Impact of Sex on Infection Risk in Patients with Systemic Lupus Erythematosus
Abstract
1. Introduction
1.1. Background
1.2. Sex Hormone-Induced Variations in Immune Response
1.3. What This Work Adds
2. Materials and Methods
2.1. Study Design and Population
2.2. Objectives
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Approval
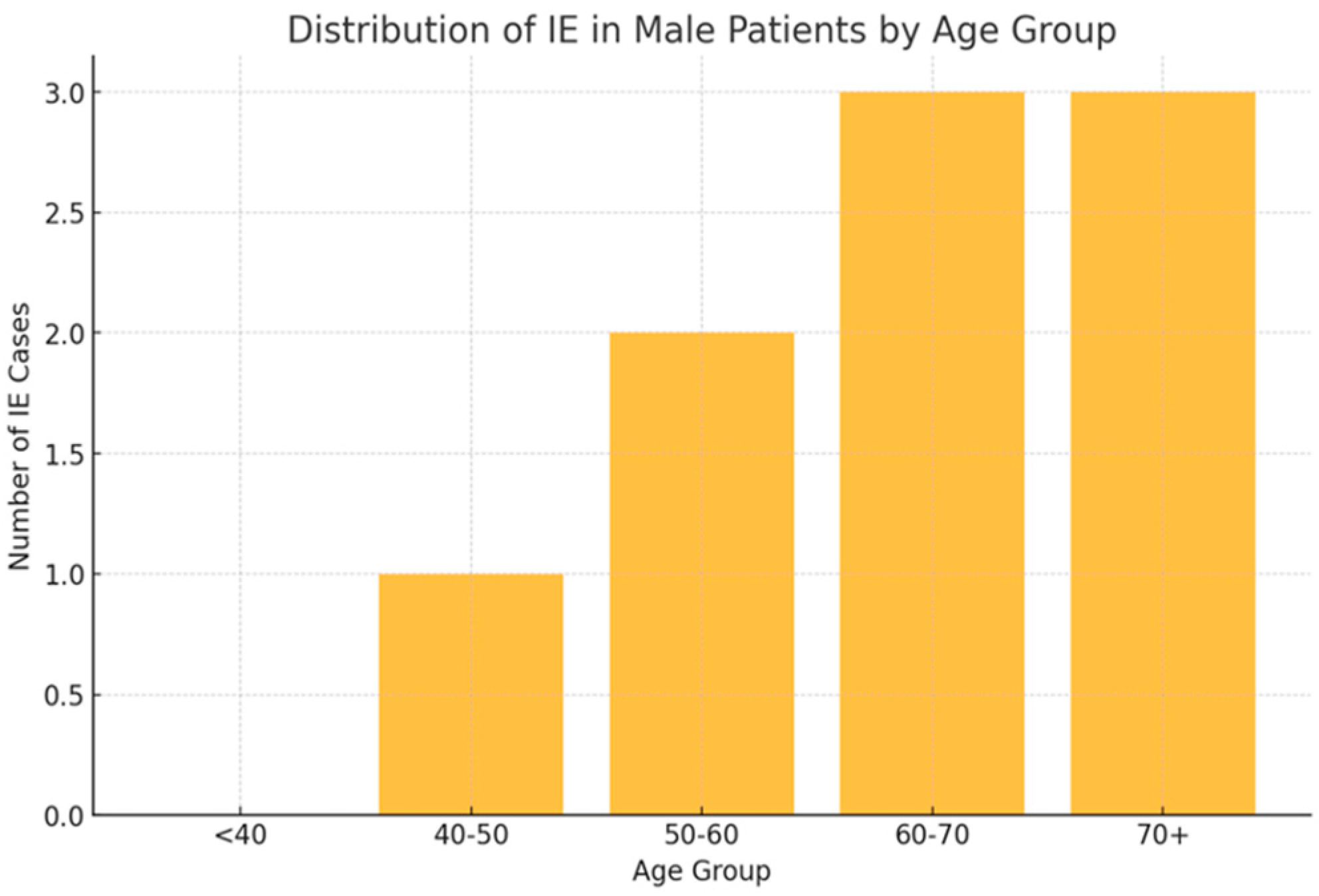
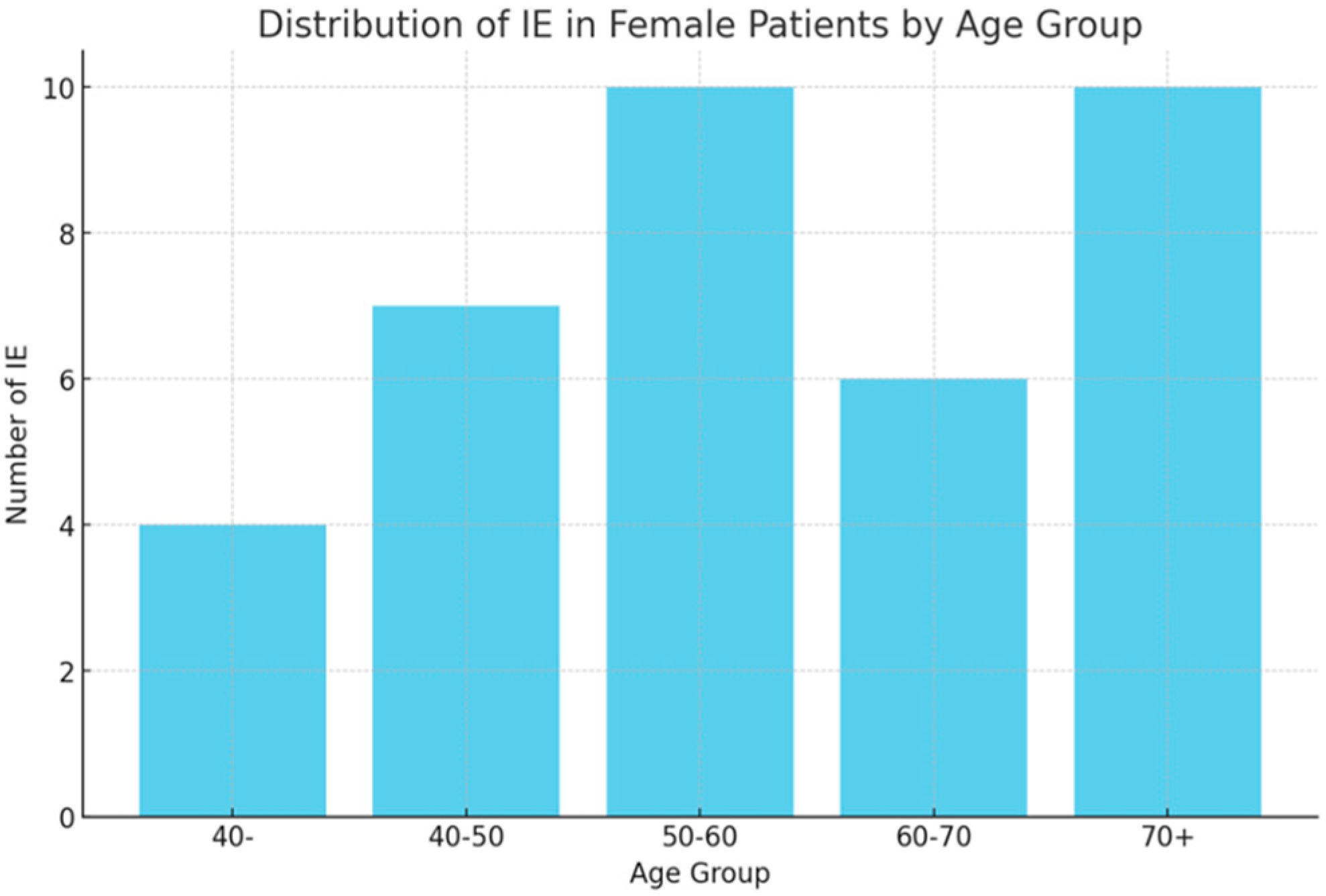
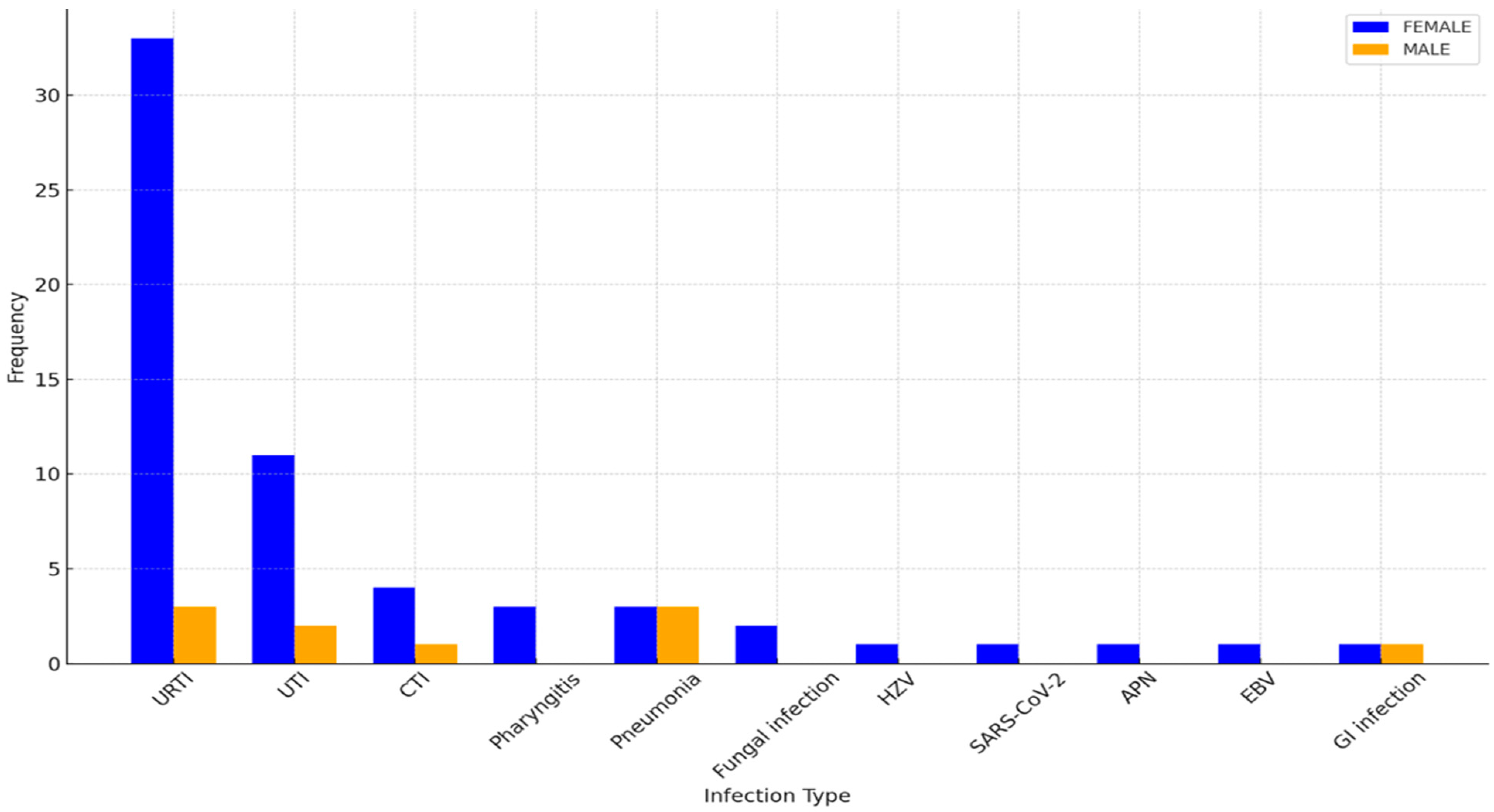
3. Results
4. Discussion
5. Conclusions
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Jha, S.B.; Rivera, A.P.; Monar, G.V.F.; Islam, H.; Puttagunta, S.M.; Islam, R.; Kundu, S.; Sange, I. Systemic Lupus Erythematosus and Cardiovascular Disease. Cureus 2022, 14, e22027. [Google Scholar] [CrossRef]
- Pego-Reigosa, J.M.; Nicholson, L.; Pooley, N.; Langham, S.; Embleton, N.; Marjenberg, Z.; Barut, V.; Desta, B.; Wang, X.; Langham, J.; et al. The risk of infections in adult patients with systemic lupus erythematosus: Systematic review and meta-analysis. J. Rheumatol. 2019, 47, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Rúa-Figueroa, I.; López-Longo, F.J.; Del Campo, V.; Galindo-Izquierdo, M.; Uriarte, E.; Torre-Cisneros, J.; Vela, P.; Tomero, E.; Narváez, J.; Olivé, A.; et al. Bacteremia in Systemic Lupus Erythematosus in Patients from a Spanish Registry: Risk Factors, Clinical and Microbiological Characteristics, and Outcomes. J. Rheumatol. 2020, 47, 234–240. [Google Scholar] [CrossRef]
- Barber, M.R.W.; Drenkard, C.; Falasinnu, T.; Hoi, A.; Mak, A.; Kow, N.Y.; Svenungsson, E.; Peterson, J.; Clarke, A.E.; Ramsey-Goldman, R. Global epidemiology of systemic lupus erythematosus. Nat. Rev. Rheumatol. 2021, 17, 515–532. [Google Scholar] [CrossRef] [PubMed]
- Trentin, F.; Signorini, V.; Manca, M.L.; Cascarano, G.; Gualtieri, L.; Schilirò, D.; Valevich, A.; Cardelli, C.; Carli, L.; Elefante, E.; et al. Gender differences in SLE: Report from a cohort of 417 Caucasian patients. Lupus Sci. Med. 2023, 10, e000880. [Google Scholar] [CrossRef] [PubMed]
- Nusbaum, J.S.; Mirza, I.; Shum, J.; Freilich, R.W.; Cohen, R.E.; Pillinger, M.H.; Izmirly, P.M.; Buyon, J.P. Sex Differences in Systemic Lupus Erythematosus: Epidemiology, Clinical Considerations, and Disease Pathogenesis. Mayo Clin. Proc. 2020, 95, 384–394. [Google Scholar] [CrossRef]
- Sepúlveda, J.I.R.; Bolin, K.; Mofors, J.; Leonard, D.; Svenungsson, E.; Jönsen, A.; Bengtsson, C.; Nordmark, G.; Dahlqvist, S.R.; Bengtsson, A.A. Sex differences in clinical presentation of systemic lupus erythematosus. Biol. Sex Differ. 2019, 10, 60. [Google Scholar]
- Christou EA, A.; Banos, A.; Kosmara, D.; Bertsias, G.; Boumpas, D. Sexual dimorphism in SLE: Above and beyond sex hormones. Lupus 2019, 28, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, D. TLR9 polymorphisms and systemic lupus erythematosus risk: An update meta-analysis study. Rheumatol. Int. 2016, 36, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Satterthwaite, A.B. TLR7 Signaling in Lupus B Cells: New Insights into Synergizing Factors and Downstream Signals. Curr. Rheumatol. Rep. 2021, 23, 80. [Google Scholar] [CrossRef]
- Khan, D.; Dai, R.; Ahmed, S.A. Sex differences and estrogen regulation of miRNAs in lupus, a prototypical autoimmune disease. Cell. Immunol. 2015, 294, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Sexual Dimorphism of miRNA Expression: A New Perspective in Understanding the Sex Bias of Autoimmune Diseases. Available online: https://www.tandfonline.com/doi/full/10.2147/TCRM.S33517 (accessed on 5 September 2024).
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 EULAR/ACR Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019, 71, 1400–1412. [Google Scholar] [CrossRef]
- Systemic Lupus Erythematosus in a Multiethnic Cohort (LUMINA): XXVIII. Factors Predictive of Thrombotic Events|Rheumatology|Oxford Academic. Available online: https://academic.oup.com/rheumatology/article/44/10/1303/1788385 (accessed on 6 September 2024).
- Schwartzman-Morris, J.; Putterman, C. Gender Differences in the Pathogenesis and Outcome of Lupus and of Lupus Nephritis. Clin. Dev. Immunol. 2012, 2012, 604892. [Google Scholar] [CrossRef]
- Nicola, S.; Borrelli, R.; Corradi, F.; Lo Sardo, L.; Badiu, I.; Romito, A.; Rashidy, N.; Quinternetto, A.; Mazzola, M.; Meli, F.; et al. Relationship between clinical manifestations and serological profile in patients affected by Systemic Lupus Erythematosus. Front. Immunol. 2024, 15, 1390642. [Google Scholar] [CrossRef]
| N | AGE | SD | DISEASE DURATION | SD | DISEASE SEVERITY (Mild–Moderate–Severe, %) | |
|---|---|---|---|---|---|---|
| TOT | 119 | 54.62 | 13.61 | 25.60 | 13.54 | |
| FEMALE | 107 | 54.3 | 13.62 | 25.30 | 13.62 | (18; 79; 3) |
| MALE | 12 | 57.25 | 13.56 | 17.98 | 9.47 | (8; 84; 8) |
| Comorbidity | F (n,%) | M (n,%) |
|---|---|---|
| Obesity | 29 (27.1) | 5 (41.7) |
| Diabetes mellitus | 7 (6.6) | 1 (8.3) |
| Hashimoto’s thyroiditis | 41 (38.3) | 0 (0.0) |
| Gastroesophageal reflux | 36 (33.6) | 4 (33.3) |
| Osteoporosis | 11 (10.3) | 1 (8.3) |
| Asthma | 2 (1.9) | 0 (0.0) |
| Treatment | Patients, N (%) | F/M | Chi Squared (p-Value) |
|---|---|---|---|
| BEL | 83 (69.75) | 74/9 | NS |
| AZA | 19 (15.97) | 18/1 | NS |
| MMF | 17 (14.29) | 15/2 | NS |
| OCS Dosage: Median, Q25, Q75 | F | M | Mann–Whitney U (p-Value) |
|---|---|---|---|
| 5.0 (5.0; 10.0) | 7.5 (5.0;10.0) | 5.0 (2.5;7.5) | NS |
| Variable | Coefficient (β) | Logistic Equation | p-Value | Hosmer–Lemeshow Test |
|---|---|---|---|---|
| Disease Duration | 0.025 | Logit(p) = −1.1319 + 0.0250 × dd | 0.102 | |
| Sex | 0.9426 | Logit(p) = −0.6061 + 0.9426 × sex | 0.05 | |
| Smoking | 0.4529 | Logit(p) = −0.8200 + 0.4529 × smoking | 0.078 | |
| Overall Model | Logit(p) = −0.6563 + 0.0283 × dd + 1.2154 × sex + 0.3971 × smoking | stat: 0.1893, df: 5, p = 0.9992 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borrelli, R.; Nicola, S.; Corradi, F.; Badiu, I.; Lo Sardo, L.; Rashidy, N.; Quinternetto, A.; Mazzola, M.; Meli, F.; Saracco, E.; et al. Impact of Sex on Infection Risk in Patients with Systemic Lupus Erythematosus. Bioengineering 2025, 12, 59. https://doi.org/10.3390/bioengineering12010059
Borrelli R, Nicola S, Corradi F, Badiu I, Lo Sardo L, Rashidy N, Quinternetto A, Mazzola M, Meli F, Saracco E, et al. Impact of Sex on Infection Risk in Patients with Systemic Lupus Erythematosus. Bioengineering. 2025; 12(1):59. https://doi.org/10.3390/bioengineering12010059
Chicago/Turabian StyleBorrelli, R., S. Nicola, F. Corradi, I. Badiu, L. Lo Sardo, N. Rashidy, A. Quinternetto, M. Mazzola, F. Meli, E. Saracco, and et al. 2025. "Impact of Sex on Infection Risk in Patients with Systemic Lupus Erythematosus" Bioengineering 12, no. 1: 59. https://doi.org/10.3390/bioengineering12010059
APA StyleBorrelli, R., Nicola, S., Corradi, F., Badiu, I., Lo Sardo, L., Rashidy, N., Quinternetto, A., Mazzola, M., Meli, F., Saracco, E., Vitali, I., Negrini, S., & Brussino, L. (2025). Impact of Sex on Infection Risk in Patients with Systemic Lupus Erythematosus. Bioengineering, 12(1), 59. https://doi.org/10.3390/bioengineering12010059






