Recent Advances in AI-Driven Mobile Health Enhancing Healthcare—Narrative Insights into Latest Progress
Abstract
1. Introduction
1.1. Brief Story of Mhealth
1.2. Current State of AI in mHealth
- Current trends: What are the main trends in AI use across different mHealth domains, and how rapidly is the technology being integrated into everyday healthcare practices?
- Categorization and impact: How can AI applications in mHealth be categorized, and which types show the greatest promise for improving patient outcomes and enhancing healthcare efficiency?
- Opportunities and challenges: What are the main opportunities offered by AI, and what challenges—including regulatory, ethical, and implementation-related barriers—need to be addressed to ensure safe, equitable, and effective deployment?
1.3. Purpose of the Narrative Review
- Trends: Examine the evolution and current trends in AI use in mHealth, including key areas of application such as chronic disease management, telemedicine, and mental health.
- Categorization: Classify AI-based mobile health tools and interventions, identifying those that are most effective and those that are emerging.
- Opportunities and Challenges: Evaluate the opportunities AI offers for improving healthcare delivery and accessibility, and address key challenges, including data privacy, regulatory frameworks, and healthcare system integration.
2. Methods
2.1. Narrative Review Approach, Search Strategy, and Quality Assessment
2.1.1. Search Strategy, Study Selection, and Scope
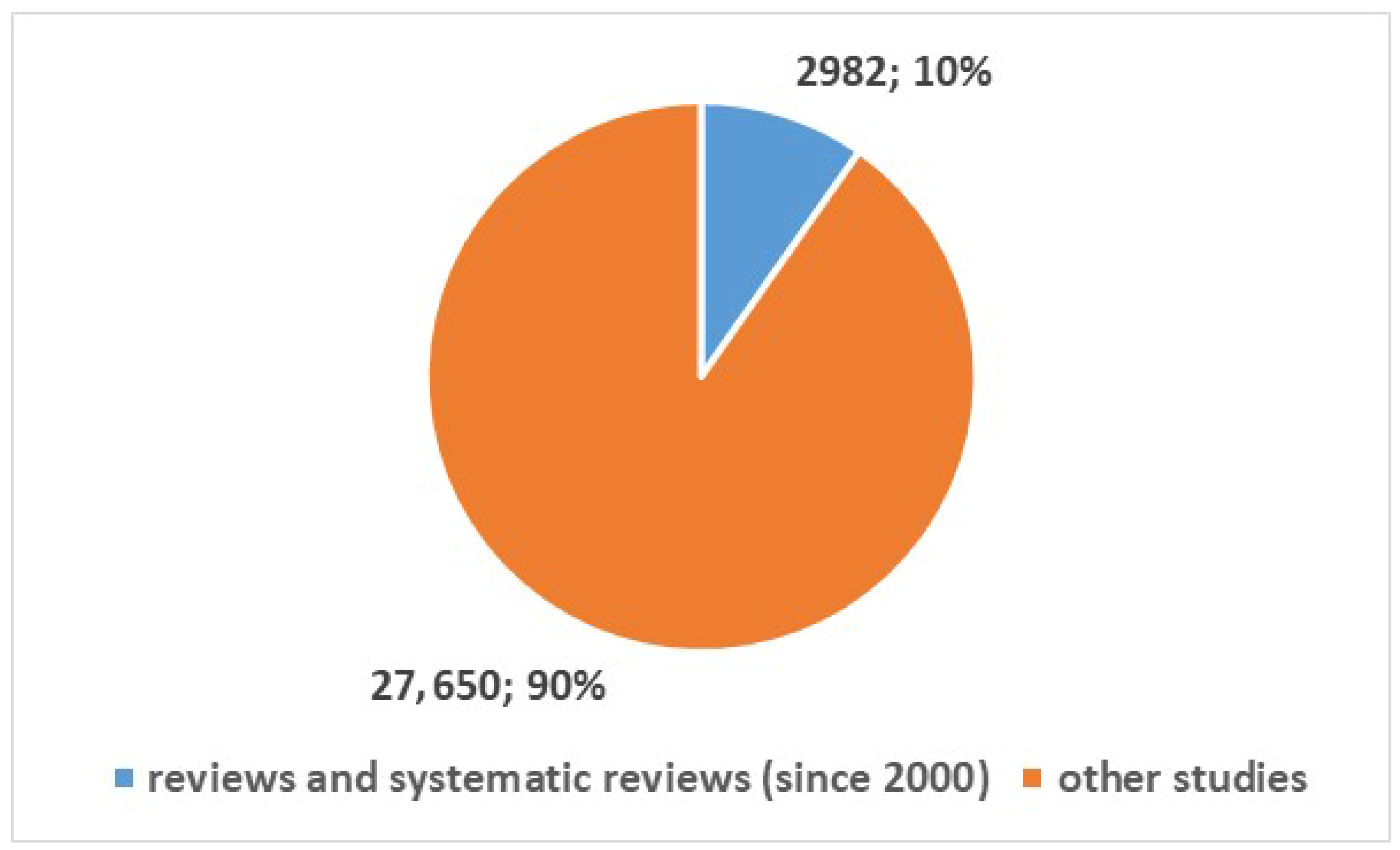
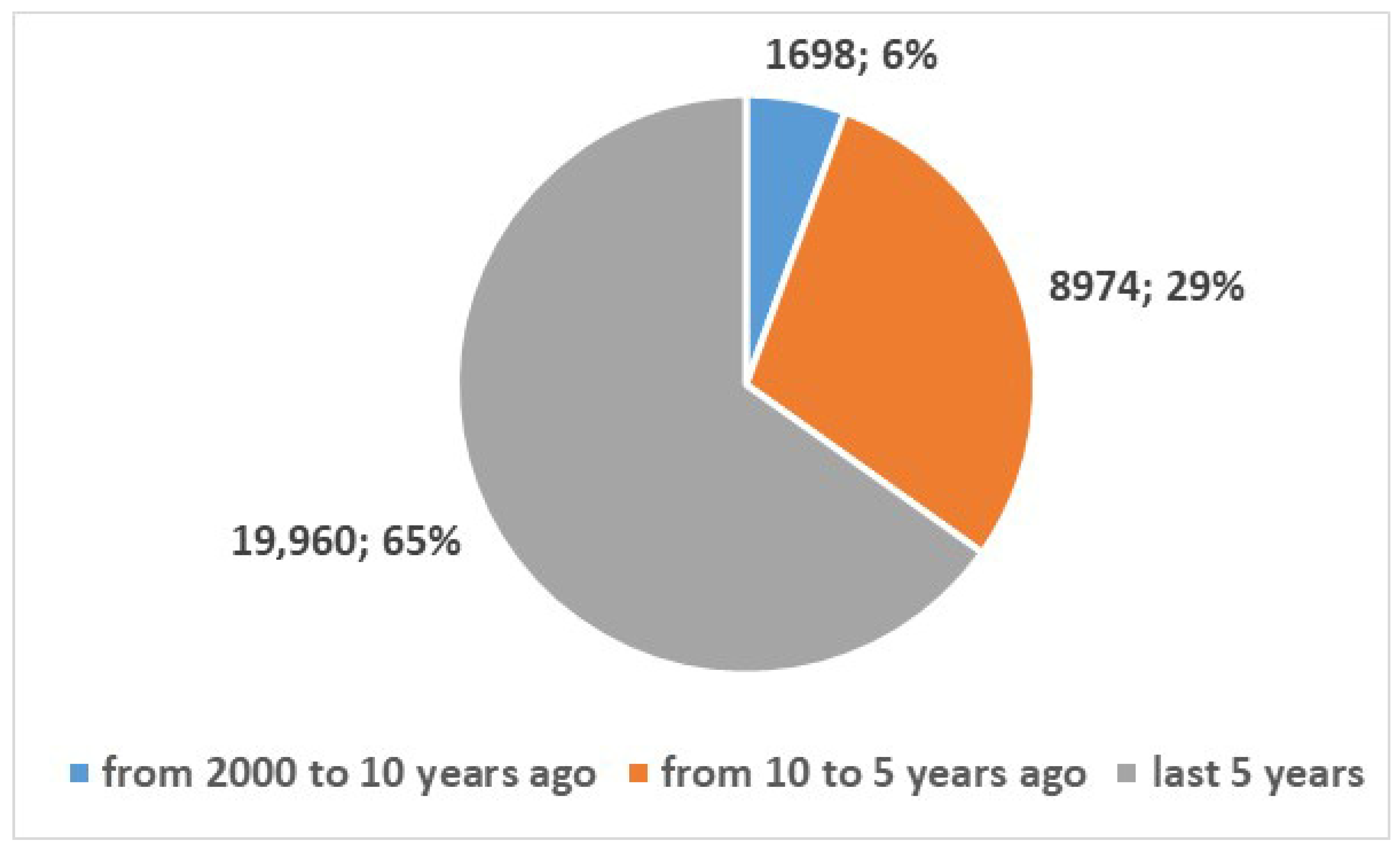
2.1.2. Selection and Qualification of Reviews
- 1.
- Define inclusion criteria
- ∘
- Primarily systematic reviews and meta-analyses were considered to ensure a high level of methodological rigor and robustness of evidence.
- ∘
- In addition, a limited number of non-systematic (narrative or scoping) reviews were included to capture emerging applications, innovative trends, and areas where systematic evidence is still limited.
- ∘
- Studies had to focus on clinical or healthcare applications of AI in mHealth, excluding purely technical or algorithmic works without tangible clinical outcomes.
- ∘
- Detailed inclusion/exclusion criteria are reported in Table 2.
- 2.
- Initial screening
- ∘
- Titles and abstracts were screened independently by two reviewers.
- ∘
- Studies irrelevant to clinical mHealth applications, such as purely computational benchmarks or software architecture reports, were excluded.
- 3.
- Evaluation parametersEach study was assessed using six core parameters:
- ∘
- N1: Clear rationale—The study clearly explains the background, objectives, and significance.
- ∘
- N2: Adequate research design—Methodology is appropriate to answer the research question.
- ∘
- N3: Clearly described methodology—Data collection, analysis, and interpretation are transparent and replicable.
- ∘
- N4: Well-presented results—Results are clearly described, with tables, figures, or statistical analysis supporting conclusions.
- ∘
- N5: Conclusions justified by results—Conclusions are evidence-based and logically derived.
- ∘
- N6: Disclosure of conflicts of interest—Conflicts of interest are explicitly reported.
- 4.
- Scoring system
- ∘
- N1–N5 were scored on a 1–5 scale (1 = poor, 5 = excellent).
- ∘
- N6 was assessed as Yes/No (Yes = disclosed; No = not disclosed).
- 5.
- Preselection of studies
- ∘
- Only studies with N1–N5 > 3 and N6 = Yes were preselected.
- ∘
- This ensured inclusion of methodologically robust studies with transparency in conflicts of interest.
- 6.
- Final synthesis
- ∘
- Preselected studies were included in the narrative synthesis, providing a clinically focused overview of trends, categories, and challenges in AI-driven mHealth.
- ∘
- The synthesis emphasized post-pandemic developments, highlighting how technological innovation intersects with practical healthcare applications.
2.2. Screening Team and Reliability Assessment
- For N1–N5, a 5-point scale was applied: 1 = Poor, 2 = Fair, 3 = Good, 4 = Very Good, 5 = Excellent.
- N6 was assessed binary (Yes/No), depending on whether conflicts of interest were explicitly disclosed.
3. Results
3.1. Study Selection Flow
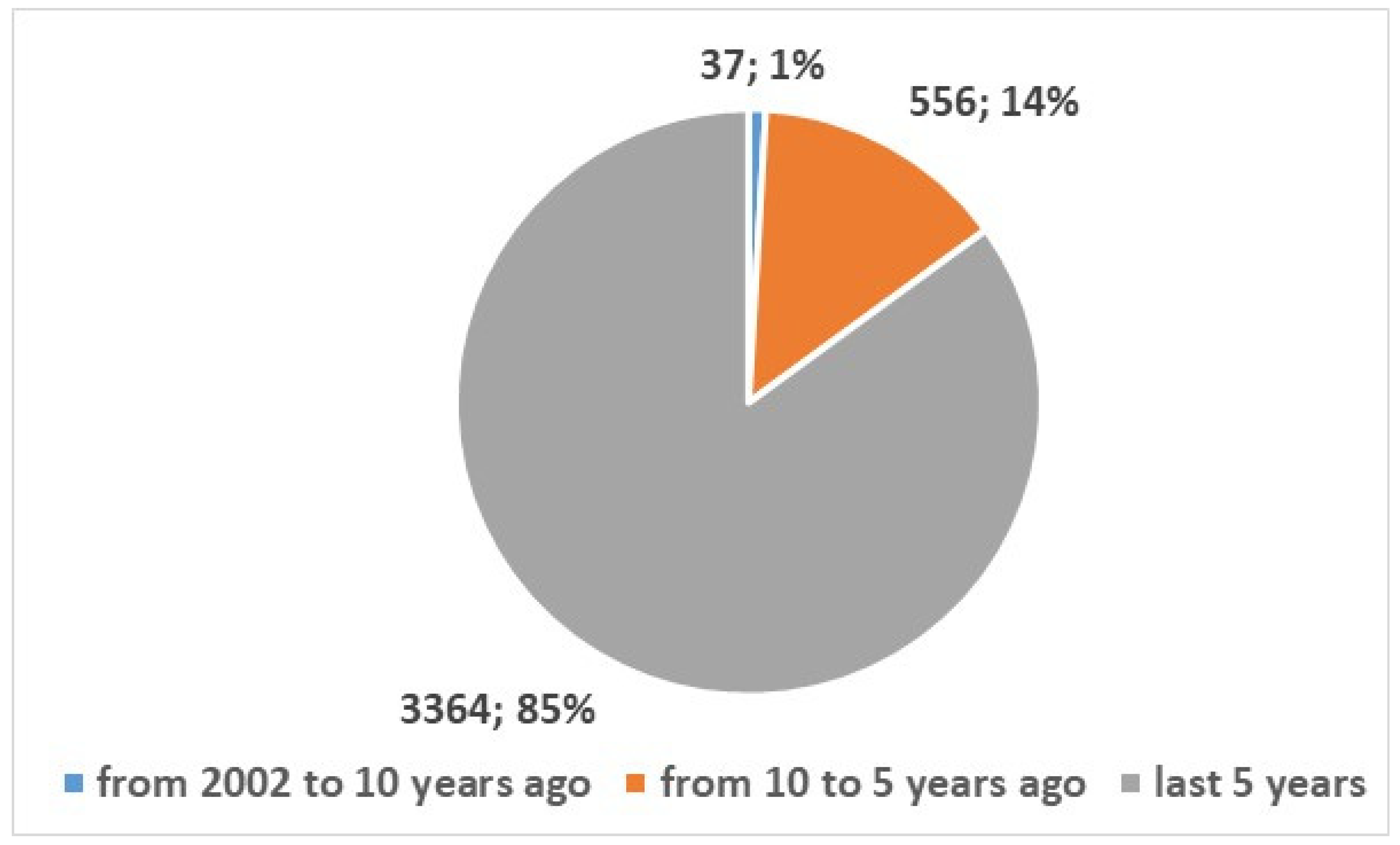
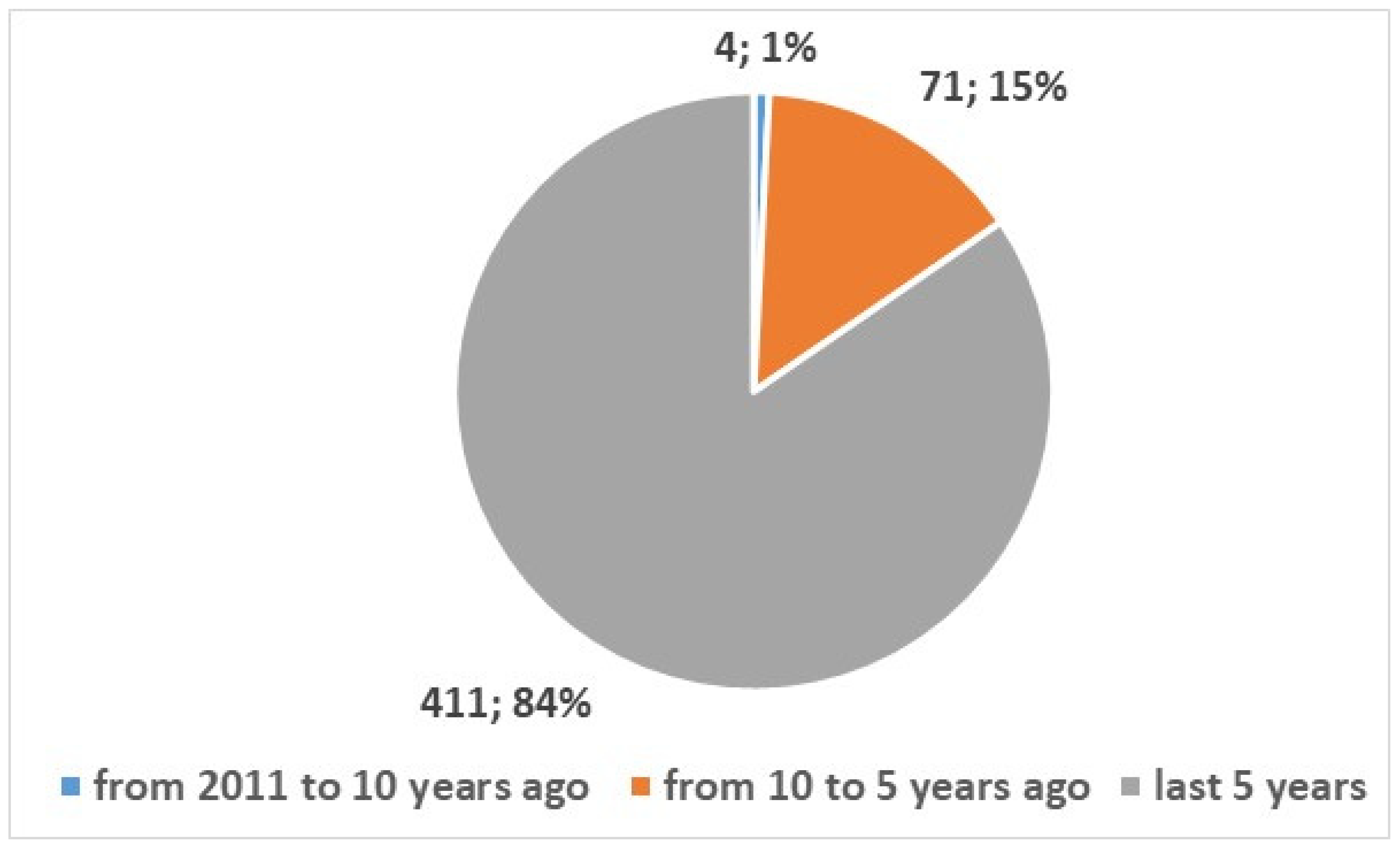
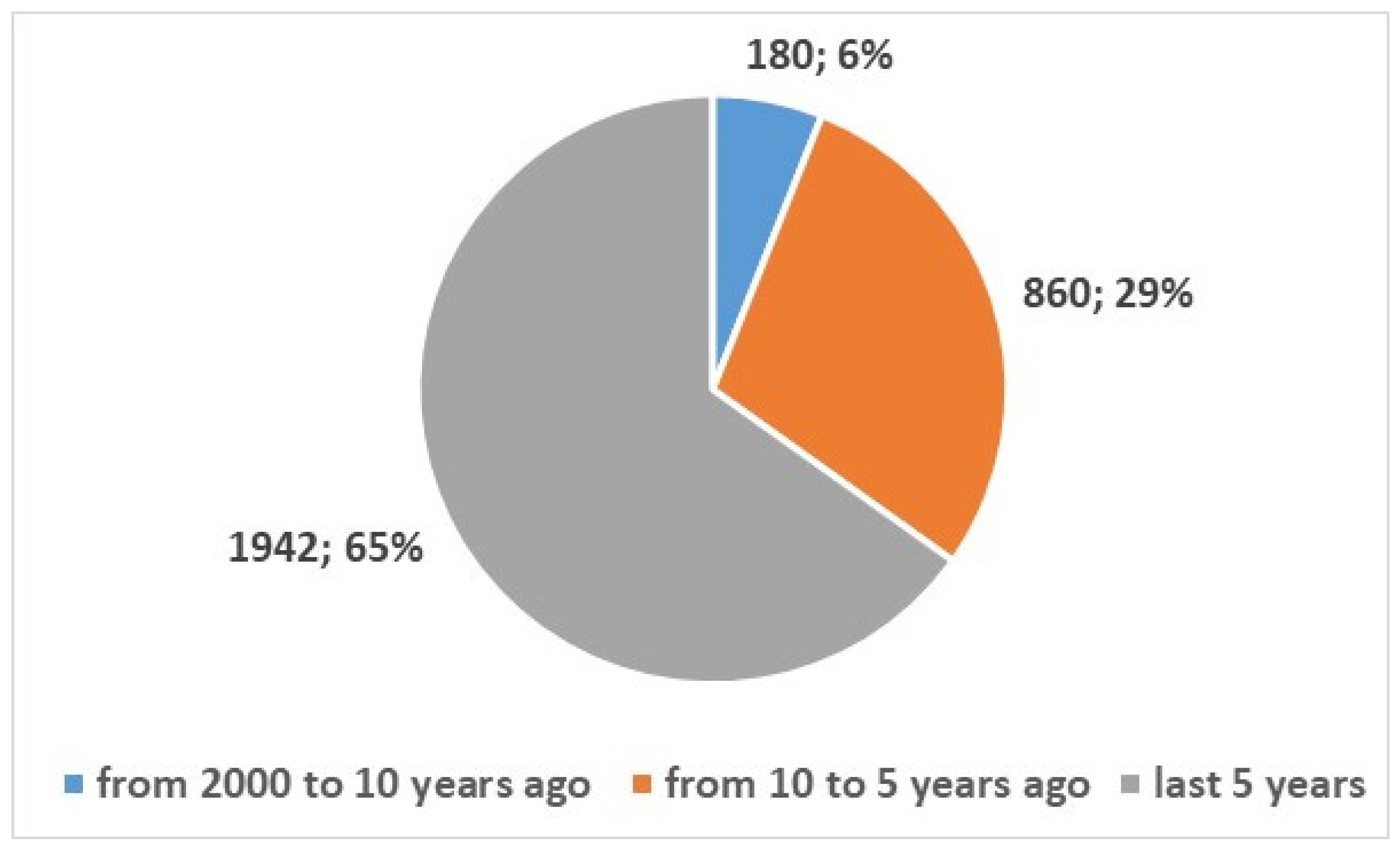
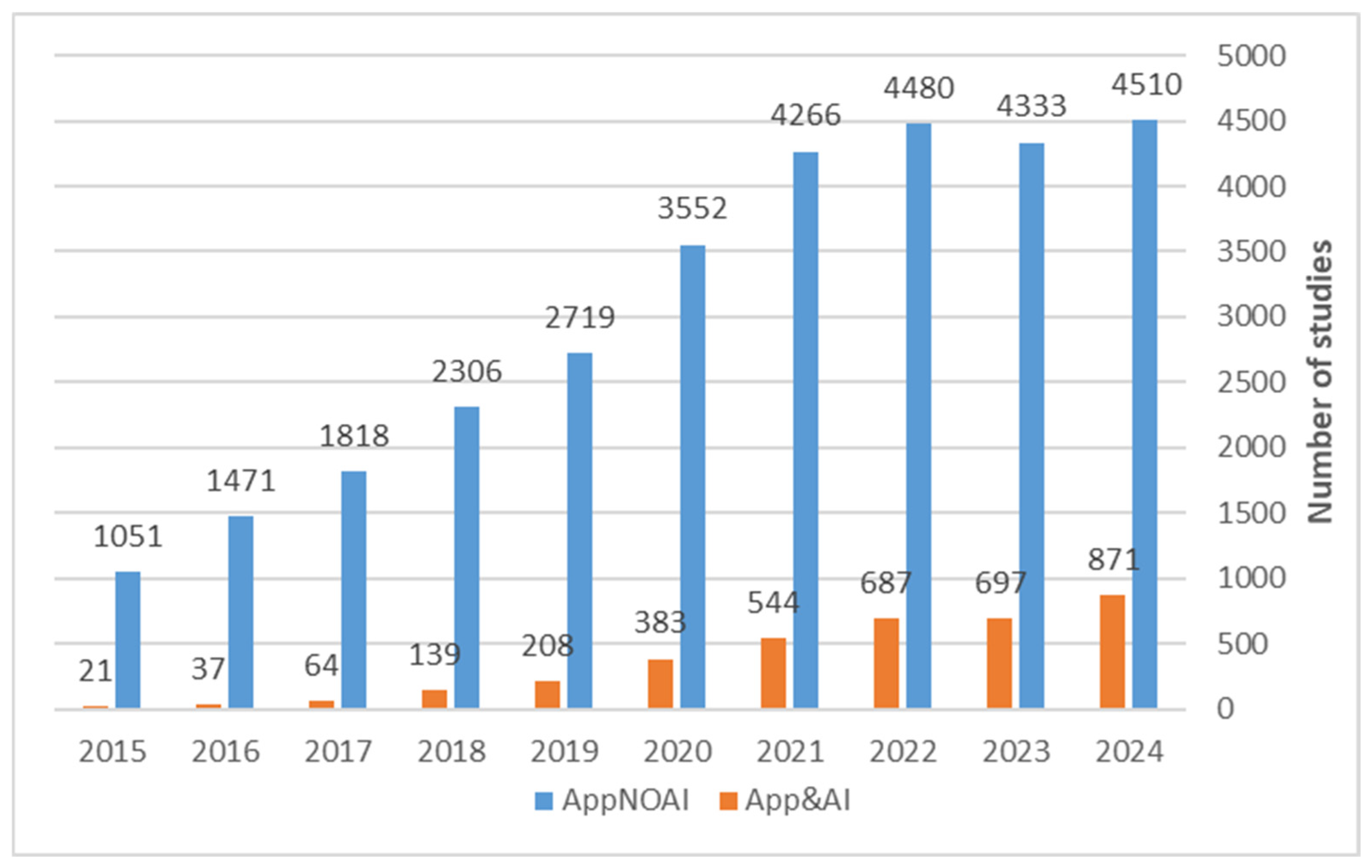
3.2. Research Trends in Mobile Apps and Their Use of Artificial Intelligence
3.3. Output from the Overview: Common Message, Themes and Categorization
- Macro Area: The broad healthcare category where AI and mHealth applications have been applied.
- Number of Included Studies: Total studies contributing to each macro-area, allowing a quick assessment of research volume.
- Evidence Maturity Level: Qualitative assessment of research maturity (e.g., emerging, developing, mature) based on the number and quality of studies.
- Typical Interventions/Focus: Provides a brief summary (1–2 sentences) of the typical interventions, aims, or contributions of the studies in that macro-area.
- Notes/Research Gaps: Highlights areas with limited evidence or underexplored topics, guiding directions for future investigation.
- Key Studies [ ]: Lists the included studies for each macro-area using numerical references corresponding to the reference list.
- Workplace Health: AI-based interventions to promote employee health and prevent disease [28].
- Technology for Medication Adherence: mHealth apps improving adherence to treatments, particularly in oncology [29].
- Nutrition & Health: Mobile apps supporting nutrition management and healthier behaviors [34].
- Surgical Care & Infections: Data-driven technologies preventing surgical site infections [54].
- Medical Informatics: Telehealth startups enhancing healthcare delivery and access [53].
3.4. Opportunities and Areas Needing Broader Investigation
4. Discussion
4.1. Summary of Key Findings
4.2. Comparison with Prior Evidence
4.3. Exploring Clinical and Policy Implications
4.4. Exploring the Regulatory Landscape Surrounding AI-Powered Mobile Health Apps
4.4.1. Characteristics of the AI-Based App Concerning Medical Device Regulation
- -
- Transparency of algorithms (known as ‘black boxes’), which do not allow clinicians to understand or verify the decisions made by the algorithm;
- -
- Effectiveness, since unlike traditional software, artificial intelligence systems can change their behaviour over time, which can lead to unnecessary treatments or missed diagnoses;
- -
- Depending on the input data, there is a risk of bias if the training data has not been diversified;
- -
- Data security and privacy, as there is a risk of accidental data loss and cyberattacks;
- -
- Regulatory and legal uncertainty, as the regulatory frameworks of various countries are still evolving.
4.4.2. Characteristics of the AI-Based App Concerning AI Regulation
- Robustness and safety: AI systems must operate reliably and safely.
- Privacy and security: AI systems must respect privacy (mandatory information on how data are collected, used, and stored.) and must be secure (system access and data encryption to ensure data quality and integrity).
- Transparency and explainability: AI operations must be understandable to users and stakeholders, from training on the data and algorithms to generating the final model.
- Fairness and inclusiveness: AI outcomes must avoid bias and discrimination toward or against certain groups of people.
- Accountability: There must be clear responsibilities for the results of the AI system, such as to the developers who design and deploy the AI system.
4.5. Quality Aspects in AI & Apps
4.5.1. Policy and Global Strategies
4.5.2. Clinical Evidence and Effectiveness
- Mental health interventions: Apps delivering mindfulness, cognitive behavioral therapy (CBT), or stress reduction programs improve well-being, reduce anxiety and depressive symptoms, and enhance coping skills [110,111]. Integration of AI-driven personalization allows dynamic adaptation of content, reminders, and exercises based on individual user progress, engagement patterns, and risk profiles.
- Chronic disease management: Diabetes, hypertension, and cardiovascular apps facilitate lifestyle modification, medication adherence, and biometric monitoring, demonstrating improvements in glycemic control, blood pressure, and symptom management [112,113,114]. AI models can identify early deviations from expected health parameters, alert patients and clinicians, and recommend timely interventions.
- Oncology care: Mobile apps support cancer survivors in self-management, symptom tracking, and psychological support, improving quality of life and reducing stress [115,116]. Predictive analytics enable anticipation of side effects or disease progression, allowing personalized follow-up schedules and care adjustments.
- Respiratory disease support: Asthma and COPD apps enhance adherence, track inhaler usage, and provide environmental alerts [117]. AI personalization can optimize medication timing, offer actionable recommendations, and support behavior change interventions to reduce exacerbations.
4.5.3. Economic Evidence and System-Level Impact
4.5.4. Adoption and Usability
- Clinician adoption: Healthcare providers consider usability, evidence of clinical effectiveness, integration with electronic health records, and compatibility with existing workflows [121]. AI recommendations must be transparent, interpretable, and explainable to gain trust and support clinical decision-making.
- Patient uptake: Sociotechnical factors—such as digital literacy, engagement strategies, trust in data handling, and behavioral design—affect sustained use [122]. Personalized notifications, gamification, and interactive feedback can improve adherence.
4.5.5. App Assessment Frameworks and Standardization
- European mHealth Hub: Offers comprehensive guidelines to assess app features, clinical validation, usability, and cybersecurity [127].
- CEN ISO/TS 82304-2: Internationally recognized criteria cover safety, effectiveness, interoperability, engagement, and transparency, supporting consistent and reproducible evaluation [128].
4.6. Technical Standards and Norms for AI-Powered Health Apps
4.6.1. ISO and IEC Standards
4.6.2. Health IT and Interoperability Standards
4.6.3. AI-Specific Guidelines and Regulatory Alignment
4.6.4. Quality Assessment, Certification, and Continuous Monitoring
4.7. The Regulatory Gray Zone and AI-Specific Advantages in mHealth
4.7.1. The Regulatory Gray Zone in mHealth Applications
4.7.2. AI-Specific Advantages vs. Traditional mHealth Tools
- Real-time Pattern Recognition and Anomaly DetectionAI algorithms can analyze continuous streams of patient data to detect subtle anomalies that human observers or traditional apps may miss. For example, in diabetes management, AI-enabled apps can monitor glucose trends and detect patterns predicting hyperglycemia or hypoglycemia, allowing for early interventions [112,114]. Similarly, AI can identify early signs of cardiac arrhythmias from wearable ECG data, outperforming rule-based alerts provided by standard apps.
- Personalization Based on Individual DataUnlike conventional mHealth tools, AI can tailor interventions to each user’s unique physiology, behavior, and health history. In oncology, AI-driven apps can provide individualized medication reminders and lifestyle recommendations for breast cancer survivors [115,116]. In mental health, AI chatbots can adapt counseling content based on real-time mood assessments, optimizing engagement and efficacy [96,98].
- Predictive Modeling and Risk StratificationAI supports predictive analytics, allowing clinicians and patients to anticipate future health events. For example, AI tools can stratify cardiovascular risk by integrating patient demographics, lab results, and lifestyle data, guiding preventive interventions [115,117]. Predictive modeling can also prioritize high-risk patients for early monitoring, reducing hospitalizations and healthcare costs.
- Natural Language Processing for Symptom AssessmentAI-powered natural language processing (NLP) enables apps to interpret unstructured patient-reported information. Chatbots and digital symptom checkers can understand patient inputs in free text, detect critical symptoms, and triage patients appropriately [96,98]. This functionality is particularly valuable in mental health, where subjective symptom reporting is crucial.
4.7.3. Implications for Practice and Policy
4.8. Limitations
4.9. Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Giansanti, D.; Maccioni, G.; Grigioni, M. Biotelemetry for monitoring the quality of life of pets: What has changed since Laika? Not. Ist. Super. Sanità 2017, 30, 3–8. (In Italian) [Google Scholar]
- Available online: https://biotelemetry.yolasite.com/history.php (accessed on 28 July 2025).
- Available online: https://airandspace.si.edu/stories/editorial/inventing-apollo-spaceflight-biomedical-sensors (accessed on 28 July 2025).
- Bonato, P. Wearable sensors/systems and their impact on biomedical engineering. IEEE Eng. Med. Boil. Mag. 2003, 22, 18–20. [Google Scholar] [CrossRef]
- Available online: https://www.arrow.com/en/research-and-events/articles/smartphone-history-from-the-first-smartphone-to-today (accessed on 28 July 2025).
- Fiordelli, M.; Diviani, N.; Schulz, P.J. Mapping mHealth research: A decade of evolution. J. Med. Internet Res. 2013, 15, e95. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hobson, G.R.; Caffery, L.J.; Neuhaus, M.; Langbecker, D.H. Mobile Health for First Nations Populations: Systematic Review. JMIR Mhealth Uhealth 2019, 7, e14877. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Holl, F.; Schobel, J.; Swoboda, W.J. Mobile Apps for COVID-19: A Systematic Review of Reviews. Healthcare 2024, 12, 139. [Google Scholar] [CrossRef]
- Mansouri, F.; Darvishpour, A. Mobile Health Applications in the COVID-19 Pandemic: A Scoping Review of the Reviews. Med. J. Islam. Repub. Iran 2023, 37, 8. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maccioni, G.; Giansanti, D. Medical Apps and the Gray Zone in the COVID-19 Era: Between Evidence and New Needs for Cybersecurity Expansion. Healthcare 2021, 9, 430. [Google Scholar] [CrossRef] [PubMed]
- Dabla, P.K.; Gruson, D.; Gouget, B.; Bernardini, S.; Homsak, E. Lessons Learned from the COVID-19 Pandemic: Emphasizing the Emerging Role and Perspectives from Artificial Intelligence, Mobile Health, and Digital Laboratory Medicine. eJIFCC 2021, 32, 224–243. [Google Scholar] [PubMed] [PubMed Central]
- Alkasassbeh, J.S.; Alawneh, T.A.; Al-Qaisi, A.; Altarawneh, M.; alja’fari, M. The Role of AI in Mobile Apps to Combat Future Pandemics: A COVID-19 Case Study. In Proceedings of the 2023 2nd International Engineering Conference on Electrical, Energy, and Artificial Intelligence (EICEEAI), Zarqa, Jordan, 27–28 December 2023; pp. 1–8. [Google Scholar] [CrossRef]
- Shahroz, M.; Ahmad, F.; Younis, M.S.; Ahmad, N.; Kamel Boulos, M.N.; Vinuesa, R.; Qadir, J. COVID-19 digital contact tracing applications and techniques: A review post initial deployments. Transp. Eng. 2021, 5, 100072. [Google Scholar] [CrossRef]
- Huang, J.A.; Hartanti, I.R.; Colin, M.N.; Pitaloka, D.A. Telemedicine and artificial intelligence to support self-isolation of COVID-19 patients: Recent updates and challenges. Digit. Health 2022, 8, 20552076221100634. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Solimini, R.; Busardò, F.P.; Gibelli, F.; Sirignano, A.; Ricci, G. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina 2021, 57, 1314. [Google Scholar] [CrossRef]
- Kritikos, M. Artificial Intelligence (AI) in a Time of Pandemics: Developing Options for the Ethical Governance of COVID-19 AI Applications. In Ethics, Integrity and Policymaking: The Value of the Case Study; Chapter 13; O’Mathúna, D., Iphofen, R., Eds.; Springer: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- Lastrucci, A.; Pirrera, A.; Lepri, G.; Giansanti, D. Algorethics in Healthcare: Balancing Innovation and Integrity in AI Development. Algorithms 2024, 17, 432. [Google Scholar] [CrossRef]
- Singareddy, S.; Sn, V.P.; Jaramillo, A.P.; Yasir, M.; Iyer, N.; Hussein, S.; Nath, T.S. Artificial Intelligence and Its Role in the Management of Chronic Medical Conditions: A Systematic Review. Cureus 2023, 15, e46066. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, X.; Ma, L.; Sun, D.; Yi, M.; Wang, Z. Artificial Intelligence in Telemedicine: A Global Perspective Visualization Analysis. Telemed. e Health 2024, 30, e1909–e1922. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, D.; Morelli, S. Exploring the Potential of Digital Twins in Cancer Treatment: A Narrative Review of Reviews. J. Clin. Med. 2025, 14, 3574. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Hung, C.; Katapally, T.R. Evaluating predictive artificial intelligence approaches used in mobile health platforms to forecast mental health symptoms among youth: A systematic review. Psychiatry Res. 2024, 343, 116277. [Google Scholar] [CrossRef] [PubMed]
- Manyazewal, T.; Davey, G.; Hanlon, C.; Newport, M.J.; Hopkins, M.; Wilburn, J.; Bakhiet, S.; Mutesa, L.; Semahegn, A.; Assefa, E.; et al. Innovative technologies to address neglected tropical diseases in African settings with persistent sociopolitical instability. Nat. Commun. 2024, 15, 10274. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Thakuria, T.; Rahman, T.; Mahanta, D.R.; Khataniar, S.K.; Goswami, R.D.; Rahman, T.; Mahanta, L.B. Deep learning for early diagnosis of oral cancer via smartphone and DSLR image analysis: A systematic review. Expert Rev. Med. Dev. 2024, 21, 1189–1204. [Google Scholar] [CrossRef] [PubMed]
- Förstel, M.; Haas, O.; Förstel, S.; Maier, A.; Rothgang, E. A Systematic Review of Features Forecasting Patient Arrival Numbers. Comput. Inform. Nurs. 2024, 43, e01197. [Google Scholar] [CrossRef] [PubMed]
- Chau, R.C.; Thu, K.M.; Hsung, R.T.; McGrath, C.; Lam, W.Y. Self-monitoring of Oral Health Using Smartphone Selfie Powered by Artificial Intelligence: Implications for Preventive Dentistry. Oral Health Prev. Dent. 2024, 22, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Zhang, Y.; Ye, B.; Babineau, J.; Zhao, Y.; Gao, Z.; Mihailidis, A. Smartphone-Based Hand Function Assessment: Systematic Review. J. Med. Internet Res. 2024, 26, e51564. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Negi, S.; Mathur, A.; Tripathy, S.; Mehta, V.; Snigdha, N.T.; Adil, A.H.; Karobari, M.I. Artificial Intelligence in Dental Caries Diagnosis and Detection: An Umbrella Review. Clin. Exp. Dent. Res. 2024, 10, e70004. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lange, M.; Löwe, A.; Kayser, I.; Schaller, A. Approaches for the Use of AI in Workplace Health Promotion and Prevention: Systematic Scoping Review. JMIR AI 2024, 3, e53506. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chow, S.M.; Tan, B.K. Effectiveness of mHealth apps on adherence and symptoms to oral anticancer medications: A systematic review and meta-analysis. Support Care Cancer 2024, 32, 426. [Google Scholar] [CrossRef] [PubMed]
- Jin, K.; Li, Y.; Wu, H.; Tham, Y.C.; Koh, V.; Zhao, Y.; Kawasaki, R.; Grzybowski, A.; Ye, J. Integration of smartphone technology and artificial intelligence for advanced ophthalmic care: A systematic review. Adv. Ophthalmol. Pract. Res. 2024, 4, 120–127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Choi, A.; Ooi, A.; Lottridge, D. Digital Phenotyping for Stress, Anxiety, and Mild Depression: Systematic Literature Review. JMIR Mhealth Uhealth 2024, 12, e40689. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Segur-Ferrer, J.; Moltó-Puigmartí, C.; Pastells-Peiró, R.; Vivanco-Hidalgo, R.M. Methodological Frameworks and Dimensions to Be Considered in Digital Health Technology Assessment: Scoping Review and Thematic Analysis. J. Med. Internet Res. 2024, 26, e48694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giunti, G.; Doherty, C.P. Cocreating an Automated mHealth Apps Systematic Review Process with Generative AI: Design Science Research Approach. JMIR Med. Educ. 2024, 10, e48949. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pala, D.; Petrini, G.; Bosoni, P.; Larizza, C.; Quaglini, S.; Lanzola, G. Smartphone applications for nutrition Support: A systematic review of the target outcomes and main functionalities. Int. J. Med. Inform. 2024, 184, 105351. [Google Scholar] [CrossRef] [PubMed]
- Jahan, E.; Almansour, R.; Ijaz, K.; Baptista, S.; Giordan, L.B.; Ronto, R.; Zaman, S.; O’Hagan, E.; Laranjo, L. Smartphone Applications to Prevent Type 2 Diabetes: A Systematic Review and Meta-Analysis. Am. J. Prev. Med. 2024, 66, 1060–1070. [Google Scholar] [CrossRef] [PubMed]
- Gheisari, M.; Ghaderzadeh, M.; Li, H.; Taami, T.; Fernández-Campusano, C.; Sadeghsalehi, H.; Afzaal Abbasi, A. Mobile Apps for COVID-19 Detection and Diagnosis for Future Pandemic Control: Multidimensional Systematic Review. JMIR Mhealth Uhealth 2024, 12, e44406, Erratum in JMIR Mhealth Uhealth 2024, 12, e58810. https://doi.org/10.2196/58810. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tomlin, H.R.; Wissing, M.; Tanikella, S.; Kaur, P.; Tabas, L. Challenges and Opportunities for Professional Medical Publications Writers to Contribute to Plain Language Summaries (PLS) in an AI/ML Environment—A Consumer Health Informatics Systematic Review. AMIA Annu. Symp. Proc. 2024, 2023, 709–717. [Google Scholar] [PubMed] [PubMed Central]
- Xue, J.; Zhang, B.; Zhao, Y.; Zhang, Q.; Zheng, C.; Jiang, J.; Li, H.; Liu, N.; Li, Z.; Fu, W.; et al. Evaluation of the Current State of Chatbots for Digital Health: Scoping Review. J. Med. Internet Res. 2023, 25, e47217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- He, X.; Zheng, X.; Ding, H. Existing Barriers Faced by and Future Design Recommendations for Direct-to-Consumer Health Care Artificial Intelligence Apps: Scoping Review. J. Med. Internet Res. 2023, 25, e50342. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sumner, J.; Lim, H.W.; Chong, L.S.; Bundele, A.; Mukhopadhyay, A.; Kayambu, G. Artificial intelligence in physical rehabilitation: A systematic review. Artif. Intell. Med. 2023, 146, 102693. [Google Scholar] [CrossRef] [PubMed]
- Bendotti, H.; Lawler, S.; Chan, G.C.K.; Gartner, C.; Ireland, D.; Marshall, H.M. Conversational artificial intelligence interventions to support smoking cessation: A systematic review and meta-analysis. Digit. Health 2023, 9, 20552076231211634. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pyper, E.; McKeown, S.; Hartmann-Boyce, J.; Powell, J. Digital Health Technology for Real-World Clinical Outcome Measurement Using Patient-Generated Data: Systematic Scoping Review. J. Med. Internet Res. 2023, 25, e46992. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hasan, S.U.; Siddiqui, M.A.R. Diagnostic accuracy of smartphone-based artificial intelligence systems for detecting diabetic retinopathy: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2023, 205, 110943. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, A.; Prinz, A.; Riegler, M.A.; Das, J. A systematic review and knowledge mapping on ICT-based remote and automatic COVID-19 patient monitoring and care. BMC Health Serv. Res. 2023, 23, 1047. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fegan, H.; Hutchinson, R. Is the answer to reducing early childhood caries in your pocket? Evid. Based Dent. 2023, 24, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Koumpouros, Y.; Georgoulas, A. Pain Management Mobile Applications: A Systematic Review of Commercial and Research Efforts. Sensors 2023, 23, 6965. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Duarte, M.; Pereira-Rodrigues, P.; Ferreira-Santos, D. The Role of Novel Digital Clinical Tools in the Screening or Diagnosis of Obstructive Sleep Apnea: Systematic Review. J. Med. Internet Res. 2023, 25, e47735. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, X.; Martinengo, L.; Jabir, A.I.; Ho, A.H.Y.; Car, J.; Atun, R.; Tudor Car, L. Scope, Characteristics, Behavior Change Techniques, and Quality of Conversational Agents for Mental Health and Well-Being: Systematic Assessment of Apps. J. Med. Internet Res. 2023, 25, e45984. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moharrami, M.; Farmer, J.; Singhal, S.; Watson, E.; Glogauer, M.; Johnson, A.E.W.; Schwendicke, F.; Quinonez, C. Detecting dental caries on oral photographs using artificial intelligence: A systematic review. Oral Dis. 2024, 30, 1765–1783. [Google Scholar] [CrossRef] [PubMed]
- Piendel, L.; Vališ, M.; Hort, J. An update on mobile applications collecting data among subjects with or at risk of Alzheimer’s disease. Front. Aging Neurosci. 2023, 15, 1134096. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lam, W.W.T.; Tang, Y.M.; Fong, K.N.K. A systematic review of the applications of markerless motion capture (MMC) technology for clinical measurement in rehabilitation. J. Neuroeng. Rehabil. 2023, 20, 57. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sumra, M.; Asghar, S.; Khan, K.S.; Fernández-Luna, J.M.; Huete, J.F.; Bueno-Cavanillas, A. Smartphone Apps for Domestic Violence Prevention: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 5246. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chakraborty, I.; Edirippulige, S.; Vigneswara Ilavarasan, P. The role of telehealth startups in healthcare service delivery: A systematic review. Int. J. Med. Inform. 2023, 174, 105048. [Google Scholar] [CrossRef] [PubMed]
- Irgang, L.; Barth, H.; Holmén, M. Data-Driven Technologies as Enablers for Value Creation in the Prevention of Surgical Site Infections: A Systematic Review. J. Healthc. Inform. Res. 2023, 7, 1–41. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Torres-Guzman, R.A.; Paulson, M.R.; Avila, F.R.; Maita, K.; Garcia, J.P.; Forte, A.J.; Maniaci, M.J. Smartphones and Threshold-Based Monitoring Methods Effectively Detect Falls Remotely: A Systematic Review. Sensors 2023, 23, 1323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Eijck, S.C.; Janssen, D.M.; van der Steen, M.C.; Delvaux, E.J.L.G.; Hendriks, J.G.E.; Janssen, R.P.A. Digital Health Applications to Establish a Remote Diagnosis of Orthopedic Knee Disorders: Scoping Review. J. Med. Internet Res. 2023, 25, e40504. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rahman, M.H.; Usmani, N.G.; Chandra, P.; Manna, R.M.; Ahmed, A.; Shomik, M.S.; Arifeen, S.E.; Hossain, A.T.; Rahman, A.E. Mobile Apps to Prevent Violence Against Women and Girls (VAWG): Systematic App Research and Content Analysis. JMIR Form. Res. 2025, 9, e66247. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdul Latif El Ejel, B.; Sattar, S.; Fatima, S.B.; Khan, H.N.; Ali, H.; Iftikhar, A.; Sarwer, M.A.; Mushtaq, M. Digital Diabetes Management Technologies for Type 2 Diabetes: A Systematic Review of Home-Based Care Interventions. Cureus 2025, 17, e84177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jafari, B.; Amiri, M.R.; Labecka, M.K.; Rajabi, R. The effect of home-based and remote exercises on low back pain during the COVID-19 pandemic: A systemic review. J. Bodyw. Mov. Ther. 2025, 43, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Vijendran, S.; Alok, Y.; Kuzhuppilly, N.I.R.; Bhat, J.R.; Kamath, Y.S. Effectiveness of smartphone technology for detection of paediatric ocular diseases-a systematic review. BMC Ophthalmol. 2025, 25, 323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Andrade, L.I.; Viñán-Ludeña, M.S. Mapping research on ICT addiction: A comprehensive review of Internet, smartphone, social media, and gaming addictions. Front. Psychol. 2025, 16, 1578457. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sylla, B.; Ismaila, O.; Diallo, G. 25 Years of Digital Health Toward Universal Health Coverage in Low- and Middle-Income Countries: Rapid Systematic Review. J. Med. Internet Res. 2025, 27, e59042. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schaap, G.; Butt, B.; Bode, C. Suitability of just-in-time adaptive intervention in post-COVID-19-related symptoms: A systematic scoping review. PLoS Digit. Health 2025, 4, e0000832. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhuang, M.; Hassan, I.I.; WAhmad, W.M.A.; Abdul Kadir, A.; Liu, X.; Li, F.; Gao, Y.; Guan, Y.; Song, S. Effectiveness of Digital Health Interventions for Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2025, 27, e76323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhong, R.; Wu, X.; Chen, J.; Fang, Y. Using Digital Phenotyping to Discriminate Unipolar Depression and Bipolar Disorder: Systematic Review. J. Med. Internet Res. 2025, 27, e72229. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kargarandehkordi, A.; Li, S.; Lin, K.; Phillips, K.T.; Benzo, R.M.; Washington, P. Fusing Wearable Biosensors with Artificial Intelligence for Mental Health Monitoring: A Systematic Review. Biosensors 2025, 15, 202. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Melia, R.; Musacchio Schafer, K.; Rogers, M.L.; Wilson-Lemoine, E.; Joiner, T.E. The Application of AI to Ecological Momentary Assessment Data in Suicide Research: Systematic Review. J. Med. Internet Res. 2025, 27, e63192. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Woll, S.; Birkenmaier, D.; Biri, G.; Nissen, R.; Lutz, L.; Schroth, M.; Ebner-Priemer, U.W.; Giurgiu, M. Applying AI in the Context of the Association Between Device-Based Assessment of Physical Activity and Mental Health: Systematic Review. JMIR Mhealth Uhealth 2025, 13, e59660. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dehbozorgi, R.; Zangeneh, S.; Khooshab, E.; Nia, D.H.; Hanif, H.R.; Samian, P.; Yousefi, M.; Hashemi, F.H.; Vakili, M.; Jamalimoghadam, N.; et al. The application of artificial intelligence in the field of mental health: A systematic review. BMC Psychiatry 2025, 25, 132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- van Genugten, C.R.; Thong, M.S.Y.; van Ballegooijen, W.; Kleiboer, A.M.; Spruijt-Metz, D.; Smit, A.C.; Sprangers, M.A.G.; Terhorst, Y.; Riper, H. Beyond the current state of just-in-time adaptive interventions in mental health: A qualitative systematic review. Front. Digit. Health 2025, 7, 1460167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abdulazeem, H.; Borges do Nascimento, I.J.; Weerasekara, I.; Sharifan, A.; Grandi Bianco, V.; Cunningham, C.; Kularathne, I.; Deeken, G.; de Barros, J.; Sathian, B.; et al. Use of Digital Health Technologies for Dementia Care: Bibliometric Analysis and Report. JMIR Ment. Health 2025, 12, e64445. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pan, M.; Li, R.; Wei, J.; Peng, H.; Hu, Z.; Xiong, Y.; Li, N.; Guo, Y.; Gu, W.; Liu, H. Application of artificial intelligence in the health management of chronic disease: Bibliometric analysis. Front. Med. 2025, 11, 1506641. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Genovese, A.; Borna, S.; Gomez-Cabello, C.A.; Haider, S.A.; Prabha, S.; Forte, A.J.; Veenstra, B.R. Artificial intelligence in clinical settings: A systematic review of its role in language translation and interpretation. Ann. Transl. Med. 2024, 12, 117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Akbarian, P.; Asadi, F.; Sabahi, A. Developing Mobile Health Applications for Inflammatory Bowel Disease: A Systematic Review of Features and Technologies. Middle East J. Dig. Dis. 2024, 16, 211–220. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bernard, R.M.; Seijas, V.; Davis, M.; Volkova, A.; Diviani, N.; Lüscher, J.; Sabariego, C. Self-Management Support Apps for Spinal Cord Injury: Results of a Systematic Search in App Stores and Mobile App Rating Scale Evaluation. JMIR Mhealth Uhealth 2024, 12, e53677. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gao, E.Y.; Tan, B.K.J.; Tan, N.K.W.; Ng, A.C.W.; Leong, Z.H.; Phua, C.Q.; Loh, S.R.H.; Uataya, M.; Goh, L.C.; Ong, T.H.; et al. Artificial intelligence facial recognition of obstructive sleep apnea: A Bayesian meta-analysis. Sleep Breath. 2024, 29, 36. [Google Scholar] [CrossRef] [PubMed]
- IMDRF SaMD Working Group. Software as a Medical Device (SaMD): Key Definitions. International Medical Device Regulators Forum (IMDRF), December 2013. Available online: https://www.imdrf.org/sites/default/files/docs/imdrf/final/technical/imdrf-tech-131209-samd-key-definitions-140901.pdf (accessed on 28 July 2025).
- US Food and Drug Administration (FDA). Software as a Medical Device (SaMD). Available online: https://www.fda.gov/medical-devices/digital-health-center-excellence/software-medical-device-samd (accessed on 28 July 2025).
- U.S. Food & Drug Administration. Device Software Functions Including Mobile Medical Applications. Available online: https://www.fda.gov/medical-devices/digital-health-center-excellence/device-software-functions-including-mobile-medical-applications (accessed on 28 July 2025).
- Health Canada. Guidance Document: Software as a Medical Device (SaMD): Definition and Classification. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/medical-devices/application-information/guidance-documents/software-medical-device-guidance-document.html (accessed on 28 July 2025).
- Therapeutic Goods Administration (TGA), Australian Government. Understanding Regulation of Software-Based Medical Devices. Available online: https://www.tga.gov.au/resources/guidance/understanding-regulation-software-based-medical-devices (accessed on 28 July 2025).
- Medical Device Coordination Group Document. MDCG2019-11 Rev1. Guidance on Qualification Classification of Software in Regulation (EU) 2017/745–MDR and Regulation (EU) 2017/746–IVDR. Available online: https://health.ec.europa.eu/document/download/b45335c5-1679-4c71-a91c-fc7a4d37f12b_en?filename=mdcg_2019_11_en.pdf (accessed on 28 July 2025).
- US Food and Drug Administration (FDA). Artificial Intelligence and Machine Learning in Software as a Medical Device. Available online: https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device (accessed on 28 July 2025).
- ISO/DTS 24971-2; Medical Devices—Guidance on the Application of ISO 14971. Part 2: Machine Learning in Artificial Intelligence—Under Development, a Draft Is Being Reviewed by the Committee. Available online: https://www.iso.org/standard/87600.html (accessed on 28 July 2025).
- Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC. Available online: https://eur-lex.europa.eu/eli/reg/2017/745/oj/eng (accessed on 28 July 2025).
- Veyron, J.H.; Deparis, F.; Al Zayat, M.N.; Belmin, J.; Havreng-Théry, C. Postimplementation Evaluation in Assisted Living Facilities of an eHealth Medical Device Developed to Predict and Avoid Unplanned Hospitalizations: Pragmatic Trial. J. Med. Internet Res. 2024, 26, e55460. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karakoyun, T.; Podhaisky, H.P.; Frenz, A.K.; Schuhmann-Giampieri, G.; Ushikusa, T.; Schröder, D.; Zvolanek, M.; Lopes Da Silva Filho, A. Digital Medical Device Companion (MyIUS) for New Users of Intrauterine Systems: App Development Study. JMIR Med. Inform. 2021, 9, e24633. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Atee, M.; Hoti, K.; Hughes, J.D. A Technical Note on the PainChek™ System: A Web Portal and Mobile Medical Device for Assessing Pain in People with Dementia. Front. Aging Neurosci. 2018, 10, 117. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- The White House. US GOV. Removing Barriers to American Leadership in Artificial Intelligence. 23 January 2025. Available online: https://www.whitehouse.gov/presidential-actions/2025/01/removing-barriers-to-american-leadership-in-artificial-intelligence/ (accessed on 28 July 2025).
- Government of Canada. Artificial Intelligence and Data Act (Pending Bill C-27). 2022. Available online: https://ised-isde.canada.ca/site/innovation-better-canada/en/artificial-intelligence-and-data-act (accessed on 28 July 2025).
- Regulation (EU) 2024/1689 of the European Parliament and of the Council of 13 June 2024 Laying Down Harmonised Rules on Artificial Intelligence and Amending Regulations (EC) No 300/2008, (EU) No 167/2013, (EU) No 168/2013, (EU) 2018/858, (EU) 2018/1139 and (EU) 2019/2144 and Directives 2014/90/EU, (EU) 2016/797 and (EU) 2020/1828 (Artificial Intelligence Act). Available online: https://eur-lex.europa.eu/eli/reg/2024/1689/oj/eng (accessed on 28 July 2025).
- Government of, UK, Department for Science, Innovation and Technology. AI Regulation: A Pro-Innovation Approach. 3 August 2023. Available online: https://www.gov.uk/government/publications/ai-regulation-a-pro-innovation-approach (accessed on 28 July 2025).
- Australia Government, National Artificial Intelligence Centre. Voluntary AI Safety Standard. Guiding Safe and Responsible Use of Artificial Intelligence in Australia. 5 September 2024. Available online: https://www.industry.gov.au/publications/voluntary-ai-safety-standard (accessed on 28 July 2025).
- Shah, S.F.H.; Arecco, D.; Draper, H.; Tiribelli, S.; Harriss, E.; Matin, R.N. Ethical implications of artificial intelligence in skin cancer diagnostics: Use-case analyses. Br. J. Dermatol. 2025, 192, 520–529. [Google Scholar] [CrossRef] [PubMed]
- Späth, J.; Sewald, Z.; Probul, N.; Berland, M.; Almeida, M.; Pons, N.; Le Chatelier, E.; Ginès, P.; Solé, C.; Juanola, A.; et al. Privacy-Preserving Federated Survival Support Vector Machines for Cross-Institutional Time-To-Event Analysis: Algorithm Development and Validation. JMIR AI 2024, 3, e47652. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zawati, M.H.; Lang, M. Does an App a Day Keep the Doctor Away? AI Symptom Checker Applications, Entrenched Bias, and Professional Responsibility. J. Med. Internet Res. 2024, 26, e50344. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wongvibulsin, S.; Yan, M.J.; Pahalyants, V.; Murphy, W.; Daneshjou, R.; Rotemberg, V. Current State of Dermatology Mobile Applications with Artificial Intelligence Features. JAMA Dermatol. 2024, 160, 646–650, Erratum in JAMA Dermatol. 2024, 160, 688. https://doi.org/10.1001/jamadermatol.2024.1011. Erratum in JAMA Dermatol. 2024, 160, 688. https://doi.org/10.1001/jamadermatol.2024.1342. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alfano, L.; Malcotti, I.; Ciliberti, R. Psychotherapy, artificial intelligence and adolescents: Ethical aspects. J. Prev. Med. Hyg. 2024, 64, E438–E442. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ouellette, S.; Rao, B.K. Usefulness of Smartphones in Dermatology: A US-Based Review. Int. J. Environ. Res. Public Health 2022, 19, 3553. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matin, R.N.; Dinnes, J. AI-based smartphone apps for risk assessment of skin cancer need more evaluation and better regulation. Br. J. Cancer 2021, 124, 1749–1750. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pashkov, V.M.; Harkusha, A.O.; Harkusha, Y.O. Artificial Intelligence in Medical Practice: Regulative Issues and Perspectives. Wiad. Lek. 2020, 73, 2722–2727. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Martin, N.; Kreitmair, K. Ethical Issues for Direct-to-Consumer Digital Psychotherapy Apps: Addressing Accountability, Data Protection, and Consent. JMIR Ment. Health 2018, 5, e32. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ebad, S.A.; Alhashmi, A.; Amara, M.; Miled, A.B.; Saqib, M. Artificial Intelligence-Based Software as a Medical Device (AI-SaMD): A Systematic Review. Healthcare 2025, 13, 817. [Google Scholar] [CrossRef] [PubMed]
- Joshi, G.; Jain, A.; Araveeti, S.R.; Adhikari, S.; Garg, H.; Bhandari, M. FDA-Approved Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices: An Updated Landscape. Electronics 2024, 13, 498. [Google Scholar] [CrossRef]
- MDCG 2025-6—Interplay Between the Medical Devices Regulation & In Vitro Diagnostic Medical Devices Regulation and the Artificial Intelligence Act (June 2025). Available online: https://health.ec.europa.eu/latest-updates/mdcg-2025-6-faq-interplay-between-medical-devices-regulation-vitro-diagnostic-medical-devices-2025-06-19_en (accessed on 28 July 2025).
- World Health Organization. Global Strategy on Digital Health 2020–2025. Available online: https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf (accessed on 4 November 2023).
- Butcher, C.J.; Hussain, W. Digital healthcare: The future. Future Healthc. J. 2022, 9, 113–117. [Google Scholar] [CrossRef]
- Deloitte. 2019 Global Health Care Outlook Shaping the Future. Available online: https://www.deloitte.com/gr/en/Industries/life-sciences-health-care/perspectives/2019-global-life-sciences-health-care-outlook.html (accessed on 19 October 2023).
- IQVIA. Digital Health Trends 2021: Innovation Evidence Regulation Adoption. Available online: https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/digital-health-trends-2021 (accessed on 4 November 2023).
- Gál, É.; Ștefan, S.; Cristea, I.A. The efficacy of mindfulness meditation apps in enhancing users’ well-being and mental health related outcomes: A meta-analysis of randomized controlled trials. J. Affect. Disord. 2021, 279, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Linardon, J.; Cuijpers, P.; Carlbring, P.; Messer, M.; Fuller-Tyszkiewicz, M. The efficacy of app-supported smartphone interventions for mental health problems: A meta-analysis of randomized controlled trials. World Psychiatry 2019, 18, 325–336. [Google Scholar] [CrossRef]
- Mao, Y.; Lin, W.; Wen, J.; Chen, G. Impact and efficacy of mobile health intervention in the management of diabetes and hypertension: A systematic review and meta-analysis. BMJ Open Diabetes Res. Care 2020, 8, 69. [Google Scholar] [CrossRef]
- Stevens, S.; Gallagher, S.; Andrews, T.; Ashall-Payne, L.; Humphreys, L.; Leigh, S. The effectiveness of digital health technologies for patients with diabetes mellitus: A systematic review. Front. Clin. Diabetes Healthc. 2022, 3, 936752. [Google Scholar] [CrossRef]
- Bretschneider, M.P.; Kolasińska, A.B.; Šomvárska, L.; Klásek, J.; Mareš, J.; Schwarz, P.E. Evaluation of the Impact of Mobile Health App Vitadio in Patients with Type 2 Diabetes: Randomized Controlled Trial. J. Med. Internet Res. 2025, 27, e68648. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Qin, M.; Chen, B.; Sun, S.; Liu, X. Effect of mobile phone app-based interventions on quality of life and psychological symptoms among adult cancer survivors: Systematic review and meta-analysis of randomized controlled trials. J. Med. Internet Res. 2022, 24, e39799. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Chen, Y.; Chen, J.; Zhang, Y.; Li, M.; Xiong, C.; Yan, J. Effectiveness of mobile health-based self-management interventions in breast cancer patients: A meta-analysis. Support Care Cancer 2022, 30, 2853–2876. [Google Scholar] [CrossRef]
- Gloeckl, R.; Spielmanns, M.; Stankeviciene, A.; Plidschun, A.; Kroll, D.; Jarosch, I.; Schneeberger, T.; Ulm, B.; Vogelmeier, C.F.; Koczulla, A.R. Smartphone application-based pulmonary rehabilitation in COPD: A multicentre randomised controlled trial. Thorax 2025, 80, 209–217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Iribarren, S.J.; Cato, K.; Falzon, L.; Stone, P.W. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS ONE 2017, 12, e0170581. [Google Scholar] [CrossRef]
- Jiang, X.; Ming, W.K.; You, J.H. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: Systematic review. J. Med. Internet Res. 2019, 21, e13166. [Google Scholar] [CrossRef]
- PwC. Socio-Economic Impact of mHealth: An Assessment Report for the European Union. 2013. Available online: https://www.gsma.com/iot/wp-content/uploads/2013/06/Socio-economic_impact-of-mHealth_EU_14062013V2.pdf (accessed on 20 October 2023).
- Jacob, C.; Sanchez-Vazquez, A.; Ivory, C. Understanding clinicians’ adoption of mobile health tools: A qualitative review of the most used frameworks. JMIR Mhealth Uhealth 2020, 8, e18072. [Google Scholar] [CrossRef]
- Jacob, C.; Sezgin, E.; Sanchez-Vazquez, A.; Ivory, C. Sociotechnical factors affecting patients’ adoption of mobile health tools: Systematic literature review and narrative synthesis. JMIR Mhealth Uhealth 2022, 10, e36284. [Google Scholar] [CrossRef] [PubMed]
- Grundy, Q. A review of the quality and impact of mobile health apps. Annu. Rev. Public Health 2022, 43, 117–134. [Google Scholar] [CrossRef]
- Hyzy, M.; Bond, R.; Mulvenna, M.; Bai, L.; Frey, A.L.; Carracedo, J.M.; Daly, R.; Leigh, S. Don’t judge a book or health app by its cover: User ratings and downloads are not linked to quality. PLoS ONE 2024, 19, e0298977. [Google Scholar] [CrossRef]
- Biliunaite, I.; van Gestel, L.; Hoogendoorn, P.; Adriaanse, M. Value of a quality label and European healthcare professionals’ willingness to recommend health apps: An experimental vignette study. J. Health Psychol. 2025, 30, 1278–1290. [Google Scholar] [CrossRef]
- Dahlhausen, F.; Zinner, M.; Bieske, L.; Ehlers, J.P.; Boehme, P.; Fehring, L. Physicians’ attitudes toward prescribable mHealth apps and implications for adoption in Germany: Mixed methods study. JMIR Mhealth Uhealth 2021, 9, e33012. [Google Scholar] [CrossRef] [PubMed]
- European mHealth Hub. D2.1 Knowledge Tool 1: Health Apps Assessment Frameworks. Available online: https://promisalute.it/wp-content/uploads/2023/02/D2.1-KT1-Health-Apps-Assessment-Frameworks.pdf (accessed on 20 October 2023).
- Hoogendoorn, P.; Versluis, A.; van Kampen, S.; McCay, C.; Leahy, M.; Bijlsma, M.; Bonacina, S.; Bonten, T.; Bonthuis, M.J.; Butterlin, A.; et al. What makes a quality health app-developing a global research-based health app quality assessment framework for CEN-ISO/TS 82304-2: Delphi study. JMIR Form. Res. 2023, 7, e43905. [Google Scholar] [CrossRef] [PubMed]
- Frey, A.L.; Phillips, B.; Baines, R.; McCabe, A.; Elmes, E.; Yeardsley-Pierce, E.; Wall, R.; Parry, J.; Vose, A.; Hewitt, J.; et al. Domain coverage and criteria overlap across digital health technology quality assessments: A systematic review. Health Technol. 2024, 15, 15–27. [Google Scholar] [CrossRef]
- Llebot, C.B.; Hoogendoorn, P.; Villalobos-Quesada, M.; Pratdepàdua, B.C. Integration of CEN ISO/TS 82304-2 for existing health authorities? App assessment frameworks: A comparative case study in Catalonia. JMIR mHealth uHealth Forthcom. 2024. Available online: https://www.iso.org/standard/78182.html (accessed on 14 November 2025).
- ISO/TS 82304-2:2021; Health and Wellness Apps—Quality and Reliability. International Organization for Standardization: Geneva, Switzerland, 2021.
- IEC 82304-1:2016; Health Software—General Requirements for Product Safety. IEC Webstore: Geneva, Switzerland, 2016.
- ISO/IEC 42001:2023; Information Technology—Artificial Intelligence—Management Systems. JTC 1: Geneva, Switzerland, 2023.
- ISO 13485:2016; Medical Devices—Quality Management Systems—Requirements for Regulatory Purposes. International Organization for Standardization: Geneva, Switzerland, 2016.
- ISO 14971:2019; Medical Devices—Application of Risk Management to Medical Devices. International Organization for Standardization: Geneva, Switzerland, 2019.
- ISO/IEC 27001:2022; Information Security Management Systems—Requirements. JTC 1: Geneva, Switzerland, 2022.
- ISO/IEEE 11073-40101:2022; Health Informatics—Device Interoperability—Cybersecurity—Vulnerability Assessment Processes. JTC 1: Geneva, Switzerland, 2022.
- IEC/TR 80002-1:2009; Medical Device Software—Guidance on Applying ISO 14971 to Software. IEC Webstore: Geneva, Switzerland, 2009.
- AAMI TIR 34971:2023; Application of ISO 14971 to Machine Learning in AI. Available online: https://webstore.ansi.org/standards/aami/aamitir349712023?srsltid=AfmBOopTNvxB0WFMnuVoZnYyQImwvUeP6X6X0fyZXAdQBC0cDL_BuG72 (accessed on 14 November 2025).
- FG-AI4H DEL2.2:2022; Good Practices for Health Applications of AI. Available online: https://www.itu.int/dms_pub/itu-t/opb/fg/T-FG-AI4H-2022-2-PDF-E.pdf (accessed on 14 November 2025).
- Hasan, M.M.; Phu, J.; Wang, H.; Sowmya, A.; Kalloniatis, M.; Meijering, E. OCT-based diagnosis of glaucoma and glaucoma stages using explainable machine learning. Sci. Rep. 2025, 15, 3592. [Google Scholar] [CrossRef]
- Hasan, M.M.; Phu, J.; Wang, H.; Sowmya, A.; Meijering, E.; Kalloniatis, M. Predicting visual field global and local parameters from OCT measurements using explainable machine learning. Sci. Rep. 2025, 15, 5685. [Google Scholar] [CrossRef] [PubMed]


| Focus Area | Mobile Health Terms | AI Terms | Notes |
|---|---|---|---|
| General AI in mHealth | “mobile health”, “mHealth”, “app *”, “smartphone” | “artificial intelligence”, “AI” | Broad capture of AI applications in mHealth |
| Machine Learning applications | “mobile health”, “mHealth”, “app *”, “smartphone”, “wearable devices” | “machine learning”, “ML”, “supervised learning”, “unsupervised learning” | Predictive analytics and automated decision-making |
| Deep Learning & Neural Networks | “mobile health”, “mHealth”, “app *”, “smartphone” | “deep learning”, “neural networks”, “CNN”, “RNN” | Advanced AI algorithms for clinical or monitoring purposes |
| Telemedicine & Remote Monitoring | “mobile health”, “mHealth”, “app *”, “smartphone”, “telemedicine”, “remote monitoring” | “AI”, “machine learning”, “deep learning”, “neural networks”, “CNN”, “RNN”, “predictive analytics”, “decision support” | Enhancing patient management and chronic disease monitoring |
| Specific Clinical Domains | “mobile health”, “mHealth”, “app *”, “smartphone”, “mobile apps” | “AI”, “machine learning”, “deep learning” + disease terms (e.g., “diabetes”, “cardiovascular disease”, “mental health”) | Targeted retrieval for specific disease areas |
| Criterion | Definition | Inclusion | Exclusion | Notes |
|---|---|---|---|---|
| Study Type | Type of publication | Reviews, with priority to Systematic reviews and Meta-analyses | Original research, Case reports, Technical notes | Ensures high level of evidence |
| Clinical/Bioengineering Relevance | Application in health or bioengineering | mHealth interventions with AI for chronic disease management, telemedicine, mental health, rehabilitation | Purely computational studies, algorithm benchmarking, data architecture without clinical/translational outcomes | Focus on real impact in clinical practice |
| Temporal Scope | Publication period | Studies up to 31 July 2025 | Studies outside this period | Updated post-pandemic coverage |
| Language | Language | English | Non-English | International accessibility and reproducibility |
| Study Focus | Main content | AI applications with tangible clinical/translational value | Technical-only AI methods without healthcare relevance | Maintains focus on clinical narrative |
| Ref. | Description | Focus | Contribution of mHealth and AI | Target Domain | Observed Patterns/Trends |
|---|---|---|---|---|---|
| [21] Patel J et al. | This review evaluates predictive artificial intelligence approaches used in mobile health platforms to forecast mental health symptoms among youth. It synthesizes how smartphone and wearable data, such as usage patterns, sleep, and physical activity, have been leveraged in predictive models to detect depression, anxiety, and stress. The study highlights both the promise of precision prediction and challenges including small sample sizes and privacy concerns that should be addressed in future work. | Predicting mental health symptoms (e.g., depression, anxiety, stress) using AI and mHealth tools. | Real-time monitoring of mental health; supports precision prevention strategies | Mental health (youth, 13–25) | Predictive AI models; mental health monitoring; youth-focused interventions |
| [22] Manyazewal T et al. | This study reviews innovative technologies, including AI and mobile health solutions, aimed at addressing neglected tropical diseases in African settings with ongoing sociopolitical instability. It discusses how these tools support disease surveillance, diagnosis, and intervention in contexts with limited healthcare infrastructure. The review emphasizes feasibility and adaptation of technological approaches in unstable and low-resource environments. | Use of AI, mobile apps, and other technologies for NTD prevention, diagnosis, and management amidst instability. | Supports NTD surveillance and treatment; AI aids in outbreak prediction and intervention planning | Neglected tropical diseases | AI for outbreak prediction; mHealth for disease management; low-resource and unstable regions |
| [23] Thakuria T et al. | This review examines the use of deep learning for early diagnosis of oral cancer via smartphone and DSLR image analysis. It highlights the role of convolutional neural networks in improving classification accuracy for early detection tasks. The study also discusses challenges such as data quality and limited annotated datasets, while noting the potential for accessible screening tools in low-resource settings. | Deep learning (CNN) applications for early oral cancer diagnosis using smartphone and DSLR imaging. | AI-based tools improve diagnostic accuracy; enhances accessibility of screening | Oral cancer diagnosis | Deep learning for image-based diagnosis; diagnostic accuracy improvements; potential for low-resource deployment |
| [24] Förstel M et al. | This review investigates features used in machine learning models to forecast patient arrival numbers in healthcare settings. It focuses on various predictor types, including non-temporal data such as weather and internet usage patterns, to enhance forecasting accuracy. The study highlights how these models can support operational planning, reducing prediction errors and improving resource allocation in clinical environments. | Machine learning feature identification for forecasting patient arrivals using non-temporal predictors. | ML forecasting aids operational planning; highlights value of diverse non-temporal features | Healthcare operations | Operational optimization via ML; non-clinical healthcare AI use; feature exploration beyond temporal data |
| [25] Chau RC et al. | This review discusses the potential of self-monitoring oral health using smartphone selfies powered by artificial intelligence for preventive dentistry. It evaluates how AI-enabled oral health tools can detect dental conditions and support early prevention by reducing plaque and gingival indices. The synthesis notes positive short-term outcomes and suggests areas requiring further research on long-term behavioral change and oral health awareness. | AI-enhanced self-monitoring of oral health via smartphone images and selfies. | Supports early detection of oral health issues; facilitates preventive dental care; reduces plaque and gingival indices | Preventive dentistry | AI for self-monitoring; smartphone-based diagnostic support; early prevention strategies |
| [26] Fu Y et al. | This systematic review evaluates smartphone-based hand function assessment tools that leverage artificial intelligence. It focuses on how sensor data from mobile devices can objectively measure hand mobility and performance, potentially improving rehabilitation and clinical assessment. The study highlights the strengths of combining smartphone sensors with automated analysis while noting gaps in standardization and clinical validation. | Smartphone-based assessment of hand function using AI and sensor data. | Provides objective measurement of hand function; enhances rehabilitation assessment; supports remote monitoring | Hand function assessment | Sensor data integration; AI-driven functional evaluation; clinical assessment support |
| [27] Negi S et al. | This umbrella review synthesizes evidence on artificial intelligence applications for dental caries diagnosis and detection. It explores a range of models and techniques used to identify caries from dental images and clinical data, summarizing diagnostic performance and limitations. The review underscores the promise of AI in improving diagnostic accuracy while calling for further validation across diverse populations. | AI for dental caries diagnosis and detection across imaging and clinical datasets. | Improves diagnostic accuracy; supports early detection workflows; highlights need for broader validation | Dental caries diagnosis | Diagnostic AI models; image and data fusion techniques; clinical applicability and validation needs |
| [28] Lange M et al. | This review identifies approaches for using AI in workplace health promotion and prevention, focusing on how digital tools can support occupational wellbeing. It synthesizes evidence on predictive models and interventions that address physical activity, stress management, and healthy behaviours. The study highlights opportunities and challenges for implementing AI-driven workplace health solutions across diverse occupational settings. | AI in workplace health promotion and preventive interventions. | Supports health behaviour monitoring; predictive models for stress and activity; enhances occupational health strategies | Workplace health promotion | AI for behavioural health support; digital intervention trends; organizational implementation |
| [29] Chow SM et al. | This systematic review and meta-analysis examines the effectiveness of mHealth apps on adherence to and symptoms from oral anticancer medications. It evaluates how mobile applications influence medication adherence, symptom reporting, and clinical outcomes. Results indicate that mHealth interventions can improve adherence and reduce symptom burden, although study heterogeneity suggests the need for standardized outcomes. | Effectiveness of mHealth apps on adherence and symptoms for oral anticancer medications. | Improves medication adherence; reduces symptom burden; supports patient engagement | Oral anticancer treatment adherence | mHealth for adherence support; symptom tracking; patient engagement trends |
| [30] Jin K et al. | This systematic review examines how smartphone technology integrated with artificial intelligence is used in advanced ophthalmic care. It synthesizes evidence from 52 studies on screening, disease detection, telemedicine, and patient management across major ocular conditions. The review emphasizes improvements in diagnostic performance and accessibility, while noting challenges related to data privacy, algorithm validation, and real-world implementation. | Integration of smartphone technology and AI to improve ophthalmic diagnosis, screening, telemedicine, and patient care. | Enhances early detection and monitoring of eye diseases; supports remote patient management; improves accessibility in underserved areas | Ophthalmic care and eye disease management | AI-driven smartphone imaging; tele-ophthalmology enhancement; accessibility and diagnostic performance improvements |
| [31] Choi A et al. | This review assesses digital phenotyping methods using smartphone sensors to detect behavioral patterns associated with stress, anxiety, and mild depression in nonclinical adult populations. It highlights evidence that passive sensing, such as GPS, accelerometer, and phone usage patterns, can identify correlates of mild mental health symptoms. The study also addresses challenges such as sensor accuracy, privacy concerns, and individual behavioral variability across contexts. | Digital phenotyping via smartphone sensors for detecting stress, anxiety, and mild depression. | Identifies behavioral patterns linked to mental health using smartphone data; highlights effective passive sensors; discusses ethical and technical challenges | Behavioral mental health monitoring | Passive sensing for behavioral markers; sensor pattern associations with mental health; privacy and technical limitations |
| [32] Segur-Ferrer J et al. | This scoping review and thematic analysis identifies methodological frameworks and key dimensions to be considered in digital health technology assessment (DHTA). It synthesizes frameworks used to evaluate digital health technologies, including metrics related to clinical effectiveness, usability, economic impact, and ethical considerations. The review highlights the need for comprehensive, multidimensional assessment approaches to support robust evaluation and regulatory decisions. | Frameworks and dimensions for assessing digital health technologies, including AI and mobile health tools. | Clarifies assessment criteria for digital health technologies; highlights clinical, usability, economic, and ethical dimensions; guides structured evaluation practices | Digital health technology assessment | Multidimensional evaluation criteria; methodological framework synthesis; implications for regulatory and policy decisions |
| [33] Giunti G et al. | This review explores the co-creation of an automated mHealth apps systematic review process using generative AI within a design science research framework. It discusses how AI-enabled tools can assist in automating literature screening, data extraction, and synthesis tasks. The study highlights the potential of generative AI to enhance efficiency and consistency in systematic review workflows while considering design challenges in human–AI collaboration. | Use of generative AI to automate components of systematic review processes for mHealth apps. | Shows generative AI supporting automation of review screening and extraction; enhances efficiency and consistency of review workflows; discusses human–AI cooperation design | Review process automation | Generative AI for review automation; human–AI collaboration challenges; efficiency improvements in evidence synthesis |
| [34] Pala D et al. | This review examines smartphone applications designed to support nutrition, focusing on target outcomes and core functionalities. It synthesizes evidence on app features such as dietary tracking, personalized feedback, and behavior change support. The study discusses how apps influence nutritional outcomes and user engagement, as well as limitations related to evidence quality and long-term adherence. | Functionality and outcomes of nutrition support smartphone applications. | Offers dietary tracking and personalized feedback; supports behavior change and nutritional monitoring; highlights engagement features | Nutrition support via mobile apps | Personalized nutrition feedback; behavior change support; functionality outcome mapping |
| [35] Jahan E et al. | This systematic review and meta-analysis evaluates smartphone applications aimed at preventing type 2 diabetes through lifestyle change support. It assesses outcomes related to weight management, physical activity, dietary behaviors, and metabolic indicators. The findings suggest that mHealth apps can contribute to diabetes prevention through structured interventions and continuous user engagement. | Smartphone apps for prevention of type 2 diabetes through lifestyle modification. | Promotes physical activity and dietary change; facilitates continuous engagement; supports metabolic outcome improvements | Type 2 diabetes prevention | Lifestyle modification support; engagement and adherence trends; preventive health impact |
| [36] Gheisari M et al. | This multidimensional systematic review examines mobile apps for COVID-19 detection and diagnosis, focusing on their potential use in pandemic control and future outbreak management. It synthesizes evidence on app functionalities, diagnostic performance, and integration with public health monitoring systems. The review highlights opportunities and limitations in using mobile tools for pandemic preparedness and response. | Mobile apps for COVID-19 detection and diagnosis and implications for future pandemic control. | Supports disease surveillance and early detection; integrates diagnostic functions with public health data; highlights limitations and future needs | Pandemic detection and control | Diagnostic surveillance via apps; pandemic preparedness relevance; integration with public health infrastructure |
| [37] Tomlin HR et al. | This review identifies challenges and opportunities for professional medical publication writers to contribute to plain language summaries (PLS) within AI/ML research environments. It discusses barriers related to interpretability, accuracy, and audience comprehension, and highlights strategies to improve the quality of PLS. The study emphasizes the role of clear communication in translating complex AI/ML evidence for diverse stakeholders. | Challenges and opportunities in creating plain language summaries in an AI/ML research context. | Highlights interpretability and communication barriers; suggests strategies for improving PLS quality; addresses stakeholder engagement in evidence translation | Health communication and AI/ML interpretation | Plain language science communication; stakeholder comprehension trends; role of writers in AI evidence translation |
| [38] Xue J et al. | This scoping review evaluates the current state of chatbots in digital health, examining their functionalities, applications, and potential benefits. It synthesizes evidence on how conversational agents support health information, triage, patient engagement, and self-management. The study discusses both opportunities and limitations, including accuracy, user trust, and integration with clinical workflows. | Evaluation of chatbot technologies in digital health contexts. | Supports health information delivery and triage; enables patient engagement and self-management; discusses challenges with trust and clinical integration | Digital health chatbots | Conversational AI applications; engagement and triage support; trust and workflow integration |
| [39] He X et al. | This scoping review identifies existing barriers faced by direct-to-consumer AI healthcare apps and provides recommendations for future design improvements. It highlights issues such as usability, transparency, data privacy, and regulatory compliance that limit adoption. The review emphasizes the need to address these challenges to enhance user trust and app effectiveness in everyday healthcare. | Barriers and design recommendations for direct-to-consumer AI healthcare applications. | Identifies usability and transparency challenges; highlights privacy and regulatory issues; offers design recommendations for future apps | Direct-to-consumer AI healthcare apps | Usability and trust barriers; privacy and regulatory considerations; future design directions |
| [40] Sumner J et al. | This systematic review evaluates AI applications in physical rehabilitation, examining availability, clinical effects, and implementation barriers. Evidence spans app-based systems, robotic devices, gaming systems, and wearables used to restore function, improve physical activity, or assist recovery. The review highlights mixed clinical effects and identifies challenges such as technology literacy, reliability issues, and user fatigue, while noting potential improvements in access and remote monitoring. | AI applications in physical rehabilitation to support recovery and functional outcomes. | AI-enhanced systems for rehabilitation tasks; supports remote monitoring and access to programmes; reduces manpower requirements | Physical rehabilitation | Diverse AI solutions (robotics, wearables); mixed clinical effectiveness; implementation and usability barriers |
| [41] Bendotti et al. | This systematic review and meta-analysis assesses conversational AI interventions for smoking cessation, focusing on their effectiveness compared with standard care or no intervention. It synthesizes evidence from RCTs using chatbots and dialogue systems across apps, social media, and web platforms. Results indicate promising benefits for sustained tobacco abstinence, though high heterogeneity and study bias suggest cautious interpretation. | Conversational AI for supporting smoking cessation outcomes. | Conversational AI increases likelihood of quitting smoking; chatbots emulate personalised support; highlights engagement and behavioural support | Smoking cessation support | AI for behaviour change support; mobile conversational agents; engagement and intervention heterogeneity |
| [42] Pyper et al. | This scoping review examines digital health technologies using patient-generated data for real-world clinical outcome measurement. It highlights frameworks and use cases where mobile tools complement clinical assessments, addressing challenges like data quality, integration, and interpretability. The review underscores potential for personalised healthcare decision-making. | Digital health technologies leveraging patient-generated data for clinical outcome measurement. | Uses mobile and digital tools to capture real-world health data; supports objective outcome measurement; highlights integration and interpretability challenges | Patient-generated outcome measurement | Real-world data integration; mobile data for outcomes; challenges in data quality and clinical integration |
| [43] Hasan et al. | This systematic review and meta-analysis evaluates smartphone-based AI systems for diabetic retinopathy detection. Evidence on sensitivity, specificity, and diagnostic performance shows potential for early identification, especially in low-resource settings. Limitations include data diversity, algorithm generalisability, and need for rigorous clinical validation. | Diagnostic accuracy of smartphone-based AI systems for diabetic retinopathy detection. | AI improves early detection accuracy; facilitates screening in non-specialist settings; highlights validation and generalisability needs | Diabetic retinopathy diagnosis | Smartphone AI for imaging diagnosis; accessibility in low-resource settings; need for broader validation |
| [44] Chatterjee et al. | This systematic review and knowledge mapping explores ICT-based remote and automatic COVID-19 patient monitoring and care. It highlights mobile apps, telemonitoring systems, and automated alerts used for tracking symptoms, vital signs, and care coordination. The review discusses opportunities and limitations, including data integration, user acceptance, and scalability. | ICT-based remote and automatic monitoring and care for COVID-19 patients. | Mobile and digital tools for remote symptom tracking; supports care coordination and alerting; highlights scalability and integration challenges | COVID-19 remote patient monitoring | Remote monitoring trend; ICT and mobile integration; pandemic-driven innovation |
| [45] Fegan & Hutchinson | This short review examines the potential of mobile technology to address early childhood caries. It discusses current interventions, smartphone-enabled dental monitoring, and preventive strategies. The article emphasizes the need for stronger evidence and standardized methodologies for real-world prevention. | Exploration of mobile technology’s role in reducing early childhood caries. | Suggests mobile tools for dental health monitoring; encourages preventive strategies; notes need for rigorous validation | Early childhood caries prevention | Mobile dental monitoring concepts; preventive focus; need for stronger evidence |
| [46] Koumpouros et al. | This systematic review investigates mobile applications for pain management, covering commercial and research efforts integrating AI or computational support. It synthesizes evidence on app features, usability, and outcomes related to tracking pain, adherence, and self-help resources. Limitations include diversity of approaches, standardization, and clinical validation. | Pain management mobile applications integrating AI and supportive technologies. | Supports pain tracking and self-management; offers therapeutic guidance and reminders; highlights usability and evidence gaps | Pain management via mobile apps | Self-management trend; pain tracking features; usability and validation limitations |
| [47] Duarte et al. | This systematic review evaluates digital clinical tools for screening or diagnosing obstructive sleep apnea. It synthesizes evidence on tool performance, including sensitivity, specificity, and feasibility across care settings. The review highlights opportunities for earlier detection and streamlined diagnostics, along with challenges in data quality, patient adherence, and integration. | Digital clinical tools and AI in screening and diagnosis of obstructive sleep apnea. | Enhances early detection of sleep apnea; supports diagnostic workflows; notes challenges in real-world integration | Obstructive sleep apnea screening and diagnosis | AI clinical tool trend; diagnostic accuracy focus; adoption challenges |
| [48] Lin et al. | This systematic assessment examines conversational agents for mental health and well-being, focusing on scope, characteristics, behaviour change techniques, and app quality. It highlights how these apps use dialogue and interaction patterns to support mental health outcomes, including cognitive behavioural strategies. Limitations in sustaining long-term mental health improvements are also discussed. | Conversational agents for mental health and well-being, including behaviour change and engagement. | Supports mental health engagement via chatbots; integrates behaviour change techniques; evaluates quality and engagement metrics | Conversational mental health support | Behaviour change focus; conversational AI engagement; quality variability |
| [49] Moharrami et al. | This systematic review evaluates AI algorithms for detecting dental caries on oral photographs, assessing diagnostic accuracy, methodology, and data sources. Evidence shows promising performance for screening and early detection, though limitations include dataset bias and the need for validation across diverse populations. | AI for detecting dental caries from oral photographs and imaging data. | AI enhances dental caries detection accuracy; supports early screening and decision support; highlights dataset and validation needs | Dental caries detection via photography | Imaging AI for dentistry; diagnostic screening trend; validation and bias issues |
| [50] Piendel et al. | This review provides an update on mobile applications that collect data among adults with or at risk of Alzheimer’s disease, focusing on passive and active data collection relevant to cognitive changes. It synthesizes evidence on how smartphone apps can monitor daily routines and behaviors that may indicate subtle cognitive decline, with potential utility for early detection and screening. The review also discusses limitations in current app validation and privacy issues, noting that widespread implementation remains underdeveloped despite promising feasibility. | Mobile applications collecting data for cognitive health and Alzheimer’s disease screening. | Passively and actively collects cognitive data; potential early detection and screening support; highlights privacy and validation concerns | Cognitive health screening and Alzheimer’s risk | Passive and active data tracking; cognitive change monitoring; screening tool feasibility |
| [51] Lam et al. | This systematic review examines applications of markerless motion capture (MMC) technology for clinical measurement in rehabilitation, highlighting its potential to track movement without physical markers. It summarizes studies where MMC has been applied to identify and measure movement patterns in various patient populations, with focuses on clinical utility and feasibility. The review notes that although the approach shows promise for rehabilitation assessments, evidence on clinical effectiveness and integration with AI models remains preliminary and requires further development. | Markerless motion capture technology applied to clinical movement measurement in rehabilitation. | Avoids need for physical markers; tracks movement kinematics; potential integration with AI for screening | Rehabilitation movement analysis | MMC for clinical assessment; motion tracking innovations; preliminary evidence and integration needs |
| [52] Sumra et al. | This systematic review evaluates smartphone apps designed for domestic violence prevention, focusing on features and effectiveness of mobile tools addressing safety, reporting, and support. It synthesizes evidence on how these apps facilitate emergency response, risk assessment, and access to resources for individuals at risk of domestic violence. The study highlights the range of functionalities offered and notes gaps in empirical evaluation and standardized outcome measurement for these prevention technologies. | Smartphone apps for domestic violence prevention and support. | Supports emergency reporting and risk assessment; provides safety resources and guidance; notes evaluation and outcome measure gaps | Domestic violence prevention | Safety and reporting functions; support resource access; need for standardized evaluation |
| [53] Chakraborty et al. | This systematic review examines the role of telehealth startups in transforming healthcare service delivery, synthesizing evidence on digital platforms, service models, and integration with clinical care. It highlights how telehealth innovations, including mobile technologies, facilitate remote consultations, monitoring, and care coordination, expanding access to healthcare services. The review also discusses barriers such as regulatory issues, interoperability challenges, and digital literacy that affect implementation and uptake. | Telehealth startups and their impact on healthcare service delivery, including digital and mobile integration. | Expands remote consultations and care coordination; integrates monitoring and patient engagement; notes regulatory and interoperability challenges | Telehealth service delivery | Remote care expansion; digital platform integration; implementation barriers |
| [54] Irgang et al. | This systematic review explores data-driven technologies used to prevent surgical site infections by enabling early detection, risk stratification, and monitoring. It synthesizes approaches that leverage AI, predictive analytics, and mobile or clinical data platforms to support infection prevention workflows. The study highlights technological contributions to value creation in healthcare by improving surveillance, informing clinical decisions, and guiding intervention strategies. | Data-driven technologies, including AI, for preventing surgical site infections. | Enhances infection surveillance and prediction; supports clinical decision-making; guides prevention strategies | Surgical site infection prevention | Predictive analytics for infection risk; AI surveillance approaches; value creation in prevention |
| [55] Torres-Guzman et al. | This systematic review examines the effectiveness of smartphones and threshold-based monitoring methods for remote fall detection, focusing on accuracy and feasibility in real-world settings. It synthesizes evidence showing that these methods can reliably detect falls using sensor data and predefined thresholds, with implications for timely response and patient safety. The review also discusses variability in algorithms, sensor performance, and usability factors that influence effectiveness in diverse populations. | Smartphone and threshold-based monitoring for remote fall detection. | Detects falls remotely using sensor thresholds; improves timeliness of alerts; highlights algorithmic and usability variability | Remote fall detection | Sensor-based monitoring; remote safety support; algorithm and usability considerations |
| [56] van Eijck et al. | This scoping review examines digital health applications designed to establish remote diagnosis of orthopedic knee disorders, focusing on mobile and digital tools that assess symptoms, function, and imaging. It synthesizes evidence on tele-assessment, diagnostic decision support, and remote clinical evaluation methods that leverage AI or automated analysis. The study highlights potential benefits in reducing in-person visits while noting challenges in validation, clinical adoption, and integration into care pathways. | Remote digital health applications for diagnosis of orthopedic knee disorders. | Enables remote clinical symptom and function assessment; supports diagnostic workflows; notes validation and adoption challenges | Orthopedic knee disorder diagnosis | Remote assessment trends; digital diagnostic tools; integration challenges |
| [57] Rahman et al. | This research review and content analysis evaluates mobile apps aimed at preventing violence against women and girls (VAWG), assessing features, reach, and content quality. It synthesizes evidence on app functionalities such as risk assessment, safety planning, incident reporting, and educational resources. The study highlights gaps in empirical validation and standard outcome measures, calling for improved evaluation frameworks and user-centered design. | Mobile apps for preventing violence against women and girls, focusing on safety and support features. | Provides risk assessment and safety planning tools; supports incident reporting and education; highlights evaluation and design gaps | Violence against women and girls prevention | Safety and education features; support tool functionalities; need for robust evaluation |
| [58] Abdul Latif El Ejel et al. | This systematic review examines digital diabetes management technologies for type 2 diabetes care in home-based settings, focusing on mobile tools that support self-management, monitoring, and behaviour modification. It synthesizes evidence on features such as glucose tracking, personalised feedback, and integration with clinical workflows that aim to improve glycemic control and patient engagement. The review discusses benefits and limitations, noting variability in evidence quality and the need for long-term effectiveness studies. | Home-based digital technologies for managing type 2 diabetes. | Facilitates glucose and lifestyle monitoring; provides personalised feedback; enhances patient engagement | Type 2 diabetes home-based management | Self-management support; personalised monitoring; evidence variability and outcome gaps |
| [59] Jafari et al. | This systematic review examines the effect of home-based and remote exercises on low back pain during the COVID-19 pandemic, synthesizing evidence on pain reduction, functional improvement, and participation outcomes. It reviews mobile and remote exercise interventions that blend digital guidance, monitoring, and user engagement. The study highlights positive effects on pain and function, while noting heterogeneity in intervention designs and outcome measures. | Effects of home-based and remote exercise interventions for low back pain. | Supports pain reduction and functional improvement; utilises mobile guidance and engagement; notes intervention design variability | Low back pain management | Remote exercise benefits; mobile engagement features; heterogeneous outcomes |
| [60] Vijendran et al. | This systematic review evaluates the effectiveness of smartphone technology for detecting pediatric ocular diseases. It summarizes diagnostic accuracy, feasibility, and applicability of mobile-based imaging and AI-assisted analysis in clinical and remote settings. The review also discusses limitations related to validation, accessibility, and integration with existing ophthalmic care pathways. | Smartphone-based detection of pediatric eye diseases. | Enables early detection using mobile imaging; supports AI-assisted diagnostics; facilitates remote and clinical screening | Pediatric ophthalmology | Mobile diagnostic tools; AI-assisted evaluation; early detection potential |
| [61] Andrade & Viñán-Ludeña | This comprehensive review maps research on ICT addiction, covering internet, smartphone, social media, and gaming addictions. It synthesizes evidence on assessment methods, prevalence, risk factors, and interventions, highlighting trends in measurement and prevention. The review also notes gaps in standardization and longitudinal studies to assess long-term outcomes. | ICT addiction, including internet, smartphone, social media, and gaming. | Summarizes assessment and intervention strategies; identifies prevalence and risk factors; highlights research gaps in standardization | Behavioral and mental health | Technology use patterns; risk and prevalence mapping; intervention development |
| [62] Sylla et al. | This rapid systematic review examines 25 years of digital health progress in low- and middle-income countries toward universal health coverage. It highlights the role of mobile and AI-enabled tools in improving access, quality, and efficiency of healthcare delivery. The review discusses implementation challenges, equity issues, and lessons learned from large-scale digital health initiatives. | Digital health in LMICs for universal health coverage. | Enhances access and healthcare efficiency; supports AI and mobile interventions; identifies barriers to scaling and equity | Global health/LMICs | Digital health adoption trends; AI and mobile integration; coverage and equity challenges |
| [63] Schaap et al. | This scoping review assesses the suitability of just-in-time adaptive interventions (JITAIs) for post-COVID-19-related symptoms. It synthesizes evidence on mobile and AI-enabled interventions delivering tailored, real-time support to patients. The review notes effectiveness in symptom monitoring and personalized feedback, while also highlighting design, engagement, and evaluation challenges. | Just-in-time adaptive interventions for post-COVID-19 symptoms. | Provides real-time adaptive support; monitors symptoms and offers feedback; uses mobile and AI tools for personalization | Post-COVID symptom management | Personalized intervention delivery; mobile and AI application; engagement and feasibility issues |
| [64] Zhuang et al. | This systematic review and meta-analysis evaluates digital health interventions for chronic obstructive pulmonary disease (COPD). It synthesizes evidence on mobile apps, remote monitoring, and AI-driven management tools, assessing impact on clinical outcomes and patient adherence. The review highlights benefits in self-management and symptom tracking, while noting variability in intervention designs and evidence quality. | Digital health interventions for COPD management. | Supports symptom monitoring and self-management; AI aids in risk prediction and adherence; facilitates remote patient care | COPD | Remote monitoring and management; AI-assisted decision support; intervention variability |
| [65] Zhong et al. | This systematic review explores the use of digital phenotyping to differentiate unipolar depression from bipolar disorder. It examines smartphone and wearable data for behavioral, cognitive, and physiological markers that may improve diagnostic precision. The review discusses the potential for personalized assessment and early intervention, along with limitations in validation and standardization. | Digital phenotyping for mood disorder differentiation. | Enables behavioral and physiological monitoring; supports diagnostic precision; guides personalized mental health assessment | Mental health/Mood disorders | Digital phenotyping trends; AI-assisted differentiation; early intervention potential |
| [66] Kargarandehkordi et al. | This systematic review investigates the integration of wearable biosensors with AI for mental health monitoring. It summarizes applications in detecting stress, anxiety, and mood disorders through physiological and behavioral data. The review highlights opportunities for continuous monitoring and personalized interventions, while noting challenges in data quality, algorithm validation, and clinical adoption. | Wearable biosensors combined with AI for mental health monitoring. | Provides continuous physiological and behavioral monitoring; supports early detection of mental health conditions; enables personalized interventions | Mental health/Wearables | Wearable-AI integration; continuous monitoring; early detection and personalization |
| [67] Melia et al. | This review examines applications of AI to ecological momentary assessment (EMA) data in suicide research. It synthesizes methods for predicting suicidal ideation and behavior using real-time digital and mobile data. The review emphasizes opportunities for early risk detection and intervention planning, alongside ethical, privacy, and methodological challenges. | AI applied to EMA data for suicide research. | Predicts suicidal ideation and behavior; supports real-time monitoring and intervention; highlights ethical and methodological considerations | Suicide prevention/Mental health | EMA-based prediction; AI-assisted risk assessment; privacy and ethics concerns |
| [68] Woll et al. | This systematic review evaluates AI applications in linking device-based physical activity assessment with mental health outcomes. It synthesizes evidence on machine learning approaches to analyze activity patterns and predict psychological well-being. The review notes potential for personalized interventions, monitoring, and mental health promotion, as well as challenges in study design and data integration. | AI and device-based physical activity assessment for mental health. | Correlates activity data with mental health outcomes; supports personalized intervention design; utilizes AI for behavioral pattern analysis | Physical activity and mental health | Activity-mental health correlations; AI-assisted monitoring; personalized intervention insights |
| [69] Dehbozorgi et al. | This systematic review investigates AI applications in mental health, covering diagnosis, treatment, monitoring, and prediction. It synthesizes evidence from diverse tools including mobile apps, wearables, and predictive algorithms, highlighting clinical and methodological contributions. The review also discusses limitations in implementation, validation, and scalability, emphasizing the need for robust evidence before clinical deployment. | AI applications in mental health care. | Supports diagnosis, monitoring, and treatment; utilizes predictive algorithms and mobile tools; highlights clinical and methodological contributions | Mental health care | AI-enabled interventions; remote monitoring; evidence gaps and implementation challenges |
| [70] van Genugten et al. | This systematic review qualitatively examines the current state of just-in-time adaptive interventions (JITAIs) in mental health. It evaluates design, implementation, and effectiveness, highlighting challenges and opportunities for personalized digital interventions. The review also identifies areas for methodological improvements and future research directions. | Just-in-time adaptive interventions for mental health. | Supports real-time, personalized mental health interventions; highlights design and implementation strategies; provides guidance for future development | Mental health | JITAI design trends; implementation challenges; personalized intervention approaches |
| [71] Abdulazeem et al. | This bibliometric analysis and report reviews the use of digital health technologies for dementia care. It summarizes research trends, intervention types, and adoption patterns, emphasizing AI and mobile solutions for monitoring, support, and caregiver assistance. The review also identifies gaps in accessibility, evaluation, and long-term outcomes. | Digital health technologies in dementia care. | Supports remote monitoring and caregiver support; highlights AI-enabled dementia interventions; maps research trends and adoption patterns | Dementia care | Technology adoption trends; AI applications; research and evaluation gaps |
| [72] Pan et al. | This bibliometric analysis examines the application of artificial intelligence in chronic disease management. It evaluates trends in AI tools for risk prediction, monitoring, and personalized interventions. The review also discusses adoption barriers, research hotspots, and integration with digital health platforms. | AI for chronic disease health management. | Enables monitoring and risk prediction; supports personalized care; highlights adoption and research trends | Chronic disease management | AI-assisted monitoring; personalized intervention applications; research hotspots and trends |
| [73] Genovese et al. | This systematic review investigates AI applications in clinical language translation and interpretation. It evaluates performance, usability, and integration of AI tools to support patient-provider communication. The review also identifies challenges in accuracy, clinical adoption, and cross-cultural considerations. | AI for language translation and interpretation in clinical settings. | Facilitates patient-provider communication; improves accessibility for multilingual populations; supports clinical decision-making | Clinical communication | AI-assisted translation tools; multilingual clinical applications; accuracy and adoption challenges |
| [74] Akbarian et al. | This systematic review examines features and technologies used in mobile health applications for inflammatory bowel disease. It synthesizes evidence on symptom tracking, monitoring, and patient self-management functionalities. The review also highlights gaps in integration, usability, and personalization of interventions. | mHealth apps for inflammatory bowel disease management. | Supports symptom monitoring and self-management; facilitates patient engagement; integrates mobile and AI functionalities | Inflammatory bowel disease | App feature trends; self-management support; gaps in personalization and usability |
| [75] Bernard et al. | This systematic review evaluates self-management support apps for individuals with spinal cord injury. It analyzes app functionalities, usability, and evidence for improving patient outcomes. The review also identifies barriers to adoption and potential enhancements for accessibility and engagement. | Self-management support apps for spinal cord injury. | Facilitates remote self-management and monitoring; provides educational and motivational support; highlights usability and accessibility issues | Spinal cord injury | App functionality trends; remote self-management; usability and engagement considerations |
| [76] Gao et al. | This meta-analysis investigates AI-based facial recognition for detecting obstructive sleep apnea. It synthesizes diagnostic accuracy, validation methods, and clinical applicability of AI algorithms. The review highlights opportunities for non-invasive, rapid screening while noting limitations in generalizability and standardization. | AI facial recognition for obstructive sleep apnea detection. | Enables non-invasive screening; supports AI-assisted diagnosis; provides rapid risk assessment | Sleep disorders/Obstructive sleep apnea | AI diagnostic trends; non-invasive screening; standardization challenges |
| Macro Area | Included Studies | Evidence Maturity Level | Typical Interventions/Focus | Notes/Research Gaps | Key Studies [ ] |
|---|---|---|---|---|---|
| Mental Health & Well-being | 12 | Developing | AI for predicting mental health symptoms, stress, mood disorders; conversational agents; Just-in-Time adaptive interventions | Emerging interest in personalized, proactive interventions; need more real-world evaluation | [21,31,41,48,61,63,65,66,67,68,69,70] |
| Disease Prevention & Management | 5 | Developing | mHealth apps for chronic disease prevention (diabetes, domestic violence, rehabilitation, Alzheimer’s monitoring) | Evidence fragmented; heterogeneous outcomes; limited AI integration | [22,35,40,50,52] |
| AI & Mobile Health Technologies | 5 | Emerging | Frameworks for AI-enabled mHealth app development, assessment of chatbots and COVID-19 detection apps | Methodological guidance still underdeveloped; limited empirical evaluation | [32,33,36,38,39] |
| Cancer & Oral Health | 5 | Developing | AI for oral cancer detection, dental caries, self-monitoring via smartphone images | Mostly early-stage studies; few large-scale validations | [23,25,27,45,49] |
| Chronic Diseases & Diagnostics | 11 | Developing | AI in diabetic retinopathy, sleep apnea, COPD, fall detection, pediatric eye screening | Need standardized datasets; cross-platform integration; longitudinal studies | [30,43,47,54,55,58,60,64,72,74,76] |
| Health Data & Outcome Measurement | 4 | Emerging | Patient-generated data for real-world outcomes, cognitive support apps | Limited data on long-term impact; interoperability challenges | [38,42,50,71] |
| Workplace Health | 1 | Emerging | AI for health promotion and prevention in occupational settings | Few studies; more evidence needed across diverse workplaces | [28] |
| Health Technologies & Innovations | 5 | Developing | Remote rehabilitation, markerless motion capture, pain management, spinal cord injury apps | Evidence growing but heterogeneous; standardization lacking | [24,46,51,59,75] |
| Healthcare Technology Integration | 4 | Emerging | Telehealth, remote monitoring, AI translation tools | Integration into clinical workflows underexplored | [44,53,56,73] |
| Technology for Medication Adherence | 1 | Emerging | mHealth apps for oral anticancer therapy adherence | Limited to specific conditions; broader applicability unclear | [29] |
| Nutrition & Health | 1 | Emerging | Apps for nutritional support and dietary management | Evidence sparse; outcomes not standardized | [34] |
| Public Health | 3 | Emerging | mHealth for violence prevention, low-income country coverage | Early-stage implementation; scaling challenges | [52,57,62] |
| Study | Opportunities | Areas Needing Broader Investigation |
|---|---|---|
| [21] | AI and mHealth platforms present valuable opportunities for predicting and managing mental health conditions such as anxiety, stress, and depression, particularly in youth. Real-time monitoring can provide timely interventions, improving mental well-being. | Privacy concerns are significant, as mental health data is highly sensitive. Furthermore, accessibility remains a challenge, especially in marginalized communities with limited access to mobile technologies. |
| [22] | AI can facilitate the early detection, diagnosis, and management of neglected tropical diseases (NTDs), particularly in resource-limited settings. Mobile apps help expand reach, improving pandemic preparedness and surveillance. | Low-tech infrastructure in many parts of the world can hinder the implementation of AI-powered health solutions. Furthermore, integrating these technologies into already strained healthcare systems remains a considerable challenge. |
| [23] | AI applications in oral health can enable early diagnosis of oral cancer and improve the detection of dental conditions such as caries. Mobile platforms can empower individuals to self-monitor, enhancing preventive care. | Despite the promise, there is resistance to integrating AI into traditional dental practices, and limited data hinders the development of robust AI tools. Additionally, costs may be prohibitive for some dental practices. |
| [24] | AI-powered mobile apps for patient monitoring can track chronic conditions like diabetes and hypertension, allowing for more personalized and proactive care. These tools provide valuable insights for both patients and healthcare providers. | Security and privacy concerns are a major challenge when handling sensitive health data. Inaccuracies in symptom tracking can also result in improper interventions or unnecessary healthcare costs. |
| [25] | AI in dental care can improve the diagnosis of dental diseases and promote preventive care. Mobile technologies enable continuous monitoring, fostering a more patient-centered and proactive approach to oral health management. | Patient engagement with AI tools in dental health is limited, and skepticism remains around their effectiveness. Additionally, regulatory hurdles exist in ensuring these tools meet medical standards. |
| [26] | AI offers substantial promise for improving diagnostic accuracy and streamlining healthcare practices, particularly for chronic disease management. Mobile health technologies also promote self-monitoring and timely intervention. | Over-reliance on AI systems in diagnostics can be problematic, particularly if clinical oversight is inadequate. Furthermore, integrating AI into healthcare systems without disrupting existing practices remains a significant challenge. |
| [27] | AI can improve the early diagnosis of oral health issues, by analyzing oral photographs and other diagnostic tools. This could significantly enhance early-stage detection and patient outcomes. | Challenges include insufficient validation data, especially regarding long-term accuracy, and resistance to adopting AI-based tools within traditional dental settings. |
| [28] | AI can assist in chronic disease management by providing personalized treatment plans and continuously monitoring health metrics. AI supports individualized health programs, while mHealth platforms extend interventions to underserved groups. | Data accuracy is crucial for effective AI-powered interventions, and patient adherence to these tools can be inconsistent. Furthermore, issues related to regulatory approval and integration into clinical practice remain. Limited evidence on AI’s broader applicability and concerns over data privacy and ethical implementation. |
| [29] | AI-based mobile health applications enable real-time symptom tracking and personalized health management, especially for chronic conditions. They can also enhance medication adherence and reduce hospital visits as in the case in anticancer oral medications. | User data privacy remains a significant concern, as sensitive health information is collected. There is also a need for further research to demonstrate the clinical efficacy of these AI-driven mobile apps. |
| [30] | AI in mobile health is revolutionizing patient monitoring and health management, especially for chronic diseases (including ophthalmology). It allows for continuous feedback, enabling more precise interventions and improving patient outcomes. | Potential challenges include insufficient patient engagement, inaccuracies in symptom tracking, and privacy concerns regarding the handling of sensitive health data. |
| [31] | AI can provide real-time interventions for mental health, offering tailored strategies for managing stress and promoting overall well-being. The focus on youth mental health is particularly promising. | Privacy and security concerns are prominent, as mental health data is especially sensitive. Additionally, achieving equitable access across diverse populations remains a challenge. |
| [32] | AI has the potential to enhance telehealth services, improving patient access and streamlining healthcare delivery. AI-powered systems can also enhance remote consultations, making healthcare more efficient. | Barriers include regulatory challenges, particularly with regard to cross-border healthcare delivery. There are also concerns about trust and reliance on AI systems for critical healthcare decisions. |
| [33] | The integration of AI into telehealth could transform healthcare systems, improving efficiency, access, and patient outcomes. Generative AI models automate the extraction, classification, and synthesis of data from mHealth app reviews. AI can assist in creating structured summaries, identifying trends, and highlighting key functionalities across various mHealth apps. | Ethical concerns about AI’s decision-making in healthcare, accountability, and the potential for biased systems need to be addressed. Legal frameworks for AI in healthcare are also still developing. Ensuring the AI tools are accurate and unbiased, and managing the complexity of app diversity and rapid development in the mHealth sector. |
| [34] | AI applications in chronic disease prevention and management can lead to personalized health plans, promoting healthier lifestyles and preventing diseases like diabetes and cardiovascular conditions. | Achieving consistent patient engagement and overcoming data privacy concerns are key obstacles. Additionally, ensuring regulatory compliance for AI applications in healthcare is an ongoing challenge. |
| [35] | AI-powered apps provide opportunities for preventing and managing chronic diseases by offering personalized recommendations, including lifestyle and dietary interventions, ultimately reducing healthcare costs. | Integration of AI into clinical workflows remains a challenge, as healthcare professionals may be hesitant to adopt AI tools. Moreover, ensuring these apps are both scientifically valid and effective is crucial for widespread acceptance. |
| [36] | AI-driven mobile apps provide new ways to manage infectious diseases through early detection, real-time monitoring, and surveillance. This has proven particularly valuable in the context of pandemics, such as COVID-19. | Variability in data quality across regions poses a challenge for AI’s effectiveness in disease management. Moreover, patient trust in AI-driven tools during health crises can be difficult to establish. |
| [37] | AI integration, including in telehealth platforms, has the potential to improve efficiency, reduce administrative costs, and enhance patient care. Real-time data processing can lead to more accurate diagnoses and treatments. AI-based simplification tools can enhance the accessibility of health information for patients and caregivers. | Resistance from healthcare workers and patients to AI-powered healthcare systems is a significant barrier, and ensuring these systems are secure and trustworthy is crucial. |
| [38] | AI can play a pivotal role in personalized treatment and monitoring of chronic conditions, leading to better management and reduced healthcare costs. Continuous monitoring through mobile health tools can facilitate early interventions. Chatbots are a promising tool for delivering accessible and personalized health interventions. | Data security and privacy concerns remain one of the primary obstacles. Additionally, AI systems must be properly calibrated to avoid misdiagnoses or ineffective interventions. |
| [39] | AI holds immense potential in health monitoring, offering tools for detecting and managing health conditions. DTC AI apps provide consumers with the potential for real-time health monitoring and diagnosis, improving health management. | Ethical issues related to AI decision-making, require careful consideration. Risks include data privacy issues, the accuracy of AI-driven diagnoses, and the need to ensure users’ trust in these technologies. |
| [40] | AI-driven rehabilitation technologies, such as markerless motion capture, enable more personalized and efficient physical therapy. These tools have the potential to significantly improve rehabilitation outcomes. | Resistance to new technologies, especially in the rehabilitation field, can delay adoption. Furthermore, clinical validation and integration into existing rehabilitation practices are necessary for success. |
| [41] | mHealth technologies, such as apps and social media platforms, integrated with AI to deliver interventions for tobacco cessation have potential. Conversational AI interventions hold promise for increasing smoking cessation rates in large populations. | Clinician trust in AI tools remains a barrier, as there may be concerns over their reliability in critical healthcare settings. High heterogeneity across studies, varying methodologies, and high participant dropout rates. More consistent and standardized trials are needed. |
| [42] | AI technologies in mobile health provide continuous patient monitoring, leading to better management of chronic conditions. These platforms offer real-time interventions and personalized care, improving long-term health outcomes. Real-world clinical data collected through DHTs can significantly enhance patient care and health monitoring. | Ensuring data privacy and security in mobile health tools is a major concern. Moreover, inconsistent user adherence to these technologies can hinder their effectiveness in long-term care. The need for more rigorous studies to validate the reliability of real-world data and ensure its integration into clinical decision-making. |
| [43] | Smartphone-based AI tools offer a promising solution for mass screening of diabetic retinopathy in low-resource settings. Mobile technologies promote preventive care by enabling mass screaning. | Further high-quality studies are needed to validate these tools in real-world clinical environments and ensure their effectiveness. Additionally, insufficient data availability limits the effectiveness of AI systems in certain applications. |
| [44] | AI has the potential to transform infectious disease management by enabling earlier detection, diagnosis, and real-time monitoring through mobile apps. This could significantly improve response times in pandemics. | Challenges include ensuring widespread accessibility of mobile health tools in low-resource settings and maintaining the accuracy of AI systems in diverse epidemiological environments. |
| [45] | mHealth apps can be an accessible, low-cost solution for improving oral health education and prevention. These apps provide users with valuable resources such as instructional videos, reminders for oral hygiene routines, and tips for maintaining healthy teeth | Ethical concerns around data usage, privacy, and AI’s decision-making processes need to be carefully addressed. Furthermore, ensuring that AI systems do not perpetuate existing biases in healthcare is a major concern. |
| [46] | AI-driven innovations in healthcare show promise in transforming disease prevention and management, including new applications for cognitive health and innovative pain management solutions. | Regulatory, ethical, and technical hurdles need to be overcome before these innovations can be implemented widely. The integration of these technologies into existing healthcare practices is also a significant challenge. |
| [47] | These digital tools could offer cost-effective, scalable solutions for OSA screening and diagnosis, particularly in underserved populations. They provide the opportunity for continuous, at-home monitoring, enabling earlier intervention and personalized care. | The tools still face challenges in terms of external validation and generalizability. Many studies have only validated models internally, and there is a need for further comparison with polysomnography across diverse populations and clinical environments. Additionally, technical limitations in sensor accuracy and data analysis may hinder full adoption. |
| [48] | AI-driven health applications in mental health management can help predict and prevent mental health crises. These apps can support early interventions for individuals at risk. | Privacy concerns are paramount when dealing with mental health data, and patient engagement with digital tools can vary, affecting their long-term impact. |
| [49] | AI applications in dental care can lead to more precise diagnoses and earlier interventions, improving patient outcomes. Mobile tools support self-care and early detection of dental issues. | The lack of sufficient clinical evidence to support AI’s efficacy in dental practice remains an issue, along with concerns regarding patient privacy and data security. |
| [50] | Emerging AI technologies in healthcare offer opportunities for advancements in AD. mHealth apps and AI can collect continuous data on cognitive performance and behavioral changes, allowing for passive monitoring and early identification of cognitive decline in individuals at risk of AD. | Regulatory barriers, including the need for thorough clinical validation of AI tools, remain a significant challenge. Moreover, concerns about patient data privacy and ethical decision-making persist. |
| [51] | AI technologies in physical rehabilitation, such as markerless motion capture, enable personalized therapy and more efficient recovery. These tools can significantly improve patient outcomes. | The adoption of AI in rehabilitation is slow due to a lack of clinician trust in the technology, and the need for comprehensive clinical trials to validate its efficacy remains a challenge. |
| [52] | mHealth apps provide emergency assistance, awareness, and legal information to potential victims of domestic violence, enabling discreet and accessible support. AI could enhance the functionality of these apps by incorporating features like speech recognition, sentiment analysis, and real-time emergency alerts based on audio cues. | Data security and privacy concerns continue to be significant, and integrating these technologies. The current lack of automation and AI integration in existing apps. |
| [53] | Telehealth startups are pivotal in offering teleconsultations, telemonitoring, and electronic health records solutions, focusing on mobile health applications and AI-driven personalized care. AI enhances telehealth through personalized care, digital therapeutics, and the development of wearable device technologies, optimizing healthcare delivery. | Ethical concerns about data usage, privacy, and AI’s role in healthcare decisions must be addressed to ensure equitable and fair healthcare delivery. Key challenges include infrastructure limitations, regulatory hurdles, and ensuring sustainable revenue generation models for telehealth startups. |
| [54] | AI applications in surgical settings can improve diagnostic accuracy and support surgical decision-making. AI and mobile health solutions offer significant opportunities in reducing healthcare costs, improving patient outcomes, and enhancing infection prevention practices. | The challenge of clinician acceptance and ensuring AI systems integrate seamlessly into existing clinical workflows remains a major obstacle. Standardizing data management, integrating DDTs with existing systems, and ensuring patient data security remain major challenges. Additionally, maintaining patient trust is crucial. |
| [55] | AI-powered mobile health tools enable more effective management of chronic conditions and improve medication adherence. These technologies offer personalized care and are scalable for widespread use. Smartphone-based fall detection systems provide an opportunity to improve elderly care by enabling real-time intervention and reducing healthcare costs. | Inconsistent adherence to digital health tools by patients is a challenge, as is ensuring the accuracy of data collected through these platforms. Adoption is limited due to technological barriers, such as sensor reliability, and reluctance from older adults to embrace new technologies. |
| [56] | AI can optimize healthcare systems by improving diagnostics and streamlining care processes, ultimately enhancing patient outcomes and reducing costs. | Challenges include the need for standardization in data collection methods, integrating multiple data sources, and improving diagnostic accuracy. |
| [57] | Mobile apps provide immediate access to resources and support for preventing violence against women, empowering users with education, safety planning, and emergency contacts. They can raise awareness and foster community engagement. | Ensuring widespread accessibility across different regions and demographics, maintaining user privacy and data security, and guaranteeing timely and reliable emergency responses remain significant hurdles. Cultural sensitivities and trust-building are also critical. |
| [58] | AI-driven digital diabetes management allows personalized treatment plans, continuous glucose monitoring, and lifestyle coaching at home, improving adherence and health outcomes. It enables scalable chronic disease care beyond clinical settings. | Challenges include ensuring accuracy of self-reported and sensor data, sustaining patient engagement over long periods, integrating AI tools with traditional healthcare providers, and addressing disparities in technology access. |
| [59] | Home-based and remote exercise interventions supported by digital tools offer safe rehabilitation during pandemics or mobility constraints, enabling continuous care, pain management, and improved physical function. | Barriers include technological literacy of patients, variable internet connectivity, lack of personalized supervision, and difficulties in monitoring and motivating patients remotely to ensure adherence and effectiveness. |
| [60] | AI-powered smartphone applications can enable early and affordable detection of pediatric ocular diseases, improving access in low-resource settings, and potentially reducing preventable vision loss through timely referrals. | Validating AI diagnostic accuracy in diverse populations, training non-specialist users, ensuring follow-up care, and managing ethical issues related to data privacy and consent pose ongoing challenges. |
| [61] | Digital tools offer potential for monitoring and intervention in ICT addiction (internet, smartphone, gaming), supporting self-regulation, psychoeducation, and behavioral therapy enhancements via AI personalization. | Risks include the paradoxical effect of increasing screen time, managing user engagement, addressing the stigma associated with addiction, and ensuring interventions are evidence-based and tailored to individual needs. |
| [62] | Digital health technologies can significantly enhance healthcare delivery in low- and middle-income countries, promoting universal health coverage by overcoming geographical and resource barriers with mobile solutions. | Infrastructure deficits, sustainability of programs, socio-cultural adaptation, regulatory challenges, and digital literacy disparities remain substantial obstacles to widespread adoption. |
| [63] | Just-in-time adaptive interventions (JITAI) can provide personalized, context-aware support to patients recovering from COVID-19, improving symptom management and quality of life through timely, adaptive feedback. | Challenges include ensuring real-time data reliability, protecting patient privacy, maintaining user engagement, and rigorously validating intervention efficacy in diverse populations. |
| [64] | Digital health interventions enable continuous monitoring and management of COPD symptoms, facilitate remote consultations, and support patient self-management, potentially reducing exacerbations and hospitalizations. | User adherence over time, integration into clinical workflows, interoperability with healthcare systems, and data security concerns must be addressed to maximize effectiveness. |
| [65] | Digital phenotyping through AI offers non-invasive methods for distinguishing unipolar depression from bipolar disorder, enabling earlier and more accurate diagnosis and personalized treatment plans. | Privacy and ethical concerns about continuous monitoring, data interpretation challenges, risk of misclassification, and the potential for stigmatization require careful management. |
| [66] | Wearable biosensors fused with AI provide real-time monitoring of mental health states, enabling timely interventions, personalized care, and better understanding of physiological correlates of mental health. | Ensuring sensor accuracy and reliability, maintaining user comfort and compliance, ethical management of sensitive physiological data, and integrating findings into clinical practice are key challenges. |
| [67] | AI applied to ecological momentary assessment data can improve suicide risk prediction by analyzing real-time mood and behavior patterns, potentially enabling preventive interventions and saving lives. | Managing false positives and negatives, respecting privacy and consent, ensuring patient engagement, and avoiding over-reliance on automated predictions present ongoing difficulties. |
| [68] | Device-based physical activity assessment combined with AI can tailor interventions to improve mental health by encouraging physical activity and tracking emotional well-being in a personalized manner. | Maintaining motivation and adherence, ensuring accuracy of mood and activity detection, integrating recommendations into everyday life, and protecting user data are significant challenges. |
| [69] | AI applications in mental health span diagnosis, treatment, and support, enhancing clinical decision-making, improving access to care, and enabling personalized interventions. | Clinical validation, overcoming biases in AI models, ensuring transparency and explainability, and integrating tools seamlessly into healthcare systems remain hurdles. |
| [70] | Advanced just-in-time adaptive interventions can offer personalized, context-sensitive support for mental health, enhancing engagement and treatment outcomes by delivering the right intervention at the right time. | Algorithmic complexity, safeguarding data privacy, adapting to diverse user contexts and needs, and ensuring equitable access require ongoing research and development. |
| [71] | Digital health technologies for dementia care provide tools for symptom monitoring, cognitive support, and caregiver assistance, improving quality of life and potentially delaying institutionalization. | Ensuring usability for elderly populations, addressing technological acceptance and training needs, managing privacy and data protection, and ensuring affordability and accessibility pose challenges. |
| [72] | AI enables enhanced chronic disease health management by supporting risk prediction, treatment personalization, and efficient resource allocation, improving patient outcomes and system sustainability. | Integrating data from heterogeneous sources, clinical adoption barriers, ethical considerations, and ensuring equitable access across different populations are key concerns. |
| [73] | AI-driven language translation and interpretation in clinical settings can overcome communication barriers, improving patient-provider interactions, reducing errors, and enhancing care quality. | Ensuring translation accuracy, maintaining cultural sensitivity, securing patient data, and achieving provider and patient acceptance are important challenges. |
| [74] | Mobile health apps for inflammatory bowel disease empower patients with symptom tracking, medication reminders, and educational content, fostering self-management and improved outcomes. | Sustaining user engagement, ensuring data accuracy and reliability, integration with healthcare provider systems, and addressing privacy concerns are ongoing challenges. |
| [75] | Self-management support apps for spinal cord injury patients facilitate personalized rehabilitation, promote autonomy, and improve quality of life through tailored interventions and monitoring. | Adapting interventions to diverse functional levels, ensuring accessibility and usability, managing technological complexity, and maintaining patient motivation are key issues. |
| [76] | AI-based facial recognition technology offers a non-invasive, accessible screening tool for obstructive sleep apnea, potentially enabling early detection and intervention. | Validation of screening accuracy across populations, privacy and ethical concerns regarding biometric data, and integration into standard clinical pathways remain challenges. |
| [Ref.] First Author (Year; Country) Title | Medical Device Characteristics Database of Registration Device Name-Risk Class Code (Nomenclature Code(s) for EUDAMED; CND for Italian Database) Manufacturer (Country)–Link DESCRIPTION |
|---|---|
| [86] Veyron JH et al. (2024; France) Postimplementation Evaluation in Assisted Living Facilities of an eHealth Medical Device Developed to Predict and Avoid Unplanned Hospitalizations: Pragmatic Trial | Registered in EUDAMED Presage Care—Class I Code: 40192-General medicine diagnosis and monitoring instruments-medical device software Manufacturer: PRESAGE (FR)—https://presage.care/, accessed on 28 July 2025 Market distribution: Belgium (from 3 April 2023 to 30 November 2028); France (from 28 February 2020 to 30 November 2028) DESCRIPTION: Presage Care is a remote monitoring system for patients using electronic patient-reported outcome measures (data recorded by nurse assistants into a smartphone app) with a machine learning algorithm (resident to a secure server) to predict the risk of emergency hospitalizations with a prediction window of 7–14 days. The smartphone app belongs to the system, but the machine learning algorithm is not a built-in algorithm. |
| [87] Karakoyun et al. (2021; Germany) Digital Medical Device Companion (MyIUS) for New Users of Intrauterine Systems: App Development Study | Registered in EUDAMED MyIUS—Class IIa Code: V92-Medical device software-not included in other classes Manufacturer: BAYOOCARE GmbH [DE]—https://www.bayoocare.com/en/myius/, accessed on 28 July 2025 Market distribution: Belgium; Czechia; Denmark; Germany; Netherlands; Poland; Portugal; Sweden. DESCRIPTION: This device is a mobile phone–based medical app, that “uses an artificial intelligence–based bleeding pattern prediction algorithm to estimate a woman’s future bleeding pattern in terms of intensity and regularity” (citation from paper). This app supports the women after the placement of an intrauterine system, by recording menstrual bleeding information into a daily diary and predicting future bleeding patterns. From paper you can read, “The app is available free of charge in the App Store (Apple Inc) and Google Play Store (Google LLC)”. |
| [88] Atee et al. (2018; Australia) Technical Note on the PainChek™ System: A Web Portal and Mobile Medical Device for Assessing Pain in People With Dementia | Registered in the Italian Database PAINCHEK APP—Class I Code: Z12040282-General medicine therapeutic treatment instruments-software accessories Manufacturer: PAINCHEK LTD [AU]—https://www.painchek.com/, accessed on 28 July 2025 Representative (for non-European manufacturers): DONAWA LIFESCIENCE CONSULTING SRL [IT] Market distribution: Australia, United Kingdom, European Union (Italy from 17 October 2020), and other jurisdictions. DESCRIPTION: From the paper you can read, “Using the smart-device camera to capture a short video of a person’s face, the App automatically identifies the face in real time, then maps the face to analyze facial expressions (using a built-in AI algorithm) indicative of the presence of pain”. |
| Ref. First Author (Year; Country) Title | Regulation Issue | Description of the Study |
|---|---|---|
| [94] Shah SFH (2025; UK) Ethical implications of artificial intelligence in skin cancer diagnostics: use-case analyses | Efficacy and safety (Robustness and safety: ethical issues) and accountability (accountability: legal issue) | Analysis of the ethical issues in the use cases of two commercial mobile applications in the UK for artificial intelligence-assisted skin cancer diagnosis aimed at patients (SkinVision and Scanoma). The authors identified specific issues related to the development and use of each app. Of the two, only one app provided detailed information about how it works and how it was developed. However, for both apps, the issues identified related to the number, quality, and consistency of studies evaluating the effectiveness of the algorithm, as well as potential skin-tone biases that could lead to the exclusion of individuals with darker skin tones as target users. To make apps safer and more useful for all, the authors recommend more effective regulation to increase vendor accountability and ensure ethics by design through integration between developers, dermatologists, ethicists, and users. SkinVision (https://www.skinvision.com, accessed on 28 July 2025), available for download in Europe, Australia and New Zealand, is classified as a class I mark medical device in the European Union (EU) and Australia. Scanoma (https://www.scanoma.com, accessed on 28 July 2025), available for download in Australia, UK and US, is classified as a class I mark medical device in Australia. |
| [95] Späth J (2024; Germany, France, Spain) Privacy-Preserving Federated Survival Support Vector Machines for Cross-Institutional Time-To-Event Analysis: Algorithm Development and Validation | Data privacy (Privacy and security) | This study develops and validates a privacy-preserving federated survival support vector machine (SVM) designed for cross-institutional time-to-event analyses in medical research. The algorithm, implemented as a freely accessible app on the FeatureCloud platform, yields results very similar to centralized models, demonstrating high accuracy and robustness, even with site-dependent variations. This approach offers a valuable tool for collaborative research while respecting strict privacy regulations. |
| [96] Zawati MH (2024; Canada) Does an App a Day Keep the Doctor Away? AI Symptom Checker Applications, Entrenched Bias, and Professional Responsibility | Entrenched bias (Fairness and inclusiveness; ethical issue) and professional accountability (Accountability; legal issue) | This paper discusses the ethical and legal challenges of AI-powered symptom checker apps in mobile health, focusing on issues like bias from training data, demographic inequalities, and lack of regulation. Using examples like Babylon and Ada apps, it highlights concerns over entrenched biases and professional accountability, including uncertainties about safety reviews and liability. The authors emphasize the need for technical safeguards, neutral data training, and effective regulation to ensure these apps are safe, fair, and transparent, underscoring that addressing these issues is crucial for responsible development and deployment of AI in healthcare. |
| [97] Wongvibulsin S (2024; US) Current State of Dermatology Mobile Applications with Artificial Intelligence Features | Efficacy and safety (Robustness and safety), and transparency (Transparency and explainability) | An analysis of dermatology apps with artificial intelligence features available for download from the Apple and Android app stores was conducted. Forty-one apps were analyzed: 14 apps were based in the US, with only 2 providing a disclaimer for lacking US Food and Drug Administration approval; additionally, 14 apps were based in Europe, and only 2 possessed CE Mark (Conformité Européenne) status. Overall, the study found that the associated risks were a lack of consistent validation, transparency in algorithm development, user privacy and misleading user communication. To minimize risks, effective regulation is needed, including the establishment of standardized validation and evaluation criteria to ensure the efficacy, safety, and transparency of these applications. |
| [98] Alfano L (2024; Italy) Psychotherapy, artificial intelligence and adolescents: ethical aspects | Responsible implementation (Accountability), patient privacy (Privacy and security), and the human-AI interaction (Robustness and safety) | This article discusses the ethical considerations surrounding the use of AI in psychotherapy, emphasizing the need for careful regulation to ensure responsible implementation, patient safety and data privacy, and human-AI interaction. |
| [99] Ouellette S (2022; US) Usefulness of Smartphones in Dermatology: A US-Based Review | Regulation of health-related apps for diagnosing and treating diseases, such as medical devices (All the basic principles) | Review of the usefulness of mobile apps for dermatology, both for patients and providers. 15.7% of the apps analyzed used artificial intelligence. The article expresses concern about the lack of regulation of medical apps in the same way as medical devices, with the authors stating that the software function of apps used to diagnose and/or treat disease should be cleared by the FDA [79]. However, no skin cancer detection app appears to be regulated by the FDA and, unfortunately, is still freely available for download. |
| [100] Matin RN (2021; UK) AI-based smartphone apps for risk assessment of skin cancer need more evaluation and better regulation | Regulation of health-related apps for diagnosing and process of CE certification (All the basic principles) | The widespread adoption of artificial intelligence (AI)-based smartphone apps in healthcare must be supported by a strong scientific evidence base and properly regulated claims by app manufacturers. Unfortunately, current CE marking evaluation processes do not adequately protect the public from the risks of using these diagnostic apps, as many of these apps, when certified, turn out to be Class I medical devices, for which there is no need for independent regulatory review, as app developers “self-certify” and effectively apply the CE mark. In this scenario, the most “dangerous” apps are mainly those developed for dermatology, which, based on captured images of the skin and using machine learning techniques, give indications of suspicious lesions (skin cancer). |
| [101] Pashkov VM (2020; Ukraine) Artificial Intelligence in Medical Practice: Regulative Issues and Perspectives | Implementation of regulated AI in healthcare (All the basic principles) | This paper provides guidance for understanding the nature of AI in healthcare and the specifics of its regulation. The main issues related to the implementation of AI in healthcare stem from the nature of the technology itself and the complexity of ensuring legal support in terms of safety, efficacy, privacy, ethical issues and liability. The main challenge lies not in the technology, which is rapidly advancing and revealing new applications, but in the inadequacy of the existing legal framework. Indeed, one must ask whether the current legal framework is adequate to regulate AI in terms of safety, efficacy, and pre- and post-market monitoring, and to build a model of accountability in the context of AI use in healthcare. |
| [102] Martinez-Martin N (2018; US) Ethical Issues for Direct-to-Consumer Digital Psychotherapy Apps: Addressing Accountability, Data Protection, and Consent | Responsibilities and ethical obligations in artificial intelligence-led counseling and conversational agents in direct-to-consumer (DTC) digital psychotherapy (All the basic principles) | Direct-to-consumer (DTC) digital psychotherapy services that do not involve supervision by a mental health professional face many ethical challenges in protecting the person in therapy due to the lack of adequate regulation in this area. Indeed, there are no clear lines of accountability or associated ethical obligations to protect the user, his or her safety and privacy. This makes services that offer counseling guided by artificial intelligence and conversational agents even more problematic. |
| Standard | Title/Scope | Relevance to AI-Powered Health Apps | Notes | Ref |
|---|---|---|---|---|
| ISO/TS 82304-2:2021 | Health and wellness apps—Quality and reliability | Establishes requirements for health apps covering development, deployment, and lifecycle management | Useful for both consumer and clinically oriented apps, supports assessment and certification | [131] |
| IEC 82304-1:2016 | Health software—General requirements for product safety | Provides general safety requirements for standalone health software, including AI components | Complements SaMD regulatory frameworks; applicable when software functions independently from hardware | [132] |
| ISO/IEC 42001:2023 | AI Management Systems | Provides a framework for governance, transparency, risk management, and continuous improvement of AI systems | Supports safe and accountable deployment of AI in clinical contexts | [133] |
| ISO 13485:2016 | Medical devices—Quality management systems | Quality management system requirements for manufacturers of medical devices | Required if the app is classified as a medical device (SaMD); ensures consistency in production and documentation | [134] |
| ISO 14971:2019 | Medical devices—Risk management | Provides guidance for clinical risk assessment and mitigation | Critical for evaluating potential harms of AI-powered apps, including decision support features | [135] |
| Standard | Title/Scope | Relevance to AI-Powered Health Apps | Notes | Ref. |
|---|---|---|---|---|
| ISO/IEC 27001:2022 | Information security management systems | Establishes requirements for information security management, including risk assessment and mitigation | Essential for protecting patient data and AI algorithms in clinical settings | [136] |
| ISO/IEEE 11073-40101:2022 | Health informatics—Device interoperability—Cybersecurity—Vulnerability assessment processes | Provides processes for secure interoperability between devices and IT systems | Particularly relevant for apps interacting with sensors, wearables, or medical devices | [137] |
| IEC/TR 80002-1:2009 | Medical device software—Guidance on applying ISO 14971 to software | Guidance on applying risk management principles specifically to software | Supports safe deployment of AI-enabled apps within medical contexts | [138] |
| Standard/Guideline | Title/Scope | Relevance to AI-Powered Health Apps | Notes | Ref. |
|---|---|---|---|---|
| AAMI TIR 34971:2023 | Application of ISO 14971 to ML/AI | Provides guidance for risk management of AI/ML in medical devices | Directly relevant to AI-powered apps; ensures risk assessment covers adaptive algorithms | [139] |
| FG-AI4H DEL2.2:2022 | Good practices for health AI applications | Development, validation, and compliance framework for AI in health | Complements formal standards with practical guidance for clinical and consumer apps | [140] |
| Standard/Framework | Title/Scope | Relevance to AI-Powered Health Apps | Notes | Ref. |
|---|---|---|---|---|
| ISO/TS 82304-2:2021 | Health and wellness apps—Quality and reliability | Provides a structured approach for app assessment and potential certification | Supports evaluation for clinical and consumer-facing apps | [131] |
| ISO/IEC 42001:2023 | AI Management System | Facilitates continuous monitoring and governance of AI algorithms | Ensures responsible AI deployment and iterative improvement | [133] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Morelli, S.; Giansanti, D. Recent Advances in AI-Driven Mobile Health Enhancing Healthcare—Narrative Insights into Latest Progress. Bioengineering 2026, 13, 54. https://doi.org/10.3390/bioengineering13010054
Morelli S, Giansanti D. Recent Advances in AI-Driven Mobile Health Enhancing Healthcare—Narrative Insights into Latest Progress. Bioengineering. 2026; 13(1):54. https://doi.org/10.3390/bioengineering13010054
Chicago/Turabian StyleMorelli, Sandra, and Daniele Giansanti. 2026. "Recent Advances in AI-Driven Mobile Health Enhancing Healthcare—Narrative Insights into Latest Progress" Bioengineering 13, no. 1: 54. https://doi.org/10.3390/bioengineering13010054
APA StyleMorelli, S., & Giansanti, D. (2026). Recent Advances in AI-Driven Mobile Health Enhancing Healthcare—Narrative Insights into Latest Progress. Bioengineering, 13(1), 54. https://doi.org/10.3390/bioengineering13010054







