Running and Jumping After Muscle Fatigue in Subjects with a History of Knee Injury: What Are the Acute Effects of Wearing a Knee Brace on Biomechanics?
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Experimental Setup and Data Acquisition
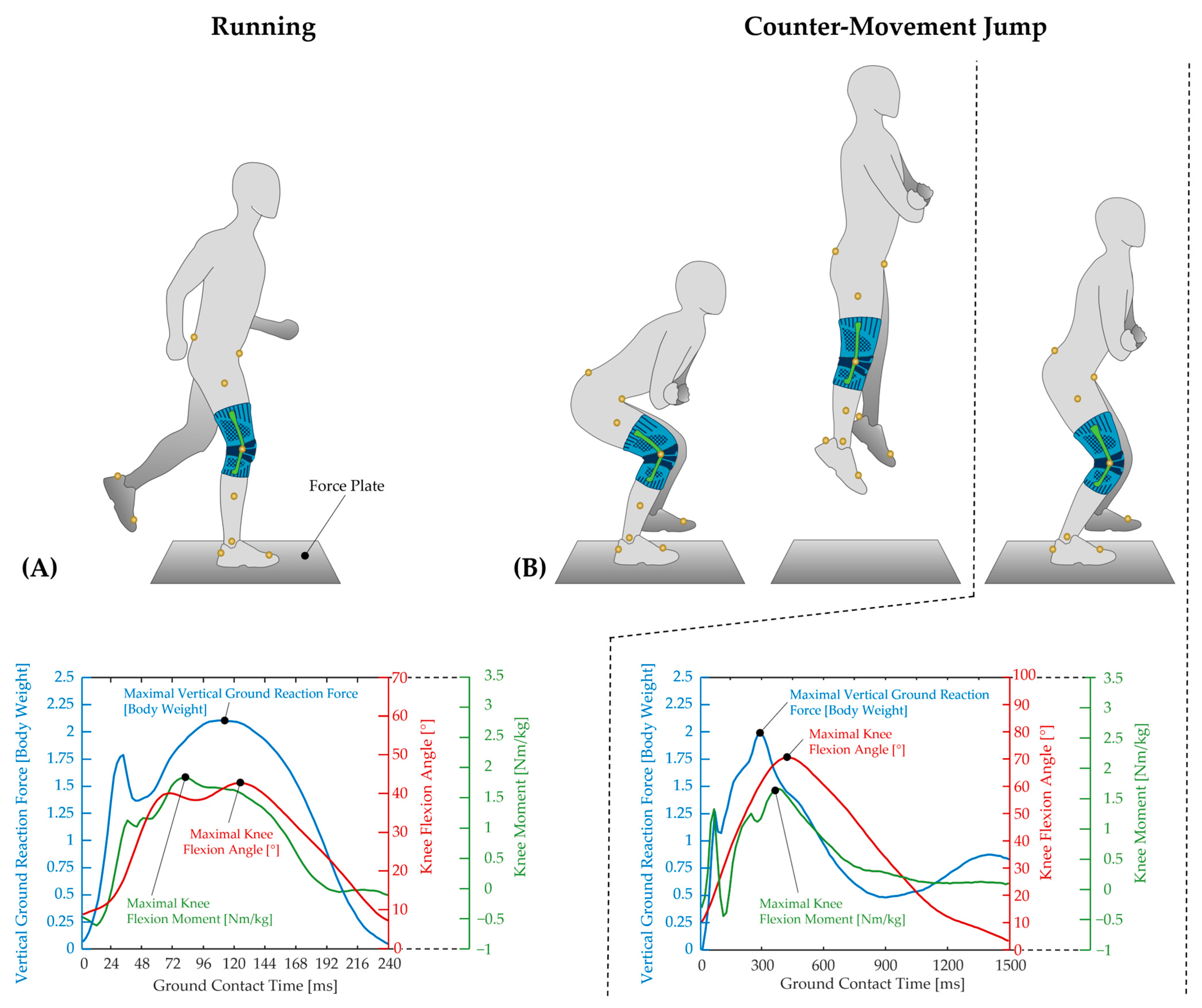
Running and Jumping Tests
2.3. Statistical Analysis
3. Results
3.1. Demographic, Clinical, and Subjective Data
3.2. Motor Performance
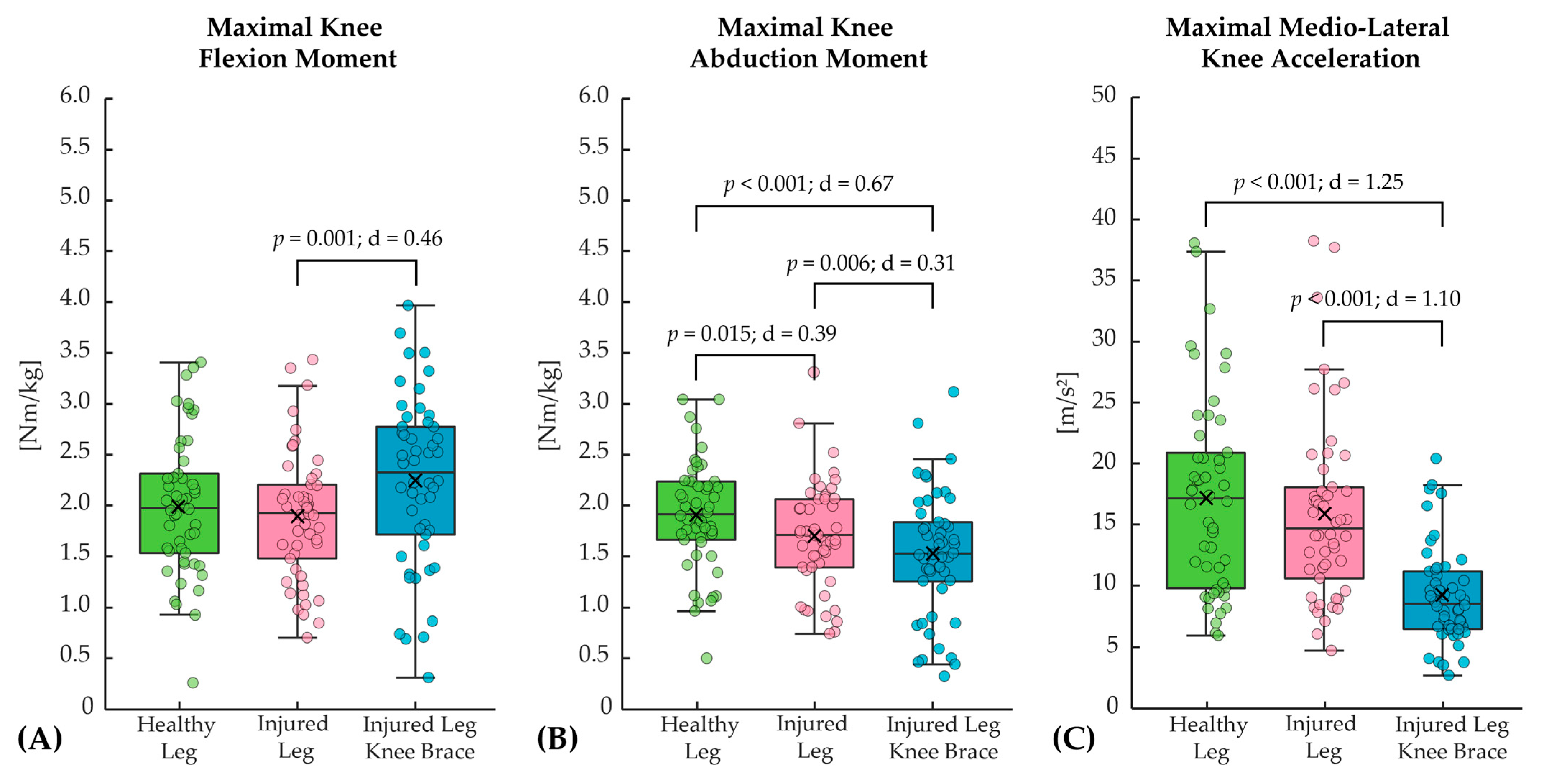
3.2.1. Running
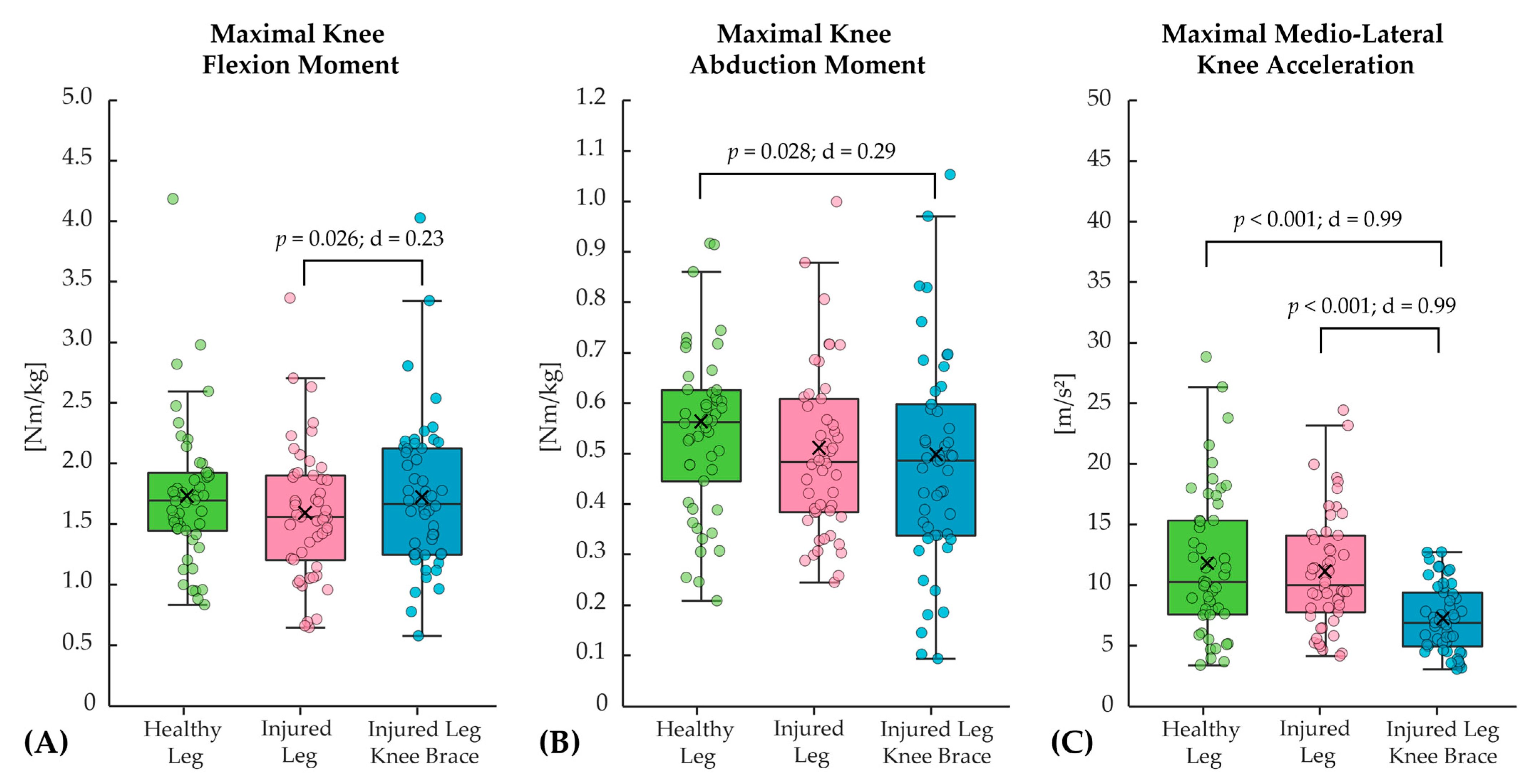
3.2.2. Counter-Movement Jump
4. Discussion
4.1. Effects of the Injuries
4.2. Effects of the Knee Brace
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| VAS | visual analog scale |
| ACL | anterior cruciate ligament |
References
- Adhitya, I.P.G.S.; Yu, W.-Y.; Kurniawati, I.; Lin, M.-R. Risk factors of knee reinjury after anterior cruciate ligament reconstruction. Int. Orthop. 2024, 48, 983–990. [Google Scholar] [CrossRef]
- Hughes, G.; Watkins, J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006, 36, 411–428. [Google Scholar] [CrossRef] [PubMed]
- Butler, L.; Olander, H.L.; Erdman, A.; Ulman, S. Relationship of knee abduction moment to lower extremity segment accelerations during sport-specific movements in youth anterior cruciate ligament reconstruction patients at return-to-play. Clin. Biomech. 2025, 124, 106485. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.; Li, R.; Wang, H.; Wang, Z. Mechanism and Prevention of Acute Knee Joint Injury During Exercise. Trans. Mater. Biotechnol. Life Sci. 2024, 7, 728–734. [Google Scholar] [CrossRef]
- Chia, L.; Silva, D.D.O.; Whalan, M.; McKay, M.J.; Sullivan, J.; Fuller, C.W.; Pappas, E. Epidemiology of gradual-onset knee injuries in team ball-sports: A systematic review with meta-analysis of prevalence, incidence, and burden by sex, sport, age, and participation level. J. Sci. Med. Sport 2022, 25, 834–844. [Google Scholar] [CrossRef]
- Almaawi, A.; Awwad, W.; Bamugaddam, A.; Alasheikh, M.; Muaddi, M.; Almutair, O.; Alomar, A.Z. Prevalence of knee injuries among male college students in Riyadh, Kingdom of Saudi Arabia. J. Orthop. Surg. Res. 2020, 15, 126. [Google Scholar] [CrossRef]
- Nicolini, A.P.; de Carvalho, R.T.; Matsuda, M.M.; Sayum, J.F.; Cohen, M. Common injuries in athletes’ knee: Experience of a specialized center. Acta Ortop. Bras. 2014, 22, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Majewski, M.; Susanne, H.; Klaus, S. Epidemiology of athletic knee injuries: A 10-year study. Knee 2006, 13, 184–188. [Google Scholar] [CrossRef]
- Bollen, S. Epidemiology of knee injuries: Diagnosis and triage. Br. J. Sports Med. 2000, 34, 227–228. [Google Scholar] [CrossRef]
- Griffin, L.Y.; Albohm, M.J.; Arendt, E.A.; Bahr, R.; Beynnon, B.D.; Demaio, M.; Dick, R.W.; Engebretsen, L.; Garrett, W.E.; Hannafin, J.A.; et al. Understanding and preventing noncontact anterior cruciate ligament injuries: A review of the Hunt Valley II meeting, January 2005. Am. J. Sports Med. 2006, 34, 1512–1532. [Google Scholar] [CrossRef]
- Barber-Westin, S.; Noyes, F.R. One in 5 Athletes Sustain Reinjury Upon Return to High-Risk Sports After ACL Reconstruction: A Systematic Review in 1239 Athletes Younger Than 20 Years. Sports Health 2020, 12, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Selin, A.S.; Gauffin, H.; Hedevik, H.; Fältström, A.; Kvist, J. More knee reinjuries after ACL reconstruction compared to nonsurgical treatment of the ACL. A 2-year follow-up of the NACOX prospective cohort study. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1709–1720. [Google Scholar] [CrossRef] [PubMed]
- Fältström, A.; Asker, M.; Weiss, N.; Lyberg, V.; Waldén, M.; Hägglund, M.; Tranaeus, U.; Skillgate, E. Poor knee strength is associated with higher incidence of knee injury in adolescent female football players: The Karolinska football injury cohort. Knee Surg. Sports Traumatol. Arthrosc. 2024. ahead of print. [Google Scholar] [CrossRef]
- Rishiraj, N.; Taunton, J.E.; Lloyd-Smith, R.; Regan, W.; Niven, B.; Woollard, R. Functional knee brace use for 21 h leads to a longer duration to achieve peak vertical ground reaction forces and the removal of the brace after 17.5 h results in faster loading of the knee joint. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, K.; Murakami, T.; Wada, C.; Yamamoto, H. Effect of Soft Knee Brace on Shank Movement in Running. J. Prosthet. Orthot. Sci. Technol. 2024, 3, 42–47. [Google Scholar] [CrossRef]
- Mougin, F.; Begon, M.; Desmyttere, G.; Bleau, J.; Nault, M.-L.; Cherni, Y. Knee Biomechanics during Walking in Individuals with Anterior Cruciate Ligament Repair: The Role of a Custom 3D Printed Knee Brace. bioRxiv 2024. preprints. [Google Scholar] [CrossRef]
- Moon, J.; Kim, H.; Lee, J.; Panday, S.B. Effect of wearing a knee brace or sleeve on the knee joint and anterior cruciate ligament force during drop jumps: A clinical intervention study. Knee 2018, 25, 1009–1015. [Google Scholar] [CrossRef]
- Yu, B.; Herman, D.; Preston, J.; Lu, W.; Kirkendall, D.T.; Garrett, W.E. Immediate effects of a knee brace with a constraint to knee extension on knee kinematics and ground reaction forces in a stop-jump task. Am. J. Sports Med. 2004, 32, 1136–1143. [Google Scholar] [CrossRef]
- Wang, J.; Yang, J.; Huang, X.; Luo, Y.; Wu, D.; Huang, X.; Wang, S. The effect of knee braces on knee joint kinematics at different exercise speeds. Sports Biomech. 2024, 23, 3526–3537. [Google Scholar] [CrossRef]
- Sinclair, J.K.; Vincent, H.; Richards, J.D. Effects of prophylactic knee bracing on knee joint kinetics and kinematics during netball specific movements. Phys. Ther. Sport 2017, 23, 93–98. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Dessery, Y.; Belzile, É.L.; Corbeil, P. Knee braces and foot orthoses multimodal 3-month treatment of medial knee osteoarthritis in a randomised crossover trial. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2919–2930. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Luo, Y.; Zhou, L.; Zhang, Z.; Zhao, Y.; Li, J.; Wu, D.; Wang, S. Kinematic study of the overall unloading brace for the knee. Heliyon 2023, 9, e13116. [Google Scholar] [CrossRef]
- Norinasab, S.; Jafarnezhadgero, A.A.; Siahkouhian, M.; Orang, A.V. Effect of using of brace in three different knee flexion angles on running economy and lower limb muscular co-contraction in individuals with genu varus. J. Arak Univ. Med. Sci. 2021, 23, 81–89. [Google Scholar]
- Siebers, H.L.; Eschweiler, J.; Pinz, J.; Tingart, M.; Rath, B. The effect of a knee brace in dynamic motion-An instrumented gait analysis. PLoS ONE 2020, 15, e0238722. [Google Scholar] [CrossRef] [PubMed]
- Mortaza, N.; Ebrahimi, I.; Jamshidi, A.A.; Abdollah, V.; Kamali, M.; Abas, W.A.B.W.; Osman, N.A.A. The effects of a prophylactic knee brace and two neoprene knee sleeves on the performance of healthy athletes: A crossover randomized controlled trial. PLoS ONE 2012, 7, e50110. [Google Scholar] [CrossRef]
- Baltaci, G.; Aktas, G.; Camci, E.; Oksuz, S.; Yildiz, S.; Kalaycioglu, T. The effect of prophylactic knee bracing on performance: Balance, proprioception, coordination, and muscular power. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1722–1728. [Google Scholar] [CrossRef]
- Kıyak, G.; Said Uyan, A.; Arslan, E.; Tolga Acar, H.; Ercan, S.; Çetin, C. The effects of knee brace use on landing error, balance, and crossover hop test in healthy athletes. Turk. J. Sports Med. 2024, 59, 105–111. [Google Scholar] [CrossRef]
- Ewing, K.A.; Begg, R.K.; Galea, M.P.; Lee, P.V.S. Effects of Prophylactic Knee Bracing on Lower Limb Kinematics, Kinetics, and Energetics During Double-Leg Drop Landing at 2 Heights. Am. J. Sports Med. 2016, 44, 1753–1761. [Google Scholar] [CrossRef]
- Murgier, J.; Duthon, V.; Deygas, A.; Ehkirch, F.-P. Does an early post traumatic knee brace reduce the incidence of knee rotational instability? Arch. Orthop. Trauma Surg. 2024, 144, 1161–1169. [Google Scholar] [CrossRef]
- Focke, A.; Steingrebe, H.; Möhler, F.; Ringhof, S.; Sell, S.; Potthast, W.; Stein, T. Effect of Different Knee Braces in ACL-Deficient Patients. Front. Bioeng. Biotechnol. 2020, 8, 964. [Google Scholar] [CrossRef]
- Yang, X.-G.; Feng, J.-T.; He, X.; Wang, F.; Hu, Y.-C. The effect of knee bracing on the knee function and stability following anterior cruciate ligament reconstruction: A systematic review and meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2019, 105, 1107–1114. [Google Scholar] [CrossRef] [PubMed]
- Théoret, D.; Lamontagne, M. Study on three-dimensional kinematics and electromyography of ACL deficient knee participants wearing a functional knee brace during running. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 555–563. [Google Scholar] [CrossRef]
- Butler, R.J.; Dai, B.; Garrett, W.E.; Queen, R.M. Changes in landing mechanics in patients following anterior cruciate ligament reconstruction when wearing an extension constraint knee brace. Sports Health 2014, 6, 203–209. [Google Scholar] [CrossRef]
- Dickerson, L.C.; Peebles, A.T.; Moskal, J.T.; Miller, T.K.; Queen, R.M. Physical Performance Improves With Time and a Functional Knee Brace in Athletes After ACL Reconstruction. Orthop. J. Sports Med. 2020, 8, 2325967120944255. [Google Scholar] [CrossRef]
- Strutzenberger, G.; Braig, M.; Sell, S.; Boes, K.; Schwameder, H. Effect of brace design on patients with ACL-ruptures. Int. J. Sports Med. 2012, 33, 934–939. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M.A.; Deliso, M.; Hong, I.S.; Saltzman, B.M.; Longobardi, R.S.; DeLuca, P.F.; Rizio, L. Rehabilitation and Return to Play Protocols After Anterior Cruciate Ligament Reconstruction in Soccer Players: A Systematic Review. Am. J. Sports Med. 2025, 53, 217–227. [Google Scholar] [CrossRef]
- Haddara, R.; Harandi, V.J.; Lee, P.V.S. Effect of Prophylactic Knee Bracing on Anterior Cruciate Ligament Agonist and Antagonist Muscle Forces During Perturbed Walking. Orthop. J. Sports Med. 2021, 9, 2325967120981641. [Google Scholar] [CrossRef]
- Liggett, C.L.; Tandy, R.D.; Young, J.C. The effects of prophylactic knee bracing on running gait. J. Athl. Train. 1995, 30, 159–161. [Google Scholar] [PubMed]
- Vickery-Howe, D.M.; Bonanno, D.R.; Dascombe, B.J.; Drain, J.R.; Clarke, A.C.; Hoolihan, B.; Willy, R.W.; Middleton, K.J. Physiological, perceptual, and biomechanical differences between treadmill and overground walking in healthy adults: A systematic review and meta-analysis. J. Sports Sci. 2023, 41, 2088–2120. [Google Scholar] [CrossRef]
- Semaan, M.B.; Wallard, L.; Ruiz, V.; Gillet, C.; Leteneur, S.; Simoneau-Buessinger, E. Is treadmill walking biomechanically comparable to overground walking? A systematic review. Gait Posture 2022, 92, 249–257. [Google Scholar] [CrossRef]
- Lee, S.J.; Hidler, J. Biomechanics of overground vs. treadmill walking in healthy individuals. J. Appl. Physiol. 2008, 104, 747–755. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.; Kiesewetter, P.; Milani, T.L.; Mitschke, C. An Investigation of Running Kinematics with Recovered Anterior Cruciate Ligament Reconstruction on a Treadmill and In-Field Using Inertial Measurement Units: A Preliminary Study. Bioengineering 2024, 11, 404. [Google Scholar] [CrossRef] [PubMed]
- Stirling, L.M.; von Tscharner, V.; Fletcher, J.R.; Nigg, B.M. Quantification of the manifestations of fatigue during treadmill running. Eur. J. Sport Sci. 2012, 12, 418–424. [Google Scholar] [CrossRef]
- Nagai, K.; Nakanishi, Y.; Kamada, K.; Hoshino, Y.; Kuroda, R. Anatomy and Biomechanics of the Collateral Ligaments of the Knee. In Orthopaedic Biomechanics in Sports Medicine; Koh, J., Zaffagnini, S., Kuroda, R., Longo, U.G., Amirouche, F., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 311–320. ISBN 978-3-030-81549-3. [Google Scholar]
- Hassebrock, J.D.; Gulbrandsen, M.T.; Asprey, W.L.; Makovicka, J.L.; Chhabra, A. Knee Ligament Anatomy and Biomechanics. Sports Med. Arthrosc. Rev. 2020, 28, 80–86. [Google Scholar] [CrossRef]
- Woo, S.L.; Debski, R.E.; Withrow, J.D.; Janaushek, M.A. Biomechanics of knee ligaments. Am. J. Sports Med. 1999, 27, 533–543. [Google Scholar] [CrossRef]
- Dashti Rostami, K.; Alizadeh, M.H.; Minoonejad, H.; Yazdi, H.; Thomas, A. Effect of Fatigue on Electromyographic Activity Patterns of the Knee Joint Muscles in Anterior Cruciate Ligament Reconstructed and Deficient Patients during Landing Task. J. Funct. Morphol. Kinesiol. 2018, 3, 22. [Google Scholar] [CrossRef]
- Pietrosimone, B.; Blackburn, J.T.; Harkey, M.S.; Luc, B.A.; Pamukoff, D.N.; Hart, J.M. Clinical Strategies for Addressing Muscle Weakness Following Knee Injury. Sports Rehabil. 2015, 34, 285–300. [Google Scholar] [CrossRef]
- Thomas, A.C.; Villwock, M.; Wojtys, E.M.; Palmieri-Smith, R.M. Lower extremity muscle strength after anterior cruciate ligament injury and reconstruction. J. Athl. Train. 2013, 48, 610–620. [Google Scholar] [CrossRef]
- Hanzlíková, I.; Richards, J.; Hébert-Losier, K.; Smékal, D. The effect of proprioceptive knee bracing on knee stability after anterior cruciate ligament reconstruction. Gait Posture 2019, 67, 242–247. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Good, L.; Risberg, M.A. The Effect of Bracing on Proprioception of Knees with Anterior Cruciate Ligament Injury. J. Orthop. Sports Phys. Ther. 2002, 32, 11–15. [Google Scholar] [CrossRef]
- Jerosch, J.; Prymka, M. Proprioception and joint stability. Knee Surg. Sports Traumatol. Arthrosc. 1996, 4, 171–179. [Google Scholar] [CrossRef]
- Pearson, K.G. Proprioceptive regulation of locomotion. Curr. Opin. Neurobiol. 1995, 5, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Drigny, J.; Rolland, M.; Remilly, M.; Guermont, H.; Reboursière, E.; Hulet, C.; Gauthier, A. Knee proprioception four months after anterior cruciate ligament reconstruction: Impact of limb dominance, anterolateral procedure, and association with readiness to return to sport. Phys. Ther. Sport 2025, 71, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, M.S.; Bali, K.; Prabhakar, S. Proprioception in anterior cruciate ligament deficient knees and its relevance in anterior cruciate ligament reconstruction. Indian J. Orthop. 2011, 45, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Norinasab, S.; Jafarnezhadgero, A.; Siahkouhian, M.; Valizadehorang, A. The Effect of Using Brace in Three Different Knee Flexion Angles on Frequency of Muscular Activity During Running in People With Genu Varus. Sarem J. Reprod. Med. 2022, 10, 1168–1181. [Google Scholar] [CrossRef]
- Huang, T.; Ruan, M.; Huang, S.; Fan, L.; Wu, X. Comparison of kinematics and joint moments calculations for lower limbs during gait using markerless and marker-based motion capture. Front. Bioeng. Biotechnol. 2024, 12, 1280363. [Google Scholar] [CrossRef]
- Camomilla, V.; Cereatti, A.; Cutti, A.G.; Fantozzi, S.; Stagni, R.; Vannozzi, G. Methodological factors affecting joint moments estimation in clinical gait analysis: A systematic review. Biomed. Eng. Online 2017, 16, 106. [Google Scholar] [CrossRef]
- Cleather, D.J.; Bull, A.M.J. Influence of inverse dynamics methods on the calculation of inter-segmental moments in vertical jumping and weightlifting. Biomed. Eng. Online 2010, 9, 74. [Google Scholar] [CrossRef]
| Age [years] | Height [cm] | Weight [kg] | Gender [Male/Female] | Physical Activity [Hours per Week] | Side of Injured Leg [Left/Right] | Time Since Injury [years] | Therapeutic Intervention [Conservative/Surgical] |
|---|---|---|---|---|---|---|---|
| 33.5 ± 9.6 | 178.5 ± 9.7 | 74.4 ± 12.8 | 31/19 | 6.4 ± 4.0 | 28/22 | 6.1 ± 3.7 | 27/23 |
| Types of Injuries of the Knee Joint | n (% of n) | ||||||
| Ligament Injuries: e.g., partial or complete tear of anterior and/or posterior cruciate ligaments, medial and/or lateral collateral ligaments | 16 (32) | ||||||
| Meniscus Injuries: e.g., contusion or tear of the medial and/or lateral meniscus | 16 (32) | ||||||
| Cartilage Damage: e.g., Patellofemoral and/or femoral-tibial cartilage damage or osteoarthritis (level 1) | 13 (26) | ||||||
| Fractures and bone injuries: e.g., fractures of the patella or femur condyles | 5 (10) | ||||||
| Inflammations and others: e.g., nonspecific load pain, tendinopathy, plica syndrome, edema | 13 (26) | ||||||
| Parameter | Before Fatigue Protocol | After Fatigue Protocol | p-Value | d | |
|---|---|---|---|---|---|
| Fatigue Protocol | Fatigue (6–20) | 7.2 ± 1.6 a | 12.0 ± 2.7 a | a < 0.001 | a = 0.73 |
| Maximal Jumping Height [cm] | 35.2 ± 7.9 a | 33.4 ± 7.9 a | a < 0.001 | a = 0.23 |
| Parameter | Injured Leg | Injured Leg with Knee Brace | p-Value | d | |
|---|---|---|---|---|---|
| Running | Pain (0–10) | 2.1 ± 1.4 a | 1.9 ± 1.3 a | a = 0.004 | a = 0.15 |
| Stability (0–10) | 2.0 ± 1.4 | 1.8 ± 1.3 | 0.125 | - | |
| Jumping | Pain (0–10) | 2.2 ± 1.4 | 2.2 ± 1.4 | 1.000 | - |
| Stability (0–10) | 2.0 ± 1.4 a | 1.9 ± 1.3 a | 0.070 | - |
| Parameter | Healthy Leg | Injured Leg | Injured Leg with Knee Brace | p-Value | d |
|---|---|---|---|---|---|
| Maximal Knee Flexion Angle [°] | 43.7 ± 6.5 | 42.1 ± 6.4 | 43.6 ± 6.0 | 0.107 | - |
| Maximal Vertical Ground Reaction Force [Body Weight] | 2.43 ± 0.37 | 2.38 ± 0.34 | 2.43 ± 0.36 | 0.232 | - |
| Ground Contact Time [ms] | 258.2 ± 32.2 a | 257.1 ± 33.1 b | 253.8 ± 34.0 a; b | 0.023 | |
| a = 0.038 | a = 0.13 | ||||
| b = 0.015 | b = 0.10 |
| Parameter | Healthy Leg | Injured Leg | Injured Leg with Knee Brace | p-Value | d |
|---|---|---|---|---|---|
| Maximal Knee Flexion Angle [°] | 77.1 ± 23.2 a | 74.4 ± 22.2 a; b | 79.2 ± 22.9 b | a = 0.015 b < 0.001 | a = 0.12 b = 0.21 |
| Maximal Vertical Ground Reaction Force [Body Weight] | 2.17 ± 0.87 | 2.04 ± 0.77 | 2.03 ± 0.85 | 0.162 | - |
| Maximal Jumping Height [cm] | - | 33.7 ± 6.8 a | 33.2 ± 6.8 a | a = 0.007 | a = 0.07 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heß, T.; Milani, T.L.; Stoll, J.; Mitschke, C. Running and Jumping After Muscle Fatigue in Subjects with a History of Knee Injury: What Are the Acute Effects of Wearing a Knee Brace on Biomechanics? Bioengineering 2025, 12, 661. https://doi.org/10.3390/bioengineering12060661
Heß T, Milani TL, Stoll J, Mitschke C. Running and Jumping After Muscle Fatigue in Subjects with a History of Knee Injury: What Are the Acute Effects of Wearing a Knee Brace on Biomechanics? Bioengineering. 2025; 12(6):661. https://doi.org/10.3390/bioengineering12060661
Chicago/Turabian StyleHeß, Tobias, Thomas L. Milani, Jan Stoll, and Christian Mitschke. 2025. "Running and Jumping After Muscle Fatigue in Subjects with a History of Knee Injury: What Are the Acute Effects of Wearing a Knee Brace on Biomechanics?" Bioengineering 12, no. 6: 661. https://doi.org/10.3390/bioengineering12060661
APA StyleHeß, T., Milani, T. L., Stoll, J., & Mitschke, C. (2025). Running and Jumping After Muscle Fatigue in Subjects with a History of Knee Injury: What Are the Acute Effects of Wearing a Knee Brace on Biomechanics? Bioengineering, 12(6), 661. https://doi.org/10.3390/bioengineering12060661






