Applications of Imaging Technologies in Fuchs Endothelial Corneal Dystrophy: A Narrative Literature Review
Abstract
1. Introduction
2. Anterior Segment Optical Coherence Tomography (AS-OCT)
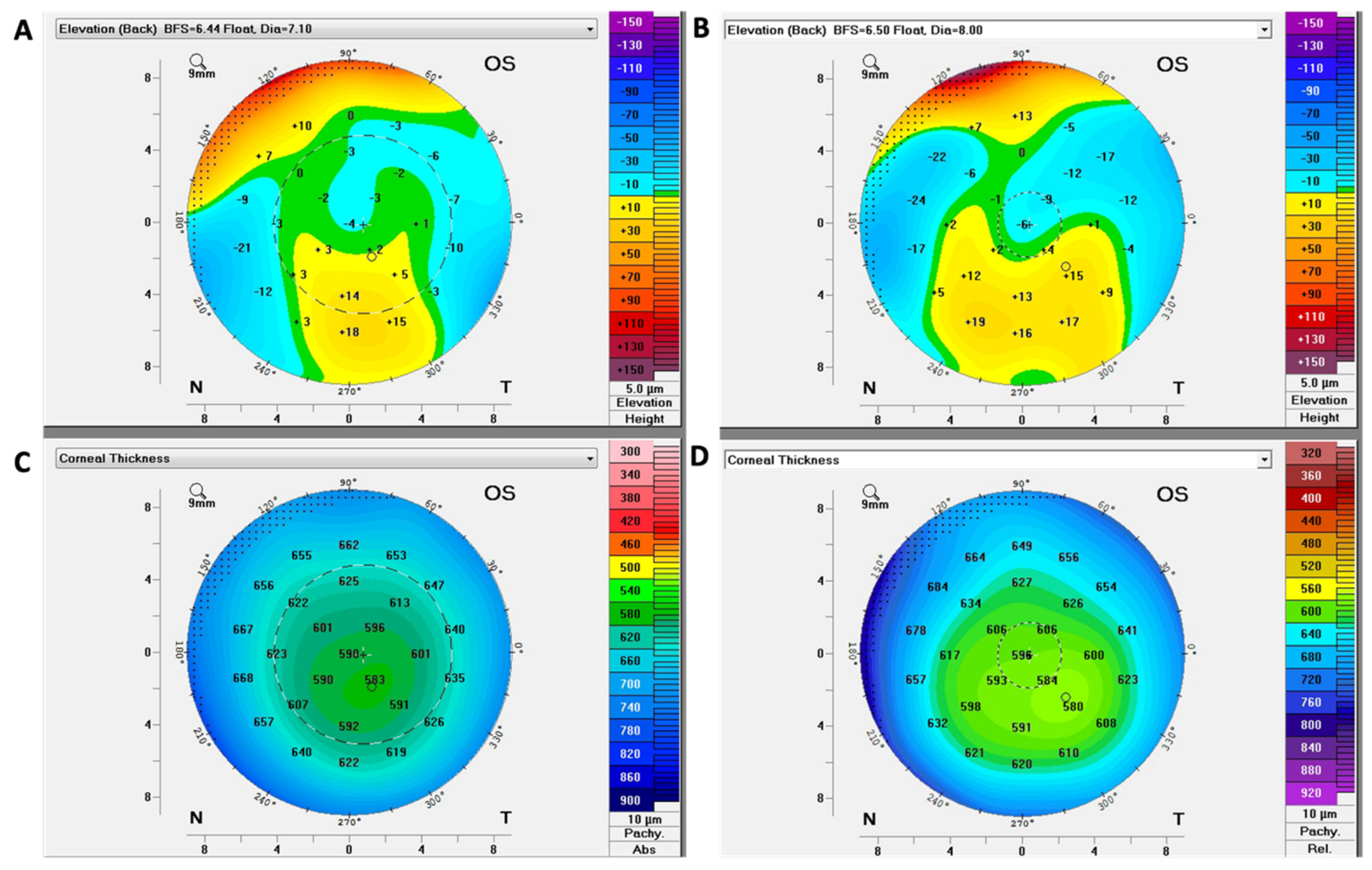
3. Scheimpflug Corneal Tomography
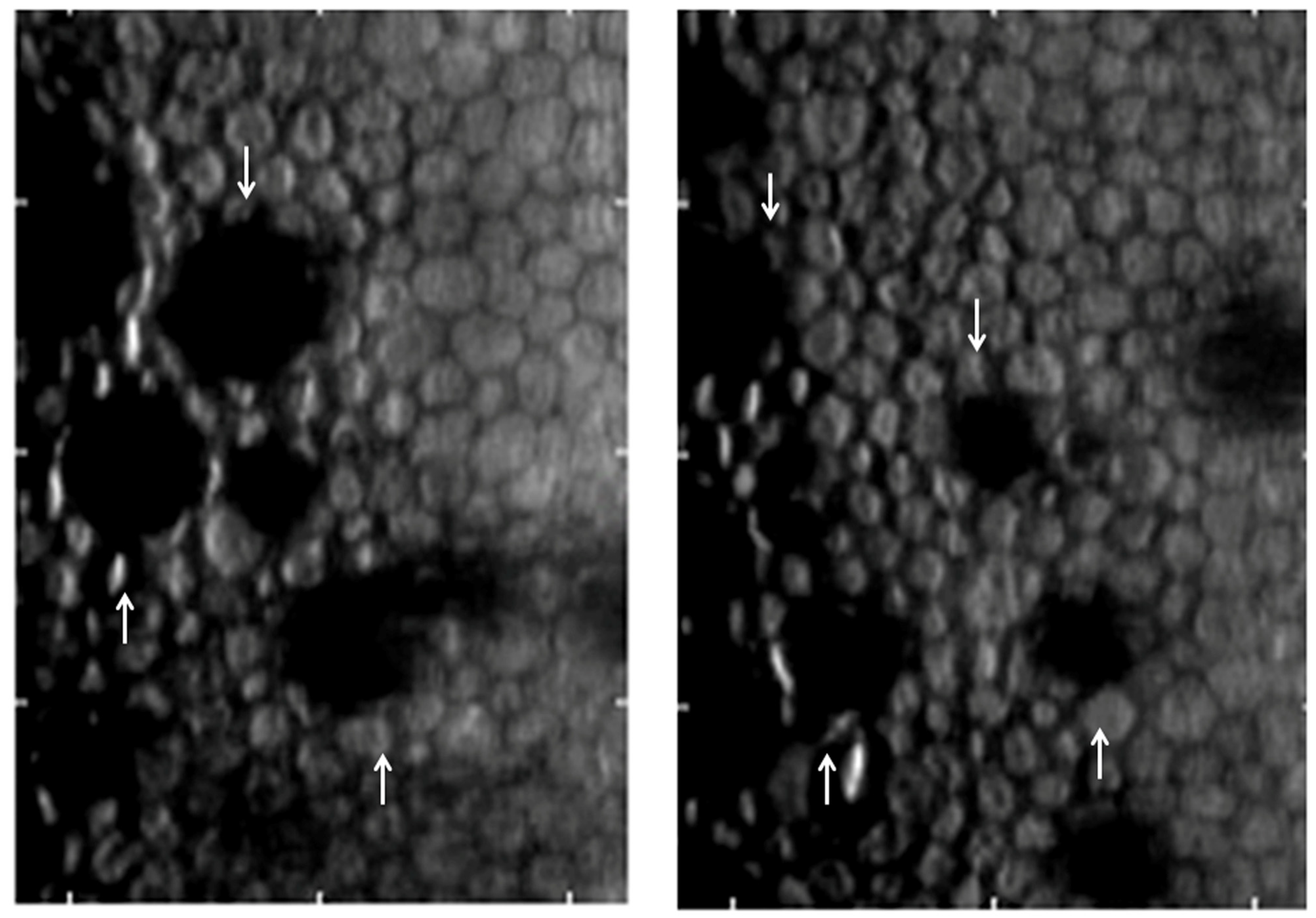
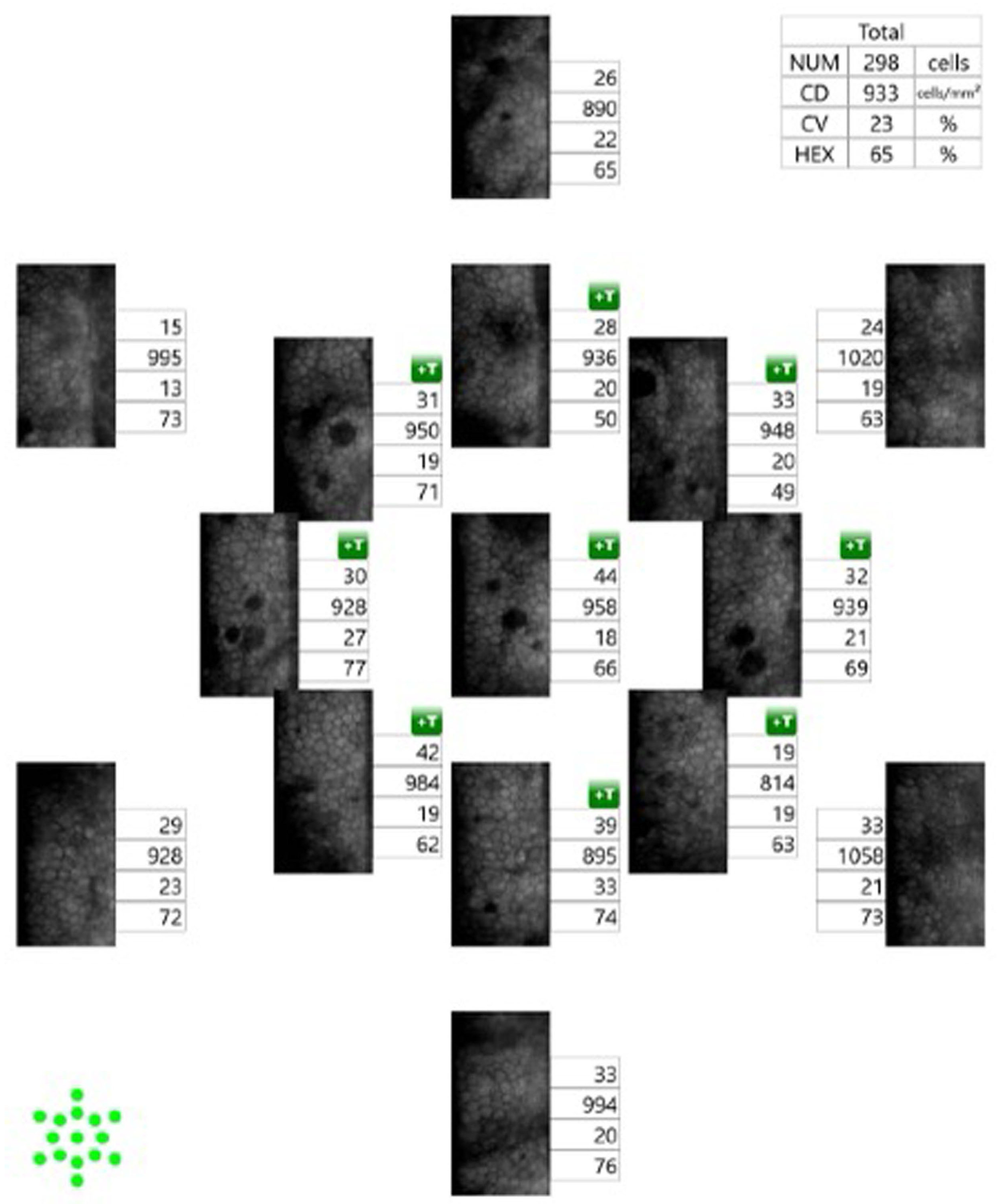
4. Specular Microscopy
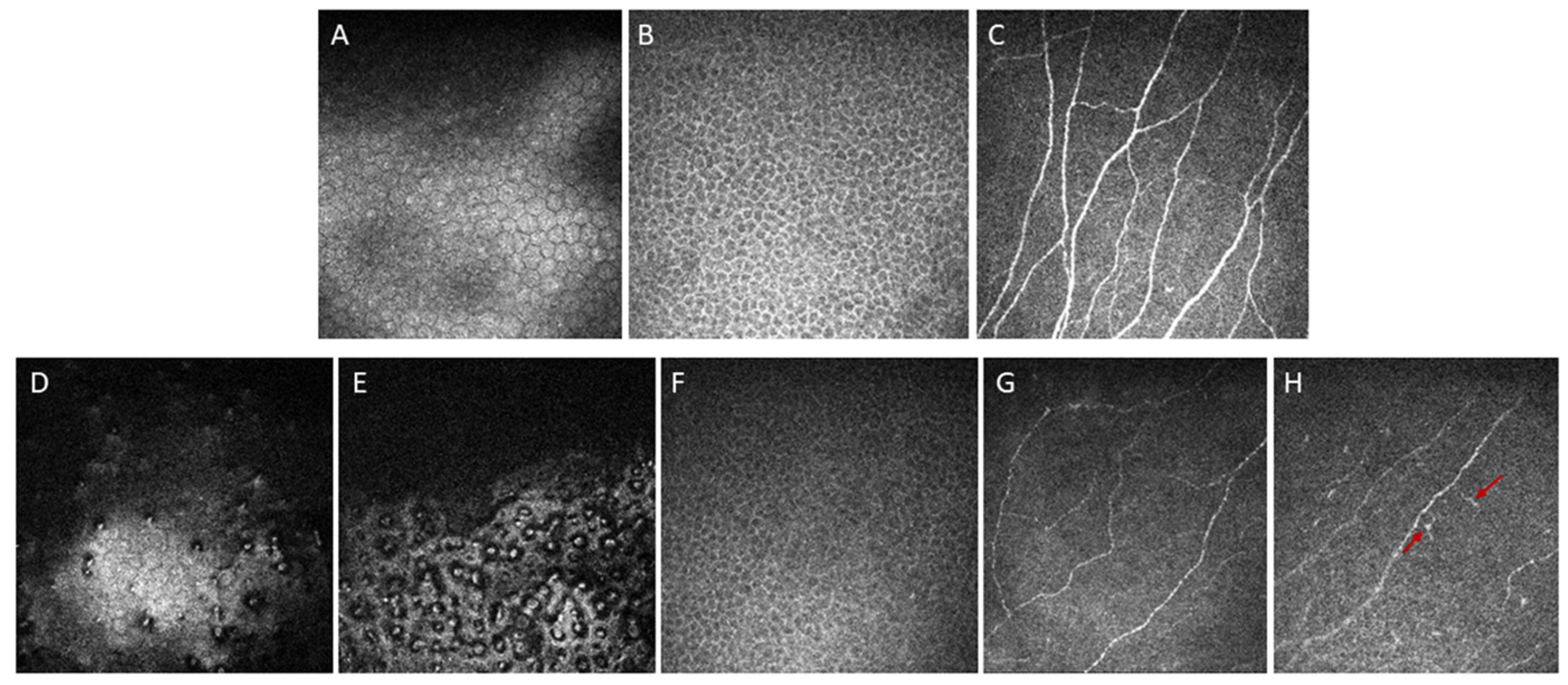
5. In Vivo Confocal Microscopy (IVCM)
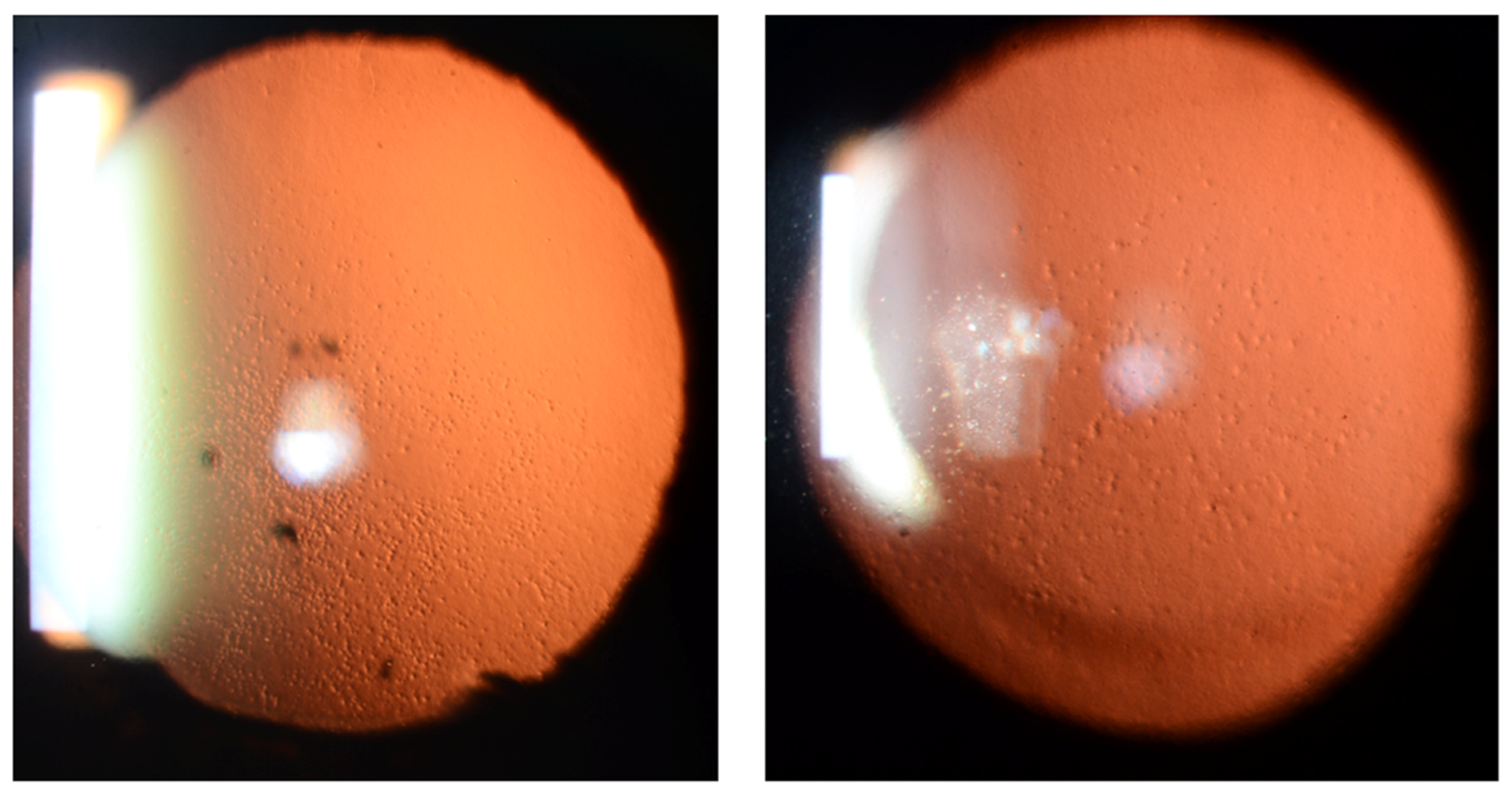
6. Analysis of Retroillumination Photography
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Van den Bogerd, B.; Dhubhghaill, S.N.; Koppen, C.; Tassignon, M.J.; Zakaria, N. A review of the evidence for in vivo corneal endothelial regeneration. Surv. Ophthalmol. 2018, 63, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Lorenzetti, D.W.; Uotila, M.H.; Parikh, N.; Kaufman, H.E. Central cornea guttata. Incidence in the general population. Am. J. Ophthalmol. 1967, 64, 1155–1158. [Google Scholar] [CrossRef] [PubMed]
- Aiello, F.; Gallo Afflitto, G.; Ceccarelli, F.; Cesareo, M.; Nucci, C. Global Prevalence of Fuchs Endothelial Corneal Dystrophy (FECD) in Adult Population: A Systematic Review and Meta-Analysis. J. Ophthalmol. 2022, 2022, 3091695. [Google Scholar] [CrossRef] [PubMed]
- Hamill, C.E.; Schmedt, T.; Jurkunas, U. Fuchs endothelial cornea dystrophy: A review of the genetics behind disease development. Semin. Ophthalmol. 2013, 28, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Altamirano, F.; Ortiz-Morales, G.; O’Connor-Cordova, M.A.; Sancén-Herrera, J.P.; Zavala, J.; Valdez-Garcia, J.E. Fuchs endothelial corneal dystrophy: An updated review. Int. Ophthalmol. 2024, 44, 61. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, P.; Sahoo, S.; Sahu, S.K.; Priyadarshini, S.; Mohanty, A.; Das, S. Demographic profile and clinical characteristics of Fuchs’ endothelial corneal dystrophy in a tertiary eye care center. Indian J. Ophthalmol. 2023, 71, 505–509. [Google Scholar] [CrossRef]
- Colby, K. Descemet Stripping Only for Fuchs Endothelial Corneal Dystrophy: Will It Become the Gold Standard? Cornea 2022, 41, 269–271. [Google Scholar] [CrossRef]
- Liu, J.-X.; Chiang, T.-L.; Hung, K.-F.; Sun, Y.-C. Therapeutic future of Fuchs endothelial corneal dystrophy: An ongoing way to explore. Taiwan J. Ophthalmol. 2024. [Google Scholar] [CrossRef]
- Pizzuto, S.; Duffey, G.; Weant, J.; Eveleth, D. Acceleration of Regeneration of the Corneal Endothelial Layer After Descemet Stripping Induced by the Engineered FGF TTHX1114 in Human Corneas in Organ Culture. Cornea 2023, 42, 232–242. [Google Scholar] [CrossRef]
- Adamis, A.P.; Filatov, V.; Tripathi, B.J.; Tripathi, R.C. Fuchs’ endothelial dystrophy of the cornea. Surv. Ophthalmol. 1993, 38, 149–168. [Google Scholar] [CrossRef]
- Laing, R.A.; Leibowitz, H.M.; Oak, S.S.; Chang, R.; Berrospi, A.R.; Theodore, J. Endothelial mosaic in Fuchs’ dystrophy. A qualitative evaluation with the specular microscope. Arch. Ophthalmol. 1981, 99, 80–83. [Google Scholar] [CrossRef]
- Soh, Y.Q.; Kocaba, V.; Pinto, M.; Mehta, J.S. Fuchs endothelial corneal dystrophy and corneal endothelial diseases: East meets West. Eye 2020, 34, 427–441. [Google Scholar] [CrossRef] [PubMed]
- Thaung, C.; Davidson, A.E. Fuchs endothelial corneal dystrophy: Current perspectives on diagnostic pathology and genetics-Bowman Club Lecture. BMJ Open Ophthalmol. 2022, 7, e001103. [Google Scholar] [CrossRef]
- Chan, T.C.Y.; Wan, K.H.; Shih, K.C.; Jhanji, V. Advances in dry eye imaging: The present and beyond. Br. J. Ophthalmol. 2018, 102, 295–301. [Google Scholar] [CrossRef]
- Ong Tone, S.; Jurkunas, U. Imaging the Corneal Endothelium in Fuchs Corneal Endothelial Dystrophy. Semin. Ophthalmol. 2019, 34, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Moutsouris, K.; Dapena, I.; Ham, L.; Balachandran, C.; Oellerich, S.; Melles, G.R. Optical coherence tomography, Scheimpflug imaging, and slit-lamp biomicroscopy in the early detection of graft detachment after Descemet membrane endothelial keratoplasty. Cornea 2011, 30, 1369–1375. [Google Scholar] [CrossRef] [PubMed]
- Han, S.B.; Liu, Y.C.; Noriega, K.M.; Mehta, J.S. Applications of Anterior Segment Optical Coherence Tomography in Cornea and Ocular Surface Diseases. J. Ophthalmol. 2016, 2016, 4971572. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Gupta, S.; Maharana, P.; Shanmugam, P.; Nagpal, R.; Vajpayee, R.B. Anterior Segment Optical Coherence Tomography-Guided Management Algorithm for Descemet Membrane Detachment After Intraocular Surgery. Cornea 2015, 34, 1170–1174. [Google Scholar] [CrossRef]
- Wylegala, E.; Nowinska, A. Usefulness of anterior segment optical coherence tomography in Descemet membrane detachment. Eur. J. Ophthalmol. 2009, 19, 723–728. [Google Scholar] [CrossRef]
- Kymionis, G.D.; Ide, T.; Donaldson, K.; Yoo, S.H. Diagnosis of Donor Graft Partial Dislocation Behind the Iris After DSAEK with Anterior Segment OCT. Ophthalmic Surg. Lasers Imaging Off. J. Int. Soc. Imaging Eye 2010, 41, 1–2. [Google Scholar] [CrossRef]
- Yeh, R.Y.; Quilendrino, R.; Musa, F.U.; Liarakos, V.S.; Dapena, I.; Melles, G.R. Predictive value of optical coherence tomography in graft attachment after Descemet’s membrane endothelial keratoplasty. Ophthalmology 2013, 120, 240–245. [Google Scholar] [CrossRef]
- Augustin, V.A.; Köppe, M.K.; Son, H.S.; Meis, J.; Yildirim, T.M.; Khoramnia, R.; Auffarth, G.U. Scheimpflug Versus Optical Coherence Tomography to Detect Subclinical Corneal Edema in Fuchs Endothelial Corneal Dystrophy. Cornea 2022, 41, 1378–1385. [Google Scholar] [CrossRef]
- Huang, J.; Tepelus, T.C.; Baghdasaryan, E.; Huang, P.; Shi, Y.; Hsu, H.Y.; Sadda, S.R.; Lee, O.L. Correlation between Guttata Severity and Thickness of Descemet’s Membrane and the Central Cornea. Curr. Eye Res. 2019, 44, 849–855. [Google Scholar] [CrossRef]
- Yasukura, Y.; Oie, Y.; Kawasaki, R.; Maeda, N.; Jhanji, V.; Nishida, K. New severity grading system for Fuchs endothelial corneal dystrophy using anterior segment optical coherence tomography. Acta Ophthalmol. 2021, 99, e914–e921. [Google Scholar] [CrossRef] [PubMed]
- Wertheimer, C.M.; Elhardt, C.; Wartak, A.; Luft, N.; Kassumeh, S.; Dirisamer, M.; Siedlecki, J.; Vounotrypidis, E.; Priglinger, S.G.; Mayer, W.J. Corneal optical density in Fuchs endothelial dystrophy determined by anterior segment optical coherence tomography. Eur. J. Ophthalmol. 2021, 31, 1771–1778. [Google Scholar] [CrossRef] [PubMed]
- Nowińska, A.; Chlasta-Twardzik, E.; Dembski, M.; Ulfik-Dembska, K.; Wylęgała, E. Corneal Analysis with Swept Source Optical Coherence Tomography in Patients with Coexisting Cataract and Fuchs Endothelial Corneal Dystrophy. Diagnostics 2021, 11, 223. [Google Scholar] [CrossRef]
- Arnalich-Montiel, F.; Ortiz-Toquero, S.; Auladell, C.; Couceiro, A. Accuracy of Corneal Thickness by Swept-Source Optical Coherence Tomography and Scheimpflug Camera in Virgin and Treated Fuchs Endothelial Dystrophy. Cornea 2018, 37, 727–733. [Google Scholar] [CrossRef]
- Shousha, M.A.; Perez, V.L.; Wang, J.; Ide, T.; Jiao, S.; Chen, Q.; Chang, V.; Buchser, N.; Dubovy, S.R.; Feuer, W.; et al. Use of ultra-high-resolution optical coherence tomography to detect in vivo characteristics of Descemet’s membrane in Fuchs’ dystrophy. Ophthalmology 2010, 117, 1220–1227. [Google Scholar] [CrossRef] [PubMed]
- Werkmeister, R.M.; Sapeta, S.; Schmidl, D.; Garhofer, G.; Schmidinger, G.; Aranha Dos Santos, V.; Aschinger, G.C.; Baumgartner, I.; Pircher, N.; Schwarzhans, F.; et al. Ultrahigh-resolution OCT imaging of the human cornea. Biomed. Opt. Express 2017, 8, 1221–1239. [Google Scholar] [CrossRef]
- Iovino, C.; Fossarello, M.; Giannaccare, G.; Pellegrini, M.; Braghiroli, M.; Demarinis, G.; Napoli, P.E. Corneal endothelium features in Fuchs’ Endothelial Corneal Dystrophy: A preliminary 3D anterior segment optical coherence tomography study. PLoS ONE 2018, 13, e0207891. [Google Scholar] [CrossRef]
- Eleiwa, T.; Elsawy, A.; Tolba, M.; Feuer, W.; Yoo, S.; Shousha, M.A. Diagnostic Performance of 3-Dimensional Thickness of the Endothelium-Descemet Complex in Fuchs’ Endothelial Cell Corneal Dystrophy. Ophthalmology 2020, 127, 874–887. [Google Scholar] [CrossRef]
- Eleiwa, T.; Elsawy, A.; Özcan, E.; Abou Shousha, M. Automated diagnosis and staging of Fuchs’ endothelial cell corneal dystrophy using deep learning. Eye Vis. 2020, 7, 44. [Google Scholar] [CrossRef] [PubMed]
- Bitton, K.; Zéboulon, P.; Ghazal, W.; Rizk, M.; Elahi, S.; Gatinel, D. Deep Learning Model for the Detection of Corneal Edema Before Descemet Membrane Endothelial Keratoplasty on Optical Coherence Tomography Images. Transl. Vis. Sci. Technol. 2022, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Treder, M.; Lauermann, J.L.; Alnawaiseh, M.; Eter, N. Using Deep Learning in Automated Detection of Graft Detachment in Descemet Membrane Endothelial Keratoplasty: A Pilot Study. Cornea 2019, 38, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Ang, M.; Baskaran, M.; Werkmeister, R.M.; Chua, J.; Schmidl, D.; Aranha Dos Santos, V.; Garhofer, G.; Mehta, J.S.; Schmetterer, L. Anterior segment optical coherence tomography. Prog. Retin. Eye Res. 2018, 66, 132–156. [Google Scholar] [CrossRef]
- Patel, S.V. Imaging Fuchs Endothelial Corneal Dystrophy in Clinical Practice and Clinical Trials. Cornea 2021, 40, 1505–1511. [Google Scholar] [CrossRef]
- Wacker, K.; McLaren, J.W.; Amin, S.R.; Baratz, K.H.; Patel, S.V. Corneal High-Order Aberrations and Backscatter in Fuchs’ Endothelial Corneal Dystrophy. Ophthalmology 2015, 122, 1645–1652. [Google Scholar] [CrossRef]
- Wacker, K.; McLaren, J.W.; Patel, S.V. Directional Posterior Corneal Profile Changes in Fuchs’ Endothelial Corneal Dystrophy. Investig. Ophthalmol. Vis. Sci. 2015, 56, 5904–5911. [Google Scholar] [CrossRef]
- Chu, H.Y.; Hsiao, C.H.; Chen, P.Y.; Ma, D.H.; Chang, C.J.; Tan, H.Y. Corneal Backscatters as an Objective Index for Assessing Fuchs’ Endothelial Corneal Dystrophy: A Pilot Study. J. Ophthalmol. 2017, 2017, 8747013. [Google Scholar] [CrossRef]
- Patel, S.V.; Hodge, D.O.; Treichel, E.J.; Spiegel, M.R.; Baratz, K.H. Repeatability of Scheimpflug Tomography for Assessing Fuchs Endothelial Corneal Dystrophy. Am. J. Ophthalmol. 2020, 215, 91–103. [Google Scholar] [CrossRef]
- Sun, S.Y.; Wacker, K.; Baratz, K.H.; Patel, S.V. Determining Subclinical Edema in Fuchs Endothelial Corneal Dystrophy: Revised Classification using Scheimpflug Tomography for Preoperative Assessment. Ophthalmology 2019, 126, 195–204. [Google Scholar] [CrossRef]
- Patel, S.V.; Hodge, D.O.; Treichel, E.J.; Spiegel, M.R.; Baratz, K.H. Predicting the Prognosis of Fuchs Endothelial Corneal Dystrophy by Using Scheimpflug Tomography. Ophthalmology 2020, 127, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Mingo-Botín, D.; Arnalich-Montiel, F.; Couceiro de Juan, A.; Ortiz-Toquero, S. Repeatability and Intersession Reproducibility of Pentacam Corneal Thickness Maps in Fuchs Dystrophy and Endothelial Keratoplasty. Cornea 2018, 37, 987–992. [Google Scholar] [CrossRef]
- Zander, D.; Grewing, V.; Glatz, A.; Lapp, T.; Maier, P.C.; Reinhard, T.; Wacker, K. Predicting Edema Resolution After Descemet Membrane Endothelial Keratoplasty for Fuchs Dystrophy Using Scheimpflug Tomography. JAMA Ophthalmol. 2021, 139, 423–430. [Google Scholar] [CrossRef] [PubMed]
- McLaren, J.W.; Bachman, L.A.; Kane, K.M.; Patel, S.V. Objective assessment of the corneal endothelium in Fuchs’ endothelial dystrophy. Investig. Ophthalmol. Vis. Sci. 2014, 55, 1184–1190. [Google Scholar] [CrossRef]
- Oie, Y.; Watanabe, S.; Nishida, K. Evaluation of Visual Quality in Patients With Fuchs Endothelial Corneal Dystrophy. Cornea 2016, 35 (Suppl. S1), S55–S58. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, S.; Oie, Y.; Fujimoto, H.; Soma, T.; Koh, S.; Tsujikawa, M.; Maeda, N.; Nishida, K. Relationship between Corneal Guttae and Quality of Vision in Patients with Mild Fuchs’ Endothelial Corneal Dystrophy. Ophthalmology 2015, 122, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, H.; Maeda, N.; Soma, T.; Oie, Y.; Koh, S.; Tsujikawa, M.; Nishida, K. Quantitative regional differences in corneal endothelial abnormalities in the central and peripheral zones in Fuchs’ endothelial corneal dystrophy. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5090–5098. [Google Scholar] [CrossRef]
- Tanaka, H.; Okumura, N.; Koizumi, N.; Sotozono, C.; Sumii, Y.; Kinoshita, S. Panoramic view of human corneal endothelial cell layer observed by a prototype slit-scanning wide-field contact specular microscope. Br. J. Ophthalmol. 2017, 101, 655–659. [Google Scholar] [CrossRef]
- Lee, J.; Mori, Y.; Ogata, M.; Minami, K.; Miyata, K. Central and Peripheral Corneal Endothelial Cell Analysis With Slit-Scanning Wide-Field Contact Specular Microscopy: Agreement with Noncontact Specular Microscopy. Cornea 2019, 38, 1137–1141. [Google Scholar] [CrossRef]
- Toslak, D.; Thapa, D.; Erol, M.K.; Chen, Y.; Yao, X. Smartphone-based imaging of the corneal endothelium at sub-cellular resolution. J. Mod. Opt. 2017, 64, 1229–1232. [Google Scholar] [CrossRef]
- Mantena, S.; Chandra, J.; Pecyna, E.; Zhang, A.; Garrity, D.; Ong Tone, S.; Sastry, S.; Uddaraju, M.; Jurkunas, U.V. Low-Cost, Smartphone-Based Specular Imaging and Automated Analysis of the Corneal Endothelium. Transl. Vis. Sci. Technol. 2021, 10, 4. [Google Scholar] [CrossRef]
- Joseph, N.; Kolluru, C.; Benetz, B.A.M.; Menegay, H.J.; Lass, J.H.; Wilson, D.L. Quantitative and qualitative evaluation of deep learning automatic segmentations of corneal endothelial cell images of reduced image quality obtained following cornea transplant. J. Med. Imaging 2020, 7, 014503. [Google Scholar] [CrossRef] [PubMed]
- Kolluru, C.; Benetz, B.A.; Joseph, N.; Menegay, H.J.; Lass, J.H.; Wilson, D. Machine learning for segmenting cells in corneal endothelium images. Proc. SPIE Int. Soc. Opt. Eng. 2019, 10950, 1126–1135. [Google Scholar] [CrossRef]
- Vigueras-Guillen, J.P.; Andrinopoulou, E.R.; Engel, A.; Lemij, H.G.; van Rooij, J.; Vermeer, K.A.; van Vliet, L.J. Corneal Endothelial Cell Segmentation by Classifier-Driven Merging of Oversegmented Images. IEEE Trans. Med. Imaging 2018, 37, 2278–2289. [Google Scholar] [CrossRef] [PubMed]
- Vigueras-Guillen, J.P.; van Rooij, J.; Lemij, H.G.; Vermeer, K.A.; van Vliet, L.J. Convolutional neural network-based regression for biomarker estimation in corneal endothelium microscopy images. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 876–881. [Google Scholar] [CrossRef]
- Heinzelmann, S.; Daniel, M.C.; Maier, P.C.; Reinhard, T.; Bohringer, D. Automated Cell Counting Using “Deep Learning” in Donor Corneas from Organ Culture Achieves High Precision and Accuracy. Klin. Monatsblatter Fur Augenheilkd. 2019, 236, 1407–1412. [Google Scholar] [CrossRef]
- Scarpa, F.; Ruggeri, A. Development of a Reliable Automated Algorithm for the Morphometric Analysis of Human Corneal Endothelium. Cornea 2016, 35, 1222–1228. [Google Scholar] [CrossRef]
- Daniel, M.C.; Atzrodt, L.; Bucher, F.; Wacker, K.; Böhringer, S.; Reinhard, T.; Böhringer, D. Automated segmentation of the corneal endothelium in a large set of ‘real-world’ specular microscopy images using the U-Net architecture. Sci. Rep. 2019, 9, 4752. [Google Scholar] [CrossRef]
- Vigueras-Guillén, J.P.; Sari, B.; Goes, S.F.; Lemij, H.G.; van Rooij, J.; Vermeer, K.A.; van Vliet, L.J. Fully convolutional architecture vs sliding-window CNN for corneal endothelium cell segmentation. BMC Biomed. Eng. 2019, 1, 4. [Google Scholar] [CrossRef]
- Vigueras-Guillén, J.P.; van Rooij, J.; Engel, A.; Lemij, H.G.; van Vliet, L.J.; Vermeer, K.A. Deep Learning for Assessing the Corneal Endothelium from Specular Microscopy Images up to 1 Year after Ultrathin-DSAEK Surgery. Transl. Vis. Sci. Technol. 2020, 9, 49. [Google Scholar] [CrossRef]
- Okumura, N.; Yamada, S.; Nishikawa, T.; Narimoto, K.; Okamura, K.; Izumi, A.; Hiwa, S.; Hiroyasu, T.; Koizumi, N. U-Net Convolutional Neural Network for Segmenting the Corneal Endothelium in a Mouse Model of Fuchs Endothelial Corneal Dystrophy. Cornea 2022, 41, 901–907. [Google Scholar] [CrossRef]
- Shilpashree, P.S.; Suresh, K.V.; Sudhir, R.R.; Srinivas, S.P. Automated Image Segmentation of the Corneal Endothelium in Patients With Fuchs Dystrophy. Transl. Vis. Sci. Technol. 2021, 10, 27. [Google Scholar] [CrossRef] [PubMed]
- Vigueras-Guillén, J.P.; van Rooij, J.; van Dooren, B.T.H.; Lemij, H.G.; Islamaj, E.; van Vliet, L.J.; Vermeer, K.A. DenseUNets with feedback non-local attention for the segmentation of specular microscopy images of the corneal endothelium with guttae. Sci. Rep. 2022, 12, 14035. [Google Scholar] [CrossRef] [PubMed]
- Niederer, R.L.; McGhee, C.N. Clinical in vivo confocal microscopy of the human cornea in health and disease. Prog. Retin. Eye Res. 2010, 29, 30–58. [Google Scholar] [CrossRef] [PubMed]
- Mustonen, R.K.; McDonald, M.B.; Srivannaboon, S.; Tan, A.L.; Doubrava, M.W.; Kim, C.K. In vivo confocal microscopy of Fuchs’ endothelial dystrophy. Cornea 1998, 17, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Hara, M.; Morishige, N.; Chikama, T.; Nishida, T. Comparison of confocal biomicroscopy and noncontact specular microscopy for evaluation of the corneal endothelium. Cornea 2003, 22, 512–515. [Google Scholar] [CrossRef] [PubMed]
- Grupcheva, C.N.; Craig, J.P.; Sherwin, T.; McGhee, C.N. Differential diagnosis of corneal oedema assisted by in vivo confocal microscopy. Clin. Exp. Ophthalmol. 2001, 29, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Han, S.B.; Liu, Y.C.; Mohamed-Noriega, K.; Tong, L.; Mehta, J.S. Objective Imaging Diagnostics for Dry Eye Disease. J. Ophthalmol. 2020, 2020, 3509064. [Google Scholar] [CrossRef]
- Kaufman, S.C.; Beuerman, R.W.; Kaufman, H.E. Diagnosis of advanced Fuchs’ endothelial dystrophy with the confocal microscope. Am. J. Ophthalmol. 1993, 116, 652–653. [Google Scholar] [CrossRef]
- Amin, S.R.; Baratz, K.H.; McLaren, J.W.; Patel, S.V. Corneal abnormalities early in the course of Fuchs’ endothelial dystrophy. Ophthalmology 2014, 121, 2325–2333. [Google Scholar] [CrossRef]
- Schrems-Hoesl, L.M.; Schrems, W.A.; Cruzat, A.; Shahatit, B.M.; Bayhan, H.A.; Jurkunas, U.V.; Hamrah, P. Cellular and subbasal nerve alterations in early stage Fuchs’ endothelial corneal dystrophy: An in vivo confocal microscopy study. Eye 2013, 27, 42–49. [Google Scholar] [CrossRef]
- Klais, C.M.; Bühren, J.; Kohnen, T. Comparison of endothelial cell count using confocal and contact specular microscopy. Ophthalmologica 2003, 217, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Salvetat, M.L.; Zeppieri, M.; Miani, F.; Parisi, L.; Felletti, M.; Brusini, P. Comparison between laser scanning in vivo confocal microscopy and noncontact specular microscopy in assessing corneal endothelial cell density and central corneal thickness. Cornea 2011, 30, 754–759. [Google Scholar] [CrossRef] [PubMed]
- Kitzmann, A.S.; Winter, E.J.; Nau, C.B.; McLaren, J.W.; Hodge, D.O.; Bourne, W.M. Comparison of corneal endothelial cell images from a noncontact specular microscope and a scanning confocal microscope. Cornea 2005, 24, 980–984. [Google Scholar] [CrossRef] [PubMed]
- Ong Tone, S.; Bruha, M.J.; Böhm, M.; Prescott, C.; Jurkunas, U. Regional variability in corneal endothelial cell density between guttae and non-guttae areas in Fuchs endothelial corneal dystrophy. Can. J. Ophthalmol. 2019, 54, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Maram, J.; Tepelus, T.C.; Sadda, S.R.; Chopra, V.; Lee, O.L. Comparison of Noncontact Specular and Confocal Microscopy for Evaluation of Corneal Endothelium. Eye Contact Lens 2018, 44 (Suppl. S1), S144–S150. [Google Scholar] [CrossRef] [PubMed]
- Syed, Z.A.; Tran, J.A.; Jurkunas, U.V. Peripheral Endothelial Cell Count Is a Predictor of Disease Severity in Advanced Fuchs Endothelial Corneal Dystrophy. Cornea 2017, 36, 1166–1171. [Google Scholar] [CrossRef] [PubMed]
- Baratz, K.H.; McLaren, J.W.; Maguire, L.J.; Patel, S.V. Corneal haze determined by confocal microscopy 2 years after Descemet stripping with endothelial keratoplasty for Fuchs corneal dystrophy. Arch. Ophthalmol. 2012, 130, 868–874. [Google Scholar] [CrossRef]
- Patel, S.V.; McLaren, J.W. In vivo confocal microscopy of Fuchs endothelial dystrophy before and after endothelial keratoplasty. JAMA Ophthalmol. 2013, 131, 611–618. [Google Scholar] [CrossRef]
- Schiano-Lomoriello, D.; Abicca, I.; Bono, V.; Giannini, D.; Colabelli-Gisoldi, R.A.; Boni, N.; Komaiha, C.; Pocobelli, A. To compare corneal confocal microscopy of eyes with Fuchs’ endothelial corneal dystrophy after two different endothelial surgeries. Eur. J. Ophthalmol. 2022, 32, 866–874. [Google Scholar] [CrossRef]
- Aggarwal, S.; Cavalcanti, B.M.; Regali, L.; Cruzat, A.; Trinidad, M.; Williams, C.; Jurkunas, U.V.; Hamrah, P. In Vivo Confocal Microscopy Shows Alterations in Nerve Density and Dendritiform Cell Density in Fuchs’ Endothelial Corneal Dystrophy. Am. J. Ophthalmol. 2018, 196, 136–144. [Google Scholar] [CrossRef]
- Bucher, F.; Adler, W.; Lehmann, H.C.; Hos, D.; Steven, P.; Cursiefen, C.; Heindl, L.M. Corneal nerve alterations in different stages of Fuchs’ endothelial corneal dystrophy: An in vivo confocal microscopy study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 252, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Dikmetas, O.; Kocabeyoglu, S.; Mocan, M.C.; Karahan, S.; İrkec, M. The relationship between corneal subbasal nerve density and corneal sensitivity in patients with Fuchs endothelial corneal dystrophy. Indian J. Ophthalmol. 2021, 69, 1730–1734. [Google Scholar] [CrossRef]
- Gillings, M.; Mastro, A.; Zhang, X.; Kiser, K.; Gu, J.; Xing, C.; Robertson, D.M.; Petroll, W.M.; Mootha, V.V. Loss of Corneal Nerves and Corneal Haze in Patients with Fuchs’ Endothelial Corneal Dystrophy with the Transcription Factor 4 Gene Trinucleotide Repeat Expansion. Ophthalmol. Sci. 2023, 3, 100214. [Google Scholar] [CrossRef]
- Ahuja, Y.; Baratz, K.H.; McLaren, J.W.; Bourne, W.M.; Patel, S.V. Decreased corneal sensitivity and abnormal corneal nerves in Fuchs endothelial dystrophy. Cornea 2012, 31, 1257–1263. [Google Scholar] [CrossRef] [PubMed]
- Abicca, I.; Gilardi, M.; Giannini, D.; Colabelli Gisoldi, R.A.M.; Pocobelli, A.; Schiano Lomoriello, D. Corneal Subbasal Plexus in Eyes with Fuchs’ Endothelial Corneal Dystrophy after Two Different Endothelial Surgeries. J. Ophthalmol. 2021, 2021, 5098272. [Google Scholar] [CrossRef]
- Al-Fahdawi, S.; Qahwaji, R.; Al-Waisy, A.S.; Ipson, S.; Ferdousi, M.; Malik, R.A.; Brahma, A. A fully automated cell segmentation and morphometric parameter system for quantifying corneal endothelial cell morphology. Comput. Methods Programs Biomed. 2018, 160, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Qu, J.H.; Qin, X.R.; Peng, R.M.; Xiao, G.G.; Cheng, J.; Gu, S.F.; Wang, H.K.; Hong, J. A Fully Automated Segmentation and Morphometric Parameter Estimation System for Assessing Corneal Endothelial Cell Images. Am. J. Ophthalmol. 2022, 239, 142–153. [Google Scholar] [CrossRef]
- Villani, E.; Arita, R. Imaging of meibomian glands: From bench to bedside and back. Eye 2019, 33, 695–697. [Google Scholar] [CrossRef]
- Badian, R.A.; Allgeier, S.; Scarpa, F.; Andréasson, M.; Bartschat, A.; Mikut, R.; Colonna, A.; Bellisario, M.; Utheim, T.P.; Köhler, B.; et al. Wide-field mosaics of the corneal subbasal nerve plexus in Parkinson’s disease using in vivo confocal microscopy. Sci. Data 2021, 8, 306. [Google Scholar] [CrossRef]
- Badian, R.A.; Ekman, L.; Pripp, A.H.; Utheim, T.P.; Englund, E.; Dahlin, L.B.; Rolandsson, O.; Lagali, N. Comparison of Novel Wide-Field In Vivo Corneal Confocal Microscopy With Skin Biopsy for Assessing Peripheral Neuropathy in Type 2 Diabetes. Diabetes 2023, 72, 908–917. [Google Scholar] [CrossRef]
- Zhou, S.; Robertson, D.M. Wide-Field In Vivo Confocal Microscopy of Meibomian Gland Acini and Rete Ridges in the Eyelid Margin. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4249–4257. [Google Scholar] [CrossRef] [PubMed]
- Allgeier, S.; Bartschat, A.; Bohn, S.; Peschel, S.; Reichert, K.-M.; Sperlich, K.; Walckling, M.; Hagenmeyer, V.; Mikut, R.; Stachs, O.; et al. 3D confocal laser-scanning microscopy for large-area imaging of the corneal subbasal nerve plexus. Sci. Rep. 2018, 8, 7468. [Google Scholar] [CrossRef] [PubMed]
- Gottsch, J.D.; Sundin, O.H.; Rencs, E.V.; Emmert, D.G.; Stark, W.J.; Cheng, C.J.; Schmidt, G.W. Analysis and documentation of progression of Fuchs corneal dystrophy with retroillumination photography. Cornea 2006, 25, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Eghrari, A.O.; Garrett, B.S.; Mumtaz, A.A.; Edalati, A.E.; Meadows, D.N.; McGlumphy, E.J.; Iliff, B.W.; Gottsch, J.D. Retroillumination Photography Analysis Enhances Clinical Definition of Severe Fuchs Corneal Dystrophy. Cornea 2015, 34, 1623–1626. [Google Scholar] [CrossRef]
- Eghrari, A.O.; Mumtaz, A.A.; Garrett, B.; Rezaei, M.; Akhavan, M.S.; Riazuddin, S.A.; Gottsch, J.D. Automated Retroillumination Photography Analysis for Objective Assessment of Fuchs Corneal Dystrophy. Cornea 2017, 36, 44–47. [Google Scholar] [CrossRef]
- Soh, Y.Q.; Peh, G.S.L.; Naso, S.L.; Kocaba, V.; Mehta, J.S. Automated Clinical Assessment of Corneal Guttae in Fuchs Endothelial Corneal Dystrophy. Am. J. Ophthalmol. 2021, 221, 260–272. [Google Scholar] [CrossRef]

| Anterior Segment Optical Coherence Tomography | Scheimpflug Corneal Tomography | Specular Microscopy | In Vivo Confocal Microscopy | Retroillumination Photography | |
|---|---|---|---|---|---|
| Tomography of corneal layers | Possible | Possible | Not possible | Not possible | Not possible |
| Evaluation of changes of corneal curvature associated with FECD | Possible | Possible | Not possible | Not possible | Not possible |
| Visualization of corneal endothelial cells | Not possible | Not possible | Possible | Possible | Not possible |
| Measurement of endothelial cell density | Not possible | Not possible | Possible | Possible | Not possible |
| Visualization of guttae | Not possible | Not possible | Possible | Possible | Possible |
| Applicable in corneas with serious edema | Possible | Possible | Not possible | Possible | Not possible |
| Cost | Expensive | Expensive | Expensive | Expensive | Cheap |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.B.; Liu, Y.-C.; Liu, C.; Mehta, J.S. Applications of Imaging Technologies in Fuchs Endothelial Corneal Dystrophy: A Narrative Literature Review. Bioengineering 2024, 11, 271. https://doi.org/10.3390/bioengineering11030271
Han SB, Liu Y-C, Liu C, Mehta JS. Applications of Imaging Technologies in Fuchs Endothelial Corneal Dystrophy: A Narrative Literature Review. Bioengineering. 2024; 11(3):271. https://doi.org/10.3390/bioengineering11030271
Chicago/Turabian StyleHan, Sang Beom, Yu-Chi Liu, Chang Liu, and Jodhbir S. Mehta. 2024. "Applications of Imaging Technologies in Fuchs Endothelial Corneal Dystrophy: A Narrative Literature Review" Bioengineering 11, no. 3: 271. https://doi.org/10.3390/bioengineering11030271
APA StyleHan, S. B., Liu, Y.-C., Liu, C., & Mehta, J. S. (2024). Applications of Imaging Technologies in Fuchs Endothelial Corneal Dystrophy: A Narrative Literature Review. Bioengineering, 11(3), 271. https://doi.org/10.3390/bioengineering11030271








