Clinical Efficacy and Safety of Two Cycles of Intra-Articular Injection of Porcine Atelocollagen Versus Hyaluronic Acid in Knee Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Participants and Eligibility Criteria
2.3. Interventions and Injection Protocol
2.4. Follow-Up Schedule and Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
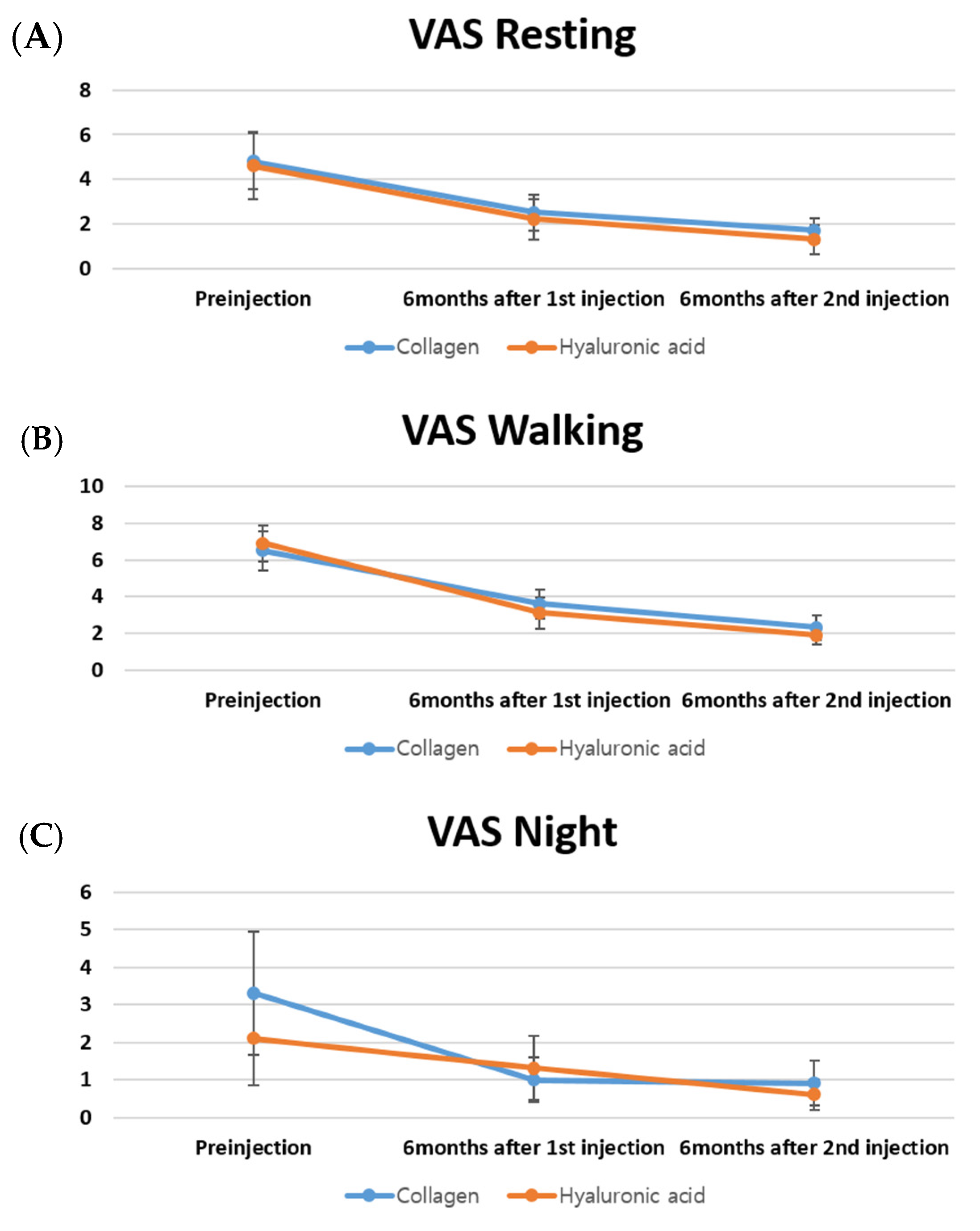
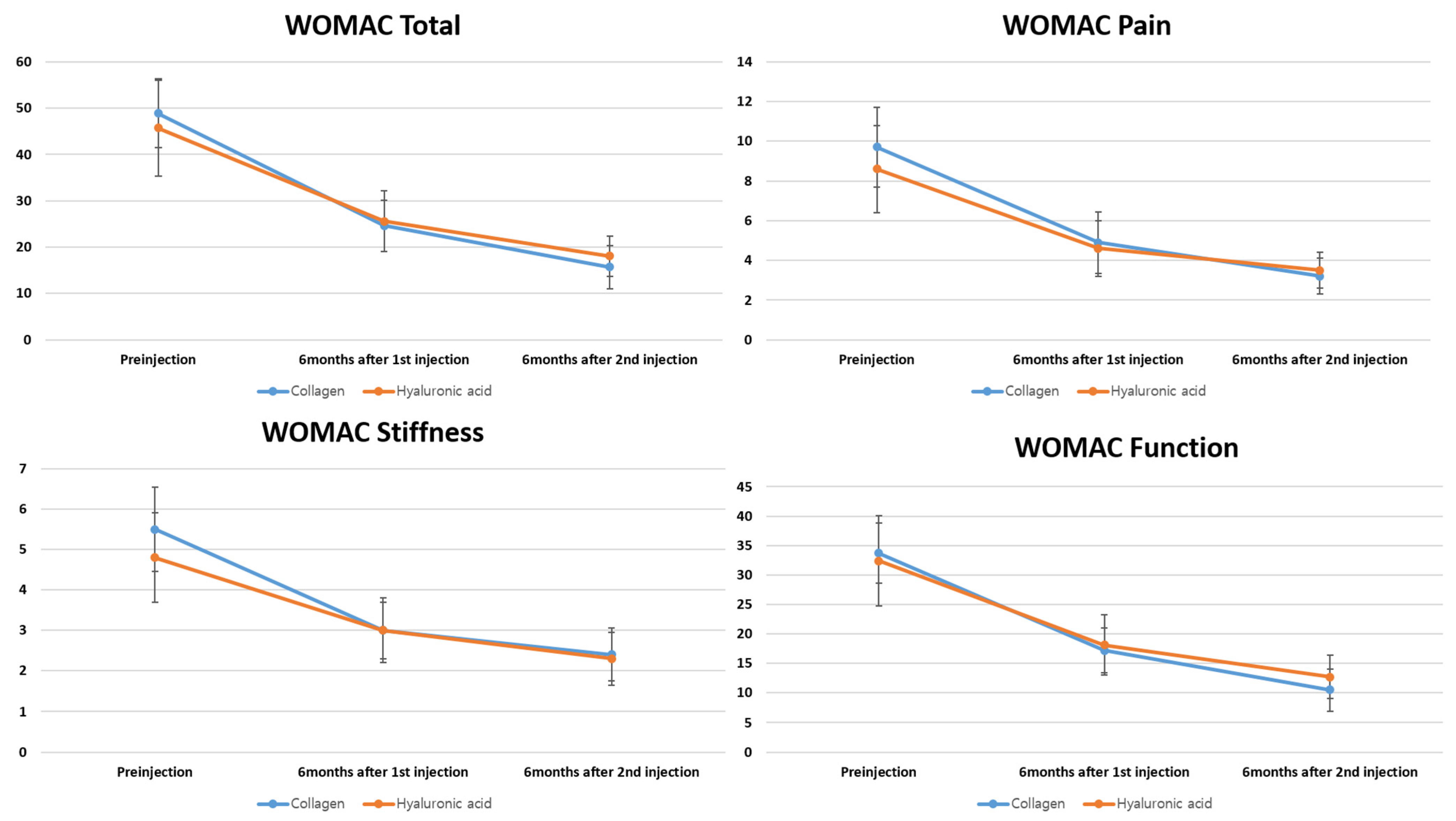
3.2. Primary Outcome: Non-Inferiority of VAS and WOMAC Score Changes
3.3. Secondary Outcome: VAS and WOMAC Scores
3.4. Patient Satisfaction
3.5. Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CI | confidence interval |
| KOA | knee osteoarthritis |
| MCID | minimal clinically important difference |
| NSAIDs | non-steroidal anti-inflammatory drugs |
| OA | osteoarthritis |
| SCB | substantial clinical benefit |
| SD | standard deviation |
| SYSADOAs | symptomatic slow-acting drugs for osteoarthritis |
| VAS | visual analog scale |
| WOMAC | the Western Ontario and McMaster Universities Osteoarthritis Index |
References
- Choi, B.S.; Ro, D.H.; Lee, M.C.; Han, H.S. Isolated Polyethylene Insert Exchange for Instability after Total Knee Arthroplasty: Comparable Survival Rates and Range of Motion and Improved Clinical Scores Regardless of Hyperextension. Clin. Orthop. Surg. 2024, 16, 550–558. [Google Scholar] [CrossRef]
- Hsu, C.E.; Tsai, M.H.; Wu, H.T.; Huang, J.T.; Huang, K.C. Phenotype-considered kinematically aligned total knee arthroplasty for windswept-deformity-associated osteoarthritis: Surgical strategy and clinical outcomes. Knee Surg. Relat. Res. 2024, 36, 16. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Park, Y.B.; Baek, S.H. Clinical and Radiological Outcomes of Computer-Assisted Navigation in Primary Total Knee Arthroplasty for Patients with Extra-articular Deformity: Systematic Review and Meta-Analysis. Clin. Orthop. Surg. 2024, 16, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.I.; Kim, J.K.; Kang, M.W.; Han, H.S. Do the Clinical and Radiological Features of Knees with Mucoid Degeneration of the Anterior Cruciate Ligament Differ According to Knee Osteoarthritis Status? Clin. Orthop. Surg. 2024, 16, 405–412. [Google Scholar] [CrossRef]
- Kim, S.E.; Choi, B.S.; Ro, D.H.; Lee, M.C.; Han, H.S. Fixed-Bearing and Higher Postoperative Knee Flexion Angle as Predictors of Satisfaction in Asian Patients Undergoing Posterior-Stabilized Total Knee Arthroplasty. Clin. Orthop. Surg. 2024, 16, 733–740. [Google Scholar] [CrossRef]
- Glyn-Jones, S.; Palmer, A.J.; Agricola, R.; Price, A.J.; Vincent, T.L.; Weinans, H.; Carr, A.J. Osteoarthritis. Lancet 2015, 386, 376–387. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. [Google Scholar] [CrossRef]
- Loeser, R.F.; Goldring, S.R.; Scanzello, C.R.; Goldring, M.B. Osteoarthritis: A disease of the joint as an organ. Arthritis Rheum. 2012, 64, 1697–1707. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. [Google Scholar] [CrossRef]
- Altman, R.; Hackel, J.; Niazi, F.; Shaw, P.; Nicholls, M. Efficacy and safety of repeated courses of hyaluronic acid injections for knee osteoarthritis: A systematic review. Semin. Arthritis Rheum. 2018, 48, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Czarnocki, Ł.; Dębiński, M.; Sasinowski, T.; Runo, E.; Deszczyński, J. Collagen injections as an alternative therapy for musculoskeletal disorders. Chir. Narzadow Ruchu Ortop. Pol. 2017, 82, 221–224. [Google Scholar]
- Milani, L. A new and refined injectable treatment for musculoskeletal disorders. Bioscaffold properties of collagen and its clinical use. Physiol. Regul. Med. 2010, 1, 3–15. [Google Scholar]
- Tarantino, D.; Mottola, R.; Palermi, S.; Sirico, F.; Corrado, B.; Gnasso, R. Intra-Articular Collagen Injections for Osteoarthritis: A Narrative Review. Int. J. Environ. Res. Public Health 2023, 20, 4390. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Oh, J.M.; Roh, H.; Lee, K.W.; Lee, J.H.; Lee, W.J. Zinc-Alpha-2-Glycoprotein Peptide Downregulates Type I and III Collagen Expression via Suppression of TGF-β and p-Smad 2/3 Pathway in Keloid Fibroblasts and Rat Incisional Model. Tissue Eng. Regen. Med. 2024, 21, 1079–1092. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.S.; Yoo, J.C.; Woo, S.H.; Kwak, A.S. Intra-Articular Atelocollagen Injection for the Treatment of Articular Cartilage Defects in Rabbit Model. Tissue Eng. Regen. Med. 2021, 18, 663–670. [Google Scholar] [CrossRef]
- Wang, Z.; Zheng, Y.; Xu, J.; Jia, Q.; Jiang, H.B.; Lee, E.S. A Simplified GBR Treatment and Evaluation of Posterior Seibert Class I Ridge Defects via Bio-collagen and Platelet-Rich Fibrin: A Retrospective Study. Tissue Eng. Regen. Med. 2024, 21, 959–967. [Google Scholar] [CrossRef]
- Yoo, J.C.; Kim, M.S.; Sohn, S.; Woo, S.H.; Choi, Y.R.; Kwak, A.S.; Lee, D.S. Atelocollagen Scaffold Enhances Cartilage Regeneration in Osteochondral Defects: A Study in Rabbits. Tissue Eng. Regen. Med. 2024, 21, 329–339. [Google Scholar] [CrossRef]
- Borja-Flores, A.; Macías-Hernández, S.I.; Hernández-Molina, G.; Perez-Ortiz, A.; Reyes-Martínez, E.; Belzazar-Castillo de la Torre, J.; Ávila-Jiménez, L.; Vázquez-Bello, M.C.; León-Mazón, M.A.; Furuzawa-Carballeda, J.; et al. Long-Term Effectiveness of Polymerized-Type I Collagen Intra-Articular Injections in Patients with Symptomatic Knee Osteoarthritis: Clinical and Radiographic Evaluation in a Cohort Study. Adv. Orthop. 2020, 2020, 9398274. [Google Scholar] [CrossRef]
- Martin Martin, L.S.; Massafra, U.; Bizzi, E.; Migliore, A. A double blind randomized active-controlled clinical trial on the intra-articular use of Md-Knee versus sodium hyaluronate in patients with knee osteoarthritis (“Joint”). BMC Musculoskelet. Disord. 2016, 17, 94. [Google Scholar] [CrossRef]
- Misir, A.; Yildiz, K.I.; Kizkapan, T.B.; Incesoy, M.A. Kellgren-Lawrence grade of osteoarthritis is associated with change in certain morphological parameters. Knee 2020, 27, 633–641. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63 (Suppl. S11), S240–S252. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Tubach, F.; Ravaud, P.; Baron, G.; Falissard, B.; Logeart, I.; Bellamy, N.; Bombardier, C.; Felson, D.; Hochberg, M.; van der Heijde, D.; et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: The minimal clinically important improvement. Ann. Rheum. Dis. 2005, 64, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Waddell, D.D.; Cefalu, C.A.; Bricker, D.C. A second course of hylan G-F 20 for the treatment of osteoarthritic knee pain: 12-month patient follow-up. J. Knee Surg. 2005, 18, 7–15. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Sung, Y.G.; Park, D.C.; Lee, H.J.; In, Y. The Minimal Clinically Important Difference (MCID) for the WOMAC and Factors Related to Achievement of the MCID After Medial Opening Wedge High Tibial Osteotomy for Knee Osteoarthritis. Am. J. Sports Med. 2021, 49, 2406–2415. [Google Scholar] [CrossRef]
- Phillips, M.; Bhandari, M.; Grant, J.; Bedi, A.; Trojian, T.; Johnson, A.; Schemitsch, E. A Systematic Review of Current Clinical Practice Guidelines on Intra-articular Hyaluronic Acid, Corticosteroid, and Platelet-Rich Plasma Injection for Knee Osteoarthritis: An International Perspective. Orthop. J. Sports Med. 2021, 9, 23259671211030272. [Google Scholar] [CrossRef]
- Tweed, C.D.; Quartagno, M.; Clements, M.N.; Turner, R.M.; Nunn, A.J.; Dunn, D.T.; White, I.R.; Copas, A.J. Exploring different objectives in non-inferiority trials. BMJ 2024, 385, e078000. [Google Scholar] [CrossRef]
- Volpi, P.; Zini, R.; Erschbaumer, F.; Beggio, M.; Busilacchi, A.; Carimati, G. Effectiveness of a novel hydrolyzed collagen formulation in treating patients with symptomatic knee osteoarthritis: A multicentric retrospective clinical study. Int. Orthop. 2021, 45, 375–380. [Google Scholar] [CrossRef]
- De Luca, P.; Colombini, A.; Carimati, G.; Beggio, M.; de Girolamo, L.; Volpi, P. Intra-Articular Injection of Hydrolyzed Collagen to Treat Symptoms of Knee Osteoarthritis. A Functional In Vitro Investigation and a Pilot Retrospective Clinical Study. J. Clin. Med. 2019, 8, 975. [Google Scholar] [CrossRef]
- Lee, H.S.; Oh, K.J.; Moon, Y.W.; In, Y.; Lee, H.J.; Kwon, S.Y. Intra-articular Injection of Type I Atelocollagen to Alleviate Knee Pain: A Double-Blind, Randomized Controlled Trial. Cartilage 2021, 13, 342S–350S. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.D.; Bedi, A.; Karlsson, J.; Sancheti, P.; Schemitsch, E. Product Differences in Intra-articular Hyaluronic Acids for Osteoarthritis of the Knee. Am. J. Sports Med. 2016, 44, 2158–2165. [Google Scholar] [CrossRef] [PubMed]
- Migliore, A.; Procopio, S. Effectiveness and utility of hyaluronic acid in osteoarthritis. Clin. Cases Miner. Bone Metab. 2015, 12, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Furuzawa-Carballeda, J.; Muñoz-Chablé, O.A.; Macías-Hernández, S.I.; Agualimpia-Janning, A. Effect of polymerized-type I collagen in knee osteoarthritis. II. In vivo study. Eur. J. Clin. Investig. 2009, 39, 598–606. [Google Scholar] [CrossRef]
- Ohara, H.; Iida, H.; Ito, K.; Takeuchi, Y.; Nomura, Y. Effects of Pro-Hyp, a collagen hydrolysate-derived peptide, on hyaluronic acid synthesis using in vitro cultured synovium cells and oral ingestion of collagen hydrolysates in a guinea pig model of osteoarthritis. Biosci. Biotechnol. Biochem. 2010, 74, 2096–2099. [Google Scholar] [CrossRef]
- Naraoka, T.; Ishibashi, Y.; Tsuda, E.; Yamamoto, Y.; Kusumi, T.; Toh, S. Periodic knee injections of collagen tripeptide delay cartilage degeneration in rabbit experimental osteoarthritis. Arthritis Res. Ther. 2013, 15, R32. [Google Scholar] [CrossRef]
- Lee, D.W.; Song, D.S.; Han, H.S.; Ro, D.H. Accurate, automated classification of radiographic knee osteoarthritis severity using a novel method of deep learning: Plug-in modules. Knee Surg. Relat. Res. 2024, 36, 24. [Google Scholar] [CrossRef]
- Migliorini, F.; Maffulli, N.; Schäfer, L.; Simeone, F.; Bell, A.; Hofmann, U.K. Minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient-acceptable symptom state (PASS) in patients who have undergone total knee arthroplasty: A systematic review. Knee Surg. Relat. Res. 2024, 36, 3. [Google Scholar] [CrossRef]
- Park, J.; Chaar, O.; Narayanakurup, J.; Abdelhamead, A.S.A.; Ro, D.H.; Kim, S.E. Do knee alignment patterns differ between Middle Eastern and East Asian populations? A propensity-matched analysis using artificial intelligence. Knee Surg. Relat. Res. 2025, 37, 11. [Google Scholar] [CrossRef]
- Yang, H.Y.; Yoon, T.W.; Kim, J.Y.; Seon, J.K. Radiologic Assessment of Knee Phenotypes Based on the Coronal Plane Alignment of the Knee Classification in a Korean Population. Clin. Orthop. Surg. 2024, 16, 422–429. [Google Scholar] [CrossRef]
- Yoon, J.Y.; Moon, S.W. Impacts of asymmetric hip rotation angle on gait biomechanics in patients with knee osteoarthritis. Knee Surg. Relat. Res. 2024, 36, 23. [Google Scholar] [CrossRef] [PubMed]
| Collagen | Hyaluronic Acid | p-Value | |
|---|---|---|---|
| Age, years | 67.3 ± 10.3 | 69.0 ± 9.0 | 0.737 |
| Sex, female/male, n | 15/5 | 16/4 | 1 |
| BMI, kg/m2 | 23.5 ± 3.8 | 24.8 ± 3.2 | 0.257 |
| Occupation (n, %) | 0.305 | ||
| Housewife | 10 (50%) | 14 (70%) | |
| White collar job | 4 (20%) | 1 (5%) | |
| Pink-collar job | 2 (10%) | 0 (0%) | |
| Blue-collar job | 0 (0%) | 3 (15%) | |
| Inoccupation | 4 (20%) | 2 (10%) | |
| Kellgren–Lawrence OA grade | 2.8 ± 1.0 | 2.35 ± 0.99 | 0.151 |
| II (n, %) | 7 (35%) | 10 (50%) | 0.337 |
| III (n, %) | 13 (65%) | 10 (50%) | |
| Previous medication history (n, %) | 0.500 | ||
| NSAIDs | 12 (60%) | 10 (50%) | |
| NSAIDs + SYSADOAs | 6 (30%) | 9 (45%) | |
| NSAIDs + SYSADOAs + Analgesics | 2 (10%) | 1 (5%) | |
| Previous injection history (n, %) | 0.100 | ||
| Yes | 11 (55%) | 6 (30%) | |
| No | 9 (45%) | 14 (70%) | |
| Injection site (Rt, %) | 14 (70%) | 18 (90%) | 0.235 |
| Underlying disease (n, %) | |||
| Hypertension | 11 (55%) | 10 (50%) | 0.751 |
| Diabetes | 4 (20%) | 5 (25%) | 1 |
| Thyroid disease | 4 (20%) | 0 (0%) | 0.106 |
| Smoking (n, %) | 6 (30%) | 6 (30%) | 1 |
| Pre-injection | |||
| VAS resting | 4.8 ± 2.5 | 4.6 ± 3.0 | 0.776 |
| VAS walking | 6.5 ± 2.1 | 6.9 ± 2.0 | 0.538 |
| VAS night | 3.3 ± 3.3 | 2.1 ± 2.5 | 0.299 |
| Total WOMAC | 48.9 ± 14.9 | 45.7 ± 20.6 | 0.583 |
| Pain WOMAC | 9.7 ± 4.0 | 8.6 ± 4.4 | 0.438 |
| Stiffness WOMAC | 5.5 ± 2.1 | 4.8 ± 2.2 | 0.281 |
| Function WOMAC | 33.7 ± 10.3 | 32.4 ± 15.3 | 0.745 |
| Collagen | Hyaluronic Acid | Non-Inferiority Test (Margin: VAS = 1.99) | ||
|---|---|---|---|---|
| p-Value | 95% CI | |||
| Pre-injection–1st injection | ||||
| VAS resting | 2.3 ± 2.0 | 2.4 ± 2.2 | 0.004 | (−1.218, ∞) |
| VAS walking | 3.0 ± 2.5 | 3.2 ± 2.1 | 0.010 | (−1.433, ∞) |
| VAS night | 1.8 ± 2.3 | 1.1 ± 1.4 | <0.0001 | (−0.312, ∞) |
| Pre-injection–2nd injection | ||||
| VAS resting | 3.1 ± 2.1 | 3.3 ± 2.6 | 0.011 | (−1.459, ∞) |
| VAS walking | 4.4 ± 2.4 | 4.7 ± 2.5 | 0.019 | (−1.635, ∞) |
| VAS night | 2.4 ± 2.6 | 1.6 ± 2.0 | 0.0003 | (−0.440, ∞) |
| Collagen | Hyaluronic Acid | Non-Inferiority Test (Margin: WOMAC = MCID) | Non-Inferiority Test (Margin: WOMAC = SCB) | |||
|---|---|---|---|---|---|---|
| p-Value | 95% CI | p-Value | 95% CI | |||
| Pre-injection–1st injection | ||||||
| Total WOMAC | 24.3 ± 11.0 | 20.1 ± 10.4 | <0.0001 | (−1.502, ∞) | <0.0001 | (−1.502, ∞) |
| Pain WOMAC | 4.8 ± 2.6 | 4.0 ± 2.6 | <0.0001 | (−0.634, ∞) | <0.0001 | (−0.634, ∞) |
| Stiffness WOMAC | 2.5 ± 1.7 | 1.8 ± 1.3 | <0.0001 | (−0.043, ∞) | <0.0001 | (−0.043, ∞) |
| Function WOMAC | 16.5 ± 7.8 | 14.2 ± 7.3 | <0.0001 | (−1.724, ∞) | <0.0001 | (−1.724, ∞) |
| Pre-injection–2nd injection | ||||||
| Total WOMAC | 33.2 ± 12.8 | 27.6 ± 14.9 | <0.0001 | (−1.858, ∞) | <0.0001 | (−1.858, ∞) |
| Pain WOMAC | 6.8 ± 3.1 | 5.4 ± 3.4 | <0.0001 | (−0.384, ∞) | <0.0001 | (−0.384, ∞) |
| Stiffness WOMAC | 3.1 ± 1.9 | 2.5 ± 1.9 | <0.0001 | (−0.372, ∞) | <0.0001 | (−0.372, ∞) |
| Function WOMAC | 23.2 ± 8.9 | 19.7 ± 10.5 | <0.0001 | (−1.651, ∞) | <0.0001 | (−1.651, ∞) |
| Collagen | Hyaluronic Acid | p-Value | |
|---|---|---|---|
| Six months after the 1st injection | 0.752 | ||
| No change (n, %) | 0(0%) | 0(0%) | |
| Slightly improved (n, %) | 9(45%) | 10(50%) | |
| Very improved (n, %) | 11(55%) | 10(50%) | |
| Six months after the 2nd injection | 0.889 | ||
| No change (n, %) | 2(10%) | 3(15%) | |
| Slightly improved (n, %) | 15(75%) | 14(70%) | |
| Very improved (n, %) | 3(15%) | 3(15%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
In, Y.; Choi, K.Y.; Kim, M.S. Clinical Efficacy and Safety of Two Cycles of Intra-Articular Injection of Porcine Atelocollagen Versus Hyaluronic Acid in Knee Osteoarthritis. Bioengineering 2025, 12, 710. https://doi.org/10.3390/bioengineering12070710
In Y, Choi KY, Kim MS. Clinical Efficacy and Safety of Two Cycles of Intra-Articular Injection of Porcine Atelocollagen Versus Hyaluronic Acid in Knee Osteoarthritis. Bioengineering. 2025; 12(7):710. https://doi.org/10.3390/bioengineering12070710
Chicago/Turabian StyleIn, Yong, Keun Young Choi, and Man Soo Kim. 2025. "Clinical Efficacy and Safety of Two Cycles of Intra-Articular Injection of Porcine Atelocollagen Versus Hyaluronic Acid in Knee Osteoarthritis" Bioengineering 12, no. 7: 710. https://doi.org/10.3390/bioengineering12070710
APA StyleIn, Y., Choi, K. Y., & Kim, M. S. (2025). Clinical Efficacy and Safety of Two Cycles of Intra-Articular Injection of Porcine Atelocollagen Versus Hyaluronic Acid in Knee Osteoarthritis. Bioengineering, 12(7), 710. https://doi.org/10.3390/bioengineering12070710








