Evolution of CPITN Index in Relation to Chlorhexidine Mouthwash Use in Patients with Deflective Occlusal Contacts
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Academy of Prosthodontics. The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar] [CrossRef] [PubMed]
- Furman, E. Association Between Dental Trauma and Periodontal Disease; IntechOpen Publisher: London, UK, 2024. [Google Scholar] [CrossRef]
- American Academy of Periodontology. Parameter on Occlusal Traumatism in Patients With Chronic Periodontitis. J. Periodontol. 2000, 71, 873–875. [Google Scholar] [CrossRef]
- Passanezi, E.; Sant’Ana, A.C.P. Role of occlusion in periodontal disease. Periodontology 2000 2019, 79, 129–150. [Google Scholar] [CrossRef]
- Lang, N.P.; Bartold, P.M. Periodontal health. J. Periodontol. 2018, 89, S9–S16. [Google Scholar] [CrossRef] [PubMed]
- Sanadi, R.M.; Chelani, L.R.; Bhakkand, S.R.; Sheth, J.K. Role of trauma from occlusion in periodontal disease-A controversy. IOSR J. Dent. Med. Sci. (IOSR-JDMS) 2016, 15, 118–122. [Google Scholar] [CrossRef]
- Nirola, A.; Batra, P.; Mohindra, K.; Kaur, T. Role of Occlusion as a Risk Factor in Periodontal Disease. J. Int. Clin. Dent. Res. Org. 2020, 12, 102–109. [Google Scholar] [CrossRef]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S.; EFP Workshop Participants and Methodological Consultants. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47, 4–60. [Google Scholar] [CrossRef]
- Fan, J.; Caton, J.G. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J. Clin. Periodontol. 2018, 45, S199–S206. [Google Scholar] [CrossRef]
- Hugar, S.S.; Patil, S.; Metgud, R.; Nanjwade, B.; Hugar, S.M. Influence of application of chlorhexidine gel and curcumin gel as an adjunct to scaling and root planing: A interventional study. J. Nat. Sci. Biol. Med. 2016, 7, 149–154. [Google Scholar] [CrossRef]
- Brookes, Z.L.S.; Bescos, R.; Belfield, L.A.; Ali, K.; Roberts, A. Current uses of chlorhexidine for management of oral disease: A narrative review. J. Dent. 2020, 103, 103497. [Google Scholar] [CrossRef]
- Chye, R.M.L.; Perrotti, V.; Piattelli, A.; Iaculli, F.; Quaranta, A. Effectiveness of Different Commercial Chlorhexidine-Based Mouthwashes after Periodontal and Implant Surgery: A Systematic Review. Implant Dent. 2019, 28, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Poppolo Deus, F.; Ouanounou, A. Chlorhexidine in Dentistry: Pharmacology, Uses, and Adverse Effects. Int. Dent. J. 2022, 72, 269–277. [Google Scholar] [CrossRef]
- Dumitriu, A.S.; Păunică, S.; Nicolae, X.A.; Bodnar, D.C.; Albu Ștefan, D.; Suciu, I.; Ciongaru, D.N.; Giurgiu, M.C. The Effectiveness of the Association of Chlorhexidine with Mechanical Treatment of Peri-Implant Mucositis. Healthcare 2023, 11, 1918. [Google Scholar] [CrossRef]
- Kaur, S.; Kour, K. Short term side effects of 0.2% and 0.12% chlorhexidine mouthwash. IP Int. J. Periodontol. Implantol. 2020, 4, 138–140. [Google Scholar] [CrossRef]
- Nicolae, X.A.; Preoteasa, E.; Murariu Magureanu, C.; Preoteasa, C.T. Cross-Sectional Study of Occlusal Loading and Periodontal Status of Teeth with Deflective Occlusal Contacts. Bioengineering 2025, 12, 766. [Google Scholar] [CrossRef]
- Miçooğulları Kurt, S.; Çalışkan, M.K. Efficacy of chlorhexidine as a final irrigant in one-visit root canal treatment: A prospective comparative study. Int. Endod. J. 2018, 51, 1069–1076. [Google Scholar] [CrossRef]
- Santos, V.R.; Lima, J.A.; Miranda, T.S.; Gonçalves, T.E.D.; Figueiredo, L.C.; Faveri, M.; Duarte, P.M. Full-mouth disinfection as a therapeutic protocol for type-2 diabetic subjects with chronic periodontitis: Twelve-month clinical outcomes. A randomized controlled clinical trial. J. Clin. Periodontol. 2013, 40, 155–162. [Google Scholar] [CrossRef]
- Sahm, N.; Becker, J.; Santel, T.; Schwarz, F. Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: A prospective, randomized, controlled clinical study. J. Clin. Periodontol. 2011, 38, 872–878. [Google Scholar] [CrossRef]
- Boyapati, R.; Peeta, J.; Dhulipalla, R.; Kolaparthy, L.; Adurty, C.; Cheruvu, R.N.S. Comparative evaluation of the efficacy of probiotic, Aloe vera, povidine-iodine, and chlorhexidine mouthwashes in the treatment of gingival inflammation: A randomized controlled trial. Dent. Med. Probl. 2024, 61, 181–190. [Google Scholar] [CrossRef]
- Haydari, M.; Bardakci, A.G.; Koldsland, O.C.; Aass, A.M.; Sandvik, L.; Preus, H.R. Comparing the effect of 0.06%-, 0.12% and 0.2% Chlorhexidine on plaque, bleeding and side effects in an experimental gingivitis model: A parallel group, double masked randomized clinical trial. BMC Oral Health 2017, 17, 118. [Google Scholar] [CrossRef] [PubMed]
- Genovesi, A.; Barone, A.; Toti, P.; Covani, U. The efficacy of 0.12% chlorhexidine versus 0.12% chlorhexidine plus hyaluronic acid mouthwash on healing of submerged single implant insertion areas: A short-term randomized controlled clinical trial. Int. J. Dent. Hyg. 2017, 15, 65–72. [Google Scholar] [CrossRef]
- Vitiello, F.; Monterubbianesi, R.; Sparabombe, S.; Bourgeois, D.; Tosco, V.; Alshehri, F.A.; Carrouel, F.; Putignano, A.; Orsini, G. Use of over-the-counter mouthwashes as an additional measure in individual oral prophylaxis on adults with plaque-induced gingivitis: A double-blind, parallel, randomized controlled trial. BMC Oral Health 2024, 24, 83. [Google Scholar] [CrossRef]
- Talebi Ardakani, M.; Farahi, A.; Mojab, F.; Moscowchi, A.; Gharazi, Z. Effect of an herbal mouthwash on periodontal indices in patients with plaque-induced gingivitis: A cross-over clinical trial. J. Adv. Periodontol. Implant Dent. 2022, 14, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Deepika, B.; Ramamurthy, J. Evaluation of occlusal pattern in periodontitis patients using T-scan analysis. J. Adv. Pharm. Technol. Res. 2022, 13, 265–271. [Google Scholar] [CrossRef]
- Nalini, M.S.; Sinha, M.; Thumati, P.; Raghunath, A. Evaluation of the Effect of Occlusal Calibration in Periodontitis Patients with Occlusal Trauma Using T-Scan. Indian. J. Dent. Res. 2024, 35, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Tanık, A.; Gül, M. The validity of the Community Periodontal Index of Treatment Needs (CPITN) in epidemiological studies of periodontal diseases. Int. Dent. Res. 2020, 10, 44–48. [Google Scholar] [CrossRef]
- James, P.; Worthington, H.V.; Parnell, C.; Harding, M.; Lamont, T.; Cheung, A.; Whelton, H.; Riley, P. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst. Rev. 2017, 3, CD008676. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, M.Y.; Al-Zawawi, A.S.; Divakar, D.D.; Aldulaijan, H.A.; Basudan, A.M. Role of Chlorhexidine and Herbal Oral Rinses in Managing Periodontitis. Int. Dent. J. 2023, 73, 235–242. [Google Scholar] [CrossRef]
- Ozmeric, N.; Enver, A.; Isler, S.C.; Gökmenoğlu, C.; Topaloğlu, M.; Selamet, H.; Altun, G.; Sayar, S.A. Evaluating the effects of chlorhexidine and vitamin c mouthwash on oral health in non-surgical periodontal therapy: A randomized controlled clinical trial. Sci. Rep. 2025, 15, 3703. [Google Scholar] [CrossRef]
- Vangipuram, S.; Jha, A.; Bhashyam, M. Comparative efficacy of aloe vera mouthwash and chlorhexidine on periodontal health: A randomized controlled trial. J. Clin. Exp. Dent. 2016, 18, 442–447. [Google Scholar] [CrossRef]
- Sun, H.; Chen, S.; Yang, C.; Kuang, H.; Huang, Y.; He, X.; Luo, W. Advances in the use of chlorhexidine for periodontitis treatment in diabetic patients: A review. Medicine 2024, 103, e39627. [Google Scholar] [CrossRef] [PubMed]
- Brookes, Z.L.S.; McCullough, M.; Kumar, P.; McGrath, C. Mouthwashes: Implications for Practice. Int. Dent. J. 2023, 73, S98–S101. [Google Scholar] [CrossRef]
- Sharma, K.; Madan, E.; Nirwal, A.; Fatima, Z. Comparative Evaluation of Efficacy of Chitosan and Chlorhexidine Mouthwash in Plaque Control and Gingivitis: An Observational Study. Cureus 2024, 16, e70810. [Google Scholar] [CrossRef]
- Carpenter, G.H.; Pramanik, R.; Proctor, G.B. An in vitro model of chlorhexidine-induced tooth staining. J. Periodontal Res. 2005, 40, 225–230. [Google Scholar] [CrossRef]
- Done, A.E.; Preoteasa, E.; Preoteasa, C.T. Psychometric Assessment of the Romanian Version of the Index of Dental Anxiety and Fear (IDAF-4C+). Healthcare 2023, 11, 2129. [Google Scholar] [CrossRef]
- Cho, Y.D.; Kim, S.; Koo, K.T.; Seol, Y.J.; Lee, Y.M.; Rhyu, I.C.; Ku, Y. Rescue of a periodontally compromised tooth by non-surgical treatment: A case report. J. Periodontal Implant Sci. 2016, 46, 128–134. [Google Scholar] [CrossRef]
- Persson, R.; Svendsen, J.; Daubert, K. A longitudinal evaluation of periodontal therapy using the CPITN index. J. Clin. Periodontol. 1989, 16, 569–574. [Google Scholar] [CrossRef]
- Muthukumar, S.; Suresh, R. Community periodontal index of treatment needs index: An indicator of anaerobic periodontal infection. Indian. J. Dent. Res. 2009, 20, 423–425. [Google Scholar] [CrossRef]
- Teodorescu, I.M.; Preoteasa, E.; Preoteasa, C.T.; Murariu-Măgureanu, C.; Teodorescu, C. Association of Systemic Pathologies on Dental, Periodontal and Orthodontic Status in Children. Biomedicines 2025, 13, 2137. [Google Scholar] [CrossRef] [PubMed]
- Könönen, E.; Gursoy, M.; Gursoy, U.K. Periodontitis: A multifaceted disease of tooth-supporting tissues. J. Clin. Med. 2019, 8, 1135. [Google Scholar] [CrossRef] [PubMed]
- Annisa, Z.U.; Sulijaya, B.; Tadjoedin, E.S.S.; Hutomo, D.I.; Masulili, S.L.C. Effectiveness of chlorhexidine gels and chips in Periodontitis Patients after Scaling and Root Planing: A systematic review and Meta-analysis. BMC Oral Health 2023, 23, 819. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Gallo, S.; Pascadopoli, M.; Frani, M.; Butera, A. Ozonized gels vs. chlorhexidine in non-surgical periodontal treatment: A randomized clinical trial. Oral Dis. 2024, 30, 3993–4000. [Google Scholar] [CrossRef] [PubMed]
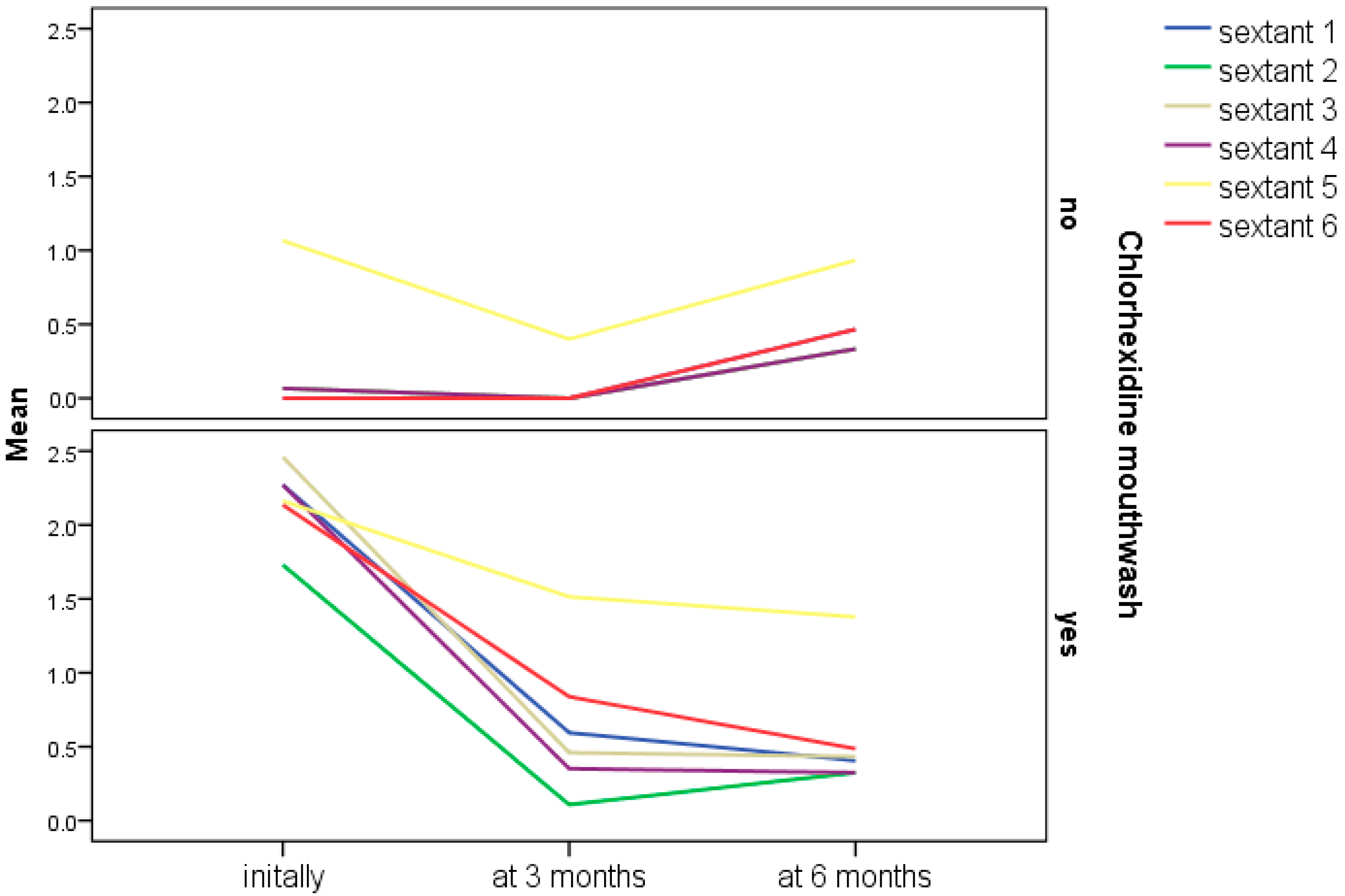
| p-Value for CPITN Values During Follow-Up | CHX (n = 37) | Without CHX (n = 15) |
|---|---|---|
| Sextant 1 | <0.001 | 0.135 |
| Sextant 2 | <0.001 | 0.607 |
| Sextant 3 | <0.001 | 0.368 |
| Sextant 4 | <0.001 | 0.368 |
| Sextant 5 | 0.007 | 0.206 |
| Sextant 6 | <0.001 | 0.135 |
| Total score | <0.001 | 0.135 |
| Friedman Test | ||
| CPITN | |||||||
|---|---|---|---|---|---|---|---|
| At 3 Months from Baseline | At 6 Months from Baseline | ||||||
| CHX n (%) | Without CHX n (%) | p | CHX n (%) | Without CHX n (%) | p | ||
| Sextant 1 | improved | 30 (81.1) | 0 (0) | <0.001 | 8 (21.6) | 0 (0) | 0.089 |
| unchanged | 7 (18.9) | 15 (100) | 27 (73) | 13 (86.7) | |||
| worsened | 0 (0) | 0 (0) | 2 (5.4) | 2 (13.3) | |||
| Sextant 2 | improved | 30 (81.1) | 1 (6.7) | <0.001 | 2 (5.4) | 0 (0) | >0.999 |
| unchanged | 7 (18.9) | 14 (93.3) | 32 (86.5) | 14 (93.3) | |||
| worsened | 0 (0) | 0 (0) | 3 (8.1) | 1 (6.7) | |||
| Sextant 3 | improved | 31 (83.8) | 1 (6.7) | <0.001 | 6 (16.2) | 0 (0) | 0.207 |
| unchanged | 6 (16.2) | 14 (93.3) | 29 (78.4) | 14 (93.3) | |||
| worsened | 0 (0) | 0 (0) | 2 (5.4) | 1 (6.7) | |||
| Sextant 4 | improved | 31 (83.8) | 1 (6.7) | <0.001 | 5 (13.5) | 0 (0) | 0.441 |
| unchanged | 6 (16.2) | 14 (93.3) | 30 (81.1) | 14 (93.3) | |||
| worsened | 0 (0) | 0 (0) | 2 (5.4) | 1 (6.7) | |||
| Sextant 5 | improved | 16 (42.2) | 6 (40) | 0.758 | 9 (24.3) | 2 (13.3) | 0.336 |
| unchanged | 16 (42.2) | 8 (53.3) | 24 (64.9) | 9 (60) | |||
| worsened | 5 (13.5) | 1 (6.7) | 4 (10.8) | 4 (26.7) | |||
| Sextant 6 | improved | 27 (73.0) | 0 (0) | <0.001 | 10 (27) | 0 (0) | 0.029 |
| unchanged | 10 (27.0) | 15 (100) | 25 (67.6) | 13 (86.7) | |||
| worsened | 0 (0) | 0 (0) | 2 (5.4) | 2 (13.3) | |||
| Total | improved | 32 (86.5) | 7 (46.7) | 0.004 | 22 (59.5) | 2 (13.3) | 0.007 |
| unchanged | 3 (8.1) | 7 (46.7) | 10 (27) | 9 (60) | |||
| worsened | 2 (5.4) | 1 (6.7) | 5 (13.5) | 4 (26.7) | |||
| Fisher‘s exact test | |||||||
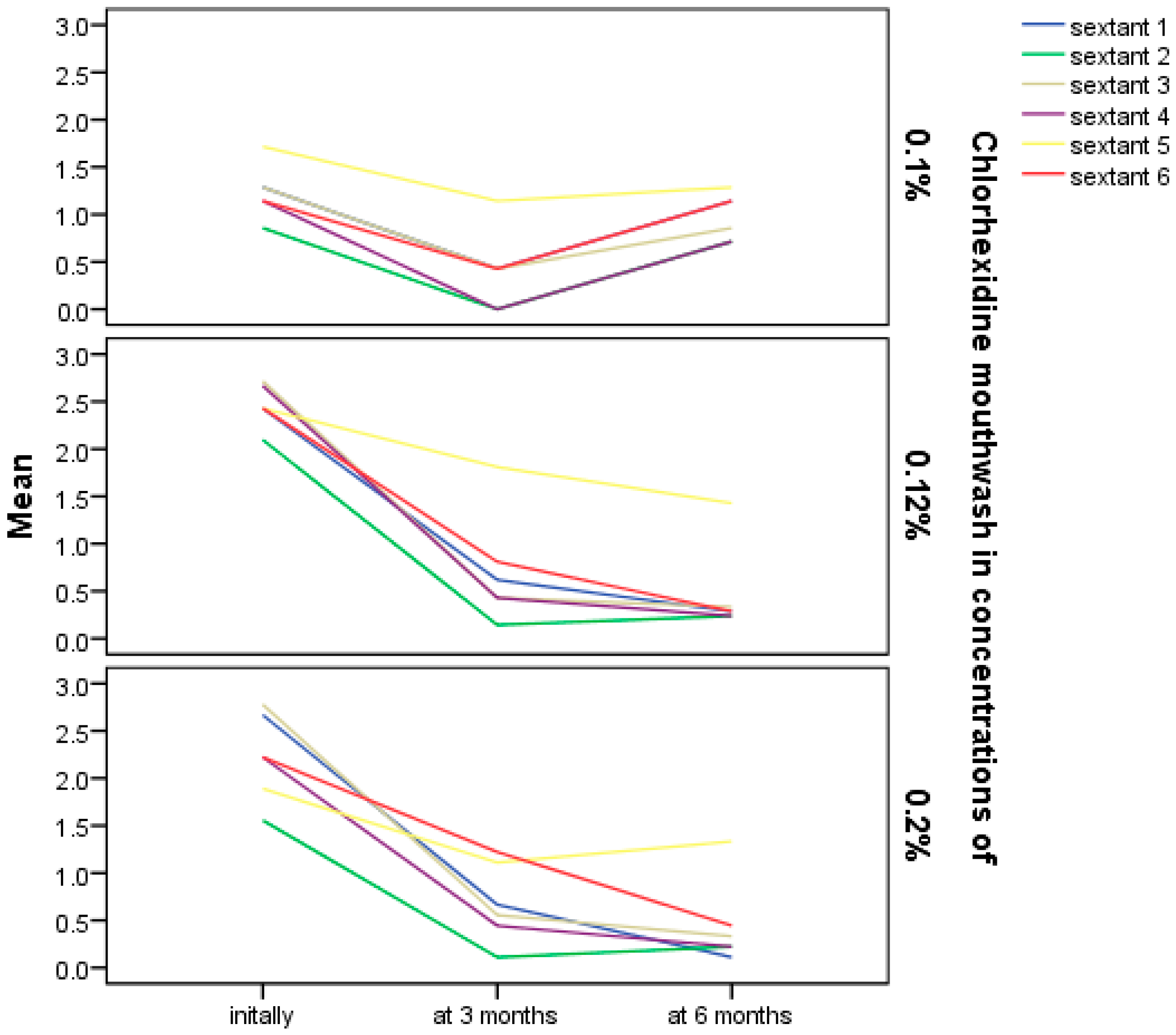
| p-Value for CPITN Values During Follow-Up | 0.1% CHX | 0.12% CHX | 0.2% CHX |
|---|---|---|---|
| Sextant 1 | 0.074 | <0.001 | 0.001 |
| Sextant 2 | 0.074 | <0.001 | 0.002 |
| Sextant 3 | 0.099 | <0.001 | <0.001 |
| Sextant 4 | 0.074 | <0.001 | <0.001 |
| Sextant 5 | 0.538 | 0.025 | 0.196 |
| Sextant 6 | 0.174 | <0.001 | 0.001 |
| Total score | 0.062 | <0.001 | 0.010 |
| Friedman Test | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicolae, X.A.; Preoteasa, E.; Murariu Măgureanu, C.; Moraru, R.; Preoteasa, C.T. Evolution of CPITN Index in Relation to Chlorhexidine Mouthwash Use in Patients with Deflective Occlusal Contacts. Bioengineering 2025, 12, 1140. https://doi.org/10.3390/bioengineering12111140
Nicolae XA, Preoteasa E, Murariu Măgureanu C, Moraru R, Preoteasa CT. Evolution of CPITN Index in Relation to Chlorhexidine Mouthwash Use in Patients with Deflective Occlusal Contacts. Bioengineering. 2025; 12(11):1140. https://doi.org/10.3390/bioengineering12111140
Chicago/Turabian StyleNicolae, Ximena Anca, Elena Preoteasa, Cătălina Murariu Măgureanu, Ruxandra Moraru, and Cristina Teodora Preoteasa. 2025. "Evolution of CPITN Index in Relation to Chlorhexidine Mouthwash Use in Patients with Deflective Occlusal Contacts" Bioengineering 12, no. 11: 1140. https://doi.org/10.3390/bioengineering12111140
APA StyleNicolae, X. A., Preoteasa, E., Murariu Măgureanu, C., Moraru, R., & Preoteasa, C. T. (2025). Evolution of CPITN Index in Relation to Chlorhexidine Mouthwash Use in Patients with Deflective Occlusal Contacts. Bioengineering, 12(11), 1140. https://doi.org/10.3390/bioengineering12111140






