Self-Healing Polymeric Puerarin Hydrogel Dressing Promotes Diabetic Wound Healing Through Synergistic Immunomodulation and Tissue-Regenerative Remodeling
Abstract
:1. Introduction
2. Materials and Methods
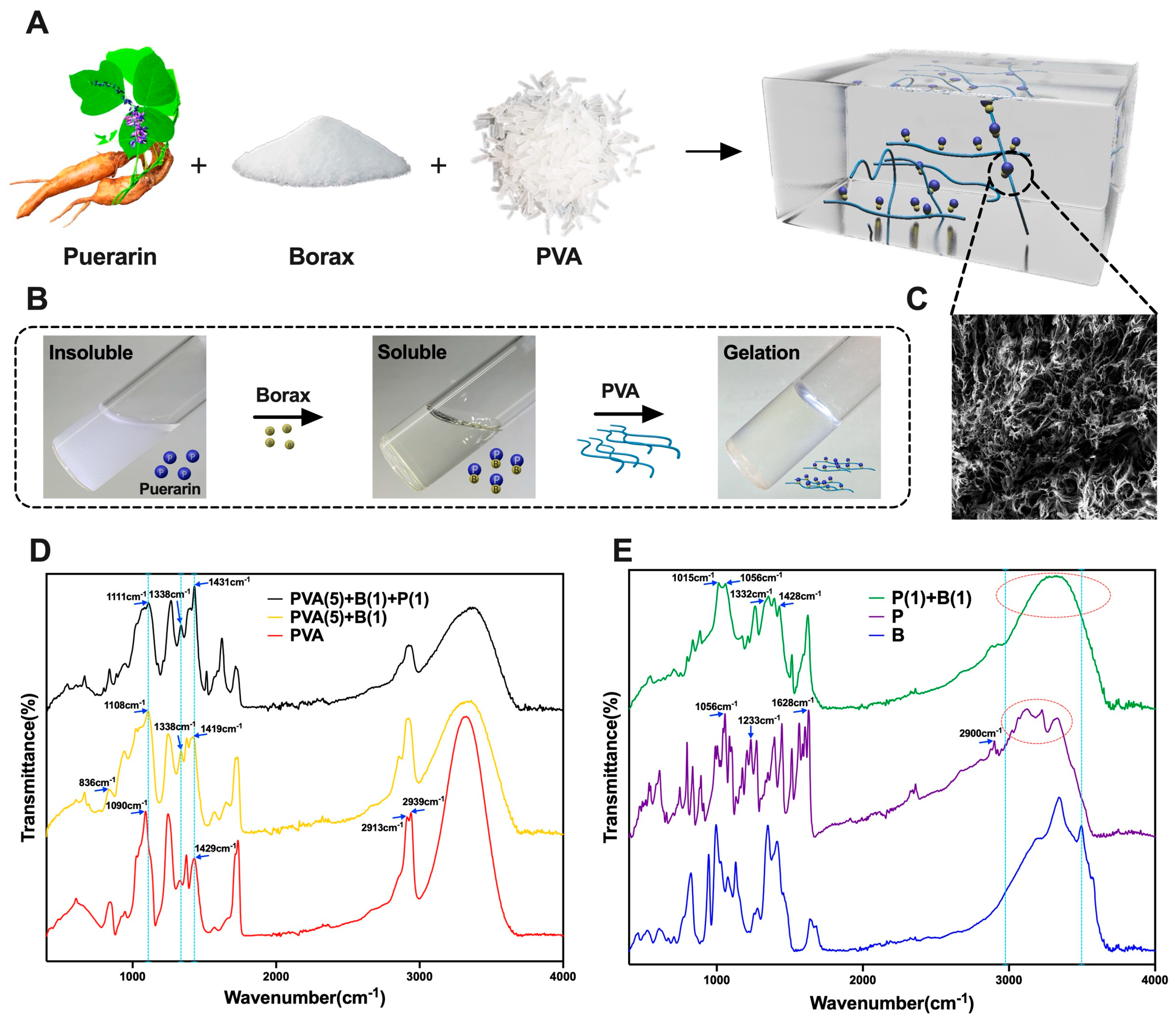
2.1. Preparation of Puerarin–Borax–PVA (BP) Hydrogel
2.2. Molecular Structure and Physical Characterization of Hydrogel
2.2.1. Fourier Transform Infrared Spectroscopy (FTIR)
2.2.2. Scanning Electron Microscope (SEM)
2.2.3. Rheological Properties
2.2.4. Physical Characterization
2.3. Evaluation of Hydrogel Biocompatibility
2.3.1. Cell Counting Kit-8 (CCK–8) Cell Proliferation Assay
2.3.2. Calcein–AM/PI Live/Dead Cell Staining
2.3.3. Hemolysis Test
2.3.4. Antibacterial Experiment of Hydrogel
2.4. Evaluation of the Efficacy of Hydrogel for Wound Healing
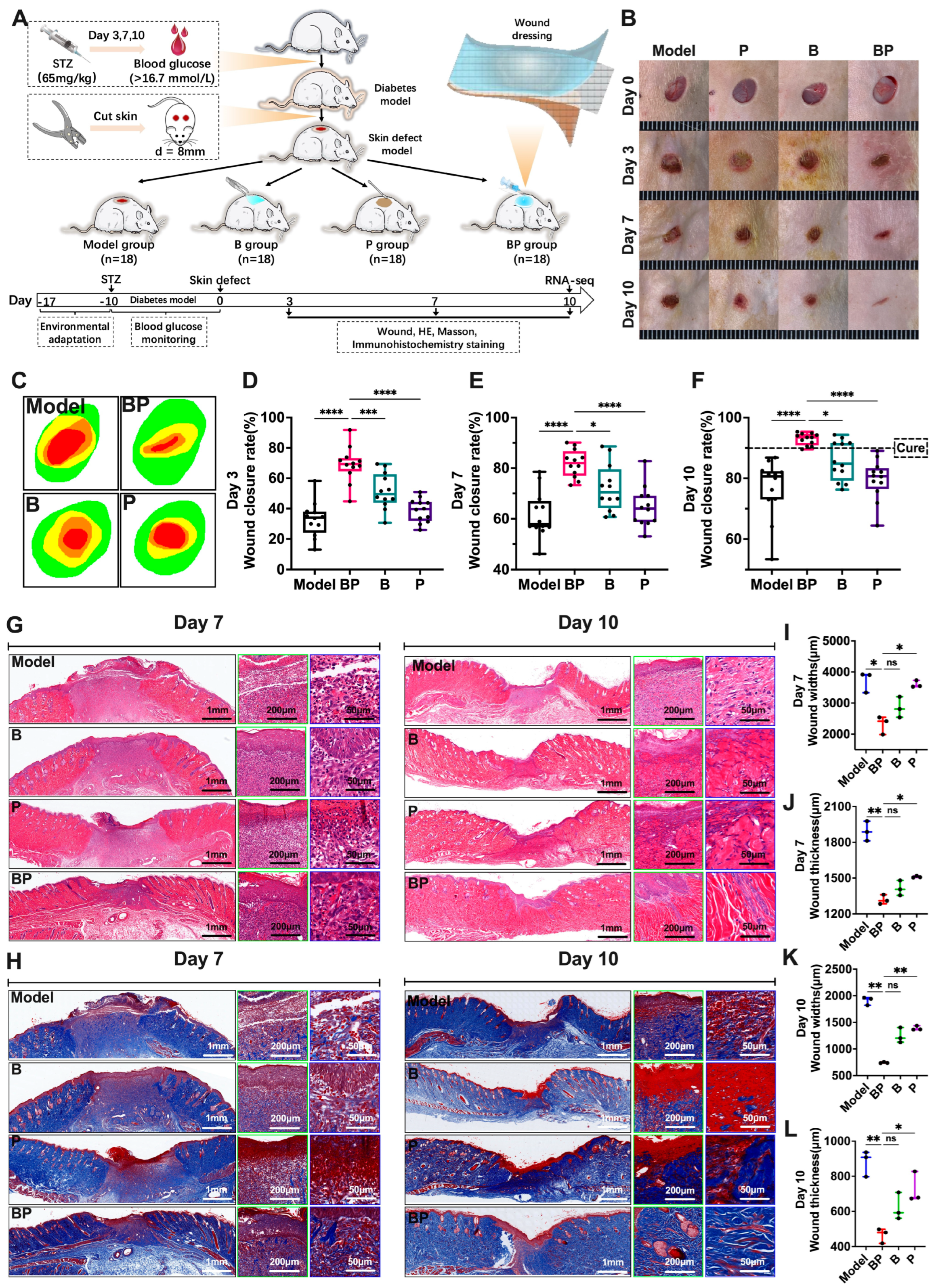
2.4.1. The Chronic Wound Model in Diabetic Rats
2.4.2. Treatment Protocol
2.4.3. Evaluation of In Vivo Wound Healing
2.4.4. Histological Analysis
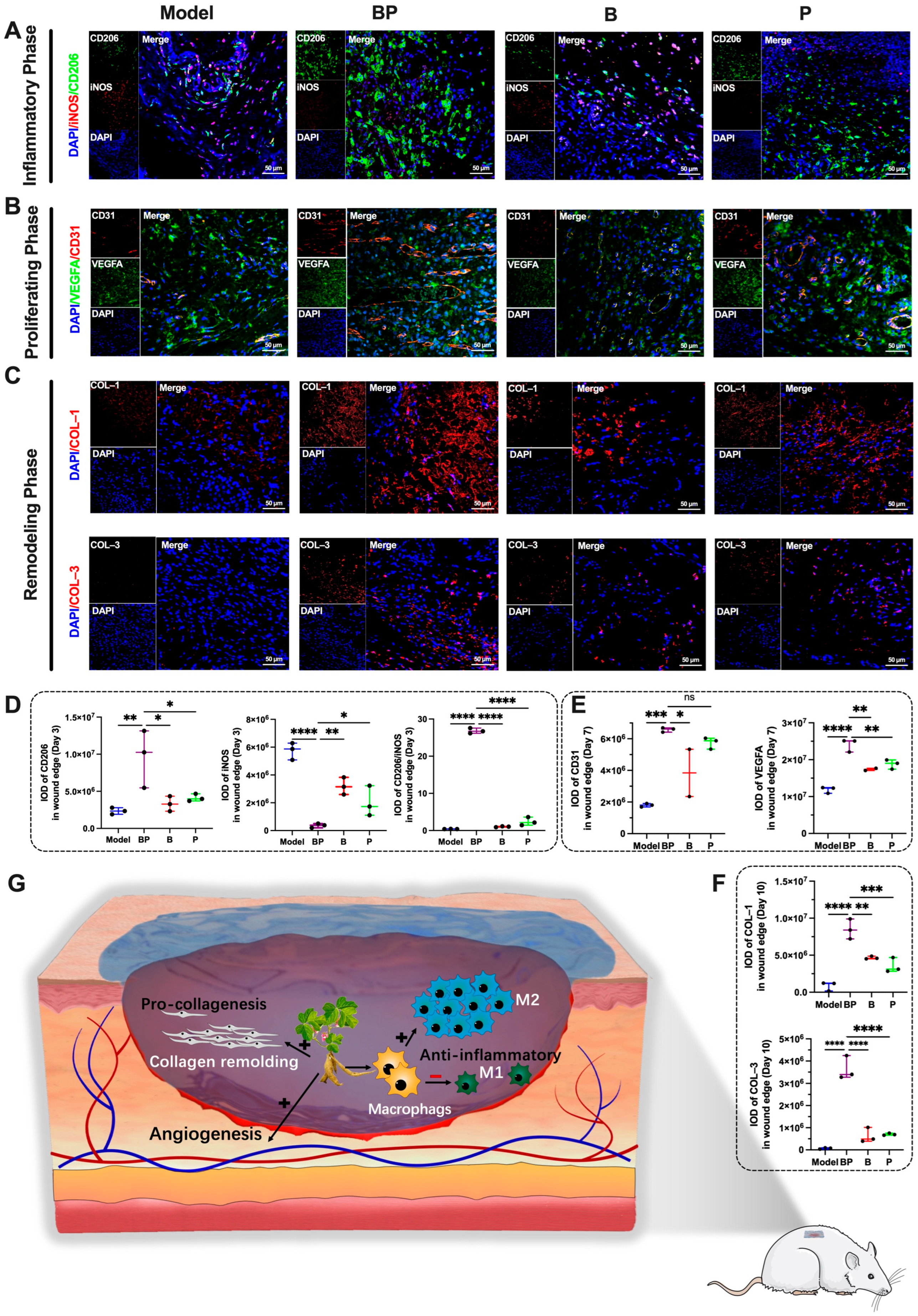
2.5. The Mechanism of BP Hydrogel in Promoting Wound Healing
2.5.1. RNA-Sequencing
2.5.2. Multiple Immunohistochemistry (mIHC)
2.6. Statistical Analysis
3. Results and Discussion
3.1. Preparation and Characterization of the BP Hydrogel
3.2. Rheological Behavior and Physical Properties of BP Hydrogel
3.3. Cell and Blood Biocompatibility of BP Hydrogel
3.4. BP Hydrogel Promoted the Healing of Chronic Wounds in Diabetic Rats
3.5. RNA–Seq Revealed the Mechanism of Hydrogel Promoting Wound Healing
3.6. BP Hydrogel Enhanced Anti-Inflammatory, Angiogenesis, and Collagen Remolding in the Process of Wound Healing
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HE | hematoxylin and eosin |
| PSR | picrosirius red |
| mIHC | multiple immunohistochemistry |
| P | puerarin |
| B | borax |
| BP | puerarin–borax–PVA |
| PVA | polyvinyl alcohol |
| SEM | scanning electron microscopy |
| FTIR | Fourier Transform Infrared |
| L929 | the mouse fibroblast cell line |
| DEGs | differentially expressed genes |
| GO | Gene Ontology |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| GSEA | Gene Set Enrichment Analysis |
| M1 | Type 1 macrophages |
| M2 | Type 2 macrophages |
| CCK-8 | Cell counting Kit-8 |
| STZ | streptozotocin |
| RIN | RNA integrity number |
| CD206 | Anti-Mannose Receptor |
References
- Gregg, E.W.; Buckley, J.; Ali, M.K.; Davies, J.; Flood, D.; Mehta, R.; Griffiths, B.; Lim, L.-L.; Manne-Goehler, J.; Pearson-Stuttard, J.; et al. Improving health outcomes of people with diabetes: Target setting for the WHO Global Diabetes Compact. Lancet 2023, 401, 1302–1312. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.C.N.; Lim, L.L.; Wareham, N.J.; Shaw, J.E.; Orchard, T.J.; Zhang, P.; Lau, E.S.H.; Eliasson, B.; Kong, A.P.S.; Ezzati, M.; et al. The Lancet Commission on diabetes: Using data to transform diabetes care and patient lives. Lancet 2021, 396, 2019–2082. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration. Worldwide trends in diabetes prevalence and treatment from 1990 to 2022: A pooled analysis of 1108 population-representative studies with 141 million participants. Lancet 2024, 404, 2077–2093. [Google Scholar] [CrossRef]
- Kumar, A.; Gangwar, R.; Ahmad Zargar, A.; Kumar, R.; Sharma, A. Prevalence of diabetes in India: A review of IDF Diabetes Atlas, 10th ed. Curr. Diabetes Rev. 2023, 20, 10. [Google Scholar] [CrossRef]
- Tottoli, E.M.; Dorati, R.; Genta, I.; Chiesa, E.; Pisani, S.; Conti, B. Skin Wound Healing Process and New Emerging Technologies for Skin Wound Care and Regeneration. Pharmaceutics 2020, 12, 735. [Google Scholar] [CrossRef]
- Bommer, C.; Sagalova, V.; Heesemann, E.; Manne-Goehler, J.; Atun, R.; Barnighausen, T.; Davies, J.; Vollmer, S. Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030. Diabetes Care 2018, 41, 963–970. [Google Scholar] [CrossRef]
- Bommer, C.; Heesemann, E.; Sagalova, V.; Manne-Goehler, J.; Atun, R.; Barnighausen, T.; Vollmer, S. The global economic burden of diabetes in adults aged 20–79 years: A cost-of-illness study. Lancet Diabetes Endocrinol. 2017, 5, 423–430. [Google Scholar] [CrossRef]
- Caskey, R.C.; Zgheib, C.; Morris, M.; Allukian, M.; Dorsett-Martin, W.; Xu, J.; Wu, W.; Liechty, K.W. Dysregulation of collagen production in diabetes following recurrent skin injury: Contribution to the development of a chronic wound. Wound Repair Regen. 2014, 22, 515–520. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration. Worldwide trends in diabetes since 1980: A pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016, 387, 1513–1530. [Google Scholar] [CrossRef]
- Rahman, M.M.; Garcia, N.; Loh, Y.S.; Marks, D.C.; Banakh, I.; Jagadeesan, P.; Cameron, N.R.; Yung-Chih, C.; Costa, M.; Peter, K.; et al. A platelet-derived hydrogel improves neovascularisation in full thickness wounds. Acta Biomater. 2021, 136, 199–209. [Google Scholar] [CrossRef]
- Park, S. Cyclic Glucans Enhance Solubility of Bioavailable Flavonoids. Molecules 2016, 21, 1556. [Google Scholar] [CrossRef]
- Dahiya, A.; Majee, C.; Mazumder, R.; Priya, N.; Atriya, A. Insight into the Glycosylation Methods of the Flavonoids as an Approach to Enhance Its Bioavailability and Pharmacological Activities. Indian J. Pharm. Educ. 2023, 57, 354–371. [Google Scholar] [CrossRef]
- Zeng, X.; Chen, B.; Wang, L.; Sun, Y.; Jin, Z.; Liu, X.; Ouyang, L.; Liao, Y. Chitosan@Puerarin hydrogel for accelerated wound healing in diabetic subjects by miR-29ab1 mediated inflammatory axis suppression. Bioact. Mater. 2023, 19, 653–665. [Google Scholar] [CrossRef]
- Yen, P.T.; Huang, S.E.; Hsu, J.H.; Kuo, C.H.; Chao, Y.Y.; Wang, L.S.; Yeh, J.L. Anti-Inflammatory and Anti-oxidative Effects of Puerarin in Postmenopausal Cardioprotection: Roles of Akt and Heme Oxygenase-1. Am. J. Chin. Med. 2023, 51, 149–168. [Google Scholar] [CrossRef]
- Liu, G.Y.; Liu, Z.H.; Yuan, S. Recent Advances in Methods of Puerarin Biotransformation. Mini Rev. Med. Chem. 2016, 16, 1392–1402. [Google Scholar] [CrossRef]
- Lee, S.; Shin, H.; Bae, J.; Lee, T.; Kim, M.; Jeon, H.B.; Lee, K.H.; Yoo, H.Y.; Park, C. Enhanced Enzymatic Synthesis of Puerarin Palmitate with Different Acyl Donors for Lipid Solubility Improvement. Int. J. Mol. Sci. 2024, 25, 709. [Google Scholar] [CrossRef]
- Zhang, G.Z.; Ji, J.W.; Sun, M.Z.; Ji, Y.Q.; Ji, H.J. Comparative Pharmacokinetic Profiles of Puerarin in Rat Plasma by UHPLC-MS/MS after Oral Administration of Pueraria lobata Extract and Pure Puerarin. J. Anal. Methods Chem. 2020, 2020, 4258156. [Google Scholar] [CrossRef]
- Geng, S.H.; Zhang, H.; Zhang, Y.C.; Liu, L.; Yu, S.S.; Lan, X.Y.; Gao, Y.R.; Ling, Z.X.; Zhang, Y.; Li, X.X.; et al. Puerarin hydrogel: Design and applications in biomedical engineering. J. Drug Deliv. Sci. Technol. 2024, 97, 105802. [Google Scholar] [CrossRef]
- Pan, Y.J.; Lin, T.C.; Shao, L.Q.; Zhang, Y.L.; Han, Q.; Sheng, L.Y.; Guo, R.; Sun, T.; Zhang, Y.L. Lignin/Puerarin Nanoparticle-Incorporated Hydrogel Improves Angiogenesis through Puerarin-Induced Autophagy Activation. Int. J. Nanomed. 2023, 18, 5095–5117. [Google Scholar] [CrossRef]
- Li, T.; Shi, C.H.; Mi, Z.A.; Xu, H.J.; Xu, J.H.; Wang, L.L.; Zhang, X.R. Biocompatible puerarin injectable-hydrogel using self-assembly tetrapeptide for local treatment of osteoarthritis in rats. J. Drug Deliv. Sci. Technol. 2022, 78, 103909. [Google Scholar] [CrossRef]
- Cai, Y.; Zhang, J.; He, Y.; Li, Z.; Hua, Y.; Wu, Z.; Gao, J.; Ou, C.; Chen, M. A Supramolecular Hydrogel of Puerarin. J. Biomed. Nanotechnol. 2018, 14, 257–266. [Google Scholar] [CrossRef]
- Kaymazlar, E.; Dikbas, C.; Matar, G.H.; Andac, O.; Andac, M. Self-healable and conductive mussel inspired PVA/borax@PDA-LiTFSI hydrogel-based self-adhesive for human motion sensor. Polym. Bull. 2024, 81, 8751–8764. [Google Scholar] [CrossRef]
- Liu, J.N.; He, Q.; Pan, M.Y.; Du, K.; Gong, C.B.; Tang, Q. An energy-saving, bending sensitive, and self-healing PVA-borax-IL ternary hydrogel electrolyte for visual flexible electrochromic strain sensors. J. Mater. Chem. A 2022, 10, 25118–25128. [Google Scholar] [CrossRef]
- Palungan, J.; Luthfiyah, W.; Mustopa, A.Z.; Nurfatwa, M.; Rahman, L.; Yulianty, R.; Wathoni, N.; Yoo, J.W.; Hasan, N. The Formulation and Characterization of Wound Dressing Releasing S-Nitrosoglutathione from Polyvinyl Alcohol/Borax Reinforced Carboxymethyl Chitosan Self-Healing Hydrogel. Pharmaceutics 2024, 16, 344. [Google Scholar] [CrossRef]
- Alifah, N.; Palungan, J.; Ardayanti, K.; Ullah, M.; Nurkhasanah, A.N.; Mustopa, A.Z.; Lallo, S.; Agustina, R.; Yoo, J.W.; Hasan, N. Development of Clindamycin-Releasing Polyvinyl Alcohol Hydrogel with Self-Healing Property for the Effective Treatment of Biofilm-Infected Wounds. Gels 2024, 10, 482. [Google Scholar] [CrossRef]
- Ding, P.; Ding, X.Y.; Li, J.Y.; Guo, W.; Okoro, O.V.; Mirzaei, M.; Sun, Y.F.; Jiang, G.H.; Shavandi, A.; Nie, L. Facile preparation of self-healing hydrogels based on chitosan and PVA with the incorporation of curcumin-loaded micelles for wound dressings. Biomed. Mater. 2024, 19, 025021. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, K.Y.; He, Y.M.; Chang, R.; Guan, F.X.; Yao, M.H. A multifunctional hydrogel dressing with high tensile and adhesive strength for infected skin wound healing in joint regions. J. Mater. Chem. B 2023, 11, 11135–11149. [Google Scholar] [CrossRef]
- Pan, X.F.; Wang, Q.H.; He, P.; Liu, K.; Ni, Y.H.; Chen, L.H.; Ouyang, X.H.; Huang, L.L.; Wang, H.P.; Xu, S.Y. A bionic tactile plastic hydrogel-based electronic skin constructed by a nerve-like nanonetwork combining stretchable, compliant, and self-healing properties. Chem. Eng. J. 2020, 379, 122271. [Google Scholar] [CrossRef]
- Pan, X.F.; Wang, Q.H.; Ning, D.W.; Dai, L.; Liu, K.; Ni, Y.H.; Chen, L.H.; Huang, L.L. Ultraflexible Self-Healing Guar Gum-Glycerol Hydrogel with Injectable, Antifreeze, and Strain-Sensitive Properties. ACS Biomater. Sci. Eng. 2018, 4, 3397–3404. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Kenawy, E.R.S.; Chen, X. A review on polymeric hydrogel membranes for wound dressing applications: PVA-based hydrogel dressings. J. Adv. Res. 2017, 8, 217–233. [Google Scholar] [CrossRef]
- Liu, S.; Li, D.; Wang, Y.; Zhou, G.; Ge, K.; Jiang, L.; Fang, D. Flexible, high-strength and multifunctional polyvinyl alcohol/MXene/polyaniline hydrogel enhancing skin wound healing. Biomater. Sci. 2022, 10, 3585–3596. [Google Scholar] [CrossRef]
- Pan, H.; Fan, D.; Zhu, C.; Duan, Z.; Fu, R.; Li, X. Preparation of physically crosslinked PVA/HLC/SA hydrogel and exploration of its effects on full-thickness skin defects. Int. J. Polym. Mater. 2019, 68, 1048–1057. [Google Scholar] [CrossRef]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef]
- Kumar, A.; Lee, Y.; Kim, D.; Rao, K.M.; Kim, J.; Park, S.; Haider, A.; Lee, D.H.; Han, S.S. Effect of crosslinking functionality on microstructure, mechanical properties, and cytocompatibility of cellulose nanocrystals reinforced poly (vinyl alcohol)/sodium alginate hybrid scaffolds. Int. J. Biol. Macromol. 2017, 95, 962–973. [Google Scholar] [CrossRef]
- Ge, W.J.; Cao, S.; Shen, F.; Wang, Y.Y.; Ren, J.L.; Wang, X.H. Rapid self-healing, stretchable, moldable, antioxidant and antibacterial tannic acid-cellulose nanofibril composite hydrogels. Carbohydr. Polym. 2019, 224, 115147. [Google Scholar] [CrossRef]
- Lei, H.; Fan, D.D. Conductive, adaptive, multifunctional hydrogel combined with electrical stimulation for deep wound repair. Chem. Eng. J. 2021, 421, 129578. [Google Scholar] [CrossRef]
- Lei, H.; Fan, D.D. A Combination Therapy Using Electrical Stimulation and Adaptive, Conductive Hydrogels Loaded with Self-Assembled Nanogels Incorporating Short Interfering RNA Promotes the Repair of Diabetic Chronic Wounds. Adv. Sci. 2022, 9, 2201425. [Google Scholar] [CrossRef]
- Matsusaki, M.; Yoshida, H.; Akashi, M. The construction of 3D-engineered tissues composed of cells and extracellular matrices by hydrogel template approach. Biomaterials 2007, 28, 2729–2737. [Google Scholar] [CrossRef]
- Chelu, M.; Moreno, J.C.; Atkinson, I.; Cusu, J.P.; Rusu, A.; Bratan, V.; Aricov, L.; Anastasescu, M.; Seciu-Grama, A.M.; Musuc, A.M. Green synthesis of bioinspired chitosan-ZnO-based polysaccharide gums hydrogels with propolis extract as novel functional natural biomaterials. Int. J. Biol. Macromol. 2022, 211, 410–424. [Google Scholar] [CrossRef]
- Türk, S.; Altinsoy, I.; Efe, G.Ç.; Ipek, M.; Özacar, M.; Bindal, C. A novel multifunctional NCQDs-based injectable self-crosslinking and in situ forming hydrogel as an innovative stimuli responsive smart drug delivery system for cancer therapy. Mat. Sci. Eng. C Mater. 2021, 121, 111829. [Google Scholar] [CrossRef]
- ASTM F756-17; Standard Practice for Assessment of Hemolytic Properties of Materials. American Society for Testing Materials: West Conshohocken, PA, USA, 2017. [CrossRef]
- Yang, Y.L.; Wang, M.; Luo, M.; Chen, M.; Wei, K.; Lei, B. Injectable self-healing bioactive antioxidative one-component poly(salicylic acid) hydrogel with strong ultraviolet-shielding for preventing skin light injury. Mat. Sci. Eng. C Mater. 2021, 126, 112107. [Google Scholar] [CrossRef]
- Rathod, L.; Bhowmick, S.; Patel, P.; Sawant, K. Calendula flower extract loaded PVA hydrogel sheet for wound management: Optimization, characterization and in-vivo study. J. Drug Deliv. Sci. Technol. 2022, 68, 103035. [Google Scholar] [CrossRef]
- Sharifiaghdam, M.; Shaabani, E.; Faridi-Majidi, R.; De Smedt, S.C.; Braeckmans, K.; Fraire, J.C. Macrophages as a therapeutic target to promote diabetic wound healing. Mol. Ther. 2022, 30, 2891–2908. [Google Scholar] [CrossRef]
- Stacey, M.C. Biomarker directed chronic wound therapy-A new treatment paradigm. J. Tissue Viability 2020, 29, 180–183. [Google Scholar] [CrossRef]
- Toriseva, M.J.; Ala-aho, R.; Karvinen, J.; Baker, A.H.; Marjomäki, V.S.; Heino, J.; Kähäri, V.M. Collagenase-3 (MMP-13) enhances remodeling of three-dimensional collagen and promotes survival of human skin fibroblasts. J. Investig. Dermatol. 2007, 127, 49–59. [Google Scholar] [CrossRef]
- Xie, J.; Wu, X.W.; Zheng, S.; Lin, K.L.; Su, J.S. Aligned electrospun poly(L-lactide) nanofibers facilitate wound healing by inhibiting macrophage M1 polarization via the JAK-STAT and NF-κB pathways. J. Nanobiotechnol. 2022, 20, 342. [Google Scholar] [CrossRef]
- Jere, S.W.; Abrahamse, H.; Houreld, N.N. The JAK/STAT signaling pathway and photobiomodulation in chronic wound healing. Cytokine Growth Factor Rev. 2017, 38, 73–79. [Google Scholar] [CrossRef]
- Wynn, T.A.; Vannella, K.M. Macrophages in Tissue Repair, Regeneration, and Fibrosis. Immunity 2016, 44, 450–462. [Google Scholar] [CrossRef]
- Huang, C.; Dong, L.L.; Zhao, B.H.; Lu, Y.F.; Huang, S.R.; Yuan, Z.Q.; Luo, G.X.; Xu, Y.; Qian, W. Anti-inflammatory hydrogel dressings and skin wound healing. Clin. Transl. Med. 2022, 12, e1094. [Google Scholar] [CrossRef]
- Martin, K.E.; García, A.J. Macrophage phenotypes in tissue repair and the foreign body response: Implications for biomaterial-based regenerative medicine strategies. Acta Biomater. 2021, 133, 4–16. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Z.H.; Zhao, K.; Mu, Y.D.; Li, K.L.; Yuan, Z.M.; Liu, Z.G.; Han, L.; Lü, W.D. Acellular embryoid body and hydroxybutyl chitosan composite hydrogels promote M2 macrophage polarization and accelerate diabetic cutaneous wound healing. Mater Today Bio 2024, 25, 100975. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Ou, J.Z.; Chen, Y.Z.; Tian, Y.; Song, W.; Hu, X.H.; Ju, X.Y.; Jiang, S.D.; Huang, S.; Niu, Z.W. Programming of macrophage polarization in different stages for accelerating wound healing. Chem. Eng. J. 2024, 491, 152131. [Google Scholar] [CrossRef]
- Wu, D.; Wu, X.Y.; Luan, Q.C.; Tang, Q.; Fan, L.; Shou, X.; Gao, X.; Qian, X.Y.; Zhao, Y.J. Dynamic hydrogel-integrated microneedle patch with extracellular vesicles encapsulation for wound healing. Chem. Eng. J. 2024, 493, 152252. [Google Scholar] [CrossRef]
- Liu, J.Y.; Zhang, Y.H.; Liu, C.; Jiang, Y.H.; Wang, Z.H.; Guo, Z.K.; Li, X.S. A single dose of VEGF-A circular RNA sustains in situ long-term expression of protein to accelerate diabetic wound healing. J. Control. Release 2024, 373, 319–335. [Google Scholar] [CrossRef]
- He, F.; Xu, P.Q.; Zhu, Z.K.; Zhang, Y.; Cai, C.H.; Zhang, Y.X.; Shao, J.M.; Jin, F.; Li, Q.; You, J.H.; et al. Inflammation-Responsive Hydrogel Accelerates Diabetic Wound Healing through Immunoregulation and Enhanced Angiogenesis. Adv. Healthc. Mater. 2024, 14, 2400150. [Google Scholar] [CrossRef]
- Zeng, J.J.; Lu, M.H.; Wang, Y.; Zhao, X.Z.; Zhao, Y.J. Photothermal Fish Gelatin-Graphene Microneedle Patches for Chronic Wound Treatment. Small 2024, 20, 2405847. [Google Scholar] [CrossRef]
- Huang, X.A.; Wang, A.A.; Sun, T.Z.; Tai, R.; Li, J.W.; Qiao, Z.Y.; Zhao, L.Z.; Zhang, T.; Zhao, Y.T. In Situ injectable photo-crosslinking hydrogel with heterojunction nanoparticles for dual-channel synergistic disinfection and cutaneous regeneration in diabetic chronic wound healing. Nano Today 2024, 56, 102235. [Google Scholar] [CrossRef]
- Ma, Y.D.; Lai, X.Y.; Luo, X.; Luo, Z.; Mao, L.Z.; Zhu, H.J.; Fan, X.T.; Kong, J.H.; Wu, Y.L.; Li, Z.B.; et al. Multifunctional Silver-Enzyme Nanogels Assembly with Efficient Trienzyme Cascades for Synergistic Diabetic Wound Healing. Adv. Funct. Mater. 2024, 34, 2405644. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, C.X.; Cheng, M.Q.; Hu, L.; Zhang, Z.Y.; Sun, Q.S.; Wang, S.S.; Fan, Y.N.; Pan, P.P.; Chen, J.D. Self-Healing Conductive Hydrogels with Dynamic Dual Network Structure Accelerate Infected Wound Healing Photothermal Antimicrobial and Regulating Inflammatory Response. ACS Appl. Mater. Inter. 2024, 16, 30776–30792. [Google Scholar] [CrossRef]
- Zhu, R.Y.; Huang, Z.Y.; Zhang, J.Y.; Shi, G.G.; Cai, X.M.; Dou, R.; Tang, J.R.; Zhang, C.P.; Zhao, Y.F.; Chen, J. The potential of collagen-based materials for wound management. Mater. Today Chem. 2024, 41, 102295. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Huang, J.H.; Zhao, J.; Li, L.S.; Miao, F.Z.; Zhang, T.R.; Chen, Z.J.; Zhou, X.; Tai, Z.G.; Zhu, Q.A. Exosome-mimetic vesicles derived from fibroblasts carrying matrine for wound healing. Burns Trauma 2024, 12, tkae015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.Y.; Huang, Y.W.; Luo, T.; Hu, C.; Li, H.H.; Fan, X.J.; Wang, K.F.; Liang, J.; Chen, Y.F.; Fan, Y.J. Advanced Wound Healing and Scar Reduction Using an Innovative Anti-ROS Polysaccharide Hydrogel with Recombinant Human Collagen Type III. ACS Appl. Mater. Inter. 2024, 16, 50305–50320. [Google Scholar] [CrossRef] [PubMed]
- Xiong, L.; Zhou, C.; Tong, L.; Han, X.W.; Zou, Y.P.; Dong, Z.Q.; Liang, J.; Chen, Y.F.; Fan, Y.J. Injectable hydrogels of recombinant human collagen type III and chitosan with antibacterial and antioxidative activities for wound healing. J. Mater. Chem. B 2023, 11, 4131–4142. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Geng, S.; Liu, L.; Yimingjiang, M.; Lin, Z.; Fu, J.; Yu, S.; Li, X.; Yan, A.; Yuan, K.; Huang, G.; et al. Self-Healing Polymeric Puerarin Hydrogel Dressing Promotes Diabetic Wound Healing Through Synergistic Immunomodulation and Tissue-Regenerative Remodeling. Bioengineering 2025, 12, 427. https://doi.org/10.3390/bioengineering12040427
Geng S, Liu L, Yimingjiang M, Lin Z, Fu J, Yu S, Li X, Yan A, Yuan K, Huang G, et al. Self-Healing Polymeric Puerarin Hydrogel Dressing Promotes Diabetic Wound Healing Through Synergistic Immunomodulation and Tissue-Regenerative Remodeling. Bioengineering. 2025; 12(4):427. https://doi.org/10.3390/bioengineering12040427
Chicago/Turabian StyleGeng, Shaohui, Li Liu, Mureziya Yimingjiang, Zhimin Lin, Jingyuan Fu, Shasha Yu, Xinxin Li, Aimin Yan, Kai Yuan, Guangrui Huang, and et al. 2025. "Self-Healing Polymeric Puerarin Hydrogel Dressing Promotes Diabetic Wound Healing Through Synergistic Immunomodulation and Tissue-Regenerative Remodeling" Bioengineering 12, no. 4: 427. https://doi.org/10.3390/bioengineering12040427
APA StyleGeng, S., Liu, L., Yimingjiang, M., Lin, Z., Fu, J., Yu, S., Li, X., Yan, A., Yuan, K., Huang, G., & Xu, A. (2025). Self-Healing Polymeric Puerarin Hydrogel Dressing Promotes Diabetic Wound Healing Through Synergistic Immunomodulation and Tissue-Regenerative Remodeling. Bioengineering, 12(4), 427. https://doi.org/10.3390/bioengineering12040427






