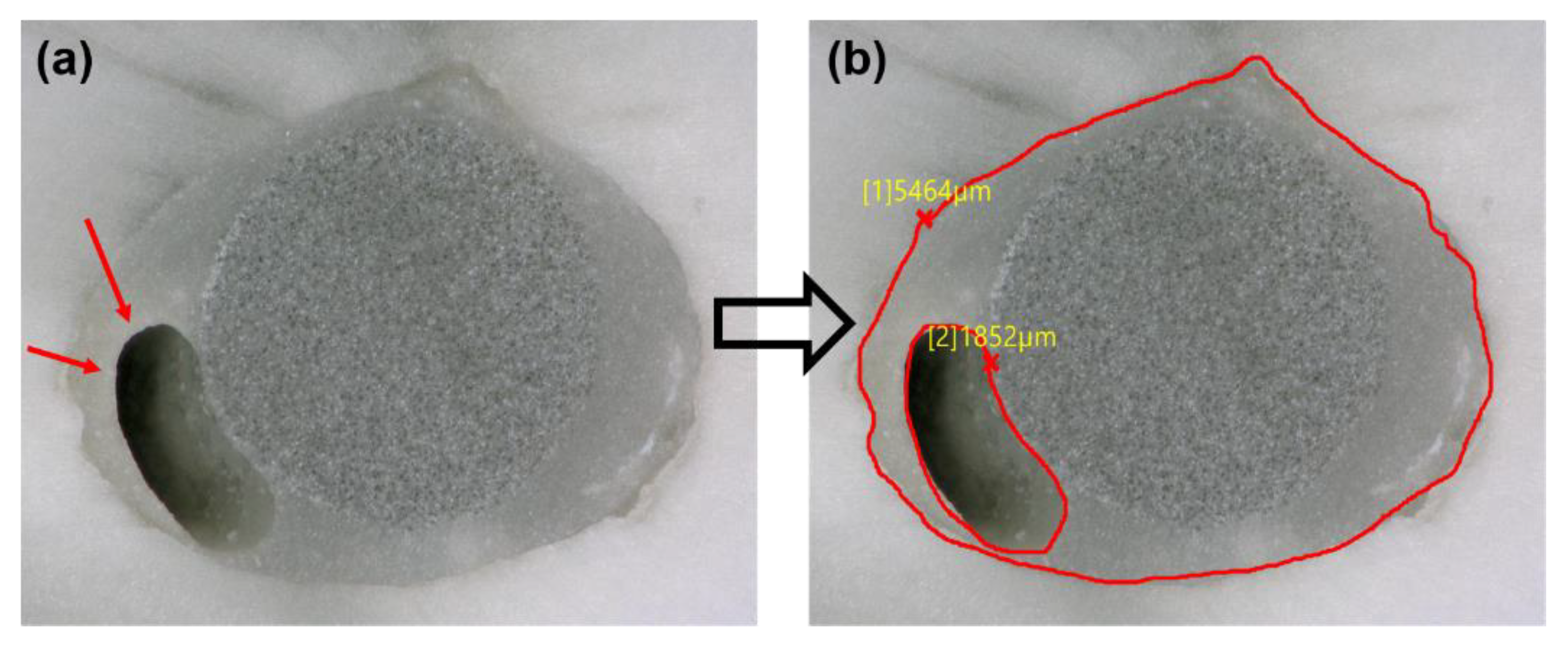
2.3. Filling Ability
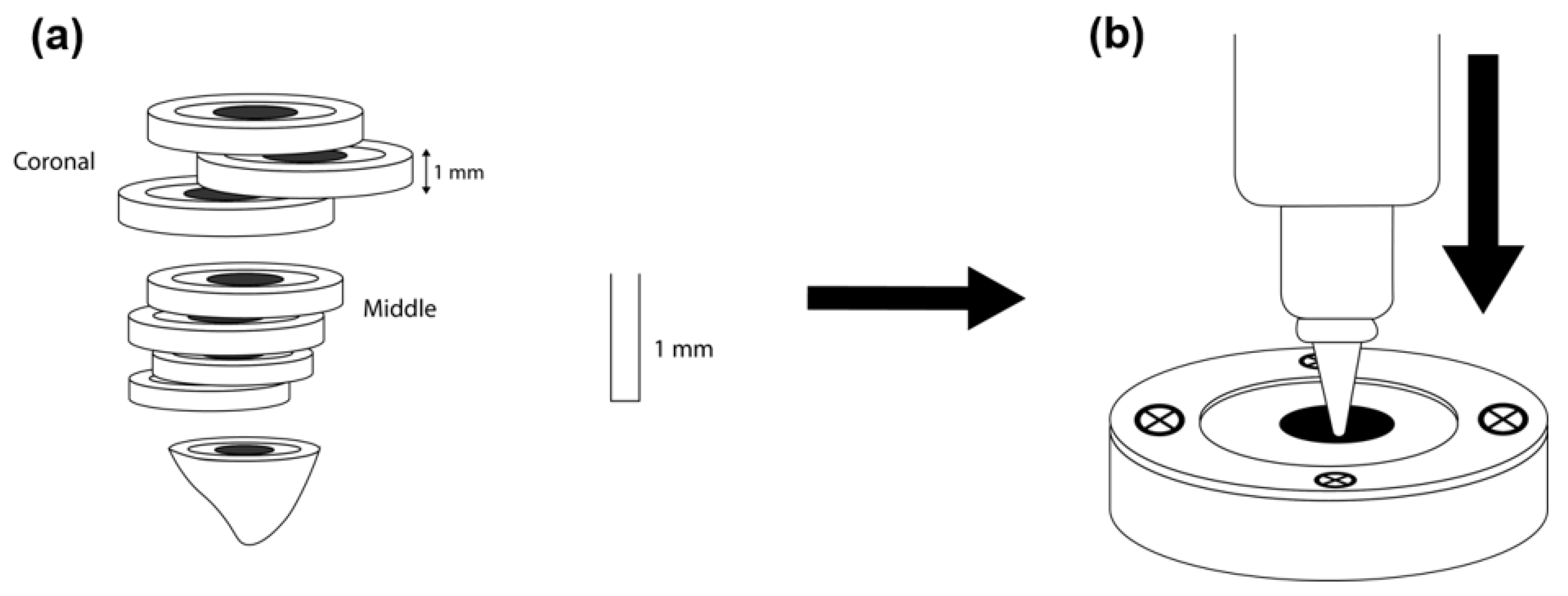
2.4. Push-Out Test
2.5. Failure Mode Analysis
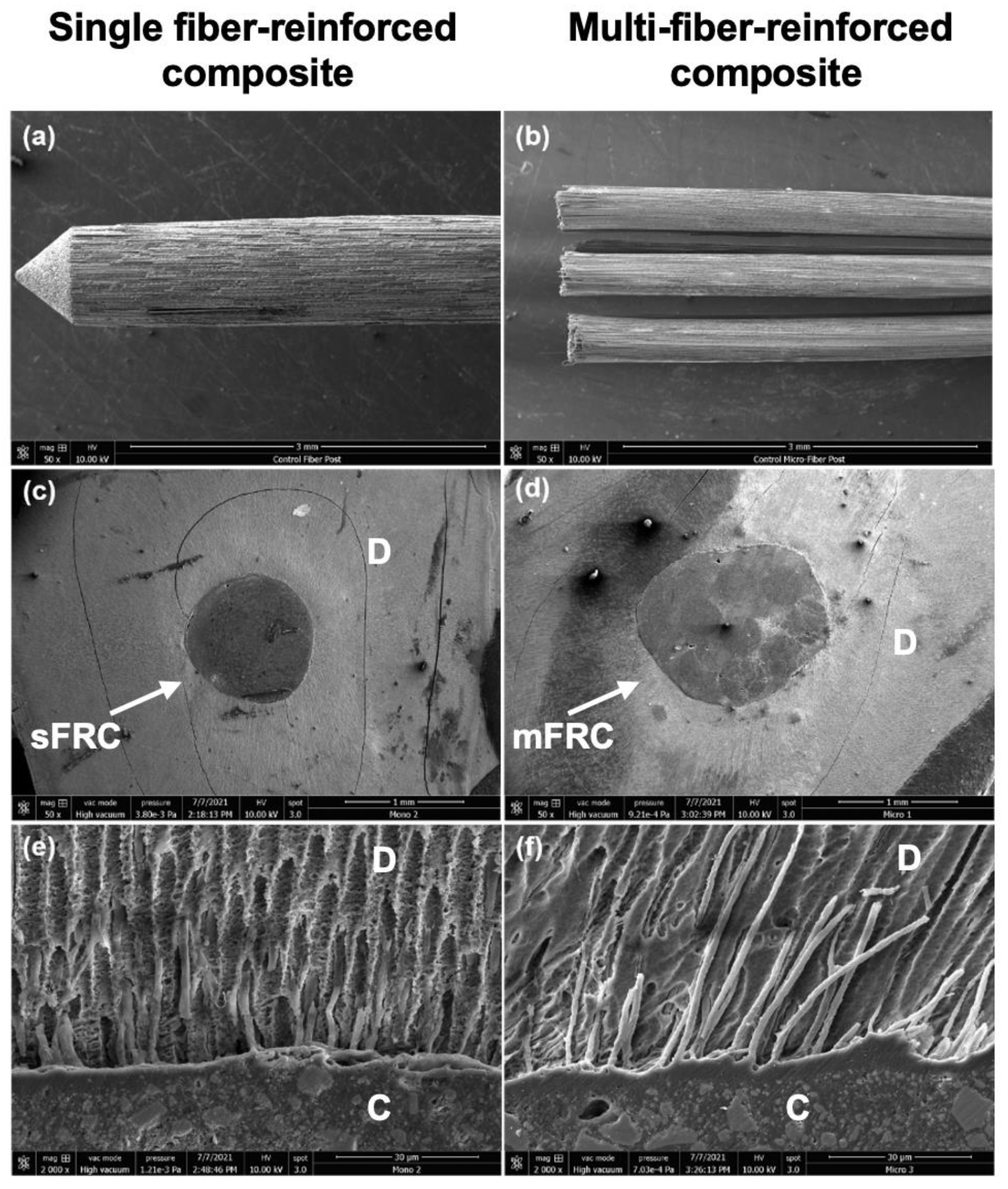
2.6. Scanning Electron Microscopy Observation (SEM)
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mancino, D.; Kharouf, N.; Cabiddu, M.; Bukiet, F.; Haïkel, Y. Microscopic and Chemical Evaluation of the Filling Quality of Five Obturation Techniques in Oval-Shaped Root Canals. Clin. Oral. Investig. 2021, 25, 3757–3765. [Google Scholar] [CrossRef] [PubMed]
- Kharouf, N.; Arntz, Y.; Eid, A.; Zghal, J.; Sauro, S.; Haikel, Y.; Mancino, D. Physicochemical and Antibacterial Properties of Novel, Premixed Calcium Silicate-Based Sealer Compared to Powder-Liquid Bioceramic Sealer. J. Clin. Med. 2020, 9, 3096. [Google Scholar] [CrossRef] [PubMed]
- Zarow, M.; Dominiak, M.; Szczeklik, K.; Hardan, L.; Bourgi, R.; Cuevas-Suárez, C.E.; Zamarripa-Calderón, J.E.; Kharouf, N.; Filtchev, D. Effect of Composite Core Materials on Fracture Resistance of Endodontically Treated Teeth: A Systematic Review and Meta-Analysis of In Vitro Studies. Polymers 2021, 13, 2251. [Google Scholar] [CrossRef]
- Bhandi, S.; Mashyakhy, M.; Abumelha, A.S.; Alkahtany, M.F.; Jamal, M.; Chohan, H.; Raj, A.T.; Testarelli, L.; Reda, R.; Patil, S. Complete Obturation—Cold Lateral Condensation vs. Thermoplastic Techniques: A Systematic Review of Micro-CT Studies. Materials 2021, 14, 4013. [Google Scholar] [CrossRef] [PubMed]
- Vire, D.E. Failure of endodontically treated teeth: Classification and evaluation. J. Endod. 1991, 17, 338–342. [Google Scholar] [CrossRef]
- Fuss, Z.; Lustig, J.; Tamse, A. Prevalence of vertical root fractures in extracted endodontically treated teeth. Int. Endod. J. 1999, 32, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Salehrabi, R.; Rotstein, I. Endodontic treatment outcomes in a large patient population in the USA: An epidemiological study. J. Endod. 2004, 30, 846–850. [Google Scholar] [CrossRef] [Green Version]
- Lazarski, M.P.; Walker, W.A., III; Flores, C.M.; Schindler, W.G.; Hargreaves, K.M. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J. Endod. 2001, 27, 791–796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tikku, A.P.; Chandra, A.; Bharti, R. Are full cast crowns mandatory after endodontic treatment in posterior teeth? J. Conserv. Dent. 2010, 13, 246–248. [Google Scholar] [CrossRef]
- Bonchev, A.; Radeva, E.; Tsvetanova, N. Fiber Reinforced Composite Posts-A Review of Literature. Int. J. Sci. Res. 2017, 6, 1887–1893. [Google Scholar]
- Ferrari, M.; Vichi, A.; Fadda, G.M.; Cagidiaco, M.C.; Tay, F.R.; Breschi, L.; Polimeni, A.; Goracci, C. A randomized controlled trial of endodontically treated and restored premolars. J. Dent. Res. 2012, 91, 72S–78S. [Google Scholar] [CrossRef]
- Ree, M.H.; Schwartz, R.S. Long-term Success of Nonvital, Immature Permanent Incisors Treated With a Mineral Trioxide Aggregate Plug and Adhesive Restorations: A Case Series from a Private Endodontic Practice. J. Endod. 2017, 43, 1370–1377. [Google Scholar] [CrossRef]
- Bhuva, B.; Giovarruscio, M.; Rahim, N.; Bitter, K.; Mannocci, F. The restoration of root filled teeth: A review of the clinical literature. Int. Endod. J. 2021, 54, 509–535. [Google Scholar] [CrossRef]
- Theodosopoulou, J.N.; Chochlidakis, K.M. A Systematic Review of Dowel (Post) and Core Materials and Systems. J. Prosthodont. 2009, 18, 464–472. [Google Scholar] [CrossRef]
- Gallo, J.R.; Miller, T.; Xu, X.; Burgess, J.O. In Vitro Evaluation of the Retention of Composite Fiber and Stainless Steel Posts. J. Prosthodont. 2002, 11, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Amarnath, G.S.; Swetha, M.U.; Muddugangadhar, B.C.; Sonika, R.; Garg, A.; Rao, T.R.P. Effect of Post Material and Length on Fracture Resistance of Endodontically Treated Premolars: An In-Vitro Study. J. Int. Oral. Health. 2015, 7, 22–28. [Google Scholar]
- Lamichhane, A.; Xu, C.; Zhang, F.Q. Dental fiber-post resin base material: A review. J. Adv. Prosthodont. 2014, 6, 60–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lemos Martins Sicuro, S.; Gabardo, M.C.L.; Castiglia Gonzaga, C.; Dias Morais, N.; Baratto-Filho, F.; Correr Nolasco, G.M.; Leonardi, D.P. Bond Strength of Self-Adhesive Resin Cement to Different Root Perforation Materials. J. Endod. 2016, 42, 1819–1821. [Google Scholar] [CrossRef] [PubMed]
- Novais, V.R.; Rodrigues, R.B.; Simamoto Júnior, P.C.; Lourenço, C.-S.; Soares, C.J. Correlation between the Mechanical Properties and Structural Characteristics of Different Fiber Posts Systems. Braz. Dent. J. 2016, 27, 46–51. [Google Scholar] [CrossRef] [Green Version]
- Bosso, K.; Gonini Júnior, A.; Guiraldo, R.D.; Berger, S.B.; Lopes, M.B. Stress Generated by Customized Glass Fiber Posts and Other Types by Photoelastic Analysis. Braz. Dent. J. 2015, 26, 222–227. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Shu, X.; Zhang, Y.; Yang, B.; Jian, Y.; Zhao, K. Evaluation of Fiber Posts vs Metal Posts for Restoring Severely Damaged Endodontically Treated Teeth: A Systematic Review and Meta-Analysis. Quintessence Int. 2019, 50, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Bitter, K.; Priehn, K.; Martus, P.; Kielbassa, A.M. In Vitro Evaluation of Push-out Bond Strengths of Various Luting Agents to Tooth-Colored Posts. J. Prosthet. Dent. 2006, 95, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Vichi, A.; Grandini, S.; Goracci, C. Efficacy of a Self-Curing Adhesive-Resin Cement System on Luting Glass-Fiber Posts into Root Canals: An SEM Investigation. Int. J. Prosthodont. 2001, 14, 543–549. [Google Scholar] [PubMed]
- Gomes, G.M.; Gomes, O.M.; Reis, A.; Gomes, J.C.; Loguercio, A.D.; Calixto, A.L. Effect of operator experience on the outcome of fiber post cementation with different resin cements. Oper. Dent. 2013, 38, 555–564. [Google Scholar] [CrossRef] [Green Version]
- Naumann, M.; Preuss, A.; Rosentritt, M. Effect of Incomplete Crown Ferrules on Load Capacity of Endodontically Treated Maxillary Incisors Restored with Fiber Posts, Composite Build-Ups, and All-Ceramic Crowns: An in Vitro Evaluation after Chewing Simulation. Acta Odontol. Scand. 2006, 64, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Sorrentino, R.; Juloski, J.; Grandini, S.; Carrabba, M.; Discepoli, N.; Ferrari Cagidiaco, E. Post-Retained Single Crowns versus Fixed Dental Prostheses: A 7-Year Prospective Clinical Study. J. Dent. Res. 2017, 96, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Richert, R.; Robinson, P.; Viguie, G.; Farges, J.-C.; Ducret, M. Multi-Fiber-Reinforced Composites for the Coronoradicular Reconstruction of Premolar Teeth: A Finite Element Analysis. Biomed. Res. Int. 2018, 2018, 4302607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santos, T.D.S.A.; Abu Hasna, A.; Abreu, R.T.; Tribst, J.P.M.; de Andrade, G.S.; Borges, A.L.S.; Torres, C.R.G.; Carvalho, C.A.T. Fracture resistance and stress distribution of weakened teeth reinforced with a bundled glass fiber-reinforced resin post. Clin. Oral. Investig. 2021, 1–12. [Google Scholar] [CrossRef]
- Braga, N.M.A.; Paulino, S.M.; Alfredo, E.; Sousa-Neto, M.D.; Vansan, L.P. Removal Resistance of Glass-Fiber and Metallic Cast Posts with Different Lengths. J. Oral. Sci. 2006, 48, 15–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomes, G.M.; Rezende, E.C.; Gomes, O.M.; Gomes, J.C.; Loguercio, A.D.; Reis, A. Influence of the Resin Cement Thickness on Bond Strength and Gap Formation of Fiber Posts Bonded to Root Dentin. J. Adhes. Dent. 2014, 16, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Kharouf, N.; Ashi, T.; Eid, A.; Maguina, L.; Zghal, J.; Sekayan, N.; Bourgi, R.; Hardan, L.; Sauro, S.; Haikel, Y.; et al. Does Adhesive Layer Thickness and Tag Length Influence Short/Long-Term Bond Strength of Universal Adhesive Systems? An In-Vitro Study. Appl. Sci. 2021, 11, 2635. [Google Scholar] [CrossRef]
- Kharouf, N.; Pedullà, E.; La Rosa, G.R.M.; Bukiet, F.; Sauro, S.; Haikel, Y.; Mancino, D. In Vitro Evaluation of Different Irrigation Protocols on Intracanal Smear Layer Removal in Teeth with or without Pre-Endodontic Proximal Wall Restoration. J. Clin. Med. 2020, 9, 3325. [Google Scholar] [CrossRef] [PubMed]
- Schneider, S.W. A comparison of canal preparations in straight and curved root canals. Oral. Surg. Oral. Med. Oral. Pathol. 1971, 32, 271–275. [Google Scholar] [CrossRef]
- Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Berry, T.P.; Watanabe, H.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Influence of Different Etching Modes on Bond Strength and Fatigue Strength to Dentin Using Universal Adhesive Systems. Dent. Mater. 2016, 32, e9–e21. [Google Scholar] [CrossRef] [PubMed]
- Farina, A.P.; Cecchin, D.; Garcia Lda, F.; Naves, L.Z.; Sobrinho, L.C.; Pires-de-Souza Fde, C. Bond strength of fiber posts in different root thirds using resin cement. J. Adhes. Dent. 2011, 13, 179–186. [Google Scholar] [PubMed]
- Zhang, W.; Suguro, H.; Kobayashi, Y.; Tsurumachi, T.; Ogiso, B. Effect of Canal Taper and Plugger Size on Warm Gutta-Percha Obturation of Lateral Depressions. J. Oral. Sci. 2011, 53, 219–224. [Google Scholar] [CrossRef] [Green Version]
- Uzun, İ.H.; Malkoç, M.A.; Keleş, A.; Öğreten, A.T. 3D Micro-CT Analysis of Void Formations and Push-out Bonding Strength of Resin Cements Used for Fiber Post Cementation. J. Adv. Prosthodont. 2016, 8, 101–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goracci, C.; Tavares, A.U.; Fabianelli, A.; Monticelli, F.; Raffaelli, O.; Cardoso, P.C.; Tay, F.; Ferrari, M. The Adhesion between Fiber Posts and Root Canal Walls: Comparison between Microtensile and Push-out Bond Strength Measurements. Eur. J. Oral. Sci. 2004, 112, 353–361. [Google Scholar] [CrossRef] [PubMed]
- do Nascimento Rechia, B.C.; Bravo, R.P.; de Oliveira, N.D.; Baratto Filho, F.; Gonzaga, C.C.; Storrer, C.L.M. Influence of Different Surface Treatments of Fiberglass Posts on the Bond Strength to Dentin. Braz. J. Oral. Sci. 2016, 15, 158–162. [Google Scholar] [CrossRef] [Green Version]
- Torbjorner, A.; Fransson, B. A literature review on the prosthetic treatment of structurally compromised teeth. J. Prosthodont. 2004, 17, 369–376. [Google Scholar]
- DeLong, R.; Douglas, W.H. Development of an artificial oral environment for the testing of dental restoratives: Bi-axial force and movement control. J. Dent. Res. 1983, 62, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Kharouf, N.; Eid, A.; Hardan, L.; Bourgi, R.; Arntz, Y.; Jmal, H.; Foschi, F.; Sauro, S.; Ball, V.; Haikel, Y.; et al. Antibacterial and Bonding Properties of Universal Adhesive Dental Polymers Doped with Pyrogallol. Polymers 2021, 13, 1538. [Google Scholar] [CrossRef] [PubMed]
- Hardan, L.; Bourgi, R.; Kharouf, N.; Mancino, D.; Zarow, M.; Jakubowicz, N.; Haikel, Y.; Cuevas-Suárez, C.E. Bond Strength of Universal Adhesives to Dentin: A Systematic Review and Meta-Analysis. Polymers 2021, 13, 814. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Machmouridou, E.; Watson, T.F.; Sauro, S.; Sherriff, M.; Pilecki, P.; Pitt-Ford, T.R. Microtensile bond strength of resin-post interfaces created with interpenetrating polymer network posts or cross-linked posts. Med. Oral. Patol. Oral. Cir. Bucal. 2008, 13, E745–E752. [Google Scholar] [PubMed]


| sFRC | mFRC | p < 0.05 | |
|---|---|---|---|
| Coronal (%) | 14.6 ± 9.4 | 5.8 ± 2.6 | Yes (p = 0.011) |
| Middle (%) | 4.2 ± 9.03 | 1.3 ± 3.2 | No (p = 0.356) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kharouf, N.; Sauro, S.; Jmal, H.; Eid, A.; Karrout, M.; Bahlouli, N.; Haikel, Y.; Mancino, D. Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal? Bioengineering 2021, 8, 195. https://doi.org/10.3390/bioengineering8120195
Kharouf N, Sauro S, Jmal H, Eid A, Karrout M, Bahlouli N, Haikel Y, Mancino D. Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal? Bioengineering. 2021; 8(12):195. https://doi.org/10.3390/bioengineering8120195
Chicago/Turabian StyleKharouf, Naji, Salvatore Sauro, Hamdi Jmal, Ammar Eid, Mohamed Karrout, Nadia Bahlouli, Youssef Haikel, and Davide Mancino. 2021. "Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal?" Bioengineering 8, no. 12: 195. https://doi.org/10.3390/bioengineering8120195
APA StyleKharouf, N., Sauro, S., Jmal, H., Eid, A., Karrout, M., Bahlouli, N., Haikel, Y., & Mancino, D. (2021). Does Multi-Fiber-Reinforced Composite-Post Influence the Filling Ability and the Bond Strength in Root Canal? Bioengineering, 8(12), 195. https://doi.org/10.3390/bioengineering8120195












