Flexible Syndesmotic Reconstruction with Two Suture Buttons Provides Equal Stability Compared to Syndesmotic Screws: A Biomechanical Study
Abstract
1. Introduction
2. Materials and Methods
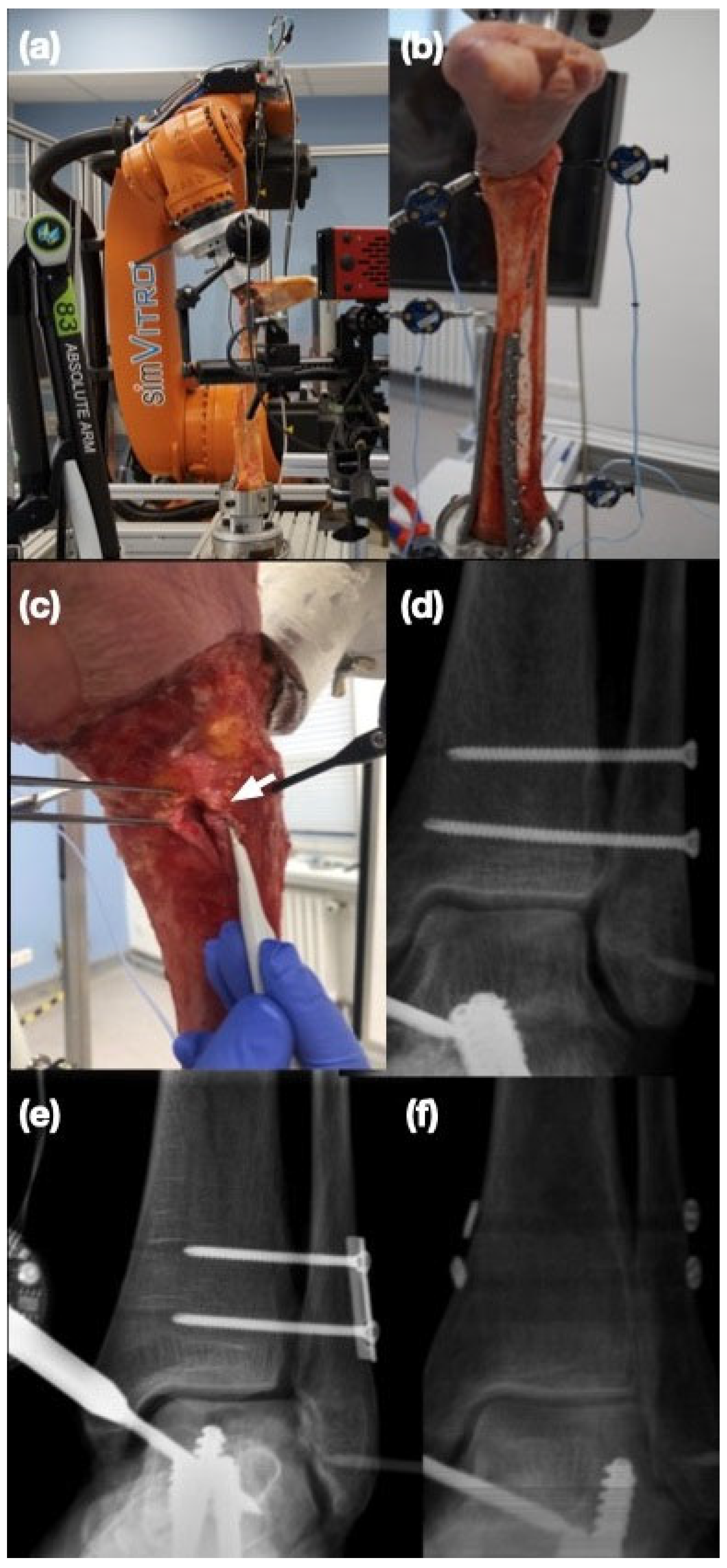
2.1. Specimen Preparation
2.2. Biomechanical Setup
2.3. Study Protocol
2.4. Sequential Cutting
2.5. Syndesmotic Screw Fixation
2.6. Suture Button Fixation
2.7. Statistical Analysis
3. Results
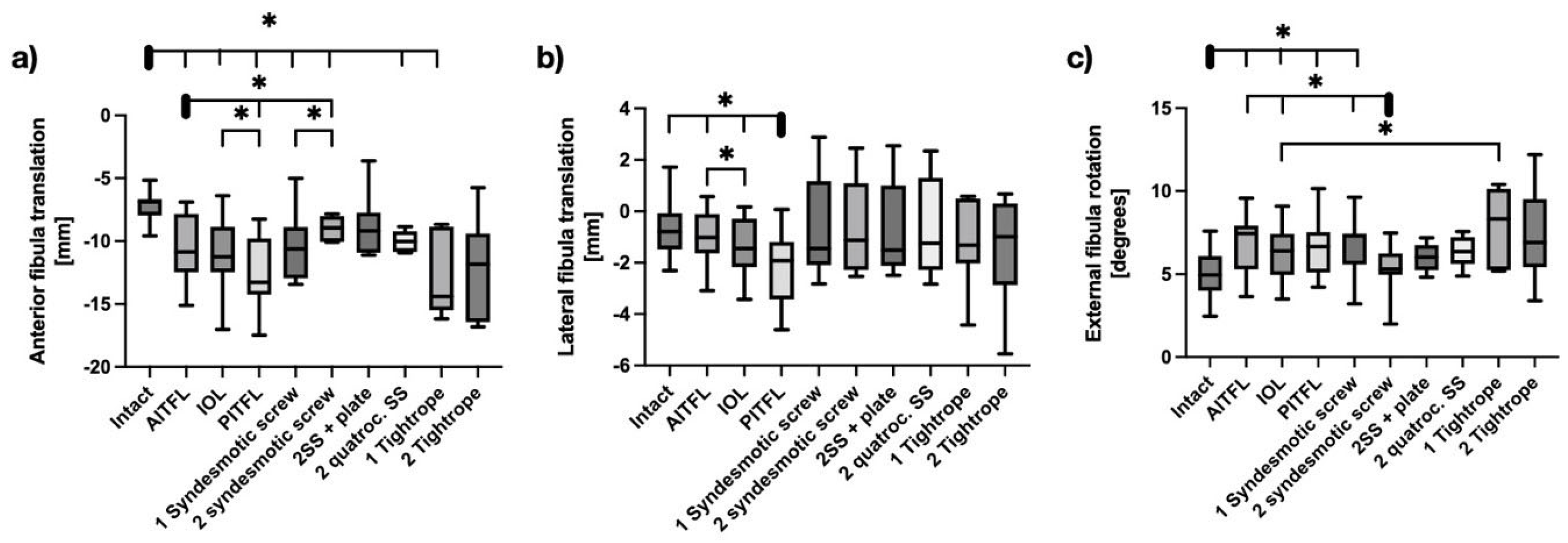
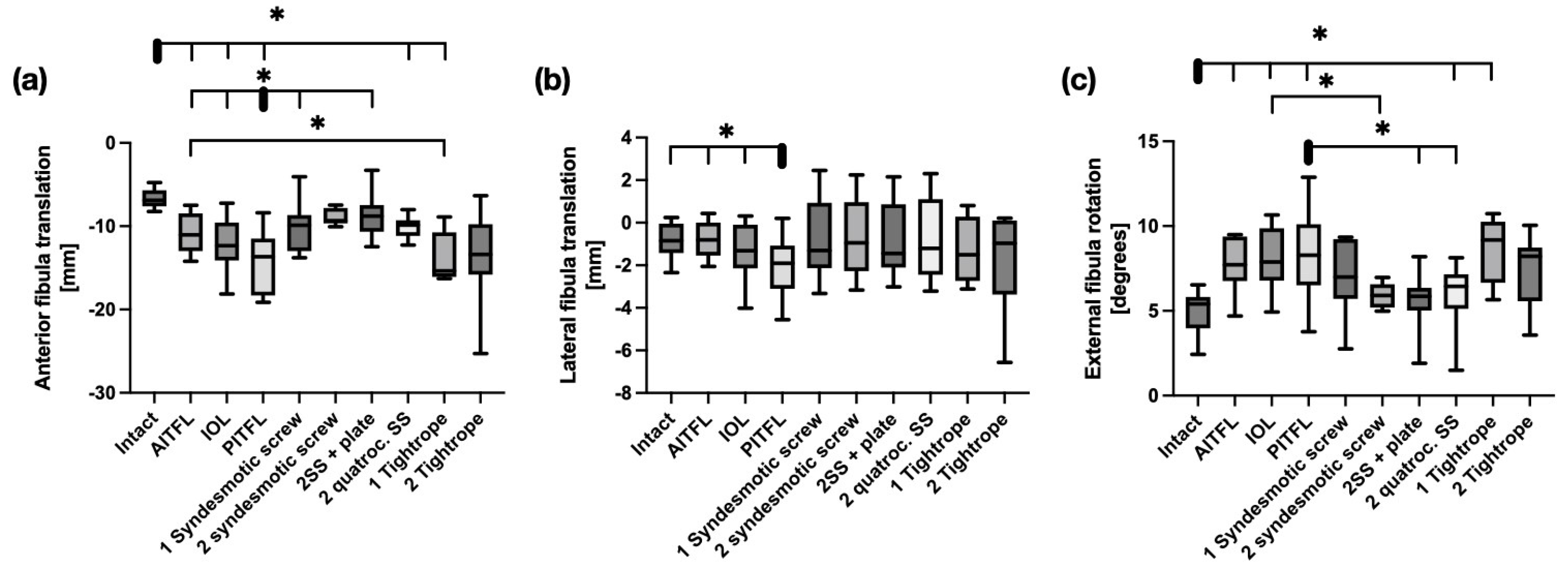
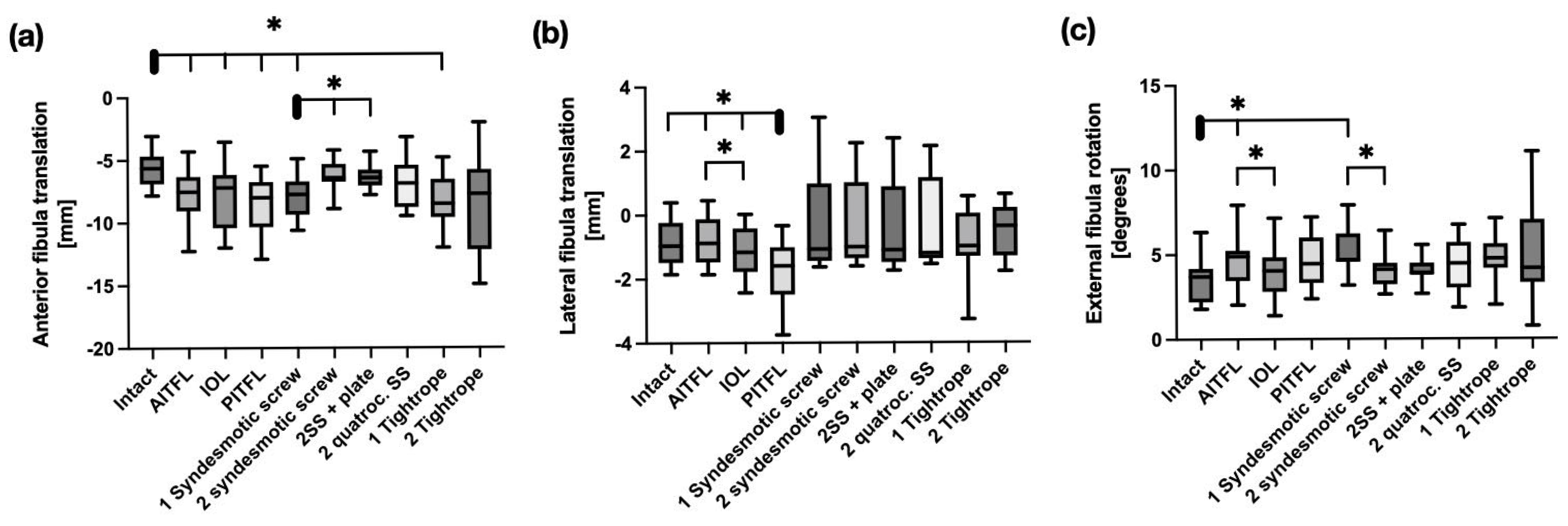
3.1. Cutting of the Syndesmosis
3.2. Syndesmotic Reconstruction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AITFL | Anterior inferior tibiofibular ligament |
| IOL | Interosseus Ligament |
| PITFL | Posterior inferior tibiofibular ligament |
| RCT | Randomized controlled trial |
| mm | Millimeter |
| N | Newton |
| Nm | Newtonmeter |
References
- McCollum, G.A.; van den Bekerom, M.P.J.; Kerkhoffs, G.M.M.J.; Calder, J.D.F.; van Dijk, C.N. Syndesmosis and Deltoid Ligament Injuries in the Athlete. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1328–1337. [Google Scholar] [CrossRef] [PubMed]
- Kellett, J.J.; Lovell, G.A.; Eriksen, D.A.; Sampson, M.J. Diagnostic Imaging of Ankle Syndesmosis Injuries: A General Review. J. Méd. Imaging Radiat. Oncol. 2018, 62, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Delahunt, E.; Farrell, G.; Boylan, A.; Kerin, F.; Tierney, P.; Hogan, H.; Boreham, C. Mechanisms of Acute Ankle Syndesmosis Ligament Injuries in Professional Male Rugby Union Players: A Systematic Visual Video Analysis. Br. J. Sports Med. 2021, 55, 691–696. [Google Scholar] [CrossRef]
- Baltes, T.P.A.; Sayrafi, O.A.; Arnáiz, J.; Al-Naimi, M.R.; Geertsema, C.; Geertsema, L.; Holtzhausen, L.; D’Hooghe, P.; Kerkhoffs, G.M.M.J.; Tol, J.L. Acute Clinical Evaluation for Syndesmosis Injury Has High Diagnostic Value. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3871–3880. [Google Scholar] [CrossRef]
- Lehtola, R.; Leskelä, H.-V.; Flinkkilä, T.; Pakarinen, H.; Niinimäki, J.; Savola, O.; Ohtonen, P.; Kortekangas, T. Suture Button versus Syndesmosis Screw Fixation in Pronation-External Rotation Ankle Fractures: A Minimum 6-Year Follow-up of a Randomised Controlled Trial. Injury 2021, 52, 3143–3149. [Google Scholar] [CrossRef]
- Elabd, A.; Abdullah, S.; Kandel, W.; Hegazy, M. Syndesmotic Stabilization: Syndesmotic Screw Versus Flexible Fixation: A Systematic Review. J. Foot Ankle Surg. 2021, 60, 998–1007. [Google Scholar] [CrossRef]
- Ræder, B.W.; Figved, W.; Madsen, J.E.; Frihagen, F.; Jacobsen, S.B.; Andersen, M.R. Better Outcome for Suture Button Compared with Single Syndesmotic Screw for Syndesmosis Injury: Five-Year Results of a Randomized Controlled Trial. Bone Jt. J. 2020, 102-B, 212–219. [Google Scholar] [CrossRef]
- Pavone, V.; Papotto, G.; Vescio, A.; Longo, G.; D’Amato, S.; Ganci, M.; Marchese, E.; Testa, G. Short and Middle Functional Outcome in the Static vs. Dynamic Fixation of Syndesmotic Injuries in Ankle Fractures: A Retrospective Case Series Study. J. Clin. Med. 2023, 12, 3637. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, S.; Wang, Z.; Li, A.; Ding, J. Meta-Analysis of Elastic versus Rigid Fixation in the Treatment of Acute Tibiofibular Syndesmosis Injury. Syst. Rev. 2024, 13, 51. [Google Scholar] [CrossRef]
- Lee, S.-W.; Yoon, S.-J.; Jung, K.-J.; Yeo, E.-D.; Won, S.-H.; Hong, C.-H.; Wang, S.-D.; Cho, Y.-C.; Ji, J.-Y.; Byeon, J.-Y.; et al. Anterior and Posterior Syndesmotic Augmentation Using Nonabsorbable Suture Tape for Acute Syndesmotic Instability: A Technical Note. J. Clin. Med. 2025, 14, 2207. [Google Scholar] [CrossRef]
- Milstrey, A.; Gartung, S.; Klimek, M.; Wermers, J.; Raschke, M.J.; Ochman, S. Assessing the Need for Additional Syndesmotic Stabilization in Open Reduction of the Posterior Malleolus: A Biomechanical Study. J. Bone Jt. Surg. 2025, 107, 1377–1385. [Google Scholar] [CrossRef]
- Shoji, H.; Teramoto, A.; Suzuki, D.; Okada, Y.; Sakakibara, Y.; Matsumura, T.; Suzuki, T.; Watanabe, K.; Yamashita, T. Suture-Button Fixation and Anterior Inferior Tibiofibular Ligament Augmentation with Suture-Tape for Syndesmosis Injury: A Biomechanical Cadaveric Study. Clin. Biomech. 2018, 60, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Candal-Couto, J.J.; Burrow, D.; Bromage, S.; Briggs, P.J. Instability of the Tibio-Fibular Syndesmosis: Have We Been Pulling in the Wrong Direction? Injury 2004, 35, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, P.; Hamilton, W. Changes in Tibiotalar Area of Contact Caused by Lateral Talar Shift. J. Bone Jt. Surg. 1976, 58, 356–357. [Google Scholar] [CrossRef]
- Er, M.S.; Verim, O.; Eroglu, M.; Altinel, L.; Gokce, B.; Tasgetiren, S. Biomechanical Evaluation of Syndesmotic Screw Design via Finite Element Analysis and Taguchi’s Method. J. Am. Podiatr. Méd. Assoc. 2015, 105, 14–21. [Google Scholar] [CrossRef]
- Xenos, J.S.; Hopkinson, W.J.; Mulligan, M.E.; Olson, E.J.; Popovic, N.A. The Tibiofibular Syndesmosis. Evaluation of the Ligamentous Structures, Methods of Fixation, and Radiographic Assessment. J. Bone Jt. Surg. 1995, 77, 847–856. [Google Scholar] [CrossRef]
- Moore, J.A.; Shank, J.R.; Morgan, S.J.; Smith, W.R. Syndesmosis Fixation: A Comparison of Three and Four Cortices of Screw Fixation Without Hardware Removal. Foot Ankle Int. 2006, 27, 567–572. [Google Scholar] [CrossRef]
- Markolf, K.L.; Jackson, S.R.; McAllister, D.R. Syndesmosis Fixation Using Dual 3.5 Mm and 4.5 Mm Screws with Tricortical and Quadricortical Purchase. Foot Ankle Int. 2013, 34, 734–739. [Google Scholar] [CrossRef]
- Nousiainen, M.T.; McConnell, A.J.; Zdero, R.; McKee, M.D.; Bhandari, M.; Schemitsch, E.H. The Influence of the Number of Cortices of Screw Purchase and Ankle Position in Weber C Ankle Fracture Fixation. J. Orthop. Trauma 2008, 22, 473–478. [Google Scholar] [CrossRef]
- Beumer, A.; Campo, M.M.; Niesing, R.; Day, J.; Kleinrensink, G.-J.; Swierstra, B.A. Screw Fixation of the Syndesmosis: A Cadaver Model Comparing Stainless Steel and Titanium Screws and Three and Four Cortical Fixation. Injury 2005, 36, 60–64. [Google Scholar] [CrossRef]
- Stuart, K.; Panchbhavi, V.K. The Fate of Syndesmotic Screws. Foot Ankle Int. 2011, 32, 519–525. [Google Scholar] [CrossRef]
- Manjoo, A.; Sanders, D.W.; Tieszer, C.; MacLeod, M.D. Functional and Radiographic Results of Patients with Syndesmotic Screw Fixation: Implications for Screw Removal. J. Orthop. Trauma 2010, 24, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Jordan, T.H.; Talarico, R.H.; Schuberth, J.M. The Radiographic Fate of the Syndesmosis after Trans-Syndesmotic Screw Removal in Displaced Ankle Fractures. J. Foot Ankle Surg. 2011, 50, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Wikerøy, A.K.B.; Høiness, P.R.; Andreassen, G.S.; Hellund, J.C.; Madsen, J.E. No Difference in Functional and Radiographic Results 8.4 Years After Quadricortical Compared with Tricortical Syndesmosis Fixation in Ankle Fractures. J. Orthop. Trauma 2010, 24, 17–23. [Google Scholar] [CrossRef]
- Gardner, R.; Yousri, T.; Holmes, F.; Clark, D.; Pollintine, P.; Miles, A.W.; Jackson, M. Stabilization of the Syndesmosis in the Maisonneuve Fracture—A Biomechanical Study Comparing 2-Hole Locking Plate and Quadricortical Screw Fixation. J. Orthop. Trauma 2013, 27, 212–216. [Google Scholar] [CrossRef]
- Kurtoglu, A.; Kochai, A.; Inanmaz, M.E.; Sukur, E.; Keskin, D.; Türker, M.; Uysal, M.; Sen, Z.; Daldal, I. A Comparison of Double Single Suture-Button Fixation, Suture-Button Fixation, and Screw Fixation for Ankle Syndesmosis Injury. Medicine 2021, 100, e25328. [Google Scholar] [CrossRef]
- Clanton, T.O.; Whitlow, S.R.; Williams, B.T.; Liechti, D.J.; Backus, J.D.; Dornan, G.J.; Saroki, A.J.; Turnbull, T.L.; LaPrade, R.F. Biomechanical Comparison of 3 Current Ankle Syndesmosis Repair Techniques. Foot Ankle Int. 2017, 38, 200–207. [Google Scholar] [CrossRef]
- Tsai, J.; Pivec, R.; Jauregui, J.J.; Hayes, W.T.; McLeold, M.; Naziri, Q.; Kapadia, B.V.; Saha, S.; Uribe, J.A. Strength of Syndesmosis Fixation: Two TightRope versus One TightRope with Plate-and-Screw Construct. J. Long-Term Eff. Méd. Implant. 2017, 26, 161–165. [Google Scholar] [CrossRef]
- Parker, A.S.; Beason, D.P.; Slowik, J.S.; Sabatini, J.B.; Waldrop, N.E. Biomechanical Comparison of 3 Syndesmosis Repair Techniques with Suture Button Implants. Orthop. J. Sports Med. 2018, 6, 2325967118804204. [Google Scholar] [CrossRef]
- Stake, I.K.; Bryniarski, A.R.; Brady, A.W.; Miles, J.W.; Dornan, G.J.; Madsen, J.E.; Haytmanek, C.T.; Husebye, E.E.; Clanton, T.O. Effect of Posterior Malleolar Fixation on Syndesmotic Stability. Am. J. Sports Med. 2022, 51, 997–1006. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milstrey, A.; Hoell, V.; Weigel, A.-S.C.; Wermers, J.; Gartung, S.; Evers, J.; Raschke, M.J.; Ochman, S. Flexible Syndesmotic Reconstruction with Two Suture Buttons Provides Equal Stability Compared to Syndesmotic Screws: A Biomechanical Study. Bioengineering 2025, 12, 685. https://doi.org/10.3390/bioengineering12070685
Milstrey A, Hoell V, Weigel A-SC, Wermers J, Gartung S, Evers J, Raschke MJ, Ochman S. Flexible Syndesmotic Reconstruction with Two Suture Buttons Provides Equal Stability Compared to Syndesmotic Screws: A Biomechanical Study. Bioengineering. 2025; 12(7):685. https://doi.org/10.3390/bioengineering12070685
Chicago/Turabian StyleMilstrey, Alexander, Vivienne Hoell, Ann-Sophie C. Weigel, Jens Wermers, Stella Gartung, Julia Evers, Michael J. Raschke, and Sabine Ochman. 2025. "Flexible Syndesmotic Reconstruction with Two Suture Buttons Provides Equal Stability Compared to Syndesmotic Screws: A Biomechanical Study" Bioengineering 12, no. 7: 685. https://doi.org/10.3390/bioengineering12070685
APA StyleMilstrey, A., Hoell, V., Weigel, A.-S. C., Wermers, J., Gartung, S., Evers, J., Raschke, M. J., & Ochman, S. (2025). Flexible Syndesmotic Reconstruction with Two Suture Buttons Provides Equal Stability Compared to Syndesmotic Screws: A Biomechanical Study. Bioengineering, 12(7), 685. https://doi.org/10.3390/bioengineering12070685





