Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review
Abstract
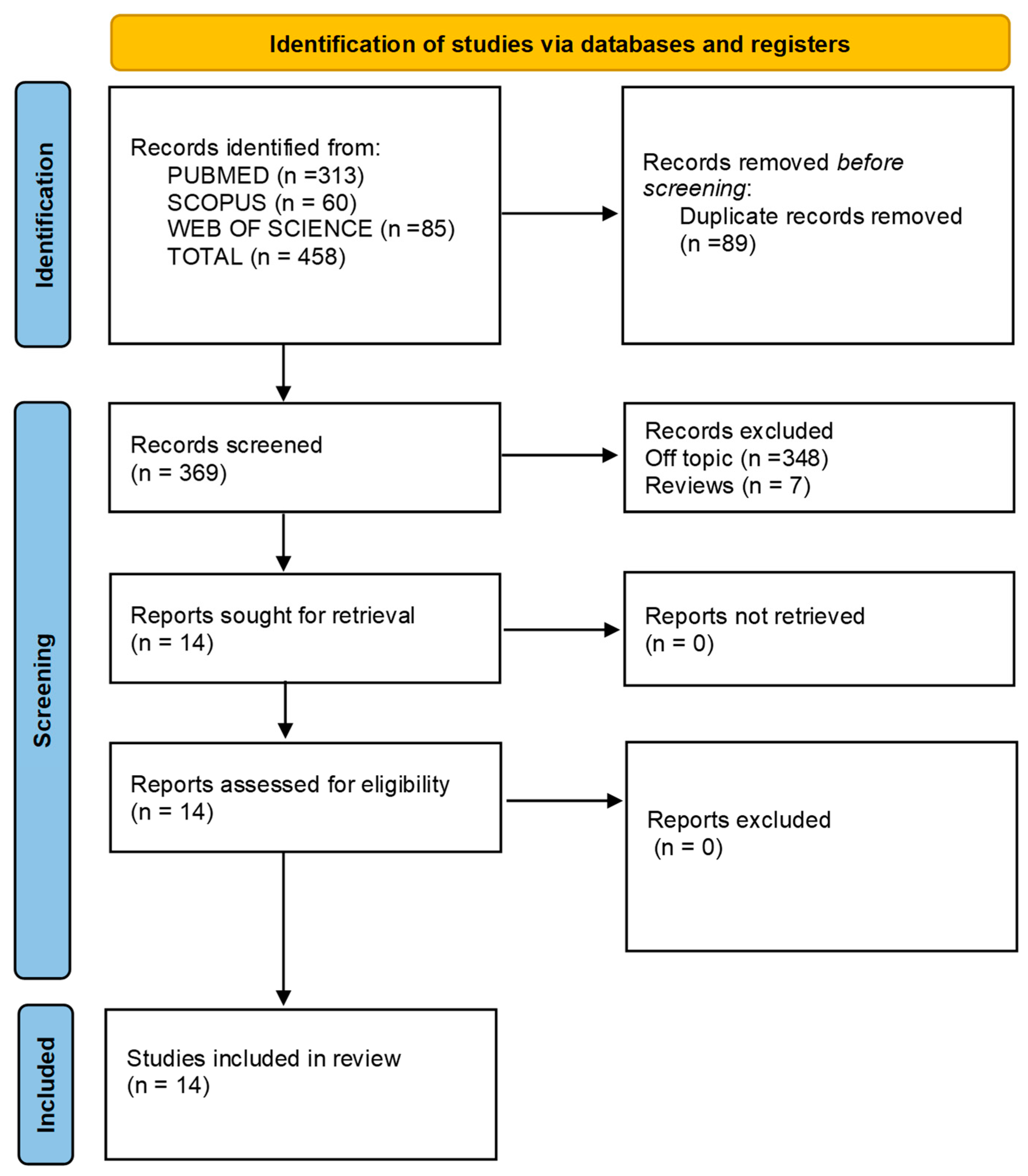
1. Introduction
1.1. Evolution of Orthodontic Treatment
1.2. Emergence and Workflow of Clear Aligners
1.3. Limitations of Aligners and the Role of TADs
1.4. Historical Background and Advances in TADs
1.5. Biomechanical Benefits of TADs
1.6. Clinical Use and Indications
1.7. Combined Use of Aligners and TADs
1.8. Recent Advances in Antimicrobial Coatings for Orthodontic Appliances
1.9. Comparison with Previous Systematic Reviews
1.10. Aim of the Review
2. Materials and Methods
2.1. Protocol and Registration
2.2. Search Processing
2.3. Inclusion Criteria
- (1)
- Studies involving patients undergoing orthodontic treatment with both clear aligners and Temporary Anchorage Devices (TADs);
- (2)
- Studies that specifically addressed malocclusions requiring complex tooth movements, such as Class II, Class III, anterior open bite, deep bite, and molar distalization;
- (3)
- Studies involving human participants aged 12 years and above, including adolescents and adults, with no craniofacial syndromes or systemic diseases;
- (4)
- Randomized clinical trials, retrospective studies, case series, and case reports;
- (5)
- Full-text articles published in English.
- Participants: Male and female patients aged ≥12 years, requiring orthodontic treatment with no syndromic or systemic pathology.
- Intervention: Orthodontic therapy combining clear aligners and TADs.
- Comparison: Treatment outcomes before and after intervention.
- Outcome: Evaluating the efficacy of clear aligners with TADs in treating complex malocclusions.
- Study Design: RCTs, retrospective studies, case series, and case reports.
| Category | Criteria |
|---|---|
| Inclusion |
|
| Exclusion |
|
2.4. Exclusion Criteria
2.5. Data Processing
2.6. Quality Assessment
- -
- Bias due to confounding;
- -
- Bias arising from the measurement of the exposure;
- -
- Bias in the selection of participants in the study;
- -
- Bias due to post-exposure intervention;
- -
- Bias due to missing data;
- -
- Bias arising from the measurement of the outcome;
- -
- Bias in the selection of the reported results.
3. Results
3.1. Study Selection and Characteristics
3.2. Quality Assessment and Risk of Bias of Included Articles
4. Discussion
4.1. Integration of TADs in Clear Aligner Therapy
4.2. Applications in Class III Malocclusions and Molar Distalization
4.3. Digital Orthodontics and Canine Impaction
4.4. Addressing Alveolar Protrusion and Vertical Control
4.5. Treatment of Anterior Open Bites
4.6. Surgical Approaches in Advanced Cases
4.7. Long-Term Stability in Hyperdivergent Cases
4.8. Forces and Limitations of TSADs
4.9. Molar Distalization and Asymmetries
4.10. Non-Extraction Approaches in Class II Malocclusions
4.11. Critical Analysis and Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| TADs | temporary anchorage devices |
References
- Kuo, E.; Miller, R.J. Automated Custom-Manufacturing Technology in Orthodontics. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 578–581. [Google Scholar] [CrossRef]
- Cardoso, P.C.; Espinosa, D.G.; Mecenas, P.; Flores-Mir, C.; Normando, D. Pain Level between Clear Aligners and Fixed Appliances: A Systematic Review. Prog. Orthod. 2020, 21, 3. [Google Scholar] [CrossRef] [PubMed]
- Weir, T. Clear Aligners in Orthodontic Treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Ke, Y.; Zhu, Y.; Zhu, M. A Comparison of Treatment Effectiveness between Clear Aligner and Fixed Appliance Therapies. BMC Oral Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Rinchuse, D.J.; Cozzani, M. Effectiveness and Efficiency in Clinical Orthodontic Practice. Int. Orthod. 2015, 13, 507–524. [Google Scholar] [CrossRef]
- Mangano, A.; Beretta, M.; Luongo, G.; Mangano, C.; Mangano, F. Conventional Vs Digital Impressions: Acceptability, Treatment Comfort and Stress Among Young Orthodontic Patients. Open Dent. J. 2018, 12, 118–124. [Google Scholar] [CrossRef]
- Lecocq, G. Digital Impression-Taking: Fundamentals and Benefits in Orthodontics. Int. Orthod. 2016, 14, 184–194. [Google Scholar] [CrossRef]
- Bai, Y.X. Application of three-dimensional digital technology in the diagnosis and treatment planning in orthodontics. Zhonghua Kouqiang Yixue Zazhi Chin. J. Stomatol. 2016, 51, 326–330. [Google Scholar] [CrossRef]
- Djeu, G.; Shelton, C.; Maganzini, A. Outcome Assessment of Invisalign and Traditional Orthodontic Treatment Compared with the American Board of Orthodontics Objective Grading System. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 292–298. [Google Scholar] [CrossRef]
- Christopoulou, I.; Kaklamanos, E.G.; Makrygiannakis, M.A.; Bitsanis, I.; Tsolakis, A.I. Patient-Reported Experiences and Preferences with Intraoral Scanners: A Systematic Review. Eur. J. Orthod. 2022, 44, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Boyd, R.L. Esthetic Orthodontic Treatment Using the Invisalign Appliance for Moderate to Complex Malocclusions. J. Dent. Educ. 2008, 72, 948–967. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How Well Does Invisalign Work? A Prospective Clinical Study Evaluating the Efficacy of Tooth Movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Kirschneck, C.; Kamuf, B.; Putsch, C.; Chhatwani, S.; Bizhang, M.; Danesh, G. Conformity, Reliability and Validity of Digital Dental Models Created by Clinical Intraoral Scanning and Extraoral Plaster Model Digitization Workflows. Comput. Biol. Med. 2018, 100, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Burhardt, L.; Livas, C.; Kerdijk, W.; Van Der Meer, W.J.; Ren, Y. Treatment Comfort, Time Perception, and Preference for Conventional and Digital Impression Techniques: A Comparative Study in Young Patients. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 261–267. [Google Scholar] [CrossRef]
- Papadimitriou, A.; Mousoulea, S.; Gkantidis, N.; Kloukos, D. Clinical Effectiveness of Invisalign® Orthodontic Treatment: A Systematic Review. Prog. Orthod. 2018, 19, 37. [Google Scholar] [CrossRef]
- Lin, E.; Julien, K.; Kesterke, M.; Buschang, P.H. Differences in Finished Case Quality between Invisalign and Traditional Fixed Appliances. Angle Orthod. 2022, 92, 173–179. [Google Scholar] [CrossRef]
- Kau, C.H.; Soh, J.; Christou, T.; Mangal, A. Orthodontic Aligners: Current Perspectives for the Modern Orthodontic Office. Med. Kaunas Lith. 2023, 59, 1773. [Google Scholar] [CrossRef]
- Liao, T.-H.; Fang, J.C.-C.; Wang, I.-K.; Huang, C.-S.; Chen, H.-L.; Yen, T.-H. Characteristics and Dental Indices of Orthodontic Patients Using Aligners or Brackets. Int. J. Environ. Res. Public Health 2022, 19, 6569. [Google Scholar] [CrossRef]
- Christou, T.; Abarca, R.; Christou, V.; Kau, C.H. Smile Outcome Comparison of Invisalign and Traditional Fixed-Appliance Treatment: A Case-Control Study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 357–364. [Google Scholar] [CrossRef]
- Antoszewska, J.; Papadopoulos, M.A.; Park, H.-S.; Ludwig, B. Editor’s Summary and Q&A. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 158–159. [Google Scholar] [CrossRef]
- Gandedkar, N.H.; Koo, C.S.; Sharan, J.; Chng, C.K.; Vaid, N. The Temporary Anchorage Devices Research Terrain: Current Perspectives and Future Forecasts! Semin. Orthod. 2018, 24, 191–206. [Google Scholar] [CrossRef]
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.-M.; Takano-Yamamoto, T. Clinical Use of Miniscrew Implants as Orthodontic Anchorage: Success Rates and Postoperative Discomfort. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef]
- Sherwood, K.H.; Burch, J.G.; Thompson, W.J. Closing Anterior Open Bites by Intruding Molars with Titanium Miniplate Anchorage. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2002, 122, 593–600. [Google Scholar] [CrossRef] [PubMed]
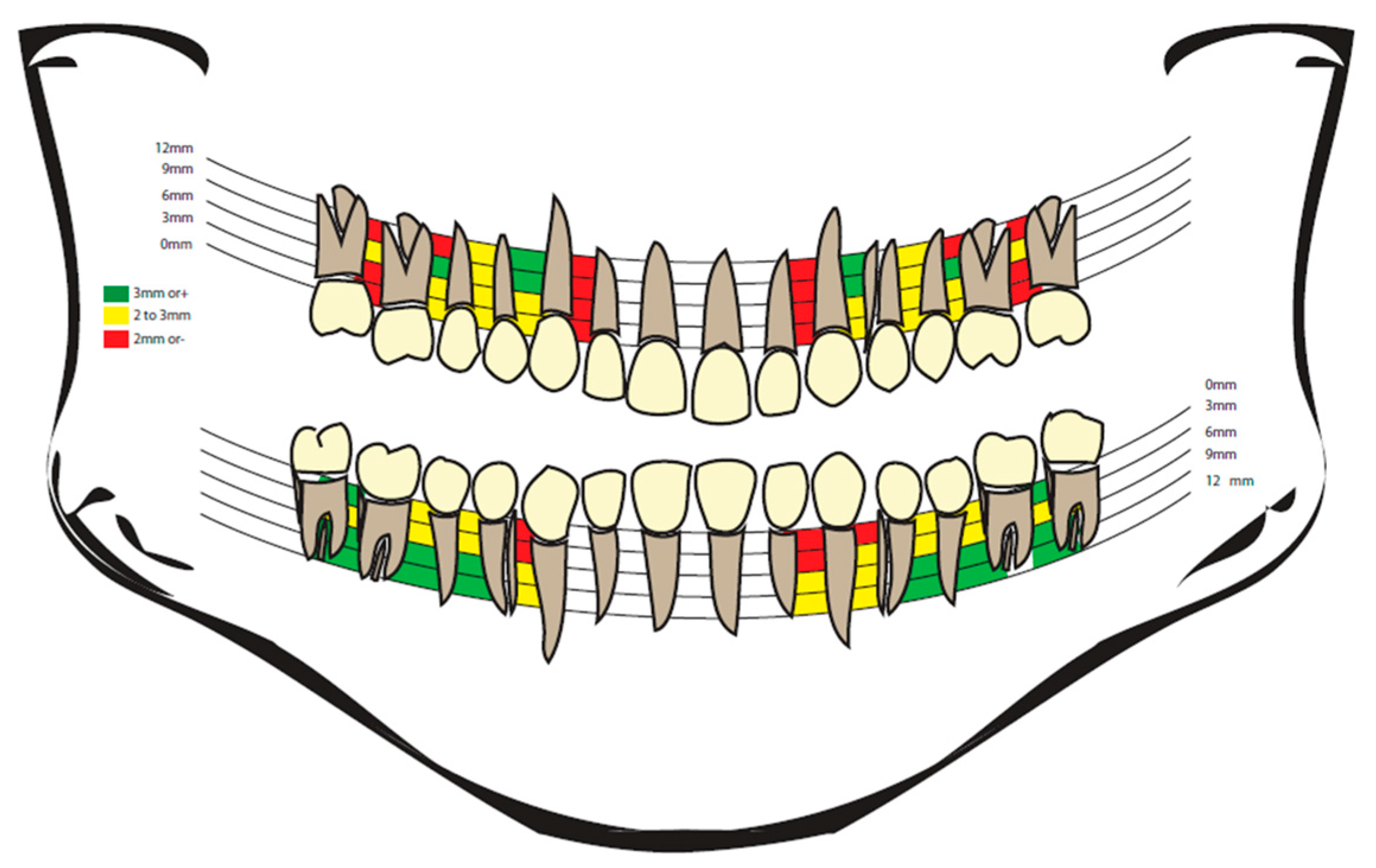
- Lima, A.; Domingos, R.G.; Cunha Ribeiro, A.N.; Rino Neto, J.; De Paiva, J.B. Safe Sites for Orthodontic Miniscrew Insertion in the Infrazygomatic Crest Area in Different Facial Types: A Tomographic Study. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 37–45. [Google Scholar] [CrossRef]
- Park, J.; Boyd, R.L. TADs and Invisalign: Making Difficult Movement Possible. In Temporary Anchorage Devices in Clinical Orthodontics; Park, J.H., Ed.; Wiley: Hoboken, NJ, USA, 2020; pp. 541–554. ISBN 978-1-119-51347-6. [Google Scholar]
- Van Den Braak, M.C.T.; Hoekstra, J.W.M.; Bronkhorst, E.M.; Schols, J.G.J.H.; Ongkosuwito, E.M.; Meijer, G.J.; Van Den Beucken, J.J.J.P. The Effect of Surface Roughening on the Success of Orthodontic Mini-Implants: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofacial Orthop. 2024, 165, 262–271. [Google Scholar] [CrossRef]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of Anatomical Sites and Correlated Risk Factors on the Survival of Orthodontic Miniscrew Implants: A Systematic Review and Meta-Analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef]
- Rodriguez, J.C.; Suarez, F.; Chan, H.-L.; Padial-Molina, M.; Wang, H.-L. Implants for Orthodontic Anchorage: Success Rates and Reasons of Failures. Implant Dent. 2014, 23, 155–161. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Kuang, S.-H.; Wu, C.-H. Factors Associated with the Stability of Mini-Implants for Orthodontic Anchorage: A Study of 414 Samples in Taiwan. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2009, 67, 1595–1599. [Google Scholar] [CrossRef]
- Miyawaki, S.; Koyama, I.; Inoue, M.; Mishima, K.; Sugahara, T.; Takano-Yamamoto, T. Factors Associated with the Stability of Titanium Screws Placed in the Posterior Region for Orthodontic Anchorage. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2003, 124, 373–378. [Google Scholar] [CrossRef]
- Shinohara, A.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Root Proximity and Inclination of Orthodontic Mini-Implants after Placement: Cone-Beam Computed Tomography Evaluation. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2013, 144, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Drescher, D. A Miniscrew System with Interchangeable Abutments. J. Clin. Orthod. JCO 2008, 42, 574–580. [Google Scholar] [PubMed]
- Uzunçıbuk, H.; Marrapodi, M.M.; Meto, A.; Ronsivalle, V.; Cicciù, M.; Minervini, G. Prevalence of Temporomandibular Disorders in Clear Aligner Patients Using Orthodontic Intermaxillary Elastics Assessed with Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Axis II Evaluation: A Cross-Sectional Study. J. Oral Rehabil. 2024, 51, 500–509. [Google Scholar] [CrossRef]
- Buschang, P.H.; Carrillo, R.; Rossouw, P.E. Orthopedic Correction of Growing Hyperdivergent, Retrognathic Patients with Miniscrew Implants. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2011, 69, 754–762. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M.A. Failure Rates and Associated Risk Factors of Orthodontic Miniscrew Implants: A Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2012, 142, 577–595.e7. [Google Scholar] [CrossRef]
- Jandial, M.; Mahajan, S.; Singh, G. Temporary Anchorage Devices in Orthodontics. Int. J. Health Sci. 2021, 5 (Suppl. S2), 333–343. [Google Scholar] [CrossRef]
- Goh, S.; Dreyer, C.; Weir, T. The Predictability of the Mandibular Curve of Spee Leveling with the Invisalign Appliance. Am. J. Orthod. Dentofacial Orthop. 2022, 162, 193–200. [Google Scholar] [CrossRef]
- Ojima, K.; Sugawara, J.; Nanda, R. Anchorage of TADs Using Aligner Orthodontics Treatment for Lower Molars Distalization. In Temporary Anchorage Devices in Orthodontics; Elsevier: Amsterdam, The Netherlands, 2020; pp. 305–319. ISBN 978-0-323-60933-3. [Google Scholar]
- Kravitz, N.D.; Kusnoto, B.; Agran, B.; Viana, G. Influence of Attachments and Interproximal Reduction on the Accuracy of Canine Rotation with Invisalign. A Prospective Clinical Study. Angle Orthod. 2008, 78, 682–687. [Google Scholar] [CrossRef]
- Kuroda, S.; Katayama, A.; Takano-Yamamoto, T. Severe Anterior Open-Bite Case Treated Using Titanium Screw Anchorage. Angle Orthod. 2004, 74, 558–567. [Google Scholar] [CrossRef]
- Yudaev, P.A.; Chistyakov, E.M. Progress in Dental Materials: Application of Natural Ingredients. Russ. Chem. Rev. 2024, 93, RCR5108. [Google Scholar] [CrossRef]
- Antibiotics in Dentistry: A Narrative Review of the Evidence Beyond the Myth. Available online: https://colab.ws/articles/10.3390%2Fijerph20116025 (accessed on 1 May 2025).
- Dental Plaque Bacteria with Reduced Susceptibility to Chlorhexidine are Multidrug Resistant. Available online: https://colab.ws/articles/10.1186%2Fs12866-016-0833-1 (accessed on 1 May 2025).
- Blundell, H.L.; Weir, T.; Byrne, G. Predictability of Overbite Control with the Invisalign Appliance Comparing SmartTrack with Precision Bite Ramps to EX30. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e71–e81. [Google Scholar] [CrossRef] [PubMed]
- Nimeri, G.; Kau, C.H.; Abou-Kheir, N.S.; Corona, R. Acceleration of Tooth Movement during Orthodontic Treatment--a Frontier in Orthodontics. Prog. Orthod. 2013, 14, 42. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Park, H.S.; Kyung, H.M. Micro-Implant Anchorage for Lingual Treatment of a Skeletal Class II Malocclusion. J. Clin. Orthod. JCO 2001, 35, 643–647. [Google Scholar]
- Nakamura, M.; Kawanabe, N.; Kataoka, T.; Murakami, T.; Yamashiro, T.; Kamioka, H. Comparative Evaluation of Treatment Outcomes between Temporary Anchorage Devices and Class III Elastics in Class III Malocclusions. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2017, 151, 1116–1124. [Google Scholar] [CrossRef]
- Kinzinger, G.; Frye, L.; Diedrich, P. Class II Treatment in Adults: Comparing Camouflage Orthodontics, Dentofacial Orthopedics and Orthognathic Surgery—A Cephalometric Study to Evaluate Various Therapeutic Effects. J. Orofac. Orthop. Fortschritte Kieferorthopadie OrganOff. J. Dtsch. Ges. Kieferorthopadie 2009, 70, 63–91. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Greco, M.; Rossini, G.; Rombolà, A. G-Block: Posterior Anchorage Device Tads-Supported after Molar Distalization with Aligners: An Adult Case Report. Int. Orthod. 2022, 20, 100687. [Google Scholar] [CrossRef]
- Greco, M.; Machoy, M. Impacted Canine Management Using Aligners Supported by Orthodontic Temporary Anchorage Devices. Int. J. Environ. Res. Public Health 2022, 20, 131. [Google Scholar] [CrossRef]
- Lu, W.; Li, Y.; Mei, L.; Li, Y. Preformed Intrusion Bulbs on Clear Aligners Facilitate Active Vertical Control in a Hyperdivergent Skeletal Class II Case with Extraction: A Case Report with 4-Year Follow-Up. APOS Trends Orthod. 2023, 13, 46–54. [Google Scholar] [CrossRef]
- Capuozzo, R.; Caruso, S.; Caruso, S.; De Felice, M.E.; Gatto, R. Canine Impaction: Digital Orthodontic Planning in Conjunction with TADs (Temporary Anchorage Devices) and Aligners. Appl. Sci. 2023, 13, 6914. [Google Scholar] [CrossRef]
- Auladell, A.; De La Iglesia, F.; Quevedo, O.; Walter, A.; Puigdollers, A. The Efficiency of Molar Distalization Using Clear Aligners and Mini-Implants: Two Clinical Cases. Int. Orthod. 2022, 20, 100604. [Google Scholar] [CrossRef] [PubMed]
- Kottemann, W.J. The Use of TADs with Clear Aligners for Asymmetry Correction. In Temporary Anchorage Devices in Clinical Orthodontics; Park, J.H., Ed.; Wiley: Hoboken, NJ, USA, 2020; pp. 555–562. ISBN 978-1-119-51347-6. [Google Scholar]
- Lin, G.; Chen, M.; Guo, N.; Shi, X. Three-Dimensional Measurement and Analysis of Mandibular Molar Distalization Assisted by Micro-Implant Anchorage Combined with Clear Aligner. Pak. J. Med. Sci. 2024, 40, 7759. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Gao, J. Clear Aligner Treatment Assisted by Mini Screw for an Adult with Class II Division 2 Malocclusion and a Right Upper Canine Completely Outside of the Dental Arch: A Case Report. Int. Orthod. 2024, 22, 100837. [Google Scholar] [CrossRef]
- Choi, N.-C.; Park, Y.-C.; Jo, Y.-M.; Lee, K.-J. Combined Use of Miniscrews and Clear Appliances for the Treatment of Bialveolar Protrusion without Conventional Brackets. Am. J. Orthod. Dentofacial Orthop. 2009, 135, 671–681. [Google Scholar] [CrossRef]
- Sabouni, W.; Venugopal, A.; Adel, S.M.; Vaid, N. Correction of Anterior Open Bite of Varying Severity Using Clear Aligner Therapy—A Case Series. Clin. Case Rep. 2022, 10, e6277. [Google Scholar] [CrossRef]
- Iodice, G.; Tartaro, G.; Santagata, M.; D’Amato, S. Full Digital Surgery-First, Skeletal Anchorage and Aligners Approach to Correct a Gummy Smile and Class II Malocclusion with Mandibular Retrusion and Deviation. Appl. Sci. 2021, 11, 9985. [Google Scholar] [CrossRef]
- De Almeida, M.R. The Biomechanics of Clear Aligners Associated with Temporary Skeletal Anchorage Devices (TSADs). Semin. Orthod. 2024, 30, 514–526. [Google Scholar] [CrossRef]
- Zhang, W.; Yang, H. Orthognathic Surgery in Invisalign Patients. J. Craniofac. Surg. 2022, 33, e112–e113. [Google Scholar] [CrossRef]
- Tseng, L.L.Y.; Chang, C.H.; Roberts, W.E. Diagnosis and Conservative Treatment of Skeletal Class III Malocclusion with Anterior Crossbite and Asymmetric Maxillary Crowding. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2016, 149, 555–566. [Google Scholar] [CrossRef]
- Ma, X.-Q.; Xiang, F.; Fan, M.-Y.; Song, Y.; Wang, X.-H.; Zhang, L.; Qian, W.-H. Clinical efficacy of the combination of miniscrew with clear aligner in controlling the roller coaster effect. Shanghai Kou Qiang Yi Xue Shanghai J. Stomatol. 2022, 31, 193–197. [Google Scholar]
- Roberts, W.E.; Chang, C.H.; Chen, J.; Brezniak, N.; Yadav, S. Integrating Skeletal Anchorage into Fixed and Aligner Biomechanics. J. World Fed. Orthod. 2022, 11, 95–106. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhan, Q.; Zhou, J.; Kuang, Q.; Yan, X.; Zhang, X.; Shan, Y.; Li, X.; Lai, W.; Long, H. Effectiveness of an Anterior Mini-Screw in Achieving Incisor Intrusion and Palatal Root Torque for Anterior Retraction with Clear Aligners. Angle Orthod. 2021, 91, 794–803. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Lam, X.Y.; Zhang, L.; Li, W.; Lin, Y. Biomechanical Analysis of Miniscrew-Assisted Molar Distalization with Clear Aligners: A Three-Dimensional Finite Element Study. Eur. J. Orthod. 2024, 46, cjad077. [Google Scholar] [CrossRef]
- Withayanukonkij, W.; Chanmanee, P.; Promsawat, M.; Viteporn, S.; Leethanakul, C. Root Resorption during Maxillary Molar Intrusion with Clear Aligners: A Randomized Controlled Trial. Angle Orthod. 2023, 93, 629–637. [Google Scholar] [CrossRef]
- Gou, Y.; Ungvijanpunya, N.; Chen, L.; Zeng, Y.; Ye, H.; Cao, L. Clear Aligner vs Fixed Self-Ligating Appliances: Orthodontic Emergency during the 2020 Coronavirus Disease 2019 Pandemic. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2022, 161, e400–e406. [Google Scholar] [CrossRef]
- Celenza, F. Implant Interactions with Orthodontics. J. Evid.-Based Dent. Pract. 2012, 12, 192–201. [Google Scholar] [CrossRef]
- Arveda, N.; Colonna, A.; Siciliani, G.; Lombardo, L. Class III Correction Using Clear Aligners, Sectional Wires, and Miniscrew Anchorage. J. Clin. Orthod. JCO 2023, 57, 54–62. [Google Scholar]
- Wang, Y.; Zhou, S.; Zheng, J.; Yan, L.; Ngan, P.; Hua, F.; He, H. Comparison of Treatment Effects between Clear Aligners and Fixed Appliances in Patients Treated with Miniscrew-Assisted Molar Distalization. Eur. J. Orthod. 2024, 46, cjae021. [Google Scholar] [CrossRef]
- Arveda, N.; Colonna, A.; Palone, M.; Lombardo, L. Aligner Hybrid Orthodontic Approach to Treat Severe Transverse Divergence in an Adolescent Girl: A Case Report. Int. Orthod. 2022, 20, 100686. [Google Scholar] [CrossRef]
- Katyal, S.; Kharbanda, O.P.; Duggal, R.; Samrit, V.D. A Quantitative Analysis of Macrophage-Colony-Stimulating Factor in Peri-Miniscrew Implant Crevicular Fluid before and after Orthodontic Loading. Angle Orthod. 2022, 93, 222–227. [Google Scholar] [CrossRef]
- Pinho, T.; Rocha, D. Asymmetrical Skeletal Class III Camouflage Treatment with Clear Aligners and Miniscrew Anchorage. J. Clin. Orthod. 2021, 55, 757–768. [Google Scholar] [PubMed]
- Machawal, J.; Kharbanda, O.P.; Duggal, R.; Chauhan, S.S.; Samrit, V.D. Quantitative Evaluation of Pentraxin-3 in Peri-Miniscrew Implant Crevicular Fluid in Patients Undergoing Orthodontic Treatment: A Prospective Study. Cureus 2023, 15, e36060. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, O.; Mota-Júnior, S.L. MARPE as an Adjunct to Orthodontic Treatment. Dent. Press J. Orthod. 2023, 27, e22bbo6. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Li, J.; Lei, F.; Wang, X.; Zhou, Y. Dentoskeletal and Soft Tissue Changes Associated with Miniscrew Anchorage in Customized Lingual Orthodontics. J. Int. Med. Res. 2019, 47, 84–95. [Google Scholar] [CrossRef]
- de Almeida, M.R. Current Status of the Biomechanics of Extra-Alveolar Miniscrews. J. World Fed. Orthod. 2024, 13, 25–37. [Google Scholar] [CrossRef]
- Shahroudi, A.S.; Golmohammadi, S. Miniscrew-Assisted Single-Tooth Distraction Osteogenesis to Align an Ankylosed Infraoccluded Maxillary Central Incisor: A Case Report. J. Orthod. 2020, 47, 345–353. [Google Scholar] [CrossRef]
- Duran, G.S.; Görgülü, S.; Dindaroğlu, F. Three-Dimensional Analysis of Tooth Movements after Palatal Miniscrew-Supported Molar Distalization. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2016, 150, 188–197. [Google Scholar] [CrossRef]
- Pu, L.; Zhou, J.; Yan, X.; Zhou, H.; Liu, X.; Yang, Z.; Hua, C.; Zhang, L.; Lai, W.; Long, H. Orthodontic Traction of an Impacted Maxillary Third Molar through a Miniscrew-Anchored Cantilever Spring to Substitute the Adjacent Second Molar with Severe Root Resorption. J. Am. Dent. Assoc. 1939 2022, 153, 884–892. [Google Scholar] [CrossRef]
- Calil, R.C.; Marin Ramirez, C.M.; Otazu, A.; Torres, D.M.; de Araújo Gurgel, J.; Oliveira, R.C.; de Oliveira, R.C.G.; Valarelli, F.P.; Freitas, K.M.S. Maxillary Dental and Skeletal Effects after Treatment with Self-Ligating Appliance and Miniscrew-Assisted Rapid Maxillary Expansion. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2021, 159, e93–e101. [Google Scholar] [CrossRef]
- Agarwal, Y.; Goyal, M.; Kumar, M.; Kaur, A. Skeletal Open Bite Treated with Clear Aligners and Miniscrews. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2021, 160, 166–167. [Google Scholar] [CrossRef]
- Waxler, R. Correcting Skeletal Open Bite with Clear Aligners and Miniscrews. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2021, 160, 165. [Google Scholar] [CrossRef] [PubMed]
- Palone, M.; Pavan, F.; Carlucci, A.; Lombardo, L. Massive Intrusion of Maxillary Second Molar for Prosthodontic Purposes through Miniscrew-Supported Biomechanics and Fixed Partial Appliances: A Case Report. Int. Orthod. 2022, 20, 100662. [Google Scholar] [CrossRef] [PubMed]
- Fahem, M.M.; Das, R.K.; Luther, H.; Ali, A.H. Template Routed Patient-Specific Implant for 1-Stage Cranioplasty. Oper. Neurosurg. Hagerstown Md 2024, 27, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Bonnick, A.M.; Nalbandian, M.; Siewe, M.S. Technological Advances in Nontraditional Orthodontics. Dent. Clin. N. Am. 2011, 55, 571–584. [Google Scholar] [CrossRef]
- Wang, X.-D.; Lei, F.-F.; Liu, D.-W.; Zhang, J.-N.; Liu, W.-T.; Song, Y.; Zhou, Y.-H. Miniscrew-Assisted Customized Lingual Appliances for Predictable Treatment of Skeletal Class II Malocclusion with Severe Deep Overbite and Overjet. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2017, 152, 104–115. [Google Scholar] [CrossRef]
- Palone, M.; Baciliero, M.; Cervinara, F.; Maino, G.B.; Paoletto, E.; Cremonini, F.; Lombardo, L. Class II Treatment of Transverse Maxillary Deficiency with a Single Bone-Borne Appliance and Hybrid Clear Aligner Approach in an Adult Patient: A Case Report. J. World Fed. Orthod. 2022, 11, 80–94. [Google Scholar] [CrossRef]
- Zhang, C.; Ji, L.; Liao, W.; Zhao, Z. A Novel Biomechanical System to Intrude the Upper Incisors and Control Overbite: Posterior Miniscrew-Assisted Lever Arm and 2 Cases Report. Medicine 2022, 101, e31616. [Google Scholar] [CrossRef]
- Fan, Y.; Li, Y.; Fan, M.; Lin, Y.; Xu, J.; Li, Z.; Luo, J. Successful Treatment for an Adult with Bilateral Posterior Teeth Crossbite by Miniscrew-Assisted Rapid Palatal Expansion: A Case Report. Clin. Case Rep. 2024, 12, e9216. [Google Scholar] [CrossRef]
- Mousa, M.R.; Hajeer, M.Y.; Burhan, A.S.; Heshmeh, O. The Effectiveness of Conventional and Accelerated Methods of Orthodontic Traction and Alignment of Palatally Impacted Canines in Terms of Treatment Time, Velocity of Tooth Movement, Periodontal, and Patient-Reported Outcomes: A Systematic Review. Cureus 2022, 14, e24888. [Google Scholar] [CrossRef]
- Kaaouara, Y.; Sara, E.A.; Rerhrhaye, W. Perception of Mini-Screw Anchorage Devices by Patients. Int. Orthod. 2018, 16, 676–683. [Google Scholar] [CrossRef]
- Fan, Y.; Han, B.; Zhang, Y.; Guo, Y.; Li, W.; Chen, H.; Meng, C.; Penington, A.; Schneider, P.; Pei, Y.; et al. Natural Reference Structures for Three-Dimensional Maxillary Regional Superimposition in Growing Patients. BMC Oral Health 2023, 23, 655. [Google Scholar] [CrossRef] [PubMed]
- Pinho, T.; Santos, M. Skeletal Open Bite Treated with Clear Aligners and Miniscrews. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2021, 159, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Eğlenen, M.N.; Yavan, M.A. Has the COVID-19 Pandemic Affected Orthodontists’ Interest in Various Orthodontic Appliances? Turk. J. Orthod. 2023, 36, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Inchingolo, A.M.; Campanelli, M.; Carpentiere, V.; de Ruvo, E.; Ferrante, L.; Palermo, A.; Inchingolo, F.; Dipalma, G. Orthodontic Treatment in Patients with Atypical Swallowing and Malocclusion: A Systematic Review. J. Clin. Pediatr. Dent. 2024, 48, 14. [Google Scholar] [CrossRef]
- Cheng, X.Y.; Sang, T.; Wu, J. Cone-beam CT evaluation of the effect of indirect anchorage of mini-screw assisted clear aligner on molar distalization. Zhonghua Kou Qiang Yi Xue Za Zhi Zhonghua Kouqiang Yixue Zazhi Chin. J. Stomatol. 2022, 57, 724–732. [Google Scholar] [CrossRef]
- Chang, C.H.; Lin, L.Y.; Roberts, W.E. Orthodontic Bone Screws: A Quick Update and Its Promising Future. Orthod. Craniofac. Res. 2021, 24 (Suppl. S1), 75–82. [Google Scholar] [CrossRef]
- Balamurali, V.; Magesh, V.; Harikrishnan, P. Effect of Cortical Bone Thickness on Shear Stress and Force in Orthodontic Miniscrew-Bone Interface—A Finite Element Analysis. Biomed. Phys. Eng. Express 2024, 10, 055013. [Google Scholar] [CrossRef]
- Ghafari, J.G. Centennial Inventory: The Changing Face of Orthodontics. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2015, 148, 732–739. [Google Scholar] [CrossRef]
- Pickard, M.B.; Dechow, P.; Rossouw, P.E.; Buschang, P.H. Effects of Miniscrew Orientation on Implant Stability and Resistance to Failure. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2010, 137, 91–99. [Google Scholar] [CrossRef]
- Allanqawi, T.; Alkadhimi, A.; Fleming, P.S. Postgraduate Orthodontic Education: An International Perspective on Content and Satisfaction Levels. J. World Fed. Orthod. 2023, 12, 239–244. [Google Scholar] [CrossRef]
- Liaw, J.J.L.; Tai, S.K.; Huang, G. Torque Recovery of the Maxillary Incisors with a Modified Double J Retractor in a Class II Division 2 Case Treated with Clear Aligners. Angle Orthod. 2022, 93, 357–371. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, L.; Carlucci, A.; Maino, B.G.; Colonna, A.; Paoletto, E.; Siciliani, G. Class III Malocclusion and Bilateral Cross-Bite in an Adult Patient Treated with Miniscrew-Assisted Rapid Palatal Expander and Aligners. Angle Orthod. 2018, 88, 649–664. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-D.; Zhang, J.-N.; Liu, D.-W.; Lei, F.-F.; Liu, W.-T.; Song, Y.; Zhou, Y.-H. Nonsurgical Correction Using Miniscrew-Assisted Vertical Control of a Severe High Angle with Mandibular Retrusion and Gummy Smile in an Adult. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2017, 151, 978–988. [Google Scholar] [CrossRef] [PubMed]
- Pepe, F.; Mannelli, E.; Palone, M.; Lombardo, L.; Cremonini, F. Nonsurgical Treatment of an Adult Patient with Severe Transversal Skeletal Discrepancy: Tooth Bone-Borne Tandem Expander and Hybrid Aligner Approach. J. World Fed. Orthod. 2024, 13, 250–256. [Google Scholar] [CrossRef]
- Tripathi, T.; Kalra, S.; Rai, P.; Farazt, F.; Singh, N. True Intrusion of Maxillary First Molars with Zygomatic and Palatal Miniscrew Anchorage: A Case Report. Aust. Orthod. J. 2016, 32, 233–240. [Google Scholar] [CrossRef]
- Noroozian, M.; Merati, M.; Heravi, F.; Shafaee, H. Introducing a User-Friendly Technique for Treatment of Palatally-Impacted Canines with the Aid of Temporary Anchorage Devices. J. Dent. Shiraz Iran 2022, 23, 511–519. [Google Scholar] [CrossRef]
- Maeda, A.; Sakoguchi, Y.; Miyawaki, S. Patient with Oligodontia Treated with a Miniscrew for Unilateral Mesial Movement of the Maxillary Molars and Alignment of an Impacted Third Molar. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2013, 144, 430–440. [Google Scholar] [CrossRef]
- Pinho, T.; Rocha, D.; Gonçalves, S.; Martins, M.L. Clear Aligners and Miniscrews in a Scissor Bite Adult Treatment. Case Rep. Dent. 2024, 2024, 8841829. [Google Scholar] [CrossRef]
- Liaw, J.; Tai, S.; Huang, G. En-Masse Retraction of Maxillary Anterior Teeth with the Double J Retractor and Palatal Miniscrews: A Case Report. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2022, 161, 592–601. [Google Scholar] [CrossRef]
- Chen, G.; Teng, F.; Xu, T.-M. Distalization of the Maxillary and Mandibular Dentitions with Miniscrew Anchorage in a Patient with Moderate Class I Bimaxillary Dentoalveolar Protrusion. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2016, 149, 401–410. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Fatone, M.C.; Malcangi, G.; Avantario, P.; Piras, F.; Patano, A.; Di Pede, C.; Netti, A.; Ciocia, A.M.; De Ruvo, E.; et al. Modifiable Risk Factors of Non-Syndromic Orofacial Clefts: A Systematic Review. Children 2022, 9, 1846. [Google Scholar] [CrossRef] [PubMed]
- Tunçer, N.İ.; Özçırpıcı, A.A. Treatment of Class II, Division 2 Malocclusion with Miniscrew Supported En-Masse Retraction: Is Deepbite Really an Obstacle for Extraction Treatment? Turk. J. Orthod. 2017, 30, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, L.; Palone, M.; Maino, G.; Paoletto, E.; Carlucci, A.; Siciliani, G. Class II Subdivision with Skeletal Transverse Maxillary Deficit Treated by Single-Sitting Bone-Borne Appliance. Angle Orthod. 2021, 91, 129–137. [Google Scholar] [CrossRef]
- Kwak, K.-H.; Oh, S.; Choi, Y.-K.; Kim, S.-H.; Kim, S.-S.; Park, S.-B.; Kim, Y.-I. Effects of Different Distalization Directions and Methods on Maxillary Total Distalization with Clear Aligners: A Finite Element Study. Angle Orthod. 2023, 93, 348–356. [Google Scholar] [CrossRef]
- Markic, G.; Katsaros, C.; Pandis, N.; Eliades, T. Temporary Anchorage Device Usage: A Survey among Swiss Orthodontists. Prog. Orthod. 2014, 15, 29. [Google Scholar] [CrossRef]
- Wang, X.-D.; Zhang, J.-N.; Liu, D.-W.; Lei, F.-F.; Zhou, Y.-H. Nonsurgical Correction of a Severe Anterior Deep Overbite Accompanied by a Gummy Smile and Posterior Scissor Bite Using a Miniscrew-Assisted Straight-Wire Technique in an Adult High-Angle Case. Korean J. Orthod. 2016, 46, 253–265. [Google Scholar] [CrossRef]
- Hodecker, L.D.; Kühle, R.; Weichel, F.; Roser, C.J.; Lux, C.J.; Bauer, C.A.J. Concept for the Treatment of Class III Anomalies with a Skeletally Anchored Appliance Fabricated in the CAD/CAM Process-The MIRA Appliance. Bioengineering 2023, 10, 616. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Avantario, P.; Azzollini, D.; Buongiorno, S.; Viapiano, F.; Campanelli, M.; Ciocia, A.M.; De Leonardis, N.; et al. Effects of Resveratrol, Curcumin and Quercetin Supplementation on Bone Metabolism—A Systematic Review. Nutrients 2022, 14, 3519. [Google Scholar] [CrossRef]
- Abedini, S.; Elkenawy, I.; Kim, E.; Moon, W. Three-Dimensional Soft Tissue Analysis of the Face Following Micro-Implant-Supported Maxillary Skeletal Expansion. Prog. Orthod. 2018, 19, 46. [Google Scholar] [CrossRef]
- Ganzer, N.; Feldmann, I.; Bondemark, L. Anchorage Reinforcement with Miniscrews and Molar Blocks in Adolescents: A Randomized Controlled Trial. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board Orthod. 2018, 154, 758–767. [Google Scholar] [CrossRef]
- Abdelhady, N.A.; Tawfik, M.A.; Hammad, S.M. Maxillary Molar Distalization in Treatment of Angle Class II Malocclusion Growing Patients: Uncontrolled Clinical Trial. Int. Orthod. 2020, 18, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Kannan, S.; Fassul, S.; Singh, A.K.; Arora, N.; Malhotra, A.; Saini, N. Effectiveness and Importance of Powered Tooth Brushes in Tooth Movement. J. Fam. Med. Prim. Care 2019, 8, 2478–2483. [Google Scholar] [CrossRef]
- Beyling, F.; Klang, E.; Niehoff, E.; Schwestka-Polly, R.; Helms, H.-J.; Wiechmann, D. Class II Correction by Maxillary En Masse Distalization Using a Completely Customized Lingual Appliance and a Novel Mini-Screw Anchorage Concept—Preliminary Results. Head Face Med. 2021, 17, 23. [Google Scholar] [CrossRef]
- Lombardo, L.; Albertini, P.; Cervinara, F.; Brucculeri, L.; Siciliani, G. Early Class III Treatment with Hybrid Rapid Palatal Expander Combined with Facemask. Int. Orthod. 2020, 18, 624–635. [Google Scholar] [CrossRef]
- Chen, Y.; Kim, K.A.; Seo, K.W.; Kang, Y.-G.; Oh, S.-H.; Choi, Y.-S.; Kim, S.-H. A New Designed Expander Supported by Spike Miniscrews With Enhanced Stability. J. Craniofac. Surg. 2016, 27, e130–e133. [Google Scholar] [CrossRef]
- Özbilen, E.Ö.; Yılmaz, H.N.; Köse, K.N. Orthodontic Extrusion with Circumferential Supracrestal Fiberotomy: A Report of Two Cases. Turk. J. Orthod. 2018, 31, 145–149. [Google Scholar] [CrossRef]
- Chang, N.-Y.; Park, J.H.; Lee, M.-Y.; Cho, J.-W.; Cho, J.-H.; An, K.-Y.; Chae, J.-M. Orthodontic Treatment of Maxillary Incisors with Severe Root Resorption Caused by Bilateral Canine Impaction in a Class II Division 1 Patient. J. Clin. Pediatr. Dent. 2016, 40, 161–168. [Google Scholar] [CrossRef]

| Featur | Details |
|---|---|
| Material | Medical-grade titanium (Grade 5, Ti-6Al-4V) |
| Dimensions | Diameter: 1.2–2.0 mm; Length: 6–10 mm |
| Insertion Sites | Alveolar bone, palatal bone, infrazygomatic crest, interradicular areas |
| Insertion Technique | Manual or motor-driven, performed under local anesthesia |
| Placement Duration | Temporary (from a few months to completion of desired movement) |
| Clinical Indications | Intrusion, extrusion, molar distalization, correction of open/deep bites |
| Auxiliary Devices | Elastics, coil springs, direct attachments to aligners |
| Main Benefits | Stable anchorage, precise control of dental movements, biomechanical support |
| Potential Complications | Failure of integration, patient discomfort, mobility, localized infection |
| Database | Timespan | Keywords (Boolean Operators) |
|---|---|---|
| PubMed, Scopus, Web of Science | 1 January 2004–17 July 2024 | (aligners OR clear aligners OR transparent aligners OR Invisalign) AND (Temporary Anchorage Devices OR TADs OR OrthoTADs OR Mini-implants in orthodontics OR Skeletal anchorage OR Mini-screws OR Micro-implants orthodontics OR Orthodontic anchorage systems OR Miniscrew implants OR Temporary skeletal anchorage devices OR Orthodontic biomechanics with TADs) |
| Authors | Study Design | Number of Patients | Average Age/Gender | Treatment and Duration | Outcomes |
|---|---|---|---|---|---|
| Greco et al. (2022) [51] | Case report | 1 | 25 (F) | Posterior anchorage device TADs-supported after molar distalization with aligners with 15 months of treatment | Effective molar distalization and posterior anchorage using TADs and aligners |
| Greco et al. (2022) [52] | Case report | 1 | 16 (M); 43 (F) | Impacted canine management using aligners supported by orthodontic TADs; treatment performed with 43 and 38 aligners, respectively | Successful alignment of impacted canine with improved patient comfort and aesthetic appeal using TADs with aligners |
| Lu et al. (2023) [53] | Case report | 1 | 31 (F) | Preformed intrusion bulbs on clear aligners for vertical control in a hyperdivergent skeletal Class II case with extraction with a total of 71 sets of aligners | Improved vertical control and stability in hyperdivergent skeletal Class II case, with effective long-term results over a 4-year follow-up period |
| Capuozzo et al. (2023) [54] | Case series | 2 | 17 (F), 18 (F) | Microimplant-assisted aligner therapy; treatment duration of 20 and 18 months respectively | A Class I canine bond was established, with overbite and overjet normalized. The coordination of the maxillary and mandibular midlines was completed. |
| Auladell et al. (2022) [55] | Case series | 2 | 40 (M), 28 (F) | Molar distalization using clear aligners and mini-implants with 24 and 20 months of treatment, respectively | Effective molar distalization with improved treatment precision and reduced duration using mini-implants and aligners |
| Kottemann et al. (2020) [56] | Case series | 2 | 37 (F), 60 (F) | Use of TADs with clear aligners for asymmetry correction with 8 and 15 months of treatment respectively | Improved asymmetry correction with precise control and efficient tooth movement using TADs and clear aligners |
| Lin et al. (2024) [57] | Prospective study | 17 | Not specified | Three-dimensional measurement and analysis of mandibular molar distalization with micro-implant anchorage and clear aligners. Group A (ten cases) received no additional anchoring, while Group B (seven cases) received micro-implant anchorage to aid in mandibular molar distalization; treatment duration not specified. | Using micro-implant anchoring and a clear aligner for mandibular molar distalization protects the central incisor and increases crown distalization efficiency. |
| Ojima et al. (2020) [39] | Case series | 2 | 27 (F), 18 (M) | Aligner treatment with TADs for distalization of lower molars; 16 and 43 months of treatment, respectively | Achieved Class I molar relationship, improved facial profile, stable occlusion, significant improvement in occlusion and facial aesthetics |
| Wang et al. (2024) [58] | Case report | 1 | 19 (M) | Clear aligner treatment assisted by mini screws for Class II division 2 malocclusion and right upper canine correction; treatment duration of 19 months | Corrected malocclusion, repositioned upper canine, improved dental and facial aesthetics, high patient satisfaction and compliance |
| Choi et al. (2009) [59] | Case report | 1 | 16 (F) | Clear aligners and miniscrews for bialveolar protrusion; treatment duration of 21 months | Effective retraction of anterior teeth, improved aesthetics and function, patient comfort and satisfaction |
| Sabouni et al. (2022) [60] | Case series | 3 | 18 (M), 25 (F), 22 (F) | Clear aligner therapy for anterior open bite; duration varies from 10 to 12 to 35 months | Significant occlusal improvements, effective closure of anterior open bites, high patient satisfaction and compliance |
| Iodice et al. (2021) [61]. | Case report | 1 | 21 (F) | Full digital surgery-first approach using skeletal anchorage and clear aligners for the correction of gummy smile and Class II malocclusion with mandibular retrusion and deviation; treatment duration of 15 months | Significant aesthetic and functional improvements, reduced gummy smile, corrected malocclusion, stable occlusion, harmonious facial profile |
| Park et al. (2020) [26] | Case series | 3 | 30 (F), 32 (M), 41 (M) | Use of TADs with Invisalign to facilitate difficult tooth movements, treatment duration specified only for the first case report of 34 sets of aligners | Successful management of difficult orthodontic movements, with enhanced precision and control using TADs with Invisalign |
| de Almeida et al. (2024) [62] | Case series | 3 | 12 (M), 15 (M), 20 (M) | Biomechanics of clear aligners associated with TADs with 26, 11, and 15 months of treatment | Enhanced efficiency and predictability of complex tooth movements with the integration of TSADs and clear aligners |
| Authors | D1 | D2 | D3 | D4 | D5 | D6 | D7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Ojima et al. (2020) [39] |  |  |  |  |  |  |  |  |
| Capuozzo et al. (2023) [54] |  |  |  |  |  |  |  |  |
| Wang et al. (2024) [58] |  |  |  |  |  |  |  |  |
| Choi et al. (2009) [59] |  |  |  |  |  |  |  |  |
| Sabouni et al. (2022) [60] |  |  |  |  |  |  |  |  |
| Iodice et al. (2021) [61] |  |  |  |  |  |  |  |  |
| Greco et al. (2022) [51] |  |  |  |  |  |  |  |  |
| Greco et al. (2022) [52] |  |  |  |  |  |  |  |  |
| Lu et al. (2023) [53] |  |  |  |  |  |  |  |  |
| Park et al. (2020) [26] |  |  |  |  |  |  |  |  |
| de Almeida et al. (2024) [62] |  |  |  |  |  |  |  |  |
| Auladell et al. (2022) [55] |  |  |  |  |  |  |  |  |
| Kottemann et al. (2020) [56] |  |  |  |  |  |  |  |  |
| Lin et al. (2024) [57] |  |  |  |  |  |  |  |  |
 High.
High.  Some concerns.
Some concerns.  Low.
Low.Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinelli, G.; Inchingolo, A.M.; Inchingolo, A.D.; Ferrante, L.; Avantario, P.; Campanelli, M.; Palermo, A.; Inchingolo, F.; Dipalma, G. Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review. Bioengineering 2025, 12, 531. https://doi.org/10.3390/bioengineering12050531
Marinelli G, Inchingolo AM, Inchingolo AD, Ferrante L, Avantario P, Campanelli M, Palermo A, Inchingolo F, Dipalma G. Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review. Bioengineering. 2025; 12(5):531. https://doi.org/10.3390/bioengineering12050531
Chicago/Turabian StyleMarinelli, Grazia, Angelo Michele Inchingolo, Alessio Danilo Inchingolo, Laura Ferrante, Pasquale Avantario, Merigrazia Campanelli, Andrea Palermo, Francesco Inchingolo, and Gianna Dipalma. 2025. "Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review" Bioengineering 12, no. 5: 531. https://doi.org/10.3390/bioengineering12050531
APA StyleMarinelli, G., Inchingolo, A. M., Inchingolo, A. D., Ferrante, L., Avantario, P., Campanelli, M., Palermo, A., Inchingolo, F., & Dipalma, G. (2025). Temporary Anchorage Devices in Clear Aligner Therapy: A Systematic Review. Bioengineering, 12(5), 531. https://doi.org/10.3390/bioengineering12050531











