Artificial Intelligence-Driven Wireless Sensing for Health Management
Abstract
1. Introduction
2. Materials and Methods
3. A Brief Overview of Wireless Sensing Technology
3.1. Radar
3.2. CSI
3.3. RFID
3.4. Acoustic Sensing
4. Results
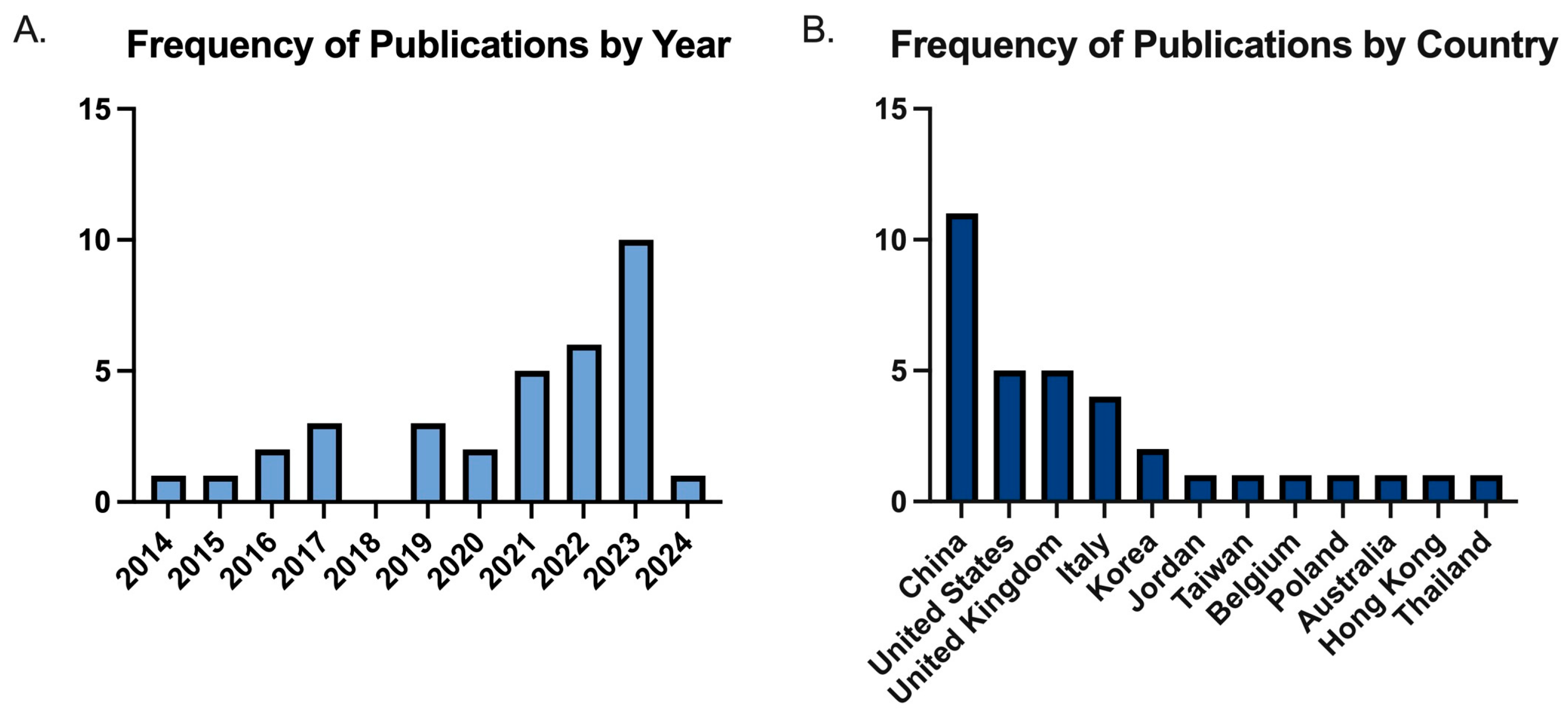
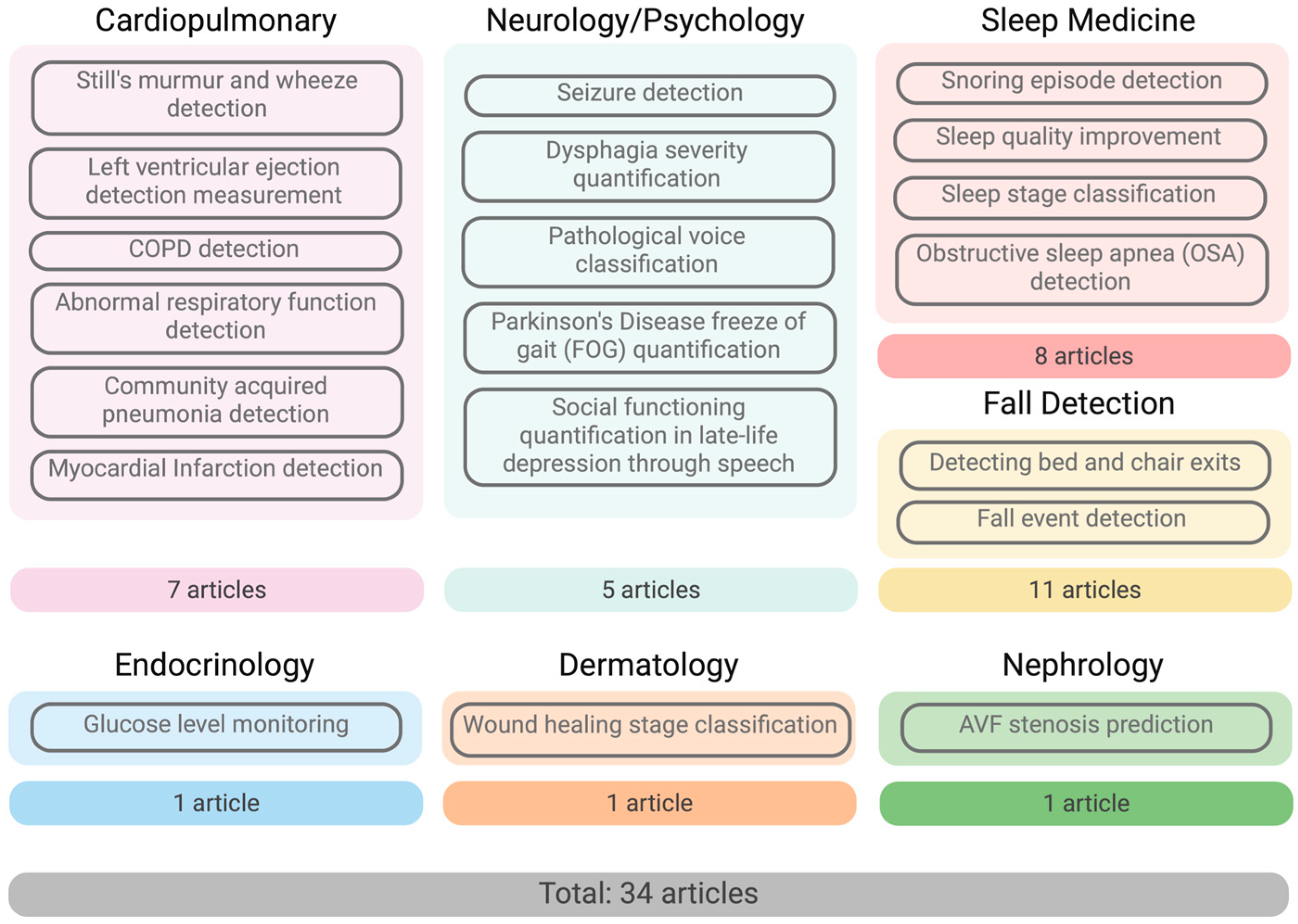
4.1. Characteristics of Individual Studies
4.2. Findings of Wireless Sensing Studies in Personal Health
4.2.1. Cardiopulmonary
4.2.2. Neurology and Psychiatry
4.2.3. Sleep Medicine
4.2.4. Fall Detection for Geriatrics
4.2.5. Endocrinology
4.2.6. Dermatology
4.2.7. Nephrology
4.3. Benefits and Limitations of Wireless Sensing Approaches
4.4. Ethical Considerations
5. Discussion
5.1. Shift from Disease-Specific to Multimodal Monitoring
5.2. Personalization for Improved Accuracy
5.3. Clinical Validation
5.4. Integration with Healthcare Systems and Interoperability
5.5. Sustainability and Device Lifespan
5.6. Ethical Considerations and Data Privacy
5.7. Next-Generation Wireless Sensing Technologies
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hoffman, C.; Rice, D.; Sung, H.Y. Persons with chronic conditions: Their prevalence and costs. JAMA 1996, 276, 1473–1479. [Google Scholar] [CrossRef] [PubMed]
- Guk, K.; Han, G.; Lim, J.; Jeong, K.; Kang, T.; Lim, E.K.; Jung, J. Evolution of Wearable Devices with Real-Time Disease Monitoring for Personalized Healthcare. Nanomaterials 2019, 9, 813. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Campbell, A.S.; de Avila, B.E.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, P.; Liu, J.; Gong, Y.; Wang, J.; Guo, Y. Emerging Artificial Intelligence-Empowered mHealth: Scoping Review. JMIR mHealth uHealth 2022, 10, e35053. [Google Scholar] [CrossRef]
- Baig, M.M.; Gholam Hosseini, H.; Moqeem, A.A.; Mirza, F.; Linden, M. A Systematic Review of Wearable Patient Monitoring Systems—Current Challenges and Opportunities for Clinical Adoption. J. Med. Syst. 2017, 41, 115. [Google Scholar] [CrossRef]
- Kaidi, H.M.; Izhar, M.A.M.; Dziyauddin, R.A.; Shaiful, N.E.; Ahmad, R. A Comprehensive Review on Wireless Healthcare Monitoring: System Components. IEEE Access 2024, 12, 35008–35032. [Google Scholar] [CrossRef]
- Haque, A.; Milstein, A.; Fei-Fei, L. Illuminating the dark spaces of healthcare with ambient intelligence. Nature 2020, 585, 193–202. [Google Scholar] [CrossRef]
- Kang, M.; Chai, K. Wearable Sensing Systems for Monitoring Mental Health. Sensors 2022, 22, 994. [Google Scholar] [CrossRef]
- Kebe, M.; Gadhafi, R.; Mohammad, B.; Sanduleanu, M.; Saleh, H.; Al-Qutayri, M. Human Vital Signs Detection Methods and Potential Using Radars: A Review. Sensors 2020, 20, 1454. [Google Scholar] [CrossRef]
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: https://www.covidence.org (accessed on 31 January 2025).
- Wang, X.; Shao, D. Chapter 1—Human physiology and contactless vital signs monitoring using camera and wireless signals. In Contactless Vital Signs Monitoring; Wang, W., Wang, X., Eds.; Academic Press: London, UK, 2022; pp. 1–24. [Google Scholar]
- Liu, X.; Cao, J.; Tang, S.; Wen, J. Wi-Sleep: Contactless Sleep Monitoring via WiFi Signals. In Proceedings of the 2014 IEEE Real-Time Systems Symposium, Rome, Italy, 2–5 December 2014; pp. 346–355. [Google Scholar]
- Liu, J.; Wang, Y.; Chen, Y.; Yang, J.; Chen, X.; Cheng, J. Tracking vital signs during sleep leveraging off-the-shelf WiFi. In Proceedings of the 16th ACM International Symposium on Mobile Ad Hoc Networking and Computing, MobiHoc 2015: Association for Computing Machinery, Hangzhou, China, 22–25 June 2015; pp. 267–276. [Google Scholar]
- Wang, X.; Yang, C.; Mao, S. On CSI-Based Vital Sign Monitoring Using Commodity WiFi. ACM Trans. Comput. Healthc. 2020, 1, 1–27. [Google Scholar] [CrossRef]
- Wang, X.; Yang, C.; Mao, S. PhaseBeat: Exploiting CSI Phase Data for Vital Sign Monitoring with Commodity WiFi Devices. In Proceedings of the 2017 IEEE 37th International Conference on Distributed Computing Systems (ICDCS), Atlanta, GA, USA, 5–8 June 2017. [Google Scholar]
- Wang, C.; Xie, L.; Wang, W.; Chen, Y.; Bu, Y.; Lu, S. RF-ECG: Heart Rate Variability Assessment Based on COTS RFID Tag Array. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2018, 2, 1–26. [Google Scholar] [CrossRef]
- Yang, C.; Wang, X.; Mao, S. Respiration Monitoring With RFID in Driving Environments. IEEE J. Sel. Areas Commun. 2021, 39, 500–512. [Google Scholar] [CrossRef]
- Yang, C.; Wang, X.; Mao, S. Unsupervised Detection of Apnea Using Commodity RFID Tags With a Recurrent Variational Autoencoder. IEEE Access 2019, 7, 67526–67538. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, J.; Yu, Z.; Mao, S.; Periaswamy, S.C.G.; Patton, J. On Remote Temperature Sensing Using Commercial UHF RFID Tags. IEEE Internet Things J. 2019, 6, 10715–10727. [Google Scholar] [CrossRef]
- Duroc, Y. From Identification to Sensing: RFID Is One of the Key Technologies in the IoT Field. Sensors 2022, 22, 7523. [Google Scholar] [CrossRef]
- Ren, Y.; Wang, C.; Yang, J.; Chen, Y. Fine-grained sleep monitoring: Hearing your breathing with smartphones. In Proceedings of the 2015 IEEE Conference on Computer Communications (INFOCOM), Hong Kong, China, 26 April–1 May 2015. [Google Scholar]
- Arjoune, Y.; Nguyen, T.N.; Salvador, T.; Telluri, A.; Schroeder, J.C.; Geggel, R.L.; May, J.W.; Pillai, D.K.; Teach, S.J.; Patel, S.J.; et al. StethAid: A Digital Auscultation Platform for Pediatrics. Sensors 2023, 23, 5750. [Google Scholar] [CrossRef]
- Howard-Quijano, K.; Saraf, K.; Borgstrom, P.; Baek, C.; Wasko, M.; Zhang, X.; Zheng, Y.; Saba, S.; Mukkamala, R.; Kaiser, W.; et al. Evaluation of Wearable Acoustic Sensors and Machine Learning Algorithms for Automated Measurement of Left Ventricular Ejection Fraction. Am. J. Cardiol. 2023, 200, 87–94. [Google Scholar] [CrossRef]
- Lalouani, W.; Younis, M.; Emokpae, R.N., Jr.; Emokpae, L.E. Enabling effective breathing sound analysis for automated diagnosis of lung diseases. Smart Health 2022, 26, 100329. [Google Scholar] [CrossRef]
- Al-Momani, O.; Gharaibeh, K.M. Effect of wireless channels on detection and classification of asthma attacks in wireless remote health monitoring systems. Int. J. Telemed. Appl. 2014, 2014, 816369. [Google Scholar] [CrossRef][Green Version]
- Tseng, S.T.; Kao, Y.H.; Peng, C.C.; Liu, J.Y.; Chu, S.C.; Hong, G.F.; Hsieh, C.H.; Hsu, K.T.; Liu, W.T.; Huang, Y.H.; et al. A 65-nm CMOS Low-Power Impulse Radar System for Human Respiratory Feature Extraction and Diagnosis on Respiratory Diseases. IEEE Trans. Microw. Theory Tech. 2016, 64, 1029–1041. [Google Scholar] [CrossRef]
- Zhang, J.; Wu, Y.; Chen, Y.; Chen, T. Health-Radio: Towards Contactless Myocardial Infarction Detection Using Radio Signals. IEEE Trans. Mob. Comput. 2022, 21, 585–597. [Google Scholar] [CrossRef]
- Huang, D.; Wang, L.; Wang, W. A Multi-Center Clinical Trial for Wireless Stethoscope-Based Diagnosis and Prognosis of Children Community-Acquired Pneumonia. IEEE Trans. Biomed. Eng. 2023, 70, 2215–2226. [Google Scholar] [CrossRef] [PubMed]
- Van de Vel, A.; Milosevic, M.; Bonroy, B.; Cuppens, K.; Lagae, L.; Vanrumste, B.; Van Huffel, S.; Ceulemans, B. Long-term accelerometry-triggered video monitoring and detection of tonic-clonic and clonic seizures in a home environment: Pilot study. Epilepsy Behav. Case Rep. 2016, 5, 66–71. [Google Scholar] [CrossRef][Green Version]
- O’Brien, M.K.; Botonis, O.K.; Larkin, E.; Carpenter, J.; Martin-Harris, B.; Maronati, R.; Lee, K.; Cherney, L.R.; Hutchison, B.; Xu, S.; et al. Advanced Machine Learning Tools to Monitor Biomarkers of Dysphagia: A Wearable Sensor Proof-of-Concept Study. Digit. Biomark. 2021, 5, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Verde, L.; Pietro, G.D.; Alrashoud, M.; Ghoneim, A.; Al-Mutib, K.N.; Sannino, G. Leveraging Artificial Intelligence to Improve Voice Disorder Identification Through the Use of a Reliable Mobile App. IEEE Access 2019, 7, 124048–124054. [Google Scholar] [CrossRef]
- Tahir, A.; Ahmad, J.; Shah, S.A.; Morison, G.; Skelton, D.A.; Larijani, H.; Abbasi, Q.H.; Imran, M.A.; Gibson, R.M. WiFreeze: Multiresolution Scalograms for Freezing of Gait Detection in Parkinson’s Leveraging 5G Spectrum with Deep Learning. Electronics 2019, 8, 1433. [Google Scholar] [CrossRef]
- Little, B.; Alshabrawy, O.; Stow, D.; Ferrier, I.N.; McNaney, R.; Jackson, D.G.; Ladha, K.; Ladha, C.; Ploetz, T.; Bacardit, J.; et al. Deep learning-based automated speech detection as a marker of social functioning in late-life depression. Psychol. Med. 2021, 51, 1441–1450. [Google Scholar] [CrossRef]
- Młyńczak, M.; Migacz, E.; Migacz, M.; Kukwa, W. Detecting Breathing and Snoring Episodes Using a Wireless Tracheal Sensor—A Feasibility Study. IEEE J. Biomed. Health Inform. 2017, 21, 1504–1510. [Google Scholar] [CrossRef]
- Nguyen, A.; Pogoncheff, G.; Dong, B.X.; Bui, N.; Truong, H.; Pham, N.; Nguyen, L.; Nguyen-Huu, H.; Bui-Diem, K.; Vu-Tran-Thien, Q.; et al. A comprehensive study on the efficacy of a wearable sleep aid device featuring closed-loop real-time acoustic stimulation. Sci. Rep. 2023, 13, 17515. [Google Scholar] [CrossRef]
- Kwon, H.B.; Choi, S.H.; Lee, D.; Son, D.; Yoon, H.; Lee, M.H.; Lee, Y.J.; Park, K.S. Attention-Based LSTM for Non-Contact Sleep Stage Classification Using IR-UWB Radar. IEEE J. Biomed. Health Inform. 2021, 25, 3844–3853. [Google Scholar] [CrossRef]
- Gu, Y.; Zhang, Y.; Li, J.; Ji, Y.; An, X.; Ren, F. Sleepy: Wireless Channel Data Driven Sleep Monitoring via Commodity WiFi Devices. IEEE Trans. Big Data 2020, 6, 258–268. [Google Scholar] [CrossRef]
- Ren, Y.; Wang, C.; Chen, Y.; Yang, J.; Li, H. Noninvasive Fine-Grained Sleep Monitoring Leveraging Smartphones. IEEE Internet Things J. 2019, 6, 8248–8261. [Google Scholar] [CrossRef]
- Gui, L.; Ma, C.; Sheng, B.; Guo, Z.; Cai, J.; Xiao, F. In-Home Monitoring Sleep Turnover Activities and Breath Rate via WiFi Signals. IEEE Syst. J. 2023, 17, 2355–2365. [Google Scholar] [CrossRef]
- Yu, B.; Wang, Y.; Niu, K.; Zeng, Y.; Gu, T.; Wang, L.; Guan, C.; Zhang, D. WiFi-Sleep: Sleep Stage Monitoring Using Commodity Wi-Fi Devices. IEEE Internet Things J. 2021, 8, 13900–13913. [Google Scholar] [CrossRef]
- Rossi, M.; Sala, D.; Bovio, D.; Salito, C.; Alessandrelli, G.; Lombardi, C.; Mainardi, L.; Cerveri, P. SLEEP-SEE-THROUGH: Explainable Deep Learning for Sleep Event Detection and Quantification From Wearable Somnography. IEEE J. Biomed. Health Inform. 2023, 27, 3129–3140. [Google Scholar] [CrossRef]
- Shinmoto Torres, R.L.; Visvanathan, R.; Abbott, D.; Hill, K.D.; Ranasinghe, D.C. A battery-less and wireless wearable sensor system for identifying bed and chair exits in a pilot trial in hospitalized older people. PLoS ONE 2017, 12, e0185670. [Google Scholar] [CrossRef]
- Taylor, W.; Dashtipour, K.; Shah, S.A.; Hussain, A.; Abbasi, Q.H.; Imran, M.A. Radar Sensing for Activity Classification in Elderly People Exploiting Micro-Doppler Signatures Using Machine Learning. Sensors 2021, 21, 3881. [Google Scholar] [CrossRef]
- Garripoli, C.; Mercuri, M.; Karsmakers, P.; Soh, P.J.; Crupi, G.; Vandenbosch, G.A.; Pace, C.; Leroux, P.; Schreurs, D. Embedded DSP-based telehealth radar system for remote in-door fall detection. IEEE J. Biomed. Health Inform. 2015, 19, 92–101. [Google Scholar] [CrossRef]
- Wang, C.; Tang, L.; Zhou, M.; Ding, Y.; Zhuang, X.; Wu, J. Indoor Human Fall Detection Algorithm Based on Wireless Sensing. Tsinghua Sci. Technol. 2022, 27, 1002–1015. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, K.; Ni, L.M. WiFall: Device-Free Fall Detection by Wireless Networks. IEEE Trans. Mob. Comput. 2017, 16, 581–594. [Google Scholar] [CrossRef]
- Mercuri, M.; Soh, P.J.; Mehrjouseresht, P.; Crupi, F.; Schreurs, D. Biomedical Radar System for Real-Time Contactless Fall Detection and Indoor Localization. IEEE J. Electromagn. RF Microw. Med. Biol. 2023, 7, 303–312. [Google Scholar] [CrossRef]
- Chu, Y.; Cumanan, K.; Sankarpandi, S.K.; Smith, S.; Dobre, O.A. Deep Learning-Based Fall Detection Using WiFi Channel State Information. IEEE Access 2023, 11, 83763–83780. [Google Scholar] [CrossRef]
- Ding, J.; Wang, Y. A WiFi-Based Smart Home Fall Detection System Using Recurrent Neural Network. IEEE Trans. Consum. Electron. 2020, 66, 308–317. [Google Scholar] [CrossRef]
- He, J.; Zhu, W.; Qiu, L.; Zhang, Q.; Wang, C. An indoor fall detection system based on WiFi signals and genetic algorithm optimized random forest. Wirel. Netw. 2024, 30, 1753–1771. [Google Scholar] [CrossRef]
- Gu, Z.; He, T.; Wang, Z.; Xu, Y. Device-Free Human Activity Recognition Based on Dual-Channel Transformer Using WiFi Signals. Wirel. Commun. Mob. Comput. 2022, 2022, 4598460. [Google Scholar] [CrossRef]
- Xia, Z.; Chong, S. WiFi-based indoor passive fall detection for medical Internet of Things. Comput. Electr. Eng. 2023, 109, 108763. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, X.; Li, S.; Xie, Y.; Li, Y.; Wang, X.; Zhang, D. LT-Fall: The Design and Implementation of a Life-threatening Fall Detection and Alarming System. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2023, 7, 40. [Google Scholar] [CrossRef]
- Sun, Y.; Cano-Garcia, H.; Kallos, E.; O’Brien, F.; Akintonde, A.; Motei, D.E.; Ancu, O.; Mackenzie, R.W.A.; Kosmas, P. Random Forest Analysis of Combined Millimeter-Wave and Near-Infrared Sensing for Noninvasive Glucose Detection. IEEE Sens. J. 2023, 23, 20294–20309. [Google Scholar] [CrossRef]
- Kalasin, S.; Sangnuang, P.; Surareungchai, W. Intelligent Wearable Sensors Interconnected with Advanced Wound Dressing Bandages for Contactless Chronic Skin Monitoring: Artificial Intelligence for Predicting Tissue Regeneration. Anal. Chem. 2022, 94, 6842–6852. [Google Scholar] [CrossRef]
- Park, J.H.; Park, I.; Han, K.; Yoon, J.; Sim, Y.; Kim, S.J.; Won, J.Y.; Lee, S.; Kwon, J.H.; Moon, S.; et al. Feasibility of Deep Learning-Based Analysis of Auscultation for Screening Significant Stenosis of Native Arteriovenous Fistula for Hemodialysis Requiring Angioplasty. Korean J. Radiol. 2022, 23, 949–958. [Google Scholar] [CrossRef]
- Parati, M.; Gallotta, M.; Muletti, M.; Pirola, A.; Bellafà, A.; De Maria, B.; Ferrante, S. Validation of Pressure-Sensing Insoles in Patients with Parkinson’s Disease during Overground Walking in Single and Cognitive Dual-Task Conditions. Sensors 2022, 22, 6392. [Google Scholar] [CrossRef] [PubMed]
- Schlachetzki, J.C.M.; Barth, J.; Marxreiter, F.; Gossler, J.; Kohl, Z.; Reinfelder, S.; Gassner, H.; Aminian, K.; Eskofier, B.M.; Winkler, J.; et al. Wearable sensors objectively measure gait parameters in Parkinson’s disease. PLoS ONE 2017, 12, e0183989. [Google Scholar] [CrossRef]
- Yen, J.M.; Lim, J.H. A Clinical Perspective on Bespoke Sensing Mechanisms for Remote Monitoring and Rehabilitation of Neurological Diseases: Scoping Review. Sensors 2023, 23, 536. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef] [PubMed]
- Appeadu, M.K.; Bordoni, B. Falls and Fall Prevention in Older Adults; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Oliver, D.; Papaioannou, A.; Giangregorio, L.; Thabane, L.; Reizgys, K.; Foster, G. A systematic review and meta-analysis of studies using the STRATIFY tool for prediction of falls in hospital patients: How well does it work? Age Ageing 2008, 37, 621–627. [Google Scholar] [CrossRef]
- Van Norman, G.A. Decentralized Clinical Trials: The Future of Medical Product Development? JACC Basic Transl. Sci. 2021, 6, 384–387. [Google Scholar] [CrossRef]
- Turbow, S.; Hollberg, J.R.; Ali, M.K. Electronic Health Record Interoperability: How Did We Get Here and How Do We Move Forward? JAMA Health Forum 2021, 2, e210253. [Google Scholar] [CrossRef]
- Ali, A.; Shaukat, H.; Bibi, S.; Altabey, W.A.; Noori, M.; Kouritem, S.A. Recent progress in energy harvesting systems for wearable technology. Energy Strategy Rev. 2023, 49, 101124. [Google Scholar] [CrossRef]
- Godawatte, K.; Branch, P.; But, J. Use of blockchain in health sensor networks to secure information integrity and accountability. Procedia Comput. Sci. 2022, 210, 124–132. [Google Scholar] [CrossRef]
- Upadrista, V.; Nazir, S.; Tianfield, H. Secure data sharing with blockchain for remote health monitoring applications: A review. J. Reliab. Intell. Environ. 2023, 9, 349–368. [Google Scholar] [CrossRef]
- Das, S.; Mazumdar, H.; Khondakar, K.R.; Mishra, Y.K.; Kaushik, A. Review—Quantum Biosensors: Principles and Applications in Medical Diagnostics. ECS Sens. Plus 2024, 3, 025001. [Google Scholar] [CrossRef]
- Aslam, N.; Zhou, H.; Urbach, E.K.; Turner, M.J.; Walsworth, R.L.; Lukin, M.D.; Park, H. Quantum sensors for biomedical applications. Nat. Rev. Phys. 2023, 5, 157–169. [Google Scholar] [CrossRef]
- Chataut, R.; Nankya, M.; Akl, R. 6G Networks and the AI Revolution-Exploring Technologies, Applications, and Emerging Challenges. Sensors 2024, 24, 1888. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.R.; Singh, V.K.; Yadav, R.; Chaurasia, S.N. 6G networks for artificial intelligence-enabled smart cities applications: A scoping review. Telemat. Inform. Rep. 2023, 9, 100044. [Google Scholar] [CrossRef]

| Sensing Techniques | Sensing Features | Pros | Cons | |
|---|---|---|---|---|
| Radar | Continuous wave (CW), frequency-modulated continuous wave (FMCW), impulse radio ultra-wideband (IR-UWB) | Doppler shift Phase Distance | Large bandwidth; directional performance | High cost |
| CSI | WiFi orthogonal frequency division multiplexing (OFDM) | CSI amplitude CSI phase | High CSI resolution; ubiquitousness | Susceptible to environmental influence |
| RFID | CW | RFID phase | Directional performance; low cost | Channel hopping |
| Acoustic | CW FMCW OFDM | Acoustic phase Acoustic distance | High resolution | Susceptible to the environment; small coverage |
| Article | Year | Purpose | Level of Research Data | Wireless Sensing Type | Subject Number | Subject Type | AI Algorithm | Outcomes of the Model | |
|---|---|---|---|---|---|---|---|---|---|
| Cardiopulmonary | Arjoune et al. [22] | 2023 | Detecting Still’s murmur and wheezes | Clinical validation | Acoustic | 120+ | Patients | DL | Still’s murmur—sensitivity 91.9%, specificity 92.6%, overall accuracy 92.2% Wheeze detection—sensitivity 83.7%, specificity 84.4%, overall accuracy 84.0% |
| Howard-Quijano et al. [23] | 2023 | Measuring left ventricular ejection fraction | Clinical validation | Acoustic | 81 (63 with cardiac pathology) | Patients and controls | DL and traditional ML | AUC 0.974 for detecting EF < 35% AUC 0.916 for detecting EF < 50% | |
| Lalouani et al. [24] | 2022 | Detecting breathing anomalies and COPD | Dataset analysis and conceptual validation | Acoustic | 128 (64 with COPD) (from dataset) | Patients and controls | DL | Precision 0.97, recall 1.0, F1-score 0.98, accuracy 0.98 for patients with COPD (exact values not given, inferred from Figure 7 [24]) | |
| Al-Momani and Garaibeh [25] | 2014 | Detecting and classifying asthma attacks | Clinical validation | Acoustic | 18 patients (hospital); 144 controls (dataset) | Patients and controls | Traditional ML | Maximum probability of correct classification of 90% at signal-to-noise ratio (SNR) = 16 dB for SVM classifier and 86% at SNR = 17 dB for HMM classifier. | |
| Tseng et al. [26] | 2016 | Classifying normal and abnormal respiratory function | Clinical validation | Radar | 50 (32 with “bad” respiratory function) | Participants with abnormal respiratory function and controls | Traditional ML | Classification accuracy 73.3% | |
| Zhang et al. [27] | 2022 | Detecting myocardial infarction | Clinical validation | Radar | 60 (30 patients, 30 healthy) | Patients with controls | Traditional ML | Median detection accuracy of 66.5% when users are not stationary, and 81.2% when the users are stationary. | |
| Huang et al. [28] | 2023 | Diagnosing and prognosticating pediatric community-acquired pneumonia (CAP) | Clinical validation | Acoustic | 198 (all with CAP) | Patients | DL | Subject-dependent setting: accuracy 97.3% for CAP diagnosis, 97.16% for CAP prognosis (sensitivity, specificity >96% for both diagnosis and prognosis) Subject-independent setting: accuracy 60.50% for CAP diagnosis, 42.18% for CAP prognosis (sensitivity, specificity >50% for CAP diagnosis and >39% for CAP prognosis) | |
| Neurology/Psychology | Van de Vel et al. [29] | 2016 | Detecting tonicclonic and clonic seizures | Pilot patient study | Radar | 2 | Patients | Traditional ML | Mean sensitivity of 66.87% and false detection rate of 1.16/night. |
| O’Brien et al. [30] | 2021 | Classifying dysphagia severity | Conceptual validation | Mechano-acoustic sensor | 19 (9 patients and 10 controls) | Patients and controls | Traditional ML | Average predictive probability of 52.8% for mild severity, 53.8% for moderate severity. | |
| Verde et al. [31] | 2019 | Classifying healthy and pathological voices | Dataset analysis and conceptual validation | Acoustic | Combined voice sample datasets (796 healthy and 1207 pathological) | Traditional ML | Sensitivity 82.9%, specificity 86.2%, precision 85.7%, F-measure 84.3%, AUC 0.91, accuracy 84.5% | ||
| Tahir et al. [32] | 2019 | Detecting Parkinson’s freezing of gait (FOG) | Clinical validation | WiFi CSI | 15 | Patients | DL | Highest accuracy of 99.7% for FOG detection; 94.3% for voluntary stop, 97.6% for walking slow | |
| Little et al. [33] | 2021 | Detecting speech as a marker of social functioning in late-life depression | Feasibility and validation study | Acoustic | 58 (29 patients and 29 controls) | Patients and matched controls | DL | Sensitivity 94.6%, specificity 87.4%, 93.8% accuracy for speech detection Sensitivity 90.3%, specificity 86.2%, accuracy 89.95% for wearer vs non-wearer speech detection | |
| Sleep Medicine | Mlynczak et al. [34] | 2017 | Classifying normal and snoring episodes | Conceptual validation | Acoustic | 16 | Healthy volunteers | DL | Accuracy 88.8%, Cohen’s kappa 0.7775, specificity 95.0%, sensitivity 76.8%, F1-score 82.4% |
| Nguyen et al. [35] | 2023 | Monitoring sleep and producing auditory stimulation for sleep quality | Clinical validation and separate pilot patient study | Acoustic | 377 | Healthy volunteers | DL | Averaged accuracy of sleep scoring 84.08 ± 1.42% Strong correlation of 0.89 ± 0.03 with gold-standard PSG 87.8% agreement of sleep stage scoring with sleep technicians. Shortens duration of falling asleep by 24.1 min | |
| Kwon et al. [36] | 2021 | Classifying sleep stage | Clinical validation | Radar | 65 | Healthy volunteers | DL | Accuracy 82.6 ± 6.7%, Cohen’s kappa coefficient 0.73 ± 0.11 | |
| Gu et al. [37] | 2020 | Monitoring sleep | Clinical validation | WiFi RSS and CSI | 7 | Healthy volunteers | Traditional ML | Short-term controlled experiments–detection accuracy 95.65%, false negative rate 2.16% 60 min real sleep studies–detection accuracy 98.22%, false negative rate 0% | |
| Ren et al. [38] | 2019 | Monitoring sleep and detect apnea | Conceptual validation | Acoustic | 9 | Healthy volunteers | Traditional ML | N/A (for sleep apnea). For different sleep events, TP around 80–90% and FP less than 10% (exact values are not given, inferred from Figure 16 [38]). | |
| Gui et al. [39] | 2022 | Monitoring sleep turnover activities and breathing rate | Conceptual validation | WiFi CSI | 15 | Healthy volunteers | DL | Mean accuracy 94.59% for turnover activities; 95.83% for sleep posture | |
| Yu et al. [40] | 2021 | Monitoring and classifying sleep stage | Clinical validation | WiFi CSI | 12 | Healthy volunteers | DL | Accuracy 81.8% | |
| Rossi et al. [41] | 2023 | Detecting sleep events | Conceptual validation | Acoustic | 20 | Healthy volunteers | DL | Classification accuracy of 97% for sleep apnea and 73% for snoring | |
| Fall Detection | Torres et al. [42] | 2017 | Detecting bed and chair exits in hospital rooms | Clinical validation | RFID | 26 | Geriatric patients | Traditional ML | Overall recall 81.4%, precision 66.8% and F1-score 72.4% |
| Taylor et al. [43] | 2021 | Classifying six human activities (walking, sitting, standing, picking up objects, drinking water, and falling) | Dataset analysis and conceptual validation | Radar | 99 (from a dataset) | Healthy, elderly volunteers | DL and traditional ML | Accuracy 95.3% for the best performing model | |
| Garripoli et al. [44] | 2015 | Detecting real-time fall events and classifying movement | Conceptual validation | Radar | 16 | Healthy volunteers | Traditional ML | Sensitivity 100%, no false positives | |
| Wang et al. [45] | 2022 | Fall Detection | Conceptual validation | WiFi CSI | 4 | Healthy volunteers | Traditional ML | SVM—average classification accuracy 91.67% XGB—average classification accuracy 90.00% | |
| Wang et al. [46] | 2017 | Fall Detection | Conceptual validation | WiFi CSI | 10 | Healthy volunteers | Traditional ML | SVM: average detection precision 90%, average false alarm rate 15% Random forest—average detection precision 94%, average false alarm rate 13% | |
| Mercuri et al. [47] | 2023 | Detecting and localizing falls | Conceptual validation | Radar | 6 | Healthy volunteers | Traditional ML | No false positives or false negatives (TP: 40, FP: 0, TN: 117000, FN: 0) for fall detection Maximum mean absolute errors of 3.8 cm and maximum root-mean-square error of 7.5 cm (for measuring person’s absolute distance) | |
| Chu et al. [48] | 2023 | Fall Detection | Conceptual validation | WiFi CSI | 22 | Healthy volunteers | DL | Accuracy > 96% accuracy in all lab environments | |
| Ding and Wang [49] | 2020 | Fall Detection | Conceptual validation | WiFi CSI | 10 | Healthy volunteers | DL | Recognition accuracies of 90%, 91%, and 93% in indoor environments (laboratory, office, dormitory, respectively) | |
| He et al. [50] | 2024 | Fall Detection | Dataset analysis and conceptual validation | WiFi CSI | DARMS dataset (21 volunteers) [51] | Traditional ML | Accuracy of >95.25% | ||
| Xia and Chong [52] | 2023 | Fall Detection | Conceptual validation | WiFi CSI | 3 | Healthy volunteers | DL | Accuracy, precision, and F1-score of 92% for detecting falls. | |
| Zhang et al. [53] | 2023 | Fall Detection | Conceptual validation | Radar | 15 | Healthy volunteers | Traditional ML | Recall 98.8%, precision 100%, false discovery rate (FDR) 0%, F1-score 0.994 | |
| Endocrinology | Sun et al. [54] | 2023 | Monitoring glucose levels | Clinical validation | RF near-infrared spectrometry | 5 | Healthy volunteers | Traditional ML | Root mean square error 21.06 mg/dL, mean absolute relative difference 7.31% for glucose prediction (compared to glucometer values). |
| Dermatology | Kalasin et al. [55] | 2022 | Classifying wound healing stages | Conceptual validation | RFID | 10 | Patients with inflamed skin | DL | Classification accuracy 94.6% |
| Nephrology | Park et al. [56] | 2022 | Predicting significant stenosis of arteriovenous fistulas | Clinical validation | Acoustic | 40 | Patients | DL | AUROC 0.98 for EfficientNetB5 and 0.99 for Resnet50 for predicting ≥50% AVF stenosis. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toruner, M.D.; Shi, V.; Sollee, J.; Hsu, W.-C.; Yu, G.; Dai, Y.-W.; Merlo, C.; Suresh, K.; Jiao, Z.; Wang, X.; et al. Artificial Intelligence-Driven Wireless Sensing for Health Management. Bioengineering 2025, 12, 244. https://doi.org/10.3390/bioengineering12030244
Toruner MD, Shi V, Sollee J, Hsu W-C, Yu G, Dai Y-W, Merlo C, Suresh K, Jiao Z, Wang X, et al. Artificial Intelligence-Driven Wireless Sensing for Health Management. Bioengineering. 2025; 12(3):244. https://doi.org/10.3390/bioengineering12030244
Chicago/Turabian StyleToruner, Merih Deniz, Victoria Shi, John Sollee, Wen-Chi Hsu, Guangdi Yu, Yu-Wei Dai, Christian Merlo, Karthik Suresh, Zhicheng Jiao, Xuyu Wang, and et al. 2025. "Artificial Intelligence-Driven Wireless Sensing for Health Management" Bioengineering 12, no. 3: 244. https://doi.org/10.3390/bioengineering12030244
APA StyleToruner, M. D., Shi, V., Sollee, J., Hsu, W.-C., Yu, G., Dai, Y.-W., Merlo, C., Suresh, K., Jiao, Z., Wang, X., Mao, S., & Bai, H. (2025). Artificial Intelligence-Driven Wireless Sensing for Health Management. Bioengineering, 12(3), 244. https://doi.org/10.3390/bioengineering12030244






