Wearable Devices in Scoliosis Treatment: A Scoping Review of Innovations and Challenges
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Study Selection
3. Results
3.1. Sensor-Integrated Wearable and Orthotic Technologies
- Pressure sensors:
- IMUs:
- Surface Electromyography (sEMG) Sensors:
- Temperature sensors:
- Textile-based or flexible sensors:
- Capacitive and dielectric sensors:
| Citation | Objective | Methodology | Key Findings and Conclusions |
|---|---|---|---|
| 3D-printed braces for individualized treatment | |||
| Redaelli, Alexander Storm (2020) [12] | Feasibility and cost-effectiveness of 3D-printed vs. thermoformed scoliosis braces. | Comparative study (N = 1) | FDM 3D printing with PETG offers a cost-effective, customizable alternative to thermoforming for scoliosis braces, with superior stiffness, comfort, and short-term durability. |
| Storm, Redaelli et al. (2022) [13] | Stability comparison of FDM, conventional, and unbraced conditions using sensors. | Pilot study evaluating the production process Clinical comparison (N = 10) | 3D-printed PETG scoliosis braces proved cost-effective and customizable, offering comparable stability to conventional braces and eliminating the need for plaster casting. |
| Costantini, Redaelli et al. (2025) [14] | To assess whether 3D-printed braces offer advantages or disadvantages over conventional braces. | Clinical pilot study (N = 10) | 3D-printed braces, providing customizable support through additive manufacturing without negatively affecting gait dynamics, showed no significant differences in mobility compared to conventional braces, with both similarly limiting trunk motion and reducing AP acceleration while preserving other gait metrics. |
| Li, Yang et al. (2022) [15] | 3D-printed patient-specific brace with asymmetric stiffness for targeted corrective force. | Design and simulation, clinical application (N = 1) | The brace featured asymmetric stiffness (concave: 145.88 N/mm, convex: 35.96 N/mm) with higher corrective force on the convex side (33.53 N vs. 3.27 N). Cobb angle reduced from 49° to 42.4° after 6 months. |
| Martin, Gugel et al. (2024) [16] | To develop a flexible, printed dielectric sensor grid for real-time pressure monitoring inside scoliosis braces. | Material and sensor development Proof-of-concept testing (N = 0) | A 34 wt.% graphite–silicone mix achieved optimal conductivity (0.32 kΩ) with stable resistance under 50% strain. Square-electrode capacitance grids enhanced sensitivity 10×. Pressure monitoring in scoliosis braces improves but still requires further calibration and testing due to uneven and lateral pressure issues. |
| Smart bracing systems | |||
| Fregna, Raccagni et al. (2024) [1] | Influence of personal and clinical factors on brace adherence in AIS patients. | Cross-sectional study (N = 638) | Brace adherence in AIS was highest among younger, less skeletally mature females, with optimal compliance at 19–22 h/day, supporting the role of psychosocial factors and sensor-based monitoring. |
| Erzurumluoglu, Ozlem et al. (2024) [4] | To examine the pressure applied to the brace by integrating a textile-based pressure sensor array. | Laboratory-based feasibility study | The textile-based capacitive sensor system showed high accuracy, low error, and stable pressure mapping, proving suitable for real-time monitoring in scoliosis braces. |
| Tymins, Zaborowska-Sapeta et al. (2022) [5] | Presents a prototype of the intelligent brace | Prototype development and clinical testing (N = 1) | The smart brace prototype, using graphene-based sensors, enabled real-time tracking of corrective forces (~150 N) and patient compliance, effectively detecting irregular usage and supporting mobile-based monitoring. |
| Guy, Labelle et al. (2021) [6] | To assess the effectiveness of CAD/CAM brace design, with and without simulations. | RCT CAD/CAM: N = 61, CAD-FEM: N = 59 | CAD-FEM and CAD-only braces showed similar clinical outcomes, with finite element method (FEM) improving design efficiency but offering no significant advantage in correction, adherence, or quality of life. |
| Yahyaiee Bavil and Rouhi (2020) [8] | To evaluate night-time Providence brace’s effectiveness in reducing the Cobb angle. | Combined experimental and computational study. (N = 1) | The Providence brace significantly reduced Cobb angle via FE modeling and clinical results, with strong predictive accuracy (4.4% error), highlighting its effectiveness in preventing scoliosis progression. |
| Fuss, Ahmad et al. (2021) [17] | To develop a cost-effective but accurate pressure sensor system for TLSOs. | Development, material testing, and experimental testing (N = 2) | The developed low-cost sensor system demonstrated viability for long-term pressure monitoring in scoliosis braces, showing minor hysteresis from foam liners while maintaining ~12% RMSE accuracy, with peak pressures (up to 0.135 MPa) during deep inspiration, primarily in thoracolumbar regions. |
| Gesbert, Colobert et al. (2021) [18] | Reliability analysis of a textile sensor system for the measurement of brace pressure. | Prospective pilot study, Calibration tests, and clinical validation (N = 4) | The (Smart T-Shirt, STS) prototype showed high accuracy (r2 = 0.99) and reproducibility (r2 > 0.9), effectively detecting posture-based pressure changes, proving reliable for real-time brace pressure monitoring and design optimization. |
| Zou, Zhou et al. (2025) [19] | To evaluate the feasibility of an integrated force-temperature for monitoring AIS brace compliance. | Prospective pilot study (N = 12) | Patients overestimated brace wear time, but a dual-sensor system (force + temperature) achieved 92.3% accuracy in detecting true wear, enabling early detection of non-compliance for timely interventions. |
| Catalina, Robert, and Calin (2020) [10] | To design a smart orthosis that can detect postural changes in the variation of spine curvature. | Design and evaluation research (N = 0) | The study presents a smart orthosis integrating inertial and flex sensors that enhances posture awareness and rehab outcomes via real-time mobile feedback. |
| Gaume, Pietton et al. (2020) [20] | To assess the mean walking distance per day in AIS patients using smartphone-based pedometers. | Prospective observational study. Control group: N = 25, AIS: N = 19 | Braced AIS patients walked significantly more than untreated peers and controls, with no link between Cobb angle and activity, showing AIS does not limit activity; smartphone pedometers offer a low-cost monitoring solution. |
| Lin, Lou et al. (2020) [21] | To compare the effectiveness of the automated pressure-adjustable orthosis (PO) and conventional orthosis (CO) for the treatment of AIS. | RCT PO group: N = 11 CO group: N = 12 | The pressure-optimized orthosis outperformed conventional braces with greater correction, no curve progression at 1-year follow-up, and significantly improved compliance and wear time, enhancing scoliosis management without affecting quality of life. |
| Ray, Nouaille et al. (2023) [22] | Proposes a robotic solution that provides greater mobility and adapts the procedure to the patient. | Validating tests and feasibility (N = 1) | A 2.5 kg modular robotic brace using Stewart-Gough platforms showed precise trajectory tracking and adaptive motion, offering improved comfort and motion accuracy over traditional rigid braces for scoliosis correction. |
| Lim, Mak et al. (2024) [23] | To assess the efficacy of a 3D customized over-corrective brace, “ScoliBrace,” an orthosis treatment for AIS | Prospective pilot study (N = 30) | ScoliBrace wear showed dose-dependent efficacy, reducing Cobb angle by 0.794° per extra hour worn, with optimal adherence at 15–18 h/day, effectively halting progression and avoiding surgery in most cases. |
| Marchese, Du Plessis et al. (2024) [24] | To evaluate short- and medium-term trunk extensor and abdominal endurance in AIS patients using ScoliBrace® and ScoliBalance® treatment. | Retrospective study (N = 33) | The combined Scoli-Brace® and ScoliBalance® treatment significantly enhanced trunk and abdominal endurance in AIS patients over time, with many achieving the 180 s maximum hold duration by follow-up. The approach particularly strengthened trunk extensors without causing muscle weakening. |
| Ali, Fontanari et al. (2022) [25] | Presents finite element analysis (FEA) of an active soft brace | Computational modeling and simulation (N = 0) | The validated FE model showed that the active soft brace reduces Cobb angle and pressure, providing a comfortable, corrective alternative to rigid braces. |
| Cakmak, Cegindir et al. (2022) [26] | A posture-supporting garment for scoliosis, developed using pattern engineering and textile structures. | Develop and test a prototype (N = 1) | Prototype A, a soft exosuit brace, matched rigid orthoses in Cobb angle correction (up to 10.7%) while providing superior comfort, increased wear time, and high satisfaction through optimized design and materials. |
| Farhadiyadkuri and Zhang (2023) [27] | A Multi-Body-FE Simscape model and an analytical model of the AIS bracing treatment are created. | Computational Modeling and Simulation (N = 0) | This study introduced the first MB-FE Simscape model with NPIC control for AIS bracing, achieving <6.5% stiffness error and superior tracking precision (<1% stiffness/damping error, 0.88–3.28% pose error) over traditional methods. |
| Zapata, Virostek et al. (2024) [28] | To measure night-time brace adherence using temperature sensors and its impact on curve progression. | Prospective case series (N = 122) | Night-time use of the Providence brace effectively prevented AIS progression, especially in patients with single or smaller curves and high adherence, with only 6% requiring surgery, lower than rates seen in full-time bracing. |
| Redchen, Vissarionov et al. (2021) [48] | Evaluated yearly outcomes of trunk orthoses post-surgery in children with congenital spinal deformities. | Prospective clinical study (N = 25) | Functional-corrective orthoses provided up to 60% curve correction post-surgery, with thoracic improvements partly sustained and lumbar curves regressing, supporting extended lumbar orthosis use until skeletal maturity. |
| Ali, Fontanari et al. (2022) [49] | Presents an active soft brace that maintains spinal mobility while applying corrective elastic forces. | Modeling and validation experiments (N = 0) | The TSA-powered brace delivered safe, effective corrective forces (0–6 kPa) with accurate control (RMSE: 1.74 mm), preserving mobility and enabling prolonged, low-power scoliosis treatment comparable to rigid braces. |
| West et al. (2022) [50] | To assess the accuracy of the Scolioscreen (smartphone with an application) compared to the Scoliometer. | Diagnostic Accuracy Study (N = 50) | Scolioscreen showed high accuracy and inter-rater reliability (ICC ≥ 0.93) for ATR measurement, offering a low-cost, user-friendly tool for reliable at-home scoliosis screening, even by untrained parents. |
| Zapata, McIntosh et al. (2023) [51] | To evaluate the effects of adding physiotherapeutic scoliosis-specific exercises (PSSE) to night-time bracing. | Prospective comparative study (N = 115) | PSSE combined with night-time bracing outperformed bracing alone in managing thoracolumbar/lumbar curves < 35°, reducing curve progression, improving Cobb angle stability, and lowering full-time bracing need in AIS patients. |
| Smart clothing embedded with sensors | |||
| Caviedes, Jammula et al. (2020) [3] | Wearable sensor system for home therapy providing real-time feedback to improve exercise accuracy. | Design and simulation, clinical application. Sensor array with mobile app integration | The wearable sensor system, using custom garments and harnesses, demonstrated 70–100% sensitivity and perfect specificity in detecting exercises, enabling real-time feedback for posture correction and therapy adherence. |
| Anwary, Cetinkaya et al. (2021) [38] | To develop the Smart-Cover for real-time sitting posture and asymmetry monitoring using pressure sensors. | Laboratory-based feasibility study (N = 10) | Smart-Cover detected sitting asymmetry with ±4% accuracy over a 4.2–8.4 kg pressure range, provided real-time mobile-app feedback, offering a cost-effective solution to promote ergonomics and prevent posture-related disorders. |
| Simegnaw, Teyeme et al. (2022) [40] | To develop a smart shirt with motion sensors for real-time monitoring of trunk posture and bending angles during cycling. | Validating tests and feasibility (N = 1) | The smart shirt accurately measured trunk bending angles (8–35°), with 99% of postures within ergonomic limits. Its CA-74 threads remained reliable after 17 washes, enabling precise, real-time posture monitoring to support cycling performance, injury prevention, and broader ergonomic applications. |
| Yağcı, Turgut, and Yakut (2020) [41] | Scapular taping effects on 3D shoulder and thoracic motion in AIS daily activities. | Prospective intervention study with pre-post testing (N = 24) | Elastic scapular taping improved scapular orientation (external and upward rotation), as well as humeral and trunk kinematics during functional tasks, supporting dynamic stability and upper limb function in adolescents with scoliosis. |
| Lee, Yip et al. (2023) [39] | To develop a smart textile with silicone-embedded fiber Bragg grating (FBG) sensors for real-time bracing pressure monitoring in AIS patients. | A PIMA cotton undergarment with embedded FBG sensors was developed and validated. | Silicone-embedded FBG sensors provided reliable and sensitive force measurements (up to 10 N, R2 > 0.90, ICC = 0.97), improving brace pressure monitoring in AIS through better stability, skin compatibility, and enhanced fit and comfort for improved clinical outcomes. |
| Lee, Wang et al. (2025) [42] | To develop body pressure mapping knitwear (BPMK) with FBG sensors for force monitoring. | Sensor-embedded textile testing, Force measurement + FEA simulation | The FBG-equipped BPMK system provided accurate real-time force monitoring with strong agreement to FEA and X-ray data, enhancing comfort, adaptability, and MRI compatibility, safety, compliance, and scoliosis treatment outcomes. |
| Mosleh, Abtew et al. (2021) [43] | To create adaptive clothing for women with scoliosis that adjusts to spinal deformity progression. | Validating tests and feasibility (N = 1) | The 3D geometrical model enables automated, adaptive garment design for AIS patients using skeleton-based referencing and ease allowances, enhancing fit and comfort while minimizing scanning and manual adjustments. |
| Liu, Zhang et al. (2025) [44] | To investigate soft brace effects on balance, proprioception, and textile design in AIS. | Pilot study, experimental trial, (N = 10), 3D scanning, EOS, motion capture | The PCG soft brace improved postural alignment and proprioception—especially in thoracic/lumbar regions—highlighting its potential for managing mild scoliosis, though personalization and long-term evaluation remain essential. |
| Xuan, Lei et al. (2024) [52] | To develop a smart wearable system for real-time brace monitoring and comfort assessment. | Experimental Sensor-integrated 3D-printed orthosis | The intelligent system offers reliable, real-time monitoring of orthopedic pressure and comfort with <2 s latency and <2% error, enhancing adherence, personalization, and clinical decision-making in scoliosis bracing. |
| Inertial Measurement Unit (IMU)-based wearables | |||
| Dehzangi, Bache et al. (2021) [29] | To develop a smart scoliosis brace system for unsupervised monitoring of wear time, tightness, and activity. | Prospective, single-center, observational study, Boston-type TLSO with wearable sensors | The system enables accurate, remote, context-aware monitoring for scoliosis bracing, achieving >99% activity classification accuracy, improving compliance from 7% to 90%, and detecting a 33% force drop, supporting early identification of poor fit and timely personalized re-fitting. |
| Kim, Hwang et al. (2024) [30] | To develop a wearable system (WLSCMS) for real-time monitoring of spine curvature using IMU sensors combined with ML. | Design and simulation (N = 20), Smart waistband, ML used to classify spinal curvature | The WLSCMS system offers a user-friendly, accurate wearable for lumbar monitoring, achieving >99% classification accuracy without individual calibration and outperforming single-sensor setups, with strong clinical potential pending further validation. |
| Selthafner, Liu et al. (2021) [9] | To evaluate the effectiveness of PSSE on postural balance in AIS patients by measuring the center of pressure (COP) metrics. | Prospective, intervention study, N = 6 (AIS patients), 12-week PSSE program, pre- and post-imaging DIERS 4D | After PSSE, measurable postural improvements were observed through COP and forefoot pressure changes—15% increase in anterior-posterior COP, 25% decrease in medial-lateral COP, and improved symmetry, supporting dynamic pressure analysis as a valuable tool for evaluating AIS therapy outcomes. |
| Fercho, Krakowiak et al. (2022) [31] | To evaluate three spinal braces’ effectiveness in restricting spinal motion using IMUs during daily tasks. | Comparative study (N = 10, healthy adults), IMU-based motion analysis | Spinal orthoses restrict motion task-specifically; TLSO excels in sitting/walking, Hohmann in lifting, with IMUs revealing significant performance differences. |
| Mak, Liang et al. (2023) [32] | To develop and evaluate a neural network using IMUs for 3D spinal curvature estimation. | Design and simulation, clinical application (N = 15, healthy participants) | The IMU-based neural network accurately estimated spinal curvature (0.26 cm error) and Cobb angles, offering a cost-effective, real-time alternative to X-rays for scoliosis monitoring, with potential for clinical, home, and biofeedback use. |
| Farella, Vanzini et al. (2022) [45] | Investigation of motor control alterations in children with idiopathic scoliosis using clinical assessments and IMU-based metrics. | Motor and gait analysis in 34 scoliosis children using ABC-2 and IMUs vs. healthy controls. | Children with idiopathic scoliosis show impaired motor control, slower and more variable gait, and reduced stability; IMU-based non-linear metrics enable early detection and support intervention planning. |
| Gan, Liu et al. (2024) [46] | Evaluating gait symmetry, regularity, and head balance control in AIS patients using wearable accelerometers. | Comparative study (N = 34; 17 scoliosis patients, 17 healthy controls) | AIS patients exhibit reduced head and lumbar vertical motion and lower head regularity, indicating impaired walking balance; wearable accelerometers offer effective, non-invasive tools for real-world gait assessment and monitoring. |
| Hong, Wang et al. (2022) [47] | To develop a flexible, non-invasive sensor tape with integrated accelerometers for real-time spinal curvature assessment. | Design and validation study (N = 15) Flexible sensor tape with 30 MEMS accelerometers | The novel sensor tape demonstrated 99% accuracy and strong correlation with Vicon in spinal angle measurements, offering a reliable, low-cost, and reusable tool for accurate, non-radiative spinal monitoring with strong clinical and ergonomic potential. |
| Wardell, Jayasuriya et al. (2022) [37] | To determine the best sensor placement and temperature threshold for accurately measuring scoliosis brace wear time. | Comparative study Seven Orthotimer and five iButton sensors are embedded in the spinal brace. | Optimal brace wear detection was achieved using abdomen and axilla sensors, with iButton preferred clinically and highest accuracy from uninsulated placement on the anterior abdominal wall using a 26 °C threshold. |
| Żurawski, Śliwiński et al. (2023) [53] | To present a 3D photogrammetric model for monitoring spinal curvature changes in children with postural disorders. | Clinical pilot study (N = 211, spinal deformity patients; 101 controls) | Photogrammetric systems enable sensitive, non-invasive monitoring of pediatric postural rehabilitation, revealing significant improvements in trunk imbalance, pelvic tilt, and spinal curvature, while highlighting the need for individualized, dynamic therapy assessment. |
| Asano, Inami et al. (2024) [54] | To study dynamic spinal and lower limb alignment during gait in adult spinal deformity (ASD) patients compared to static posture using IMUs. | Comparative study (N = 34, ASD patients), IMUs used to track gait-phase spinal and joint changes | IMU data show that in ASD patients, forward trunk tilt during gait results from lumbar flexion and pelvic anteversion, with worsened posture compared to standing, emphasizing the importance of dynamic assessment. |
| Truong, Matsumoto et al. (2024) [55] | To establish guidelines for safely managing pediatric scoliosis with implanted programmable devices (IPD). | Modified Delphi consensus study (N = 25 experts) | Experts reached over 94% consensus on safe use of neuromonitoring and MCGRs in IPD patients, supporting device deactivation during surgery and confirming that, with precautions, standard tools are safe for scoliosis care. |
3.2. EMG-Based Wearables
| Citation | Objective | Methodology | Key Findings and Conclusions |
|---|---|---|---|
| Garg, Gupta et al. (2021) [33] | To compare gait patterns among AIS, congenital scoliosis, and healthy controls to identify differences in gait parameters. | Prospective Cohort Study with EMG and radiographic analysis. 79 AIS Patients | Lumbar and thoracolumbar scoliosis exhibit convex-side EMG asymmetry and coronal imbalance, with asymmetry strongly correlated with the lumbar Cobb angle—most notably at L3—whereas thoracic scoliosis shows no significant muscle activity asymmetry. |
| Zhang, Bao et al. (2024) [34] | To evaluate the clinical effectiveness of sEMG combined with a spine 3D data system. | Original research Participants: 10 AIS patients (6 thoracic, 4 lumbar curves) | sEMG combined with 3D motion data enables accurate, non-invasive assessment of muscle asymmetry and Cobb angle, especially in lumbar scoliosis, with strong correlation to EOS imaging (r = 0.971), supporting dynamic scoliosis monitoring. |
| Wong, Shayestehpour et al. (2024) [35] | To investigate spinal muscle roles in AIS—stabilization vs. progression—using TES, radiography, and EMG. | Cross-sectional study, 45 AIS (subgroups: TES = 5, EMG = 6). | In small-curve AIS, spinal muscles contribute to stability, while in larger curves (>20°), thoracic erector spinae (TES) activation may worsen deformity. Higher summed EMG ratios indicate corrective muscle function, whereas lower ratios are associated with progression risk. |
| Wilczynski and Karolak. (2021) [36] | To explore the relationship between the sEMG frequency of erector spinae and scoliosis curve characteristics in children. | Observational Participants: 244 children, 103 with scoliosis, 141 with scoliotic posture. | sEMG patterns in AIS reveal gender-specific differences and abnormal erector spinae activity, suggesting CNS dysfunction, with potential for standardized sEMG profiles in early detection and prevention |
| Park, Ko et al. (2021) [56] | Study muscle imbalance (EMG), leg length difference, and scoliosis curve types in AIS patients. | Prospective Comparative Study, groups: AIS (n = 20), congenital scoliosis (n = 20), healthy controls (n = 20). | AIS and congenital scoliosis patients exhibit similar gait abnormalities driven by spinal deformity, with convex-side muscle dominance highlighting the need for concave-side strengthening and leg length assessment. |
| Wang, Jiang et al. (2022) [57] | To investigate neuromuscular synergy patterns in the back muscles of AIS patients using high-density EMG. | Prospective comparative study with 10 AIS patients and 10 healthy controls | AIS patients demonstrate asymmetric muscle activation during dynamic tasks, particularly with Cobb angles >20°, including increased convex-side activity and reduced dominant-side control. High-density EMG and synergy analysis effectively reveal these neuromuscular adaptations, supporting their use in guiding targeted therapies. |
| Haksever, Soylu et al. 2024) [58] | To analyze spinae muscle activation during three types of 3D scoliosis-specific elongation exercises. | Prospective cohort study, 24 adolescents with AIS | TheraBand resistance elicits strong paraspinal activation in AIS patients, with LES showing greater side differences, supporting its use in 3D-targeted exercises for bilateral muscle rebalancing. |
| Vongsirinavarat, Kao-ngampanich et al. (2023) [59] | Comparing the paraspinal muscle activity during three self-corrective positions and the habitual standing in AIS. | Cross-sectional observational study 33 adolescents with AIS | Corrective positions enhance EMG ratios compared to habitual standing, with the O1 position most effective for thoracic curves and symmetrical correction optimal for lumbar curves. These self-corrective exercises improve muscle activation across all PUMC curve subtypes. |
| Liang, Yip et al. (2022) [60] | To analyze the relationship between physical features and EMG signals in scoliosis patients using ML. | Cross-sectional study with 106 participants (73 scoliosis patients, 33 controls) | Lumbar EMG asymmetry and paraspinal imbalance in AIS patients support sEMG biofeedback and ML-based early detection, with SVM achieving 85% prediction accuracy using ATR, height, and EMG ratio as key features. |
| Wilczynski and Karolak. (2021) [61] | To analyze the relationship between scoliosis features and sEMG amplitude of the erector spinae in young school children. | Cross-sectional study, N = 251 children, 41%: scoliosis, 56%: scoliotic posture, 3%: normal posture | Thoracic curvatures and sex-related curve direction differences were most common, with elevated erector spinae sEMG amplitudes correlating with curve characteristics, supporting sEMG as a non-invasive tool for early scoliosis detection and monitoring. |
| Banno, Yamoto et al. (2022) [62] | To compare muscle activity in ASD patients and age-matched controls using surface EMG. | Prospective case series study. ASD Group: 14 Control Group: 8 | Improved post-op muscle activity in ASD patients suggests pre-op sEMG abnormalities may reflect CNS dysfunction contributing to scoliosis onset, supporting standardized sEMG profiles for early detection and prevention. |
| Asada, Miura et al. (2023) [63] | Examined time-based changes in spinal alignment and muscle activity during walking in ASD patients. | Retrospective study 26 ASD patients | In ASD patients, walking worsens spinal alignment with increased SpSVA and compensatory cervical PVM and Gmax activity; degeneration limits thoracic/lumbar PVM response, and quadriceps fatigue may reduce walking endurance. |
| Fan, To et al. (2023) [64] | To analyze EMG differences in paravertebral muscles and compare EMG patterns between AIS patients and healthy individuals. | Prospective cohort study with 6-month follow-up. 534 girls (267 AIS, 267 age-matched controls). | AIS patients showed significant EMG asymmetry, with rms-EMG ratios strongly predicting curve progression (AUC: 96% thoracic, 90% lumbar), making asymmetry at AV during back extension a powerful early indicator of scoliosis progression. |
| Fan, Wang et al. (2024) [65] | To develop a pressure and sEMG sensor array into a scoliosis brace to enhance treatment efficiency. | Proof-of-concept study integrating wearable sensors with ML. | The MXene-based sensor array enabled real-time scoliosis monitoring with high durability, accurate sEMG and pressure sensing, and 100% motion classification, supporting brace optimization and curve progression prediction. |
| Ng, Duncombe et al. (2024) [66] | Compared activation in resisted vs. unresisted trunk extension in adolescents with and without scoliosis. | Cross-sectional study Participants: 44 females (AIS = 24, controls = 20). | No group-level difference in peak activation between unresisted and resisted tasks, but high individual variability suggests both are needed to accurately assess paraspinal MVC in adolescents. |
| Wang, Xia et al. (2024) [67] | Analyzed activation to assess neuromuscular characteristics of scapular stabilizers in AIS patients. | Cross-sectional study, observational study. Participants: 17 AIS, 19 controls | AIS patients exhibited impaired scapular neuromuscular control with reduced concave-side AMAs and altered muscle timing, suggesting a need for targeted rehab to enhance stability and motor control. |
| Muraoka, Hasegawa et al. (2025) [68] | To determine whether spinal correction surgery in ASD patients reduces muscle activity and fatigue. | Prospective cohort study, Participants: 16 ASD patients, 16 healthy controls | Preoperative ASD patients had elevated muscle activity that decreased post-surgery, reflecting reduced fatigue and improved alignment, HRQOL, and pain, with I-EMG confirming enhanced postoperative muscle efficiency. |
| Wang, Wang et al. (2025) [69] | Paraspinal muscle activity comparison in AIS vs. healthy individuals for rehab optimization. | Case-control study Participants: 12 AIS patients. 10 healthy controls (age-matched). | AIS patients showed greater muscle asymmetry and reduced sitting activity; targeted Schroth exercises improved paraspinal activation, while erect sitting may worsen S-curve asymmetry. |
3.3. Digital and Remote Therapeutic Platforms
| Citation | Objective | Methodology | Key Findings |
|---|---|---|---|
| Günther, Schober et al. (2023) [70] | Explored motivational barriers and tools to improve home-based scoliosis therapy. | Cross-sectional survey study (Patients: N = 72, Therapists: N = 30) | Most scoliosis patients under-exercised, but motivation—especially in older adults—improved with peer support, assistive devices, and digital tools, highlighting the value of tech-integrated strategies for effective home-based therapy. |
| Culpepper, Murphy et al. (2024) [11] | To assess how telehealth use evolved in early-onset scoliosis (EOS) care during and after the COVID-19 pandemic. | Web-based survey (N = 191, Pediatric Spine Study Group members) | Telehealth use for early-onset scoliosis surged during the pandemic, with bracing and curve monitoring most compatible; common virtual exam methods included back inspection and gait observation, while legal and reimbursement issues continue to limit broader adoption. Telehealth is a lasting, valuable complement to in-person EOS care, especially for follow-ups. |
| Moreira, Teles et al. (2020) [71] | To the use of smart mobile apps with ML for measuring human posture and ROM. | Design and simulation Mobile app prototype using TensorFlow and PoseNet | AI-powered smartphone apps accurately measured posture and ROM by identifying key landmarks, offering a low-cost, accessible tool for musculoskeletal monitoring in clinical and home settings. |
| Martínez-Borba, Suso-Ribera et al. (2021) [72] | To test the feasibility of a mobile app to monitor brace adherence and wellbeing in AIS. | Clinical pilot study (N = 40 adolescents) 90-day trial using a mobile app | Since this is a study protocol, outcome data are not available. The anticipated outcomes include high adherence and usability rates, effective detection of brace-related issues, and increased treatment safety through early interventions based on app-generated alerts. |
| Xia, Hou et al. (2021) [73] | To develop a spinal orthopedic system using BLE and IoT for remote control and monitoring of spinal deformity treatment. | Design and simulation, BLE-enabled growing rod system integrated with mobile app and cloud server | The mobile app-enabled system accurately monitored spinal elongation and adherence with real-time cloud connectivity, offering a personalized, low-power solution to enhance AIS care and reduce clinical workload. |
| Bottino, Settino et al. (2023) [74] | To evaluate digital tools for scoliosis management and propose a framework to assess their features and usability. | Comparative analysis study (N = 7 tools) | Most scoliosis apps measure ATR via motion sensors; only one estimates Cobb angle. Functions vary, and a selection guideline was proposed based on OS, features, and user skill. Digital scoliosis tools enhance monitoring and engagement. The evaluation framework supports clinicians and patients in selecting the right app, encouraging smarter scoliosis care. |
| Akazawa, Torii et al. (2021) [76] | To create an accessible, low-cost mobile app with a standard 2D camera for screening scoliosis. | Design and simulation, clinical application, Trunk asymmetry detection, | A 2D camera-based mobile app reliably detects trunk asymmetry for scoliosis screening using image analysis, offering a scalable solution for resource-limited settings. |
| Yates, Rehman et al. (2021) [77] | Demonstration of wearable-based Human digital twin (HDT) for remote post-op scoliosis recovery monitoring. | Case study (N = 1) | Recovery times varied across physiological metrics (e.g., 3 weeks for sleep, 19 weeks for resting HR). By 5 months post-op, the patient exceeded baseline step count by over 800 steps/day, indicating improved mobility and activity. |
| Yuan, Shi et al. (2025) [78] | To compare digital scoliosis-specific exercise therapy using the Healbone system with traditional in-person care for AIS. | RCT, (N = 128 patients), Digital care (HIRS-supported home therapy) vs. usual care | The digital care group showed significantly greater Cobb angle improvement and pelvic tilt correction, along with higher engagement and daily exercise adherence compared to usual care. Home-based PSSE via the HIRS system offers an effective and accessible alternative for managing AIS. |
| Taslimipour, Rojhani-Shirazi et al. (2021) [75] | Evaluation of a VR dance training program’s effect on thoracic kyphosis angle and respiratory function (FVC, FEV1). | Randomized controlled trial (32 women). Compare traditional therapy vs. therapy + Xbox Kinect-based VR dance training. | Both groups showed improvements in kyphosis angle and FVC. The VRRT group demonstrated greater improvements than the RT group in all outcomes: Kyphosis angle: −13.23° vs. −7.33°, FEV1 increase: +8.06% vs. +1.81%, FVC increase: +7.93% vs. +3.31%. VRRT had larger effect sizes and statistical power. VR enhances engagement, motor control, and proprioception. |
| Kandasamy, Bettany-Saltikov et al. (2021) [79] | Evaluation of a VBAR app’s impact on physiotherapy students’ learning of spinal anatomy and deformities. | A crossover study (N = 74 students) comparing traditional learning to VBAR | VBAR significantly improved students’ understanding of spinal anatomy, increased engagement, and clarified misconceptions compared to traditional methods, with high usability and strong support for collaborative and self-directed learning. |
| Moraes, Cardoso et al. (2022) [80] | To evaluate whether immersive virtual reality (IVR) enhances the effectiveness of postural therapy for scoliosis treatment. | Randomized controlled trial (N = 22 children) Comparison of VR-assisted therapy vs. traditional therapy | The VR training group showed significantly greater improvements in postural stability, tolerance time, and proprioceptive control than the control group, with enhanced engagement contributing to better consistency and endurance. Immersive VR showed promise as a physiotherapy adjunct, though sustained motivation and long-term effects require further study. |
| Misterska, Górski et al. (2023) [81] | To develop a VR system using biometric avatars to assess body image perception in adolescent girls with AIS | Design and simulation, comparative study, Use of “Avatar Scoliosis 3D” VR app with 3D body scans | AIS patients often overestimated their deformity, with avatar-based VR revealing individual body image distortions correlated with Cobb angle, offering objective insight into body perception issues and even post-surgery. The VR-based tool provided a promising method for both clinical assessment and psychological support. |
| Nam, Park et al. (2023) [82] | To evaluate the Smart-Bar Device (SBD) with AR for improving posture accuracy in scoliosis exercises. | Clinical pilot study (N = 10 healthy adults + AIS patients) | The SBD demonstrated high validity (r = 0.836–0.988) and significantly improved posture accuracy in scoliosis patients using AR guidance, with real-time visual and auditory feedback enhancing movement precision. AR-based feedback improves the accuracy of stretching exercises and may benefit home-based rehabilitation for scoliosis patients. |
| Moraes, Palmeira et al. (2024) [83] | To assess the effectiveness of VR-supported postural therapy versus traditional methods using baropodometric analysis. | RCT, (N = 22) Comparison of VR-assisted therapy vs. traditional therapy | While both groups improved posturally, the VR-assisted group showed greater gains in balance and foot pressure metrics, with significant reductions in asymmetries, attributed to enhanced visual feedback and interactive engagement in the VR environment. |
| Wan, Mak et al. (2024) [84] | To evaluate the effectiveness of a motion-sensing video game in improving posture and alignment in adults with adult degenerative scoliosis (ADS). | Clinical pilot study (N = 10 older women with ADS) 6-week training program using a posture-controlled video game | Participants improved sagittal alignment (notably head and C7 position). While spine length slightly decreased, shoulder and pelvis symmetry improved over the 6 weeks. Muscle activity remained imbalanced, indicating habitual movement patterns. Although some effects diminished over time, video games promoted engagement and could support long-term posture correction when used frequently or in conjunction with home-based systems. |
3.4. Integration of AI and Machine Learning for Personalized Rehabilitation
| Citation | Objective | Methodology | Key Findings and Conclusions |
|---|---|---|---|
| Yahara, Tamura et al. (2022) [2] | To develop and evaluate a deep convolutional neural network (DCNN) model for predicting curve progression in AIS patients. | Pilot study (N = 58) | The DCNN model outperformed surgeons in predicting scoliosis progression (69% accuracy, AUC 0.70), with improved performance via transfer learning and focus on spinal regions per Grad-CAM, enabling early, objective, and personalized treatment planning for mild, immature cases. |
| Kaczmarek, Pulik et al. (2023) [7] | Evaluation of lumbar torsional mobility via real-time DSC for physiotherapy planning. | Clinical pilot study, (N = 55 healthy adults) | Mean rotation to the right: 4.78° ± 2.24°; to the left: 2.99° ± 1.44° (p < 0.0001). Max rotation: right 11.35° ± 3.33°, left 7.42° ± 1.97°. No significant sex-based differences. The DSC device offers real-time spinal mobility assessment, supports low back pain therapy planning, and shows reliable performance for future clinical use. |
| Rothstock, Weiss et al. (2020) [85] | To develop a semi-automatic ML method using 3D surface topography for scoliosis severity and treatment group classification. | Design and simulation, clinical application (N = 50 AIS patients), neural network trained | The model achieved 90% accuracy (80% sensitivity, 100% specificity) in classifying scoliosis severity and up to 75% accuracy in simplified ALS group classification, with reduced performance when distinguishing similar curve patterns. |
| Petrosyan, Makaryan et al. (2024) [86] | To propose and validate a targeted safe model using MoCap and ultrasound for continuous IS therapy monitoring. | Clinical pilot study (N = 6 AIS patients) 6-month PSSE and Boston brace rehabilitation program | Reductions in Cobb angle (X-ray: from 36.2° to 23.6°, p < 0.001; MoCap: from 34.6° to 21.4°, p = 0.0014). SRS-22 score improved from 2.6 to 3.9 (p = 0.002). Strong negative correlation between muscle thickness/mass and Cobb angle (SMM: R = –0.96). L3–L4 muscle gains were linked to curve reduction, supporting personalized, segment-targeted PSSE and bracing. |
| Farhadiyadkuri, Popal et al. (2022) [87] | To develop and validate a patient-specific robotic spine exoskeleton with adaptive control to overcome limitations of traditional AIS bracing. | Designed a robotic exoskeleton using 3 Stewart-Gough platforms with 18 actuators, employing inverse dynamics and adaptive impedance control. | MRAIC provided superior position tracking and smoother, safer interaction than conventional control, enabling the exoskeleton to deliver precise corrective forces at T4, T7, and T11 while maintaining performance under uncertainty and sensor noise. The robotic exoskeleton with MRAIC enables safer, adaptive, closed-loop scoliosis treatment. |
| Li, Qian et al. (2024) [88] | To assess an AI app for Cobb angle measurement, validating its accuracy against manual picture archiving and communication system (PACS) methods. | Design and simulation, clinical application (N = 601 scoliosis patients) Mobile app for Cobb angle estimation. | The app demonstrated excellent consistency with PACS (ICC > 0.97), low mean absolute error (~2°), and high accuracy across scoliosis severities, outperforming PACS in repeatability for Cobb angle measurements. The AI app offered a fully automated, portable solution for clinical and remote scoliosis follow-up. |
4. Discussion
4.1. Key Findings
4.2. Limitations of Existing Evidence
4.3. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AIS | Adolescent idiopathic scoliosis |
| ASD | Adult spinal deformity |
| AI | Artificial intelligence |
| ATR | Axial trunk rotation |
| BPMK | Body pressure mapping knitwear |
| CO | Conventional orthosis |
| DSC | Dynamic segmental calibration |
| EMG | Electromyography |
| EOS | Early-onset scoliosis |
| FBG | Fiber Bragg grating |
| FEM | Finite element method |
| FEA | Finite element analysis |
| HDT | Human digital twin |
| IPDs | Implanted programmable devices |
| IVR | Immersive virtual reality |
| IMU | Inertial measurement unit |
| ML | Machine learning |
| MCGRs | Magnetically controlled growing rods |
| MB-FE | Multi-body finite element |
| PETG | Polyethylene terephthalate glycol-modified |
| PSSE | Physiotherapeutic scoliosis-specific exercises |
| PACS | Picture archiving and communication system |
| PCG | Posture correction girdle |
| PO | Pressure-adjustable orthosis |
| RMSE | Root mean square error |
| ROM | Range of motion |
| SVM | Support vector machine |
| TLSO | Thoracolumbosacral orthoses |
| VR | Virtual reality |
References
- Fregna, G.; Raccagni, S.R.; Negrini, A.; Zaina, F.; Negrini, S. Personal and Clinical Determinants of Brace-Wearing Time in Adolescents with Idiopathic Scoliosis. Sensors 2024, 24, 116. [Google Scholar] [CrossRef] [PubMed]
- Yahara, Y.; Tamura, M.; Seki, S.; Kondo, Y.; Makino, H.; Watanabe, K.; Kamei, K.; Futakawa, H.; Kawaguchi, Y. A deep convolutional neural network to predict the curve progression of adolescent idiopathic scoliosis: A pilot study. BMC Musculoskelet. Disord. 2022, 23, 610. [Google Scholar] [CrossRef] [PubMed]
- Caviedes, J.E.; Li, B.; Jammula, V.C. Wearable Sensor Array Design for Spine Posture Monitoring during Exercise Incorporating Biofeedback. IEEE Trans. Biomed. Eng. 2020, 67, 2828–2838. [Google Scholar] [CrossRef]
- Erzurumluoglu, O.F.; Ozlem, K.; Tunc, H.; Gumus, C.; Khalilbayli, F.; Buyukaslan, A.; Yilmaz, H.; Atalay, A.T.; Atalay, O.; İnce, G. Pressure Monitoring for Scoliosis Braces using Textile-based Pressure Sensor Arrays. Proc. Procedia Comput. Sci. 2024, 239, 1409–1416. [Google Scholar] [CrossRef]
- Tymińska, P.; Zaborowska-Sapeta, K.; Janczak, D.; Giżewski, T. TLSO with Graphene Sensors—An Application to Measurements of Corrective Forces in the Prototype of Intelligent Brace. Sensors 2022, 22, 4015. [Google Scholar] [CrossRef]
- Guy, A.; Labelle, H.; Barchi, S.; Audet-Duchesne, E.; Cobetto, N.; Parent, S.; Raison, M.; Aubin, C.-É. Braces Designed Using CAD/CAM Combined or Not With Finite Element Modeling Lead to Effective Treatment and Quality of Life After 2 Years A Randomized Controlled Trial. Spine 2021, 46, 9–16. [Google Scholar] [CrossRef]
- Kaczmarek, W.; Pulik, Ł.; Łęgosz, P.; Mucha, K. Mobility Analysis of the Lumbar Spine with a Dynamic Spine-Correction Device. Sensors 2023, 23, 1940. [Google Scholar] [CrossRef]
- Bavil, A.Y.; Rouhi, G. The biomechanical performance of the night-time Providence brace: Experimental and finite element investigations. Heliyon 2020, 6, e05210. [Google Scholar] [CrossRef]
- Selthafner, M.; Liu, X.; Ellis, F.; Tassone, C.; Thometz, J.; Escott, B. Effect of PSSE on postural sway in AIS using center of pressure. Stud. Health Technol. Inform. 2021, 280, 121–125. [Google Scholar] [CrossRef]
- Luca, C.; Fuior, R.; Corciovă, C.; Munteanu, C. Study on the postural rehabilitation devices used in the prevention of postural defects and the need to use a smart orthosis. Balneo Res. J. 2020, 11, 430–434. [Google Scholar] [CrossRef]
- Culpepper, S.; Murphy, R.F.; Clement, R.C. The evolution of telehealth in early-onset scoliosis care throughout the COVID-19 pandemic. Spine Deform. 2024, 13, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Redaelli, D.F.; Abbate, V.; Storm, F.A.; Ronca, A.; Sorrentino, A.; De Capitani, C.; Biffi, E.; Ambrosio, L.; Colombo, G.; Fraschini, P. 3D printing orthopedic scoliosis braces: A test comparing FDM with thermoforming. Int. J. Adv. Manuf. Technol. 2020, 111, 1707–1720. [Google Scholar] [CrossRef]
- Storm, F.A.; Redaelli, D.F.; Biffi, E.; Reni, G.; Fraschini, P. Additive Manufacturing of Spinal Braces: Evaluation of Production Process and Postural Stability in Patients with Scoliosis. Materials 2022, 15, 6221. [Google Scholar] [CrossRef]
- Costantini, S.; Redaelli, D.F.; Fraschini, P.; Biffi, E.; Storm, F.A. On mobility and gait in scoliosis patients: A comparison of conventional and 3D-printed braces during an instrumented timed-up and go test. BMC Musculoskelet. Disord. 2025, 26, 86. [Google Scholar] [CrossRef]
- Li, H.; Yang, Z.; Li, D.; Qiao, F. A Novel Low-Cost Three-3Dimensional Printed Brace Design Method for Early Onset Scoliosis. J. Med. Devices Trans. ASME 2022, 16, 031013. [Google Scholar] [CrossRef]
- Martin, S.; Gugel, L.; Schedel, S.; Reitelshöfer, S.; Franke, J.; Madden, J.D.; Skov, A.L.; Seelecke, S.S. Printed stretchable dielectric sensor grids for pressure monitoring in orthopedics. Electroact. Polym. Actuators Devices Eapad Xxvi 2024, 12945, 129450S. [Google Scholar]
- Fuss, F.K.; Ahmad, A.; Tan, A.M.; Razman, R.; Weizman, Y. Pressure Sensor System for Customized Scoliosis Braces. Sensors 2021, 21, 1153. [Google Scholar] [CrossRef]
- Gesbert, J.C.; Colobert, B.; Rakotomanana, L.; Violas, P. Idiopathic scoliosis and brace treatment: An innovative device to assess corrective pressure. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 131–136. [Google Scholar] [CrossRef]
- Zou, Y.; Zhou, L.; Wang, J.; Lou, E.; Wong, M.-S. The Application of Integrated Force and Temperature Sensors to Enhance Orthotic Treatment Monitoring in Adolescent Idiopathic Scoliosis: A Pilot Study. Sensors 2025, 25, 686. [Google Scholar] [CrossRef]
- Gaume, M.; Pietton, R.; Vialle, R.; Chaves, C.; Langlais, T. Is daily walking distance affected in adolescent idiopathic scoliosis? An original prospective study using the pedometer on smartphones. Arch. De Pediatr. 2020, 27, 333–337. [Google Scholar] [CrossRef]
- Lin, Y.; Lou, E.; Lam, T.P.; Cheng, J.C.-Y.; Sin, S.W.; Kwok, W.K.; Wong, M.S. The Intelligent Automated Pressure-Adjustable Orthosis for Patients With Adolescent Idiopathic Scoliosis. Spine 2020, 45, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Ray, R.; Nouaille, L.; Colobert, B.; Calistri, L.; Poisson, G. Design and position control of a robotic brace dedicated to the treatment of scoliosis. Robotica 2023, 41, 1466–1482. [Google Scholar] [CrossRef]
- Lim, K.B.L.; Mak, H.K.W.; Rahaman, S.H.A.; Ong, L.L.; Ooi, S.Y.J.; Lee, N.K.L. A pilot study on the “ScoliBrace” in the treatment of adolescent idiopathic scoliosis. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1803–1809. [Google Scholar] [CrossRef]
- Marchese, R.; Du Plessis, J.; Pooke, T.; McAviney, J. The Improvement of Trunk Muscle Endurance in Adolescents with Idiopathic Scoliosis Treated with ScoliBrace® and the ScoliBalance® Exercise Approach. J. Clin. Med. 2024, 13, 653. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Fontanari, V.; Schmölz, W.; Agrawal, S.K. Active Soft Brace for Scoliotic Spine: A Finite Element Study to Evaluate in-Brace Correction. Robotics 2022, 11, 37. [Google Scholar] [CrossRef]
- Cakmak, S.; Cegindir, N.Y.; Yilmaz, H.G. The development of posture supporting soft exosuit design for adolescent idiopathic scoliosis. Int. J. Cloth. Sci. Technol. 2022, 34, 228–240. [Google Scholar] [CrossRef]
- Farhadiyadkuri, F.; Zhang, X. Novel Interaction Control in Adolescent Idiopathic Scoliosis Treatment Using a Robotic Brace. J. Intell. Robot. Syst. Theory Appl. 2023, 109, 73. [Google Scholar] [CrossRef]
- Zapata, K.A.; Virostek, D.; Ma, Y.; Datcu, A.-M.; Gunselman, M.R.; Herring, J.A.; Johnson, M.E. Outcomes for nighttime bracing in adolescent idiopathic scoliosis based on brace wear adherence. Spine Deform. 2024, 12, 643–650. [Google Scholar] [CrossRef]
- Dehzangi, O.; Bache, B.A.; Iftikhar, O.; Wensman, J.; Li, Y. A smart point-of-care compliance monitoring solution for brace treatment of adolescent idiopathic scoliosis patients. Smart Health 2021, 21, 100179. [Google Scholar] [CrossRef]
- Kim, J.; Hwang, J.-Y.; Kang, M.; Cheon, S.; Park, S.H. WLSCMS: Wearable Lumbar Spine Curve Monitoring System Based on Integrated Sensors. IEEE Trans. Instrum. Meas. 2024, 73, 4007510. [Google Scholar] [CrossRef]
- Fercho, J.; Krakowiak, M.; Yuser, R.; Szmuda, T.; Zieliński, P.; Szarek, D.; Pettersson, S.D.; Miękisiak, G. Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units. Int. J. Environ. Res. Public Health 2022, 19, 16515. [Google Scholar] [CrossRef]
- Mak, T.H.A.; Liang, R.; Chim, T.W.; Yip, J. A Neural Network Approach for Inertial Measurement Unit-Based Estimation of Three-Dimensional Spinal Curvature. Sensors 2023, 23, 6122. [Google Scholar] [CrossRef]
- Garg, B.; Gupta, M.; Mehta, N.; Malhotra, R. Influence of Etiology and Onset of Deformity on Spatiotemporal, Kinematic, Kinetic, and Electromyography Gait Variables in Patients with Scoliosis—A Prospective, Comparative Study. Spine 2021, 46, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.-H. Effectiveness study of surface electromyography combined with spine 3D data system to evaluate scoliosis. Am. J. Clin. Exp. Immunol. 2024, 13, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.; Shayestehpour, H.; Koutras, C.; Dahl, B.; Otaduy, M.A.; Rasmussen, J.; Bencke, J. Using Electric Stimulation of the Spinal Muscles and Electromyography during Motor Tasks for Evaluation of the Role in Development and Progression of Adolescent Idiopathic Scoliosis. J. Clin. Med. 2024, 13, 1758. [Google Scholar] [CrossRef] [PubMed]
- Wilczyński, J.; Karolak, P. Relationship Between Electromyographic Frequency of the Erector Spinae and Location, Direction, and Number of Spinal Curvatures in Children with Scoliotic Changes. Risk Manag. Health Policy 2021, 14, 1881–1896. [Google Scholar] [CrossRef]
- Wardell, D.; Jayasuriya, R.; Mills, A.; Totton, N.; Breakwell, L.; Cole, A. A294: Optimisation and validation of thermal adherence sensors for monitoring scoliosis brace wear-time in a clinical trial. Glob. Spine J. 2022, 12, 167S. [Google Scholar] [CrossRef]
- Anwary, A.R.; Cetinkaya, D.; Vassallo, M.; Bouchachia, H. Smart-Cover: A real time sitting posture monitoring system. Sens. Actuators A Phys. 2021, 317, 112451. [Google Scholar] [CrossRef]
- Lee, K.-P.; Yip, J.; Yick, K.-L.; Lu, C.; Lu, L.; Lei, Q.-W.E. A Novel Force-Sensing Smart Textile: Inserting Silicone-Embedded FBG Sensors into a Knitted Undergarment. Sensors 2023, 23, 5145. [Google Scholar] [CrossRef]
- Simegnaw, A.A.; Teyeme, Y.; Malengier, B.; Tesfaye, T.; Daba, H.; Esmelealem, K.; Van Langenhove, L. Smart Shirt for Measuring Trunk Orientation. Sensors 2022, 22, 9090. [Google Scholar] [CrossRef]
- Yagci, G.; Turgut, E.; Yakut, Y. Effect of elastic scapular taping on shoulder and spine kinematics in adolescents with idiopathic scoliosis. Acta Orthop. Et Traumatol. Turc. 2020, 54, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-P.; Wang, Z.; Zheng, L.; Liang, R.; Fok, Q.; Lu, C.; Lu, L.; Cheung, J.P.-Y.; Yick, K.-L.; Yip, J. Enhancing Orthotic Treatment for Scoliosis: Development of Body Pressure Mapping Knitwear with Integrated FBG Sensors. Sensors 2025, 25, 1284. [Google Scholar] [CrossRef]
- Mosleh, S.; Abtew, M.A.; Bruniaux, P.; Tartare, G.; Xu, Y. Developments of adapted clothing for physically disabled people with scoliosis using 3D geometrical model. Appl. Sci. 2021, 11, 10655. [Google Scholar] [CrossRef]
- Liu, P.-Y.; Zhang, J.; Wan, K.-W.F.; Yu, H.-T.H.; Lau, K.-L.K.; Cheung, M.-C.K.; Chen, B.Y.; Yip, J. Evaluating the impact of soft bracing and textile engineering in enhancing postural control and proprioception in adolescent idiopathic scoliosis. J. Ind. Text. 2025, 55, 15280837251313520. [Google Scholar] [CrossRef]
- Farella, G.; Vanzini, F.; Tedeschi, R.; Benedetti, M.; Bisi, M.; Stagni, R. IMU-based assessment of motor control in a population of young subjects with idiopathic scoliosis: Preliminary results from the motor-child study. Gait Posture 2022, 97, 40–41. [Google Scholar] [CrossRef]
- Gan, X.; Liu, X.; Cai, D.; Zhang, R.; Li, F.; Fang, H.; Huang, J.; Qiu, C.; Zhan, H. Wearable accelerometers reveal objective assessment of walking symmetry and regularity in idiopathic scoliosis patients. PeerJ 2024, 12, e17739. [Google Scholar] [CrossRef]
- Hong, T.T.-H.; Wang, Y.; Tan, Q.; Zhang, G.; Wong, D.W.-C.; Zhang, M. Measurement of covered curvature based on a tape of integrated accelerometers. Meas. J. Int. Meas. Confed. 2022, 193, 110959. [Google Scholar] [CrossRef]
- Redchenko, I.A.; Vissarionov, S.V.; Gusev, M.G.; Lein, G.A.; Pavlov, I.V. Stage results of the use of orthoses in children after surgical treatment of congenital spine deformity (Preliminary report). Pediatr. Traumatol. Orthop. Reconstr. Surg. 2021, 9, 41–50. [Google Scholar] [CrossRef]
- Ali, A.; Fontanari, V.; Schmoelz, W.; Fontana, M. Actuator and Contact Force Modeling of an Active Soft Brace for Scoliosis. Bioengineering 2022, 9, 303. [Google Scholar] [CrossRef]
- van West, H.M.; Herfkens, J.; Rutges, J.P.H.J.; Reijman, M. The smartphone as a tool to screen for scoliosis, applicable by everyone. Eur. Spine J. 2021, 31, 990–995. [Google Scholar] [CrossRef]
- Zapata, K.A.; McIntosh, A.L.; Jo, C.-H.; Virostek, D.B. The Addition of Daytime Physiotherapeutic Scoliosis-specific Exercises to Adolescent Idiopathic Scoliosis Nighttime Bracing Reduces Curve Progression. J. Pediatr. Orthop. 2023, 43, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Xuan, L.; Lei, L.; Shao, M.; Han, Q. Design and development of an intelligent wearing system for adolescent spinal orthotics. Med. Biol. Eng. Comput. 2024, 62, 2653–2667. [Google Scholar] [CrossRef]
- Żurawski, A.; Śliwiński, Z.; Nowak-Starz, G.; Kiebzak, W. Monitoring changes in the shape of the spine in children with postural disorders. Med. Stud. 2023, 39, 132–139. [Google Scholar] [CrossRef]
- Asano, F.; Inami, S.; Takeuchi, D.; Moridaira, H.; Ueda, H.; Aoki, H.; Iimura, T.; Taneichi, H. Dynamic Alignment Changes of the Spine, Pelvis, and Lower Limbs during Gait Analyzed Using Inertial Motion Capture in Patients with Adult Spinal Deformity. Spine Surg. Relat. Res. 2024, 8, 631–636. [Google Scholar] [CrossRef]
- Truong, W.H.; Matsumoto, H.; Brooks, J.T.; Guillaume, T.J.; Andras, L.M.; Cahill, P.J.; Fitzgerald, R.E.; Li, Y.; Ramo, B.A.; Soumekh, B.; et al. Development of Consensus-Based Best Practice Guidelines for the Perioperative and Postoperative Care of Pediatric Patients With Spinal Deformity and Programmable Implanted Devices. Spine 2024, 49, 1636–1644. [Google Scholar] [CrossRef]
- Park, Y.; Ko, J.Y.; Jang, J.Y.; Lee, S.; Beom, J.; Ryu, J.S. Asymmetrical activation and asymmetrical weakness as two different mechanisms of adolescent idiopathic scoliosis. Sci. Rep. 2021, 11, 17582. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, N.; Teng, L.; Sui, M.; Li, C.; Wang, L.; Li, G. Synergy Analysis of Back Muscle Activities in Patients With Adolescent Idiopathic Scoliosis Based on High-Density Electromyogram. IEEE Trans. Biomed. Eng. 2022, 69, 2006–2017. [Google Scholar] [CrossRef] [PubMed]
- Haksever, B.; Soylu, C.; Demir, P.; Yildirim, N.U. Unraveling the Muscle Activation Equation: 3D Scoliosis-Specific Exercises and Muscle Response in Adolescent Idiopathic Scoliosis. Appl. Sci. 2024, 14, 6984. [Google Scholar] [CrossRef]
- Vongsirinavarat, M.; Kao-Ngampanich, P.; Sinsurin, K. Electromyography of paraspinal muscles during self-corrective positions in adolescent idiopathic scoliosis. J. Back Musculoskelet. Rehabil. 2023, 37, 165–173. [Google Scholar] [CrossRef]
- Liang, R.; Yip, J.; Fan, Y.; Cheung, J.P.Y.; To, K.-T.M. Electromyographic Analysis of Paraspinal Muscles of Scoliosis Patients Using Machine Learning Approaches. Int. J. Environ. Res. Public Health 2022, 19, 1177. [Google Scholar] [CrossRef]
- Wilczyński, J.; Karolak, P. Correlations between electromyographic amplitude of the erector spinae and the location, direction and number of spinal curvatures in young school children. Med. Stud.-Stud. Med. 2021, 37, 49–57. [Google Scholar] [CrossRef]
- Banno, T.; Yamato, Y.; Nojima, O.; Hasegawa, T.; Yoshida, G.; Arima, H.; Oe, S.; Ushirozako, H.; Yamada, T.; Ide, K.; et al. Comparison of the postoperative changes in trunk and lower extremity muscle activities between patients with adult spinal deformity and age-matched controls using surface electromyography. Spine Deform. 2022, 10, 141–149. [Google Scholar] [CrossRef]
- Asada, T.; Miura, K.; Kadone, H.; Sakashita, K.; Funayama, T.; Takahashi, H.; Noguchi, H.; Sato, K.; Eto, F.; Gamada, H.; et al. The relationship between spinal alignment and activity of paravertebral muscle during gait in patients with adult spinal deformity: A retrospective study. BMC Musculoskelet. Disord. 2023, 24, 2. [Google Scholar] [CrossRef]
- Fan, Y.; To, M.K.-T.; Yeung, E.H.K.; Kuang, G.-M.; Liang, R.; Cheung, J.P.Y. Electromyographic Discrepancy in Paravertebral Muscle Activity Predicts Early Curve Progression of Untreated Adolescent Idiopathic Scoliosis. Asian Spine J. 2023, 17, 922–932. [Google Scholar] [CrossRef]
- Fan, W.; Wang, S.; Li, Q.; Ren, X.; Zhang, C.; Wang, H.; Li, M.; Yang, W.; Deng, W. An All-in-One Array of Pressure Sensors and sEMG Electrodes for Scoliosis Monitoring. Small 2024, 20, e2404136. [Google Scholar] [CrossRef] [PubMed]
- Ng, P.T.; Duncombe, P.; Hoorn, W.v.D.; Claus, A.; Izatt, M.T.; Pivonka, P.; Labrom, R.D.; Tucker, K. Achieving maximal voluntary contraction of paraspinal muscles requires two tasks: Insight from an EMG study of females with and without adolescent idiopathic scoliosis. J. Biomech. 2024, 173, 112251. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xia, N.; Gu, M.; Chen, Z.; Xu, J.; Wang, L.; Liao, Y.; Xie, L.; Huang, X. Neuromuscular disturbances in adolescent idiopathic scoliosis observed from the anticipatory muscle activations in scapula stabilizers: A cross-sectional study. BMC Musculoskelet. Disord. 2024, 25, 1019. [Google Scholar] [CrossRef]
- Muraoka, M.; Hasegawa, K.; Sakai, M.; Hatsushikano, S.; Watanabe, K. Quantitative assessment of muscle activity of back and lower extremities, whole body sagittal alignment, body sway, and health-related quality of life in adult spinal deformity patients before and after spinopelvic correction surgery: From the standpoint of the “cone of economy”. J. Orthop. Sci. 2025, 30, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, S.; Gu, M.; Xu, J.; Huang, X.; Xie, L. Paraspinal muscles activities in S-shaped adolescent idiopathic scoliosis during physiotherapeutic scoliosis specific exercise: A case–control study. BMC Musculoskelet. Disord. 2025, 26, 167. [Google Scholar] [CrossRef]
- Günther, F.; Schober, F.; Hunger, S.; Schellnock, J.; Derlien, S.; Schleifenbaum, S.; Drossel, W.-G.; Heyde, C.-E. Improving Home-Based Scoliosis Therapy: Findings From a Web-Based Survey. JMIR Rehabil. Assist. Technol. 2023, 10, e46217. [Google Scholar] [CrossRef]
- Moreira, R.; Teles, A.; Fialho, R.; dos Santos, T.C.P.; Vasconcelos, S.S.; de Sá, I.C.; Bastos, V.H.; Silva, F.; Teixeira, S. Can human posture and range of motion be measured automatically by smart mobile applications? Med. Hypotheses 2020, 142, 109741. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Borba, V.; Suso-Ribera, C.; Díaz-García, A.; Salat-Batlle, J.; Castilla, D.; Zaragoza, I.; García-Palacios, A.; Sánchez-Raya, J. mHealth for the Monitoring of Brace Compliance and Wellbeing in Adolescents with Idiopathic Scoliosis: Study Protocol for a Feasibility Study. Int. J. Environ. Res. Public Health 2021, 18, 7767. [Google Scholar] [CrossRef]
- Xia, K.; Hou, R.; Yang, J.; Li, X. A Real-Time Spine Orthopedic System Based on Bluetooth Low Energy and Internet of Things. IEEE Access 2021, 9, 153977–153984. [Google Scholar] [CrossRef]
- Bottino, L.; Settino, M.; Promenzio, L.; Cannataro, M. Scoliosis Management through Apps and Software Tools. Int. J. Environ. Res. Public Health 2023, 20, 5520. [Google Scholar] [CrossRef] [PubMed]
- Taslimipour, S.; Rojhani-Shirazi, Z.; Hemmati, L.; Rezaei, I. Effects of a Virtual Reality Dance Training Program on Kyphosis Angle and Respiratory Parameters in Young Women With Postural Hyperkyphosis: A Randomized Controlled Clinical Trial. J. Sport Rehabil. 2021, 30, 293–299. [Google Scholar] [CrossRef]
- Akazawa, T.; Torii, Y.; Ueno, J.; Saito, A.; Niki, H. Mobile Application for Scoliosis Screening Using a Standard 2D Digital Camera. Cureus 2021, 13, e13944. [Google Scholar] [CrossRef]
- Yates, H.; Rehman, M.; Cucchiaro, G.; Varughese, A.; Ahumada, L.; Lonsdale, H. Leveraging the Human Digital Twin for Perioperative Monitoring of Pediatric Patients- An Early Case Study. Anesth. Analg. 2021, 132, 1030–1031. [Google Scholar] [CrossRef]
- Yuan, W.; Shi, W.; Chen, L.; Liu, D.; Lin, Y.; Li, Q.; Lu, J.; Zhang, H.; Feng, Q.; Zhang, H.; et al. Digital Physiotherapeutic Scoliosis-Specific Exercises for Adolescent Idiopathic Scoliosis-A Randomized Clinical Trial. Phys. Med. Rehabil. 2025, 8, e2459929. [Google Scholar]
- Kandasamy, G.; Bettany-Saltikov, J.; Cordry, J.; McSherry, R. Use of vision-based augmented reality to improve student learning of the spine and spinal deformities. Explor. Study S. Afr. J. Physiother. 2021, 77, 10. [Google Scholar] [CrossRef]
- Moraes, Í.A.; Cardoso, A.; Soares, A.B.; de Oliveira, D.A.R.; Júnior, E.L. Combining immersive virtual reality and postural therapy for scoliosis treatment and prevention in children. Res. Biomed. Eng. 2022, 38, 1003–1016. [Google Scholar] [CrossRef]
- Misterska, E.; Górski, F.; Tomaszewski, M.; Buń, P.; Gapsa, J.; Słysz, A.; Głowacki, M. “Scoliosis 3D”—A Virtual-Reality-Based Methodology Aiming to Examine AIS Females’ Body Image. Appl. Sci. 2023, 13, 2374. [Google Scholar] [CrossRef]
- Nam, Y.-G.; Park, S.Y.; Kwon, B.S. Rehabilitation Exercise Using a Smart-Bar Device with Augmented Reality Guide Function. Int. J. Precis. Eng. Manuf. 2023, 24, 1263–1270. [Google Scholar] [CrossRef]
- Moraes, Í.A.; Palmeira, E.G.Q.; Matsushita, R.; De Siqueira, A.G.; De Oliveira, D.A.R.; Cardoso, A.; Júnior, E.A.L. A baropodometric analysis of postural therapy supported by immersive virtual reality. J. Braz. Comput. Soc. 2024, 30, 542–553. [Google Scholar] [CrossRef]
- Wan, F.K.W.; Mak, A.T.H.; Chung, C.W.Y.; Yip, J.Y.W. Development of a Motion-Based Video Game for Postural Training: A Feasibility Study on Older Adults With Adult Degenerative Scoliosis. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 2106–2113. [Google Scholar] [CrossRef] [PubMed]
- Rothstock, S.; Weiss, H.-R.; Krueger, D.; Paul, L. Clinical classification of scoliosis patients using machine learning and markerless 3D surface trunk data. Med. Biol. Eng. Comput. 2020, 58, 2953–2962. [Google Scholar] [CrossRef]
- Petrosyan, T.; Makaryan, N.; Hovhannisyan, H.; Kamrany, R.; Mkrtchyan, H. Monitoring therapy outcomes in idiopathic scoliosis patients: Case series and a proposed model. J. Phys. Educ. Sport 2024, 24, 219–228. [Google Scholar] [CrossRef]
- Farhadiyadkuri, F.; Popal, A.M.; Paiwand, S.S.; Zhang, X. Interaction dynamics modeling and adaptive impedance control of robotic exoskeleton for adolescent idiopathic scoliosis. Comput. Biol. Med. 2022, 145, 105495. [Google Scholar] [CrossRef]
- Li, H.; Qian, C.; Yan, W.; Fu, D.; Zheng, Y.; Zhang, Z.; Meng, J.; Wang, D. Use of Artificial Intelligence in Cobb Angle Measurement for Scoliosis: Retrospective Reliability and Accuracy Study of a Mobile App. J. Med. Internet Res. 2024, 26, e50631. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Hannink, E.; Shannon, T.; Dawes, H.; Barker, K. The validity of the kinect sensor for the measurement of sagittal spine curvature against the gold standard lateral spinal radiograph. Physiotherapy 2020, 107, e28–e29. [Google Scholar] [CrossRef]
- Hannink, E.; Shannon, T.; Dawes, H.; Barker, K. Measurement of sagittal spine curvature: Comparing the Kinect depth camera to the flexicurve and digital inclinometers in a clinical population. Physiotherapy 2020, 107, e21. [Google Scholar] [CrossRef]
- Kokabu, T.; Kanai, S.; Kawakami, N.; Uno, K.; Kotani, T.; Suzuki, T.; Tachi, H.; Abe, Y.; Iwasaki, N.; Sudo, H. An algorithm for using deep learning convolutional neural networks with three dimensional depth sensor imaging in scoliosis detection. Spine J. 2021, 21, 980–987. [Google Scholar] [CrossRef]
- Kurzeja, P.; Ogrodzka-Ciechanowicz, K.; Rozek, K.; Hudakova, Z. Selected aspects of using surface topography and scoliometer in screening for scoliotic postural asymmetry in girls. Arch. Budo Sci. Martial Arts Extrem. Sports 2021, 17, 29–39. [Google Scholar]
- Li, C.; Zhang, B.; Liu, L.; Li, Y.; Xu, Y.; Wang, L.; Yun, C.; Zhao, Y. Design, reliability, and validity of a portable electronic device based on ergonomics for early screening of adolescent scoliosis. J. Orthop. Transl. 2021, 28, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Shchurova, E.N.; Saifutdinov, M.S.; Dolganova, T.I.; Akhmedova, M.A.; Gorbach, A.P. Analysis of the degree of involvement of the lower limb muscles in the pathological process in adolescents with idiopathic scoliosis. Acta Biomed. Sci. 2021, 6, 154–165. [Google Scholar] [CrossRef]
- Tajdari, M.; Maqsood, A.; Li, H.; Saha, S.; Sarwark, J.F.; Liu, W.K. Artificial intelligence data-driven 3D model for AIS. In Research into Spinal Deformities; Proceedings of the Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 2021; pp. 141–145. [Google Scholar]
- Tang, H.Y.; Tan, S.H.; Su, T.Y.; Chiang, C.J.; Chen, H.H. Upper Body Posture Recognition Using Inertial Sensors and Recurrent Neural Networks. Appl. Sci. 2021, 11, 12101. [Google Scholar] [CrossRef]
- Xu, L.H.; Chen, J.S.; Wang, F.; Chen, Y.T.; Yang, W.; Yang, C.J. Machine-learning-based children’s pathological gait classification with low-cost gait-recognition system. Biomed. Eng. Online 2021, 20, 62. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Luo, H.; Yang, C.; Li, J.; Deng, Q.; Liu, P.; Fu, M.; Li, L.; Li, X. Anatomical prior based vertebra modelling for reappearance of human spines. Neurocomputing 2022, 500, 750–760. [Google Scholar] [CrossRef]
- Sabri, N.; Hamed, H.N.A.; Ibrahim, Z.; Ibrahim, K.; Isa, M.A. Integrated Evolving Spiking Neural Network and Feature Extraction Methods for Scoliosis Classification. Comput. Mater. Contin. 2022, 73, 5559–5573. [Google Scholar] [CrossRef]
- Sabri, N.; Hamed, H.N.A.; Ibrahim, Z.; Ibrahim, K.; Isa, M.A.; Diah, N.M. The hybrid feature extraction method for classification of adolescence idiopathic scoliosis using Evolving Spiking Neural Network. J. King Saud Univ. Comput. Inf. Sci. 2022, 34, 8899–8908. [Google Scholar] [CrossRef]
- Sikidar, A.; Vidyasagar, K.E.C.; Gupta, M.; Garg, B.; Kalyanasundaram, D. Classification of mild and severe adolescent idiopathic scoliosis (AIS) from healthy subjects via a supervised learning model based on electromyogram and ground reaction force data during gait. Biocybern. Biomed. Eng. 2022, 42, 870–887. [Google Scholar] [CrossRef]
- Shepel, A.I.; Horoshko, V.I. Effectiveness of the application of kinesiotaping in the recovery treatment of idiopathic scoliosis, degree 1–2. Rehabil. Recreat. 2022, 2022, 81–85. [Google Scholar] [CrossRef]
- Simoneau, M.; Pialasse, J.P.; Mercier, P.; Blouin, J.S. Adolescents with idiopathic scoliosis show decreased intermuscular coherence in lumbar paraspinal muscles: A new pathophysiological perspective. Clin. Neurophysiol. 2022, 138, 38–51. [Google Scholar] [CrossRef]
- Villi, H.; Pinsault, N.; Thomann, G. Spine pathologies detections: Users’ requirements, technological development and first results. Procedia CIRP 2022, 109, 209–214. [Google Scholar] [CrossRef]
- Tileston, K.R.; Naz, K.; Pham, N.; Bryson, X.; Policy, J.; Vorhies, J. P96. Postoperative mobility following posterior spinal fusion for adolescent idiopathic scoliosis. Spine J. 2023, 23, S153–S154. [Google Scholar] [CrossRef]
- Vutan, A.M.; Gruescu, C.M.; Sticlaru, C.; Lovasz, E.C. The Use of Accelerometers to Track Changes in Cobb Angles During Scoliosis Rehabilitation Exercises. New Trends Med. Serv. Robot. 2023, 133, 279–286. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Kokabu, T.; Yamada, K.; Abe, Y.; Tachi, H.; Suzuki, H.; Ohnishi, T.; Endo, T.; Ukeba, D.; Ura, K.; et al. Prediction of Cobb Angle Using Deep Learning Algorithm with Three-Dimensional Depth Sensor Considering the Influence of Garment in Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 499. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, M.; Onu, I.; Trofin, D.; Talaghir, L.G.; Coja, D.M.; Iordan, D.A.; Filip, F.; Silisteanu, S.C.; Vizitiu, E.; Musat, C.L.; et al. Scoliotic postural alignment in prepubertal children: Somatoscopic analysis of anatomical landmarks and development of a working model to limit spinal changes. Balneo Prm Res. J. 2024, 15, 655. [Google Scholar] [CrossRef]
- Goto, G.; Ariga, K.; Tanaka, N.; Oda, K.; Haro, H.; Ohba, T. Clinical Significance of Pose Estimation Methods Compared with Radiographic Parameters in Adolescent Patients with Idiopathic Scoliosis. Spine Surg. Relat. Res. 2024, 8, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Shangyu, G.; Dahui, W. Combining artifícial intelligence fór diagnosing adolescent idiopathic scoliosis. J. Clin. Pediatr. Surg. 2024, 23, 89–92. [Google Scholar] [CrossRef]
- Keil, F.; Schneider, R.; Polomac, N.; Zabar, O.; Finger, T.; Holzgreve, F.; Czabanka, M.; Erbe, C.; Groneberg, D.A.; Hattingen, E.; et al. Improving Therapy for Children with Scoliosis through Reducing Ionizing Radiation by Using Alternative Imaging Methods-A Study Protocol. J. Clin. Med. 2024, 13, 5768. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.G.; Kim, S.; Park, J.H.; Yang, S.; Jang, M.; Yun, Y.J.; Cho, J.S.; You, S.; Jang, S.H. Explainable Deep-Learning-Based Gait Analysis of Hip-Knee Cyclogram for the Prediction of Adolescent Idiopathic Scoliosis Progression. Sensors 2024, 24, 4504. [Google Scholar] [CrossRef]
- Mohamed, N.; Acharya, V.; Schreiber, S.; Parent, E.C.; Westover, L. Effect of adding Schroth physiotherapeutic scoliosis specific exercises to standard care in adolescents with idiopathic scoliosis on posture assessed using surface topography: A secondary analysis of a Randomized Controlled Trial (RCT). PLoS ONE 2024, 19, e0302577. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zhou, Y.; Xu, N.; Zhou, Y.; Zhao, H.; Chang, Z.; Hu, Z.; Han, X.; Song, Y.; Zhou, Z.; et al. Advanced Camera-Based Scoliosis Screening via Deep Learning Detection and Fusion of Trunk, Limb, and Skeleton Features. IEEE J. Biomed. Health Inform. 2024. [Google Scholar] [CrossRef]
- Yang, J.; Li, Y.; Hu, A.; Wang, J.; Meng, M.Q.H. An automated adolescent idiopathic scoliosis assessment and monitoring model based on back surface. Biomed. Signal Process. Control 2025, 102, 107321. [Google Scholar] [CrossRef]
- Mohamed, N.; Ruiz, J.M.G.; Hassan, M.; Costa, O.A.; Burke, T.N.; Mei, Q.; Westover, L. Three-dimensional markerless surface topography approach with convolutional neural networks for adolescent idiopathic scoliosis screening. Sci. Rep. 2025, 15, 8728. [Google Scholar] [CrossRef]
- Rauber, C.; Lüscher, D.; Poux, L.; Schori, M.; Deml, M.C.; Hasler, C.C.; Bassani, T.; Galbusera, F.; Büchler, P.; Schmid, S. Predicted vs. measured paraspinal muscle activity in adolescent idiopathic scoliosis patients: EMG validation of optimization-based musculoskeletal simulations. J. Biomech. 2024, 163, 111922. [Google Scholar] [CrossRef]
- Ahmed, T.; Al Zubayer Swapnil, A.; Islam, M.R.; Wang, I.; Rahman, M. An Exoskeleton Based Robotic Device for Providing Rehabilitative Therapies to Human Forearm and Wrist Joints (UWM-FWRR). Arch. Phys. Med. Rehabil. 2020, 101, e56. [Google Scholar] [CrossRef]
- Barsotti, C.E.; Gavassi, B.M.; Prado, F.E.; Batista, B.N.; de Resende Pratali, R.; Ribeiro, A.P.; de Oliveira, C.E.S.; Ferreira, R.R. Diagnostic accuracy of perioperative electromyography in the positioning of pedicle screws in adolescent idiopathic scoliosis treatment: A cross-sectional diagnostic study. BMC Musculoskelet Disord. 2020, 21, 473. [Google Scholar] [CrossRef]
- Carl, B.; Bopp, M.; Sass, B.; Pojskic, M.; Voellger, B.; Nimsky, C. Spine Surgery Supported by Augmented Reality. Glob. Spine J. 2020, 10, 41S–55S. [Google Scholar] [CrossRef]
- McClendon, J.; Almekkawi, A.K.; Abi-Aad, K.R.; Maiti, T. Use of Pheno Room, Augmented Reality, and 3-Rod Technique for 3-Dimensional Correction of Adolescent Idiopathic Scoliosis. World Neurosurg. 2020, 137, 291. [Google Scholar] [CrossRef]
- Salci, H.; Acar, H.; Taskapilioglu, M.O. Electromyographic Evaluation of Early Stage Results of Exoscopic Microdecompressive Spinal Surgery in Dogs. Acta Sci. Vet. 2020, 48. [Google Scholar] [CrossRef]
- Zhao, J.; Chen, K.; Li, Q.h.; Hang, H.d.; Mao, N.f.; Shen, L.y.; Yang, C.w.; Li, M. Spine morphology measuring instrument based on three-dimensional projection position of the spinous process on body surface: Preliminary application in scoliosis. Acad. J. Second Mil. Med. Univ. 2020, 41, 1198–1202. [Google Scholar] [CrossRef]
- Croci, D.M.; Guzman, R.; Netzer, C.; Mariani, L.; Schaeren, S.; Cattin, P.C.; Jost, G.F. Novel patient-specific 3D-virtual reality visualisation software (SpectoVR) for the planning of spine surgery: A case series of eight patients. BMJ Innov. 2020, 6, 215–219. [Google Scholar] [CrossRef]
- Edstrom, E.; Burstrom, G.; Nachabe, R.; Gerdhem, P.; Terander, A.E. A Novel Augmented-Reality-Based Surgical Navigation System for Spine Surgery in a Hybrid Operating Room: Design, Workflow, and Clinical Applications. Oper. Neurosurg. 2020, 18, 496–502. [Google Scholar] [CrossRef]
- Edström, E.; Burström, G.; Omar, A.; Nachabe, R.; Söderman, M.; Persson, O.; Gerdhem, P.; Elmi-Terander, A. Augmented Reality Surgical Navigation in Spine Surgery to Minimize Staff Radiation Exposure. Spine 2020, 45, E45–E53. [Google Scholar] [CrossRef]
- Edström, E.; Burström, G.; Persson, O.; Charalampidis, A.; Nachabe, R.; Gerdhem, P.; Elmi-Terander, A. Does Augmented Reality Navigation Increase Pedicle Screw Density Compared to Free-Hand Technique in Deformity Surgery? Single Surgeon Case Series of 44 Patients. Spine 2020, 45, E1085–E1090. [Google Scholar] [CrossRef]
- Elmi-Terander, A.; Burström, G.; Nachabé, R.; Fagerlund, M.; Ståhl, F.; Charalampidis, A.; Edström, E.; Gerdhem, P. Augmented reality navigation with intraoperative 3D imaging vs fluoroscopy-assisted free-hand surgery for spine fixation surgery: A matched-control study comparing accuracy. Sci. Rep. 2020, 10, 707. [Google Scholar] [CrossRef]
- Feng, L.; Zhang, X. Protocol selecting and technical dilemmas of intraoperative neurophysiological monitoring during corrective procedures for pediatric scoliosis. J. Clin. Pediatr. Surg. 2020, 2020, 93–97. [Google Scholar] [CrossRef]
- Halsey, M.F.; Myung, K.S.; Ghag, A.; Vitale, M.G.; Newton, P.O.; de Kleuver, M. Neurophysiological monitoring of spinal cord function during spinal deformity surgery: 2020 SRS neuromonitoring information statement. Spine Deform. 2020, 8, 591–596. [Google Scholar] [CrossRef]
- Inoue, M.; Orita, S.; Inage, K.; Suzuki, M.; Fujimoto, K.; Shiga, Y.; Kanamoto, H.; Abe, K.; Kinoshita, H.; Norimoto, M.; et al. Objective evaluation of postoperative changes in real-life activity levels in the postoperative course of lumbar spinal surgery using wearable trackers. BMC Musculoskelet. Disord. 2020, 21, 72. [Google Scholar] [CrossRef]
- Lohre, R.; Wang, J.C.; Lewandrowski, K.U.; Goel, D.P. Virtual reality in spinal endoscopy: A paradigm shift in education to support spine surgeons. J. Spine Surg. 2020, 6, S208–S223. [Google Scholar] [CrossRef] [PubMed]
- Peh, S.; Chatterjea, A.; Pfarr, J.; Schäfer, J.P.; Weuster, M.; Klüter, T.; Seekamp, A.; Lippross, S. Accuracy of augmented reality surgical navigation for minimally invasive pedicle screw insertion in the thoracic and lumbar spine with a new tracking device. Spine J. 2020, 20, 629–637. [Google Scholar] [CrossRef]
- Ali, L.; Jahangiri, F.R.; Ali, A.; Belkhair, S.; Elalamy, O.; Adeli, G.; Alghazow, M.; Krishnan, R.; Karim, F.; Iqrar, A.; et al. Emerging Super-specialty of Neurology: Intraoperative Neurophysiological Monitoring (IONM) and Experience in Various Neurosurgeries at a Tertiary Care Hospital in Doha, Qatar. Cureus J. Med. Sci. 2021, 13, e20432. [Google Scholar] [CrossRef]
- Kovalev, E.V.; Kirilenko, S.I.; Mazurenko, A.N.; Filiustin, A.E.; Dubrovsky, V.V. Smartphone-assisted augmented reality technology for preoperative planning in spine surgery. Hir. Pozvonochnika 2021, 18, 94–99. [Google Scholar] [CrossRef]
- Madrid, C.; Gómez-Rice, A.; Cordón, S.; Sanz-Barbero, E.; Zúñiga, L. Change in triggered EMG thresholds for thoracic pedicle screws caused by pneumothorax during surgery for adolescent idiopathic scoliosis. Report of two cases. Rev. Esp. De Cir. Ortop. Y Traumatol. 2021, 65, 472–476. [Google Scholar] [CrossRef]
- Shao, X.; Huang, Z.; Yang, J.; Deng, Y.; Yang, J.; Sui, W. Efficacy and safety for combination of t-EMG with O-arm assisted pedicle screw placement in neurofibromatosis type I scoliosis surgery. J. Orthop. Surg. Res. 2021, 16, 731. [Google Scholar] [CrossRef] [PubMed]
- Siemionow, K.B.; Forsthoefel, C.W.; Foy, M.P.; Gawel, D.; Luciano, C.J. Autonomous lumbar spine pedicle screw planning using machine learning: A validation study. J. Craniovertebral Junction Spine 2021, 12, 223–227. [Google Scholar] [CrossRef]
- Yahanda, A.T.; Moore, E.; Ray, W.Z.; Pennicooke, B.; Jennings, J.W.; Molina, C.A. First in-human report of the clinical accuracy of thoracolumbar percutaneous pedicle screw placement using augmented reality guidance. Neurosurg. Focus 2021, 51, E10. [Google Scholar] [CrossRef]
- Polyzoidis, S.; McGuire, L.S.; Nikas, D.; Ashkan, K. 3D printing in adult and pediatric neurosurgery: The present and the future. In 3D Printing: Applications in Medicine and Surgery Volume 2; Elsevier: Amsterdam, The Netherlands, 2021; pp. 243–259. [Google Scholar]
- Takahashi, M.; Imagama, S.; Kobayashi, K.; Yamada, K.; Yoshida, G.; Yamamoto, N.; Ando, M.; Kawabata, S.; Kanchiku, T.; Fujiwara, Y.; et al. Validity of the Alarm Point in Intraoperative Neurophysiological Monitoring of the Spinal Cord by the Monitoring Working Group of the Japanese Society for Spine Surgery and Related Research A Prospective Multicenter Cohort Study of 1934 Cases. Spine 2021, 46, E1069–E1076. [Google Scholar] [CrossRef]
- Sayari, A.J.; Chen, O.; Harada, G.K.; Lopez, G.D. Success of Surgical Simulation in Orthopedic Training and Applications in Spine Surgery. Clin. Spine Surg. 2021, 34, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Aoyama, R.; Anazawa, U.; Hotta, H.; Watanabe, I.; Takahashi, Y.; Matsumoto, S.; Ishibashi, T. Augmented Reality Device for Preoperative Marking of Spine Surgery Can Improve the Accuracy of Level Identification. Spine Surg. Relat. Res. 2022, 6, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Mohar, J. Fatal Fulminant Fat Embolism Syndrome in Adult Spine Deformity Surgery: A Case Report. JBJS Case Connect. 2022, 12, e22. [Google Scholar] [CrossRef]
- Butler, A.J.; Rush, A.J.; Lynch, J.J.; Colman, M.; Phillips, F.M. 216. The arrival of augmented reality in MIS: Initial results of use for percutaneous pedicle screw instrumentation. Spine J. 2022, 22, S115. [Google Scholar] [CrossRef]
- McMahon, R.; Morgan, S.J.; Brooks, J.T.; Cahill, P.; Fitzgerald, R.; Li, Y.; Abdullah, A.S.A.; Ahn, E.; Akbarnia, B.; Akoto, H.; et al. Does the presence of programmable implanted devices in patients with early onset scoliosis alter typical operative and postoperative practices? A survey of spine surgeons. Spine Deform. 2022, 10, 951–964. [Google Scholar] [CrossRef] [PubMed]
- Marx, W.; Niemeyer, T.; Conta, A.; Hartmann, C.; Obid, P. Results of a biomechanical pilot study to determine the ROM before and after dorsal correction spondylodesis by means of real-time three-dimensional representation using strain gauges. Eur. Spine J. 2022, 31, 3198–3199. [Google Scholar] [CrossRef]
- Hofler, R.C.; Dinsmore, T.H.; Fessler, R.G. Surgery for Adult Deformity Correction. In Koht, Sloan, Toleikis’s Monitoring the Nervous System for Anesthesiologists and Other Health Care Professionals, 3rd ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2022; pp. 603–616. [Google Scholar]
- Claeson, A.A.; Schwab, F.J.; Gandhi, A.A.; Skaggs, D.L. Power-assisted Pedicle Screw Technique Protects Against Risk of Surgeon Overuse Injury A Comparative Electromyography Study of the Neck and Upper Extremity Muscle Groups in a Simulated Surgical Environment. Spine 2022, 47, E86–E93. [Google Scholar] [CrossRef]
- Courvoisier, A.; Cebrian, A.; Simon, J.; Désauté, P.; Aubert, B.; Amabile, C.; Thiébaut, L. Virtual Scoliosis Surgery Using a 3D-Printed Model Based on Biplanar Radiographs. Bioengineering 2022, 9, 469. [Google Scholar] [CrossRef]
- Gadella, M.; Dulfer, S.; Lange, F.; Scholtens, C.; Absalom, A.; Groen, R.; Faber, C.; Tamasi, K.; Sahinovic, M.; Drost, G. TH-278. Surface versus needle electrodes for recording motor evoked potentials in scoliosis surgery. The NERFACE pilot study. Clin. Neurophysiol. 2022, 141, S176. [Google Scholar] [CrossRef]
- Ishii, K.; Isogai, N.; Funao, H. Navigation-Guided Spinal Fusion: MIS Fusion and Reconstruction in Complex Spine Disease and Deformity. In Technical Advances in Minimally Invasive Spine Surgery: Navigation, Robotics, Endoscopy, Augmented and Virtual Reality; Springer: Berlin/Heidelberg, Germany, 2022; pp. 65–71. [Google Scholar]
- Jahangiri, F.R.; Jahangiri, R.H.; Asad, H.; Farooq, L.; Khattak, W.H. Scoliosis Corrective Surgery with Continuous Intraoperative Neurophysiological Monitoring (IONM). Cureus J. Med. Sci. 2022, 14, e29958. [Google Scholar] [CrossRef]
- Kondylakis, H.; Giglioli, I.A.C.; Katehakis, D.G.; Aldemir, H.; Zikas, P.; Papagiannakis, G.; Hors-Fraile, S.; González-Sanz, P.L.; Apostolakis, K.C.; Stephanidis, C.; et al. A Digital Health Intervention for Stress and Anxiety Relief in Perioperative Care: Protocol for a Feasibility Randomized Controlled Trial. JMIR Res. Protoc. 2022, 11, e38536. [Google Scholar] [CrossRef] [PubMed]
- Zarchi, O.; Ohana, N.; Mercado, E.; Amitai, A.; Berestizshevsky, Y.; Sheinis, D.; Benharroch, D.; Bar-On, E. A practical method for real-time detection of pedicle wall breaching during funneling. Arch. Orthop. Trauma Surg. 2022, 142, 3017–3025. [Google Scholar] [CrossRef]
- Liu, A.; Jin, Y.; Cottrill, E.; Khan, M.; Westbroek, E.; Ehresman, J.; Pennington, Z.; Lo, S.F.L.; Sciubba, D.M.; Molina, C.A.; et al. Clinical accuracy and initial experience with augmented reality-assisted pedicle screw placement: The first 205 screws. J. Neurosurg. Spine 2022, 36, 351–357. [Google Scholar] [CrossRef]
- Mozaffari, K.; Foster, C.H.; Rosner, M.K. Practical Use of Augmented Reality Modeling to Guide Revision Spine Surgery: An Illustrative Case of Hardware Failure and Overriding Spondyloptosis. Oper. Neurosurg. 2022, 23, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Sommer, F.; Waterkeyn, F.; Hussain, I.; Goldberg, J.L.; Kirnaz, S.; Navarro-Ramirez, R.; Ahmad, A.A.; Balsano, M.; Medary, B.; Shabani, H.; et al. Feasibility of smart glasses in supporting spinal surgical procedures in low- and middle-income countries: Experiences from East Africa. Neurosurg. Focus 2022, 52, E4. [Google Scholar] [CrossRef]
- Sumdani, H.; Aguilar-Salinas, P.; Avila, M.J.; Barber, S.R.; Dumont, T. Utility of Augmented Reality and Virtual Reality in Spine Surgery: A Systematic Review of the Literature. World Neurosurg. 2022, 161, e8–e17. [Google Scholar] [CrossRef] [PubMed]
- Atai, N.A.; Mehta, V.; Kobbe, P.; Weidle, P. 173. Can augmented reality data visualization support more effective intraoperative rod optimization? An in-vitro biomechanical study. Spine J. 2023, 23, S89. [Google Scholar] [CrossRef]
- Butler, A.J.; Colman, M.W.; Lynch, J.; Phillips, F.M. Augmented reality in minimally invasive spine surgery: Early efficiency and complications of percutaneous pedicle screw instrumentation. Spine J. 2023, 23, 27–33. [Google Scholar] [CrossRef]
- Ma, X.; Ren, J.; Zhou, X.; Wu, Z.; Wang, D.; Kong, L. Personalized Modeling and Analysis of Mild Adolescent Idiopathic Scoliosis Based on OpenSim. Yiyong Shengwu Lixue/J. Med. Biomech. 2023, 38, 1146–1153. [Google Scholar] [CrossRef]
- Shetty, A.P.; Raja, D.C. Current trends and advancements in spine surgery. J. Orthop. 2023, 44, 31–32. [Google Scholar] [CrossRef]
- Cardozo, M.R.; Singh, S.; Barot, K.; Carey-Ewend, A.; Brehm, S.; Verastegui, G.T.; De La Paz, M.; Hanafy, A.; Olufawo, M.; Yahanda, A.; et al. A360: Augmented reality-assisted percutaneous pedicle screw insertion in the cervical vertebrae: A cadaveric proof-of concept study. Glob. Spine J. 2023, 13, 214S. [Google Scholar] [CrossRef]
- Sun, W.; Wei, Y.; Zheng, X.; Guo, J.; Yu, L. The application value of 3D finite element analysis technology and 3D printing biological model technology in the precise surgery of degenerative lumbar scoliosis. J. Chin. Physician 2023, 25, 1692–1696. [Google Scholar] [CrossRef]
- Tillman, L.C.; Truong, W.H.; Morgan, S.J.; Guillaume, T.J. An in vivo analysis of implanted programmable device interference during magnetically controlled growing rod lengthenings: A story of 129 lengthenings. Spine Deform. 2023, 11, 1283–1289. [Google Scholar] [CrossRef]
- Daroszewski, P.; Huber, J.; Kaczmarek, K.; Janusz, P.; Glówka, P.; Tomaszewski, M.; Domagalska, M.; Kotwicki, T. Comparison of Motor Evoked Potentials Neuromonitoring Following Pre- and Postoperative Transcranial Magnetic Stimulation and Intraoperative Electrical Stimulation in Patients Undergoing Surgical Correction of Idiopathic Scoliosis. J. Clin. Med. 2023, 12, 6312. [Google Scholar] [CrossRef]
- Garg, D.; Dubey, N.; Goel, P.; Ramoliya, D.; Ganatra, A.; Kotecha, K. Improvisation in Spinal Surgery Using AR (Augmented Reality), MR (Mixed Reality), and VR (Virtual Reality). Eng. Proc. 2023, 59, 186. [Google Scholar] [CrossRef]
- Pahwa, B.; Azad, T.D.; Liu, J.; Ran, K.; Liu, C.J.; Tracz, J.; Sattari, S.A.; Khalifeh, J.M.; Judy, B.F.; Bydon, A.; et al. Assessing the Accuracy of Spinal Instrumentation Using Augmented Reality (AR): A Systematic Review of the Literature and Meta-Analysis. J. Clin. Med. 2023, 12, 6741. [Google Scholar] [CrossRef] [PubMed]
- Yahara, Y.; Seki, S.; Makino, H.; Futakawa, H.; Kamei, K.; Kawaguchi, Y. Asymmetric Load Transmission Induces Facet Joint Subchondral Sclerosis and Hypertrophy in Patients with Idiopathic Adolescent Scoliosis: Evaluation Using Finite Element Model and Surgical Specimen. JBMR Plus 2023, 7, e10812. [Google Scholar] [CrossRef]
- Sakai, D.; Schol, J.; Kawachi, A.; Sako, K.; Hiyama, A.; Katoh, H.; Sato, M.; Watanabe, M. Adolescent Idiopathic Scoliotic Deformity Correction Surgery Assisted by Smart Glasses Can Enhance Correction Outcomes and Accuracy and Also Improve Surgeon Fatigue. World Neurosurg. 2023, 178, E96–E103. [Google Scholar] [CrossRef]
- Bcharah, G.; Gupta, N.; Panico, N.; Winspear, S.; Bagley, A.; Turnow, M.; D’Amico, R.; Ukachukwu, A.E.K. Innovations in Spine Surgery: A Narrative Review of Current Integrative Technologies. World Neurosurg. 2024, 184, 127–136. [Google Scholar] [CrossRef]
- Bhimreddy, M.; Jiang, K.; Weber-Levine, C.; Theodore, N. Computational Modeling, Augmented Reality, and Artificial Intelligence in Spine Surgery. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2024; Volume 1462, pp. 453–464. [Google Scholar]
- Daroszewski, P.; Huber, J.; Kaczmarek, K.; Janusz, P.; Główka, P.; Tomaszewski, M.; Kotwicki, T. “Real-Time Neuromonitoring” Increases the Safety and Non-Invasiveness and Shortens the Duration of Idiopathic Scoliosis Surgery. J. Clin. Med. 2024, 13, 1497. [Google Scholar] [CrossRef]
- De Jesus Encarnacion Ramirez, M.; Chmutin, G.; Nurmukhametov, R.; Soto, G.R.; Kannan, S.; Piavchenko, G.; Nikolenko, V.; Efe, I.E.; Romero, A.R.; Mukengeshay, J.N.; et al. Integrating Augmented Reality in Spine Surgery: Redefining Precision with New Technologies. Brain Sci. 2024, 14, 645. [Google Scholar] [CrossRef] [PubMed]
- Dietz, N.; Alkin, V.; Lieberman, I.; Manista, A.; Kim, T.; Johnson, J.P.; Drazin, D. Scoping review of robotics technology in spinal surgery with highlights of the Annual Seattle Science Foundation Course. Ann. Transl. Med. 2024, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Hiranaka, Y.; Takeoka, Y.; Yurube, T.; Tsujimoto, T.; Kanda, Y.; Miyazaki, K.; Ohnishi, H.; Matsuo, T.; Ryu, M.; Kumagai, N.; et al. The Utility and Feasibility of Smart Glasses in Spine Surgery: Minimizing Radiation Exposure During Percutaneous Pedicle Screw Insertion. Neurospine 2024, 21, 432–439. [Google Scholar] [CrossRef]
- Kanno, H.; Handa, K.; Murotani, M.; Ozawa, H. A Novel Intraoperative CT Navigation System for Spinal Fusion Surgery in Lumbar Degenerative Disease: Accuracy and Safety of Pedicle Screw Placement. J. Clin. Med. 2024, 13, 2105. [Google Scholar] [CrossRef]
- Nguyen, A.; Dinglasan, M.; Holland, C.; Chung, J.M. The accuracy of pulse-train stimulation for implantation of pedicle screws in adolescent scoliosis. J. Clin. Neurophysiol. 2024, 41, e22. [Google Scholar]
- Ohashi, M.; Sato, M.; Tashi, H.; Minato, K.; Makino, T.; Kawashima, H. Mixed Reality-Based Navigation for Pedicle Screw Placement: A Preliminary Study Using a 3D-Printed Spine Model. Cureus J. Med. Sci. 2024, 16, e59240. [Google Scholar] [CrossRef]
- Saghbiny, E.; Leblanc, L.; Harle, A.; Bobbio, C.; Vialle, R.; Morel, G.; Tamadazte, B. Breach Detection in Spine Surgery Based on Cutting Torque. IEEE Trans. Med. Robot. Bionics 2024, 6, 1084–1092. [Google Scholar] [CrossRef]
- Turlip, R.W.; Khela, H.S.; Dagli, M.M.; Chauhan, D.; Ghenbot, Y.; Ahmad, H.S.; Yoon, J.W. Redefining precision: The current and future roles of artificial intelligence in spine surgery. Artif. Intell. Surg. 2024, 4, 324–330. [Google Scholar] [CrossRef]
- Winkler, D.; Kropla, F.; Busse, M.; Jung, S.; Scholz, S.; Güresir, E.; Gericke, M.; Vychopen, M.; Wach, J.; Grunert, R. Mixed reality for spine surgery: A step into the future with a human cadaveric accuracy study. Neurosurg. Focus 2024, 56, E10. [Google Scholar] [CrossRef]
- Leblanc, L.; Saghbini, E.; Da Silva, J.; Harlé, A.; Vafadar, S.; Chandanson, T.; Vialle, R.; Morel, G.; Tamadazte, B. Automatic Spinal Canal Breach Detection During Pedicle Screw Placement. IEEE Robot. Autom. Lett. 2024, 9, 1915–1922. [Google Scholar] [CrossRef]
- Tanaka, M.; Schol, J.; Sakai, D.; Sako, K.; Yamamoto, K.; Yanagi, K.; Hiyama, A.; Katoh, H.; Sato, M.; Watanabe, M. Low Radiation Protocol for Intraoperative Robotic C-Arm Can Enhance Adolescent Idiopathic Scoliosis Deformity Correction Accuracy and Safety. Glob. Spine J. 2024, 14, 1504–1514. [Google Scholar] [CrossRef]
- Lewis, S.J.; Kelly, M.P.; Charalampidis, A.; Swamy, G.; Lenke, L.G. Is a 50% loss in IONM signal the appropriate cut-off in spinal deformity surgery? Spine J. 2024, 24, S85. [Google Scholar] [CrossRef]
- Misterska, E.; Tomaszewski, M.; Górski, F.; Gapsa, J.; Slysz, A.; Glowacki, M. Assessing the Efficacy of Cognitive-Behavioral Therapy on Body Image in Adolescent Scoliosis Patients Using Virtual Reality. J. Clin. Med. 2024, 13, 6422. [Google Scholar] [CrossRef] [PubMed]
- Youssef, S.; McDonnell, J.M.; Wilson, K.V.; Turley, L.; Cunniffe, G.; Morris, S.; Darwish, S.; Butler, J.S. Accuracy of augmented reality-assisted pedicle screw placement: A systematic review. Eur. Spine J. 2024, 33, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Azad, T.D.; Horowitz, M.A.; Tracz, J.A.; Khalifeh, J.M.; Liu, C.J.; Hughes, L.P.; Judy, B.F.; Khan, M.; Bydon, A.; Witham, T.F. Augmented Reality Versus Freehand Spinopelvic Fixation in Spinal Deformity: A Case-Control Study. Surg. Innov. 2025, 32, 36–45. [Google Scholar] [CrossRef]
- Dada, A.; Saggi, S.; Ambati, V.S.; Patel, A.; Mummaneni, P.V. Evolution of the Minimally Invasive Surgery Transforaminal Lumbar Interbody Fusion: Where Are We Now? Neurosurgery 2025, 96, S33–S41. [Google Scholar] [CrossRef]
- Ikwuegbuenyi, C.A.; Inzerillo, S.; Wang, E.; Hussain, I. Strategies for Optimizing Clinical Outcomes in Minimally Invasive Spine Surgery. Neurosurgery 2025, 96, S139–S147. [Google Scholar] [CrossRef]
- Kim, J.Y.; Hwang, J.Y.; Park, E.; Nam, H.U.; Cheon, S. Flat-Feet Prediction Based on a Designed Wearable Sensing Shoe and a PCA-Based Deep Neural Network Model. IEEE Access 2020, 8, 199070–199080. [Google Scholar] [CrossRef]
- Slater, H.; Stinson, J.N.; Jordan, J.E.; Chua, J.; Low, B.; Lalloo, C.; Pham, Q.; Cafazzo, J.A.; Briggs, M. Evaluation of Digital Technologies Tailored to Support Young People’s Self-Management of Musculoskeletal Pain: Mixed Methods Study. J. Med. Internet Res. 2020, 22, e18315. [Google Scholar] [CrossRef]
- Zaltieri, M.; Massaroni, C.; Lo Presti, D.; Bravi, M.; Sabbadini, R.; Miccinilli, S.; Sterzi, S.; Formica, D.; Schena, E. A Wearable Device Based on a Fiber Bragg Grating Sensor for Low Back Movements Monitoring. Sensors 2020, 20, 3825. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A. Significant advancements of 4D printing in the field of orthopaedics. J. Clin. Orthop. Trauma 2020, 11, S485–S490. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.Y.; Yang, C.M.; Kim, J.J. Effectiveness of Combined Stretching and Strengthening Exercise Using Rehabilitation Exercise System with a Linear Actuator and MR Damper on Static and Dynamic Sitting Postural Balance: A Feasibility Study. Appl. Sci. 2021, 11, 7329. [Google Scholar] [CrossRef]
- Yan, R.G.; Xu, Y.L.; Zhang, H.W.; Jiang, R.A. A ToF-based system for recording human sagittal back shape. Technol. Health Care 2021, 29, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Willwacher, S.; Koopmann, T.; Dill, S.; Kurz, M.; Bruggemann, G.P. Dorsal muscle fatigue increases thoracic spine curvature in all-out recreational ergometer rowing. Eur. J. Sport Sci. 2021, 21, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Zheng, Y.; Zhang, K. Textile-Based Capacitive Pressure Distribution Measurement System for Human Sitting Posture Monitoring. J. Donghua Univ. 2021, 38, 492–497. [Google Scholar] [CrossRef]
- Asadullah, G.M.; Sabyrov, N.; Kamal, M.A.S.; Ali, M.H. Design of a fluid-driven 3D printed spinal posture corrector. Mater. Today-Proc. 2021, 44, 1555–1559. [Google Scholar] [CrossRef]
- Odeh, K.; Wu, W.; Taylor, B.; Leasure, J.; Kondrashov, D. In-vitro 3D Analysis of Sacroiliac Joint Kinematics: Primary and Coupled Motions. Spine 2021, 46, E467–E473. [Google Scholar] [CrossRef]
- Adibatti, S.; Sudhindra, K.R.; Joshi Manisha, S. Survey of Advances in Cobb Angle Measurement for Automatic Spine Detection in X-Ray. WSEAS Trans. Syst. Control 2022, 17, 446–457. [Google Scholar] [CrossRef]
- Willemsen, K.; Magré, J.; Mol, J.; Noordmans, H.J.; Weinans, H.; Hekman, E.E.G.; Kruyt, M.C. Vital Role of In-House 3D Lab to Create Unprecedented Solutions for Challenges in Spinal Surgery, Practical Guidelines and Clinical Case Series. J. Pers. Med. 2022, 12, 395. [Google Scholar] [CrossRef]
- Wu, Y.; Lu, Y.; Ma, C.; Zhang, X.; Pan, Z.; Yu, X.; Zhang, Y. Spinal Posture Recognition Device Using Cloud Storage and BP Neural Network Approach Based on Surface Electromyographic Signal. In Communications in Computer and Information Science; Springer: Berlin/Heidelberg, Germany, 2022; pp. 507–517. [Google Scholar]
- Asadullah, G.M.; Ali, H.; Hashikura, K.; Kamal, M.A.S.; Yamada, K. Development of an Automatic Air-Driven 3D-Printed Spinal Posture Corrector. Actuators 2022, 11, 184. [Google Scholar] [CrossRef]
- Aydın, R.; Alnajjar, F.; Sonoo, M.; Costa Garcia, A.; Takatsune, K.; Shimoda, S. The Influence of Harmonics Filtering for Weak EMG Analysis. In Biosystems and Biorobotics; Springer: Berlin/Heidelberg, Germany, 2022; Volume 28, pp. 791–795. [Google Scholar]
- Fan, Z.; Hu, X.; Chen, W.M.; Zhang, D.W.; Ma, X. A deep learning based 2-dimensional hip pressure signals analysis method for sitting posture recognition. Biomed. Signal Process. Control 2022, 73, 103432. [Google Scholar] [CrossRef]
- Hannink, E.; Dawes, H.; Shannon, T.M.L.; Barker, K.L. Validity of sagittal thoracolumbar curvature measurement using a non-radiographic surface topography method. Spine Deform. 2022, 10, 1299–1306. [Google Scholar] [CrossRef]
- Lee, D.; Kim, S.; Park, H.J.; Kim, S.; Shin, D. A Spine Assistive Robot With a Routed Twisted String Actuator and a Flat-Back Alleviation Mechanism for Lumbar-Degenerative Flat Back. IEEE-Asme Trans. Mechatron. 2022, 27, 5185–5196. [Google Scholar] [CrossRef]
- Ekambaram, D.; Ponnusamy, V. AI-assisted Physical Therapy for Post-injury Rehabilitation: Current State of the Art. IEIE Trans. Smart Process. Comput. 2023, 12, 234–242. [Google Scholar] [CrossRef]
- Kurland, D.B.; Lau, D.; Kim, N.C.; Ames, C. A bibliometric analysis of patient-reported outcome measures in adult spinal deformity, and the future of patient-centric outcome assessments in the era of predictive analytics. Semin. Spine Surg. 2023, 35, 101032. [Google Scholar] [CrossRef]
- Yan, J.; Wang, A. iGuard: An Intelligent Sitting Posture Monitoring System with Pressure Sensors. In Proceedings of the 3rd International Conference on Computer Vision and Pattern Analysis (ICCPA 2023), Hangzhou, China, 7–9 April 2023. [Google Scholar]
- Casey, H.L.; Shah, V.V.; Muzyka, D.; McNames, J.; El-Gohary, M.; Sowalsky, K.; Safarpour, D.; Carlson-Kuhta, P.; Schmahmann, J.D.; Rosenthal, L.S.; et al. Standing Balance Conditions and Digital Sway Measures for Clinical Trials of Friedreich’s Ataxia. Mov. Disord. 2024, 39, 996–1005. [Google Scholar] [CrossRef]
- Ding, Q.P.; Jiang, J.Y.; Lee, K.M. Reconstruction of a Human Spine Curve in the Sagittal Plane From the Measured Contour of the Human Back. IEEE Trans. Instrum. Meas. 2024, 73, 5014910. [Google Scholar] [CrossRef]
- Ding, Q.P.; Lee, K.M.; Jiang, J.Y.; Guo, J.J. Subject-Specific Parametric Identification of a Spine-Equivalent Beam Model for Lumbar Force Prediction in Sagittal Plane. IEEE Trans. Instrum. Meas. 2024, 73, 7507415. [Google Scholar] [CrossRef]
- García-Luna, M.A.; Jimenez-Olmedo, J.M.; Pueo, B.; Manchado, C.; Cortell-Tormo, J.M. Concurrent Validity of the Ergotex Device for Measuring Low Back Posture. Bioengineering 2024, 11, 98. [Google Scholar] [CrossRef]
- Gupta, M.C.; Lenke, L.G.; Gupta, S.; Farooqi, A.S.; Boachie-Adjei, O.; Erickson, M.A.; Newton, P.O.; Samdani, A.F.; Shah, S.A.; Shufflebarger, H.L.; et al. Intraoperative neuromonitoring predicts postoperative deficits in severe pediatric spinal deformity patients. Spine Deform. 2024, 12, 109–118. [Google Scholar] [CrossRef]
- Hou, Y.; Liu, H.; Wang, Z. Research status and development trend of smart sitting posture correction garment. Fangzhi Xuebao/J. Text. Res. 2024, 45, 250–258. [Google Scholar] [CrossRef]
- Kim, H.; Won, Y.I.; Kang, S.; Choi, Y.; Park, J.H.; Lee, J.; Kim, I.Y.; Chung, C.K. Comparison of Neck Pain and Posture with Spine Angle Tracking System between Static and Dynamic Computer Monitor Use. Electronics 2024, 13, 1363. [Google Scholar] [CrossRef]
- Kovalenko, A.; Misikov, V.; Kondur, A. Methodology of Botulinum Therapy in the Treatment of Dystonic Scoliosis in Generalized Dystonia (clinical case). Toxicon 2024, 237, 107424. [Google Scholar] [CrossRef]
- Leoncini, S.; Boasiako, L.; Di Lucia, S.; Beker, A.; Scandurra, V.; Vignoli, A.; Canevini, M.P.; Prato, G.; Nobili, L.; Nicotera, A.G.; et al. 24-h continuous non-invasive multiparameter home monitoring of vitals in patients with Rett syndrome by an innovative wearable technology: Evidence of an overlooked chronic fatigue status. Front. Neurol. 2024, 15, 1388506. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, A.; Kazim, H.; Eltawil, M.; Aburukba, R. IoT-Based Solution for Detecting and Monitoring Upper Crossed Syndrome. Sensors 2024, 24, 135. [Google Scholar] [CrossRef] [PubMed]
- Shigematsu, H.; Yasuda, A.; Tangente, R.; Chan, C.Y.W.; Shetty, A.P.; Cheung, J.P.Y.; Hai, Y.; Sakai, D.; Cho, K.J.; Chen, C.W.; et al. Current trends in intraoperative neurophysiological monitoring among Asia-Pacific countries: An Asia-Pacific Spine Society survey. Asian Spine J. 2024, 18, 813–821. [Google Scholar] [CrossRef]
- Vos, N.; Kleinendorst, L.; van der Laan, L.; van Uhm, J.; Jansen, P.R.; van Eeghen, A.M.; Maas, S.M.; Mannens, M.M.A.M.; van Haelst, M.M. Evaluation of 100 Dutch cases with 16p11.2 deletion and duplication syndromes; from clinical manifestations towards personalized treatment options. Eur. J. Hum. Genet. 2024, 32, 1387–1401. [Google Scholar] [CrossRef]
- Yang, X.; Fu, R.; Li, P.; Wang, K.; Chen, H. A New Method for Predicting the Porosity of an Interbody Fusion Cage by the Equivalent Material Method. J. Med. Biol. Eng. 2024, 44, 90–98. [Google Scholar] [CrossRef]
- Girdler, S.; Cho, B.; Mikhail, C.M.; Cheung, Z.B.; Maza, N.; Cho, S.K.W. Emerging Techniques in Diagnostic Imaging for Idiopathic Scoliosis in Children and Adolescents: A Review of the Literature. World Neurosurg. 2020, 136, 128–135. [Google Scholar] [CrossRef]
- Huang, R.; Maag, A.; Bhuiyan, M. Augmented reality navigation in spine surgery. In Proceedings of the 2020 5th International Conference on Innovative Technologies in Intelligent Systems and Industrial Applications (CITISIA), Sydney, Australia, 25–27 November 2020. [Google Scholar]
- Applebaum, A.; Ference, R.; Cho, W. Evaluating the role of surface topography in the surveillance of scoliosis. Spine Deform. 2020, 8, 397–404. [Google Scholar] [CrossRef]
- Moreira, R.; Teles, A.; Fialho, R.; Baluz, R.; Santos, T.C.; Goulart, R.; Rocha, L.; Silva, F.J.; Gupta, N.; Bastos, V.H.; et al. Mobile Applications for Assessing Human Posture: A Systematic Literature Review. Electronics 2020, 9, 1196. [Google Scholar] [CrossRef]
- Yan, D.; Vassar, R. Neuromuscular electrical stimulation for motor recovery in pediatric neurological conditions: A scoping review. Dev. Med. Child Neurol. 2021, 63, 1394–1401. [Google Scholar] [CrossRef]
- Kamalapathy, P.N.; Karhade, A.V.; Tobert, D.; Schwab, J.H. Artificial Intelligence in Adult Spinal Deformity. In Acta Neurochirurgica, Supplementum; Springer: Berlin/Heidelberg, Germany, 2022; Volume 134, pp. 313–318. [Google Scholar]
- Li, X.; Huo, Z.; Hu, Z.; Lam, T.P.; Cheng, J.C.Y.; Chung, V.C.; Yip, B.H.K. Which interventions may improve bracing compliance in adolescent idiopathic scoliosis? A systematic review and meta-analysis. PLoS ONE 2022, 17, e0271612. [Google Scholar] [CrossRef] [PubMed]
- Ameta, K.L.; Solanki, V.S.; Singh, V.; Devi, A.P.; Chundawat, R.S.; Haque, S. Critical appraisal and systematic review of 3D & 4D printing in sustainable and environment-friendly smart manufacturing technologies. Sustain. Mater. Technol. 2022, 34, e00481. [Google Scholar] [CrossRef]
- Syamlan, A.; Fathurachman; Denis, K.; Vander Poorten, E.; Pramujati, B.; Tjahjowidodo, T. Haptic/virtual reality orthopedic surgical simulators: A literature review. Virtual Real. 2022, 26, 1795–1825. [Google Scholar] [CrossRef]
- Karandikar, P.; Massaad, E.; Hadzipasic, M.; Kiapour, A.; Joshi, R.S.; Shankar, G.M.; Shin, J.H. Machine Learning Applications of Surgical Imaging for the Diagnosis and Treatment of Spine Disorders: Current State of the Art. Neurosurgery 2022, 90, 372–382. [Google Scholar] [CrossRef]
- Ng, P.T.T.; Claus, A.; Izatt, M.T.; Pivonka, P.; Tucker, K. Is spinal neuromuscular function asymmetrical in adolescents with idiopathic scoliosis compared to those without scoliosis?: A narrative review of surface EMG studies. J. Electromyogr. Kinesiol. 2022, 63, 102640. [Google Scholar] [CrossRef]
- Grivas, T.B.; Negrini, S.; Aubin, C.E.; Aulisa, A.G.; De Mauroy, J.C.; Donzelli, S.; Hresko, M.T.; Kotwicki, T.; Lou, E.; Maruyama, T.; et al. Nonoperative management of adolescent idiopathic scoliosis (AIS) using braces. Prosthet. Orthot. Int. 2022, 46, 383–391. [Google Scholar] [CrossRef]
- Webster, T. 25 years of commercializing nanomedicine: From tissue engineering to fighting COVID. Tissue Eng. Part A 2022, 28, 335. [Google Scholar] [CrossRef]
- Bottino, L.; Settino, M.; Cannataro, M. Distributed ICT solutions for scoliosis management. In Proceedings of the 2023 31st Euromicro International Conference on Parallel, Distributed and Network-Based Processing (PDP), Naples, Italy, 1–3 March 2023; pp. 258–262. [Google Scholar]
- Cerillo, J.L.; Becsey, A.N.; Sanghadia, C.P.; Root, K.T.; Lucke-Wold, B. Spine Bracing: When to Utilize-A Narrative Review. Biomechanics 2023, 3, 136–154. [Google Scholar] [CrossRef]
- Cordani, C.; Malisano, L.; Febbo, F.; Giranio, G.; Del Furia, M.J.; Donzelli, S.; Negrini, S. Influence of Specific Interventions on Bracing Compliance in Adolescents with Idiopathic Scoliosis-A Systematic Review of Papers Including Sensors’ Monitoring. Sensors 2023, 23, 7660. [Google Scholar] [CrossRef] [PubMed]
- Kurland, D.; Bi, C.; Ber, R.; Kondziolka, D.; Lau, D.; Pacione, D.; Frempong-Boadu, A.; Laufer, I.; Oermann, E. P464: Smartphones, wearables, and digital biomarkers: The evolution of spine care outcomes research. Glob. Spine J. 2023, 13, 458S. [Google Scholar] [CrossRef]
- Khan, M.A.; Pogonchenkova, I.V.; Talkovsky, E.M.; Vybornov, D.Y.; Kuyantseva, L.V.; Tarasov, N.I.; Koroteev, V.V. Electrical Stimulation Methods for Scoliosis in Children: A Literature Review. Vestn. Vosstanov. Med. 2024, 23, 116–124. [Google Scholar] [CrossRef]
- Paramento, M.; Passarotto, E.; Maccarone, M.C.; Agostini, M.; Contessa, P.; Rubega, M.; Formaggio, E.; Masiero, S. Neurophysiological, balance and motion evidence in adolescent idiopathic scoliosis: A systematic review. PLoS ONE 2024, 19, e0303086. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Chang, B.S.; Chang, S.Y. Current issues in the treatment of adolescent idiopathic scoliosis: A comprehensive narrative review. Asian Spine J. 2024, 18, 731–742. [Google Scholar] [CrossRef]
- Cheng, F.; Lu, L.; Sun, M.; Wang, X.; Wang, Y. Non-invasive Scoliosis Assessment in Adolescents. In Multimedia Technology and Enhanced Learning; Springer: Berlin/Heidelberg, Germany, 2024; pp. 221–230. [Google Scholar]
- Agravante, A.N.L.; Carpeso, I.R.T.; Guillermo, K.M.S.; Lim, K.D.C.; Lim, R.A.U.; Lopez, N.N.C.; Baldovino, R.G. Emerging Technologies of Sensor-Based Assistive Devices for Spinal Position Monitoring: A Review. In Proceedings of the 2024 5th International Conference on Biomedical Engineering (IBIOMED), Bali, Indonesia, 23–25 October 2024; pp. 23–28. [Google Scholar]
- Lee, S.; Jung, J.Y.; Mahatthanatrakul, A.; Kim, J.S. Artificial Intelligence in Spinal Imaging and Patient Care: A Review of Recent Advances. Neurospine 2024, 21, 474–486. [Google Scholar] [CrossRef]
- Karimi, M.T.; Kavyani, M. Evaluation of the effectiveness of soft braces on idiopathic scoliosis: A review of literature. J. Orthop. Trauma Rehabil. 2024, 31, 85–92. [Google Scholar] [CrossRef]
- Förstl, N.; Adler, I.; Süss, F.; Dendorfer, S. Technologies for Evaluation of Pelvic Floor Functionality: A Systematic Review. Sensors 2024, 24, 4001. [Google Scholar] [CrossRef]
- Ratnaparkhi, A.; Beckett, J. Digital Phenotyping, Wearables, and Outcomes. Neurosurg. Clin. N. Am. 2024, 35, 235–241. [Google Scholar] [CrossRef]
- Luo, C.; Wu, H.; Liu, W.; Luo, Y.; Jie, Y.; Ma, C.Z.H.; Wong, M. The Biomechanics of Spinal Orthoses for Adolescent Idiopathic Scoliosis: A Systematic Review of the Controlling Forces. Bioengineering 2024, 11, 1242. [Google Scholar] [CrossRef]
- Kaelin, A.J. Adolescent idiopathic scoliosis: Indications for bracing and conservative treatments. Ann. Transl. Med. 2020, 8, 28. [Google Scholar] [CrossRef] [PubMed]
- Tapp, A.; Payer, C.; Schmid, J.; Polanco, M.; Kumi, I.; Bawab, S.; Ringleb, S.; St. Remy, C.; Bennett, J.; Kakar, R.S.; et al. Generation of Patient-Specific, Ligamentoskeletal, Finite Element Meshes for Scoliosis Correction Planning. In Clinical Image-Based Procedures, Distributed and Collaborative Learning, Artificial Intelligence for Combating COVID-19 and Secure and Privacy-Preserving Machine Learning; Springer: Berlin/Heidelberg, Germany, 2021; pp. 13–23. [Google Scholar]
- Negrini, S.; Aulisa, A.G.; Cerny, P.; de Mauroy, J.C.; McAviney, J.; Mills, A.; Donzelli, S.; Grivas, T.B.; Hresko, M.T.; Kotwicki, T.; et al. The classification of scoliosis braces developed by SOSORT with SRS, ISPO, and POSNA and approved by ESPRM. Eur. Spine J. 2022, 31, 980–989. [Google Scholar] [CrossRef] [PubMed]
- Te Hennepe, N.; Steegh, V.; Pouw, M.H.; Roukema, J.; De Kleuver, M.; Van Hooff, M.L. Pulmonary function in patients with adolescent idiopathic scoliosis: An explorative study of a wearable smart shirt as a measurement instrument. Spine Deform. 2025, 13, 101–110. [Google Scholar] [CrossRef] [PubMed]

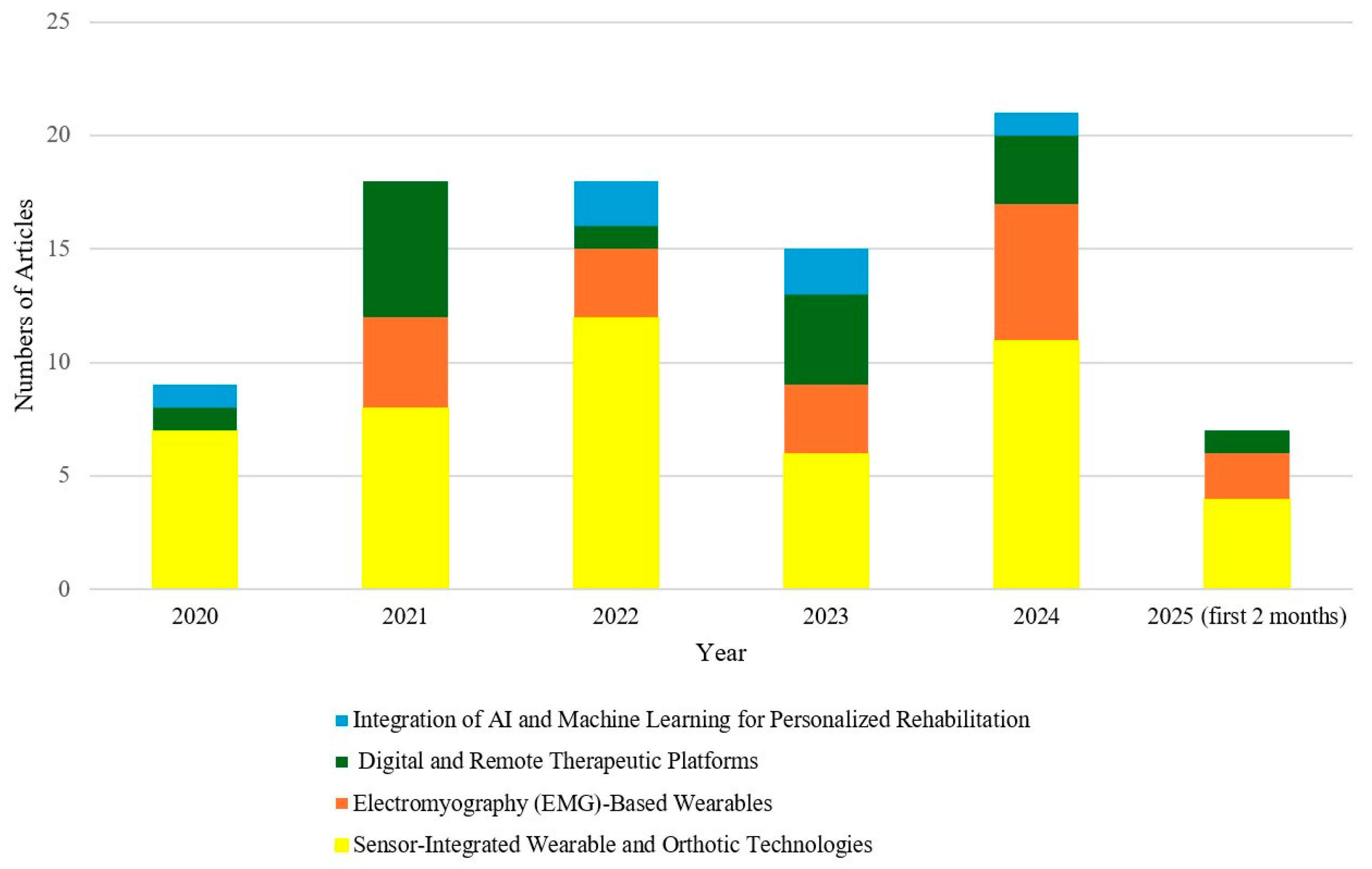


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fazeli Veisari, S.; Bidari, S.; Barati, K.; Atlasi, R.; Komeili, A. Wearable Devices in Scoliosis Treatment: A Scoping Review of Innovations and Challenges. Bioengineering 2025, 12, 696. https://doi.org/10.3390/bioengineering12070696
Fazeli Veisari S, Bidari S, Barati K, Atlasi R, Komeili A. Wearable Devices in Scoliosis Treatment: A Scoping Review of Innovations and Challenges. Bioengineering. 2025; 12(7):696. https://doi.org/10.3390/bioengineering12070696
Chicago/Turabian StyleFazeli Veisari, Samira, Shahrbanoo Bidari, Kourosh Barati, Rasha Atlasi, and Amin Komeili. 2025. "Wearable Devices in Scoliosis Treatment: A Scoping Review of Innovations and Challenges" Bioengineering 12, no. 7: 696. https://doi.org/10.3390/bioengineering12070696
APA StyleFazeli Veisari, S., Bidari, S., Barati, K., Atlasi, R., & Komeili, A. (2025). Wearable Devices in Scoliosis Treatment: A Scoping Review of Innovations and Challenges. Bioengineering, 12(7), 696. https://doi.org/10.3390/bioengineering12070696








