Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography
Abstract
1. Introduction
2. Methods
2.1. Statement of Ethics
2.2. Participant and Eligibility Criteria
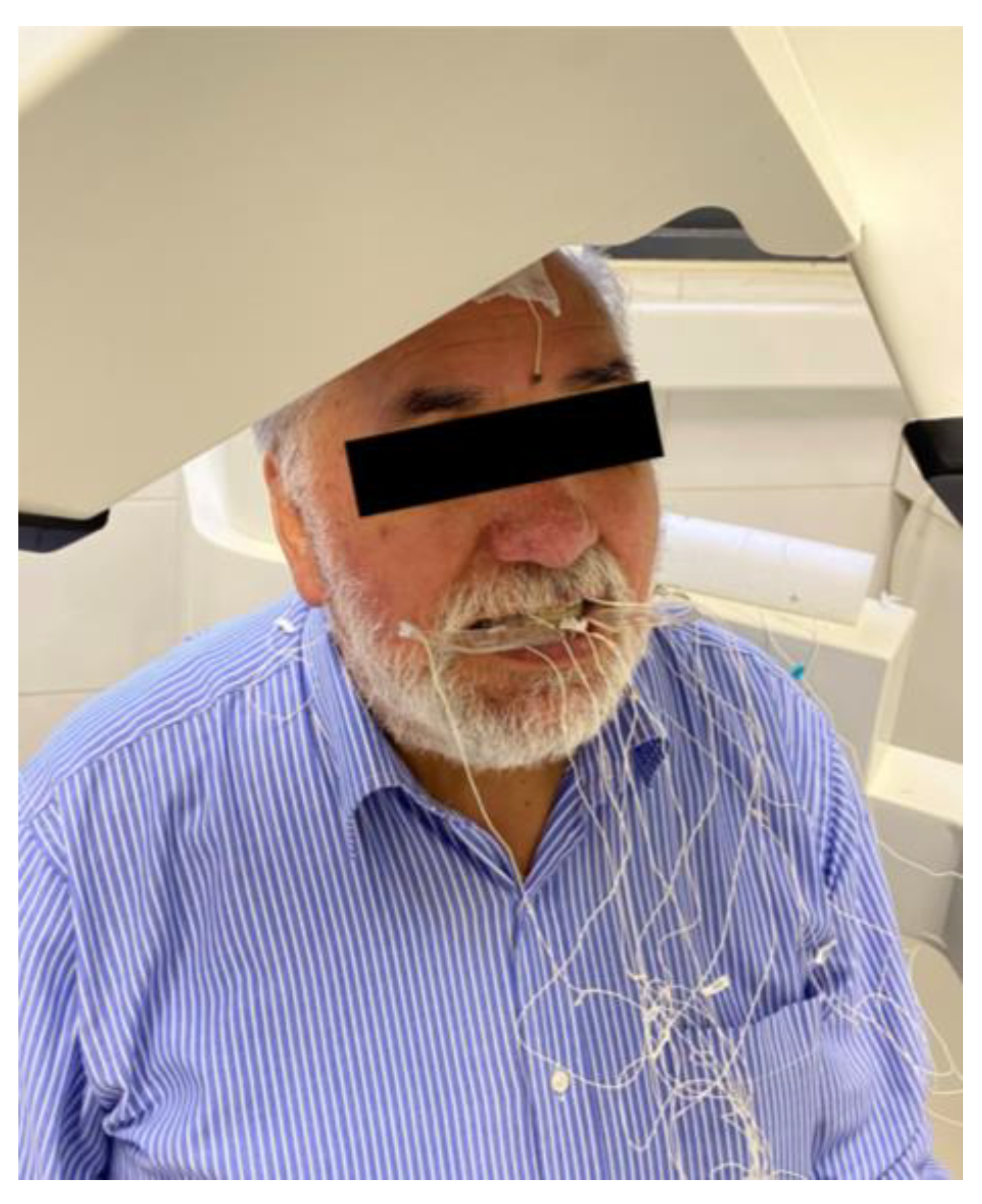
2.3. AG501 Electromagnetic Articulograph Description
2.4. Recording Method
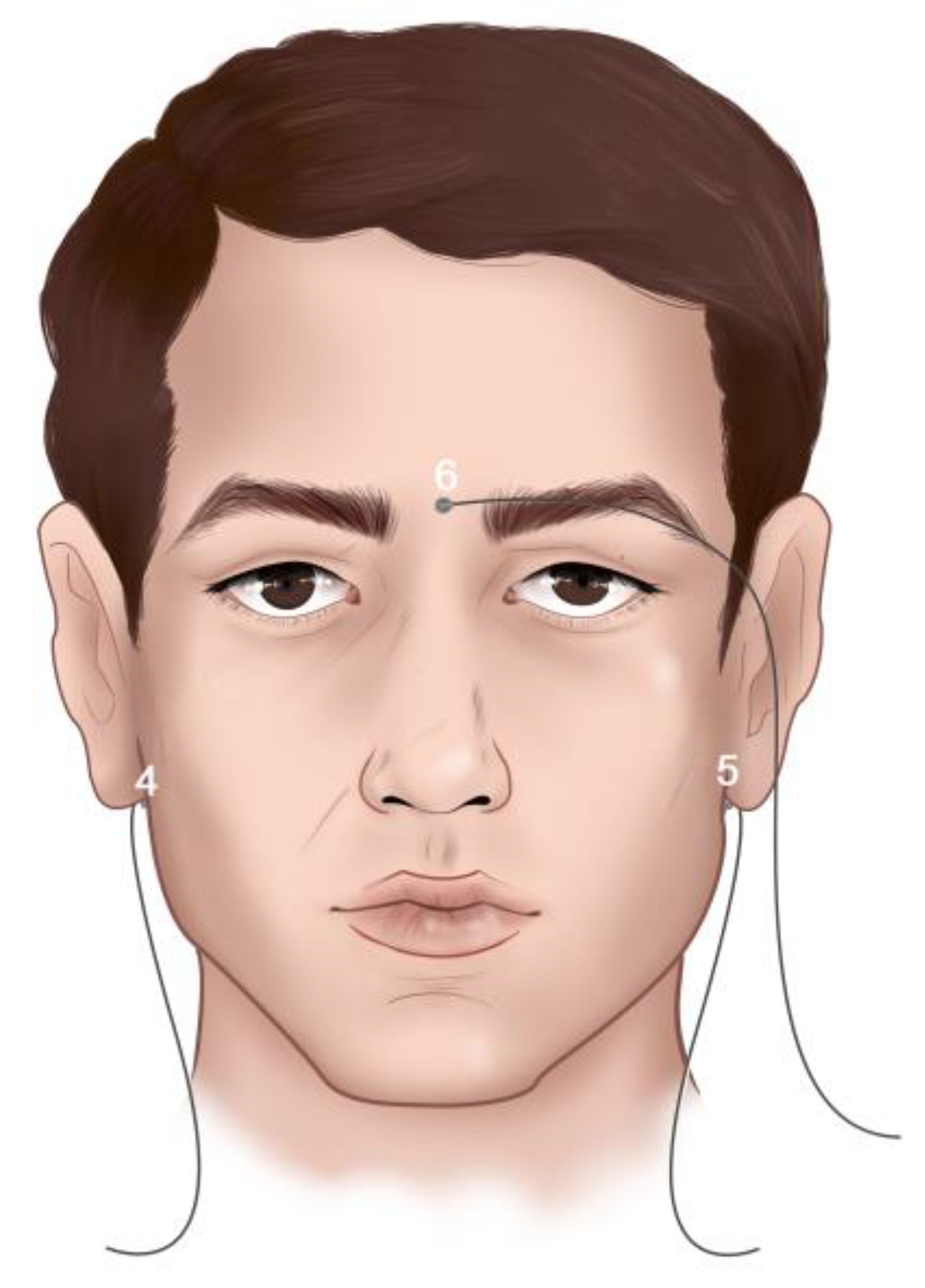
Location of EMA-3D Sensors
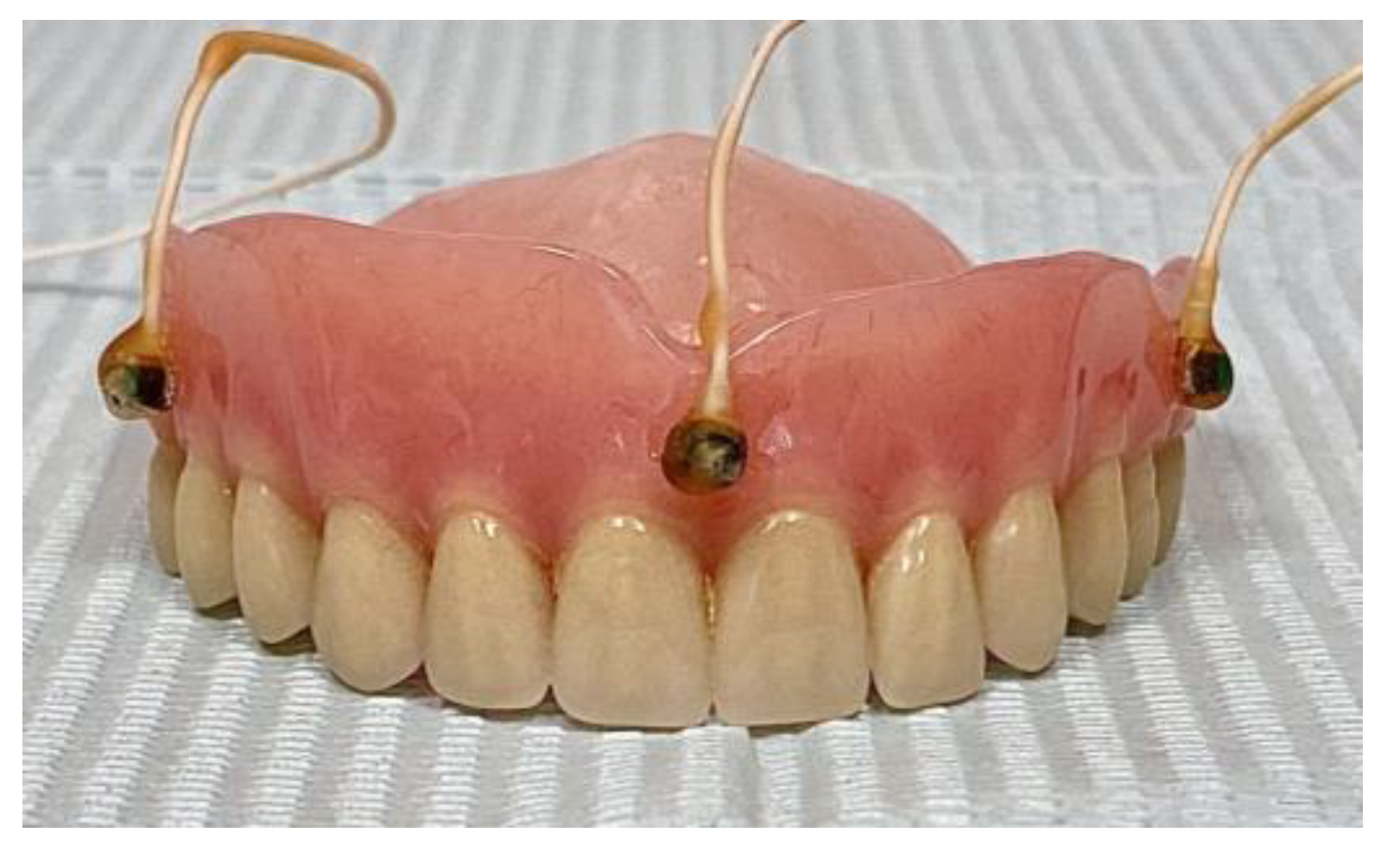
- Arrangement of sensors in the upper total removable prosthesis:
- Arrangement of sensors in the lower removable partial prosthesis:
2.5. Recordings
2.6. Data Processing
3. Results
3.1. Simultaneous Analysis of Upper Total Prosthesis and Lower Partial Prosthesis with a Metal Base
3.1.1. Interference Analysis of Sensors Located on Upper Total Prosthesis and Lower Partial Prosthesis Simultaneously in the Postural Position
3.1.2. Interference Analysis of Sensors Located on Upper Total Prosthesis and Lower Partial Prosthesis Simultaneously
3.1.3. Micromovement Analysis in Upper Total Prosthesis
3.1.4. Micromovement Analysis in Lower Partial Prosthesis
3.1.5. Tridimensional Movement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Belaúnde Gómez, M.A.; Salazar Silva, F.; Castillo-Andamayo, D.; Manrique Chávez, J.; Orejuela Ramírez, F.; Zavaleta Boza, C.; López Pinedo, M. Asociación Del Acceso a La Atención Dental y El Edentulismo. Rev. Estomatol. Hered. 2014, 22, 77. [Google Scholar] [CrossRef]
- Gutierrez-Vargas, V.L.; Leon-Manco, R.A.; Castillo-Andamayo, D.E. Edentulismo y Necesidad de Tratamiento Protésico En Adultos de Ámbito Urbano Marginal. Rev. Estomatol. Hered. 2015, 25, 179–186. [Google Scholar] [CrossRef]
- Müller, F.; Naharro, M.; Carlsson, G.E. What Are the Prevalence and Incidence of Tooth Loss in the Adult and Elderly Population in Europe? Clin. Oral. Implant. Res. 2007, 18, 2–14. [Google Scholar] [CrossRef] [PubMed]
- Arteaga, O.; Urzúa, I.; Espinoza, I.; Muñoz, A.; Mendoza, C.; Arteaga, O.; Urzúa, I.; Espinoza, I.; Muñoz, A.; Mendoza, C. Prevalencia de Caries y Pérdida de Dientes en Población de 65 a 74 Años de Santiago, Chile. Rev. Clínica Periodoncia Implantol. Y Rehabil. Oral 2009, 2, 161–166. [Google Scholar] [CrossRef][Green Version]
- Von Marttens, A.; Carvajal, J.; Leighton, Y.; Von Marttens, M.; Pinto, L. Experiencia y Significado Del Proceso de Edentulismo de Adultos Mayores, Atendidos En Un Consultorio Del Servicio Público Chileno. Rev. Clin. Periodoncia Implantol. Rehabil. Oral 2010, 3, 27–33. [Google Scholar] [CrossRef][Green Version]
- Sanz Fernández, G.; Llanes Molleda, C.; Gretel Chibás, L.; Valdés Valdés, Y. Consecuencias Del Edentulismo Total y Parcial En El Adulto Mayor. GeroInfo 2018, 13, 1–13. [Google Scholar]
- Douglass, C.W.; Watson, A.J. Future Needs for Fixed and Removable Partial Dentures in the United States. J. Prosthet. Dent. 2002, 87, 9–14. [Google Scholar] [CrossRef]
- The Academy of Prosthodontics. The Glossary of Prosthodontic Terms. J. Prosthet. Dent. 2017, 117, E1–E105. [Google Scholar] [CrossRef]
- Montero, J.; Castillo-Oyagüe, R.; Lynch, C.D.; Albaladejo, A.; Castaño, A. Self-Perceived Changes in Oral Health-Related Quality of Life after Receiving Different Types of Conventional Prosthetic Treatments: A Cohort Follow-up Study. J. Dent. 2013, 41, 493–503. [Google Scholar] [CrossRef]
- Gurevich, K.; Fabrikant, E.; Hassan, M.; Aqou, S. Oral Health–Related Quality of Life in Partially Edentulous Patients Treated with Removable, Fixed, Fixed-Removable, and Implant-Supported Prostheses. Int. J. Prosthodont. 2014, 27, 338–347. [Google Scholar] [CrossRef]
- De Andrade Lima Chaves, C.; Alves Gomes, E.; Faria, T.; Rocha Correa Da Silva, S.; De Souza Filho, C.B.; Borie, E.; Corrêa Silva Sousa, Y.T. Perfil de Los Pacientes Rehabilitados Por Medio de Prótesis Atendidos En Servicio Público de Salud En Ribeirão Preto, Brasil. Av. Odontoestomatol. 2015, 31, 347–353. [Google Scholar] [CrossRef]
- Reda, R.; Zanza, A.; Di Nardo, D.; Bellanova, V.; Xhajanka, E.; Testarelli, L. Implant Survival Rate and Prosthetic Complications of OT Equator Retained Maxillary Overdenture: A Cohort Study. Prosthesis 2022, 4, 730–738. [Google Scholar] [CrossRef]
- Guisard Silva, L.; Goldenberg, M. A Mastigação No Processo De Envelhecimento. Rev. Cefac 2001, 3, 27–35. [Google Scholar]
- Rendell, J.; Grasso, J.E.; Gay, T. Retention and Stability of the Maxillary Denture during Function. J. Prosthet. Dent. 1995, 73, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Compagnoni, M.A.; Souza, R.F.D.; Leles, C.R. Kinesiographic Study of Complete Denture Movement Related to Mucosa Displacement in Edentulous Patients. Pesqui. Odontol. Bras. 2003, 17, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Hoke, P.; Tiede, M.; Grender, J.; Klukowska, M.; Peters, J.; Carr, G. Using Electromagnetic Articulography to Measure Denture Micromovement during Chewing with and without Denture Adhesive. J. Prosthodont. 2019, 28, e252–e258. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, R.; Dias, F.; Álvarez, G.; Lezcano, M.F.; Farfán, C.; Astete, N.; Arias, A. Application of 3D Electromagnetic Articulography in Dentistry: Mastication and Deglutition Analysis. Protocol Report. Int. J. Odontostomat. 2018, 12, 105–112. [Google Scholar] [CrossRef][Green Version]
- Álvarez, G.; Dias, F.J.; Lezcano, M.F.; Arias, A.; Fuentes, R. A Novel Three-Dimensional Analysis of Tongue Movement during Water and Saliva Deglutition: A Preliminary Study on Swallowing Patterns. Dysphagia 2019, 34, 397–406. [Google Scholar] [CrossRef]
- Mefferd, A.S. Tongue- and Jaw-Specific Contributions to Acoustic Vowel Contrast Changes in the Diphthong /Ai/ in Response to Slow, Loud, and Clear Speech. J. Speech Lang. Hear. Res. 2017, 60, 3144–3158. [Google Scholar] [CrossRef]
- Rebernik, T.; Jacobi, J.; Jonkers, R.; Noiray, A.; Wieling, M. A Review of Data Collection Practices Using Electromagnetic Articulography. Lab. Phonol. J. Assoc. Lab. Phonol. 2021, 12, 6. [Google Scholar] [CrossRef]
- Temporomandibular Disorders: Guidelines for Classification, Assessment, and Management, American Academy of Orofacial Pain, McNeill, C., American Academy of Craniomandibular Disorders, Eds.; 2nd ed.; Quintessence Books: Chicago, IL, USA, 1993; ISBN 978-0-86715-253-1. [Google Scholar]
- Fuentes, R.; Arias, A.; Saravia, D.; Lezcano, M.F.; Dias, F.J. An Innovative Method to Analyse the Range of Border Mandibular Movements Using 3D Electromagnetic Articulography (AG501) and MATLAB. Biomed. Res. 2017, 28, 4239–4247. [Google Scholar]
- Hasegawa-Johnson, M. Electromagnetic Exposure Safety of the Carstens Aerticulograph AG100. J. Acoust. Soc. Am. 1998, 104, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Aasen, R. The Effects of Electromagnetic Fields on Cardiac Pacemakers. IEEE Trans. Broadcast. 1992, 38, 136–139. [Google Scholar] [CrossRef]
- Tognola, G.; Parazzini, M.; Sibella, F.; Paglialonga, A.; Ravazzani, P. Electromagnetic Interference and Cochlear Implants. Ann. Ist. Super. Sanita 2007, 43, 241–247. [Google Scholar] [PubMed]
- Zhang, Y.; Jones, P.L.; Jetley, R. A Hazard Analysis for a Generic Insulin Infusion Pump. J. Diabetes Sci. Technol. 2010, 4, 263–283. [Google Scholar] [CrossRef] [PubMed]
- Hoole, P.; Nguyen, N. Electromagnetic Articulography. In Coarticulation; Hardcastle, W.J., Hewlett, N., Eds.; Cambridge University Press: Cambridge, UK, 1999; pp. 260–269. ISBN 978-0-521-44027-1. [Google Scholar]
- AG501 Manual; Carstens Medizinelektronik GmbH: Göttingen, Germay, 2015.
- Gonçalves, T.M.S.V.; Vilanova, L.S.R.; Gonçalves, L.M.; Rodrigues Garcia, R.C.M. Effect of Complete and Partial Removable Dentures on Chewing Movements. J. Oral. Rehabil. 2014, 41, 177–183. [Google Scholar] [CrossRef] [PubMed]
- McCord, J.F.; Grant, A.A. Identification of Complete Denture Problems: A Summary. Br. Dent. J. 2000, 189, 128–134. [Google Scholar] [CrossRef]
- Jain, P.; Rathee, M. Stability in Mandibular Denture. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Čelebić, A.; Knezović-Zlatarić, D. A Comparison of Patient’s Satisfaction between Complete and Partial Removable Denture Wearers. J. Dent. 2003, 31, 445–451. [Google Scholar] [CrossRef]
- Milone, D.H. Introducción a las Señales y los Sistemas Discretos; Universidad Nacional de Entre Ríos: Concepción del Uruguay, Argentina, 2006; ISBN 978-950-698-173-0. [Google Scholar]
- Gower, J.G. Procrustes Analysis. In International Encyclopedia of the Social & Behavioral Sciences; Elsevier: Amsterdam, The Netherlands, 2001; pp. 12141–12143. ISBN 978-0-08-043076-8. [Google Scholar]
- Chew, C.L.; Boone, M.E.; Swartz, M.L.; Phillips, R.W. Denture Adhesives: Their Effects on Denture Retention and Stability. J. Dent. 1985, 13, 152–159. [Google Scholar] [CrossRef]
- Kapur, K.K. A Clinical Evaluation of Denture Adhesives. J. Prosthet. Dent. 1967, 18, 550–558. [Google Scholar] [CrossRef]
- Marin, D.O.M.; Leite, A.R.P.; Paleari, A.G.; Rodriguez, L.S.; Oliveira Junior, N.M.D.; Pero, A.C.; Compagnoni, M.A. Effect of a Denture Adhesive on the Satisfaction and Kinesiographic Parameters of Complete Denture Wearers: A Cross-Over Randomized Clinical Trial. Braz. Dent. J. 2014, 25, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Compagnoni, M.; Paleari, A.; Rodriguez, L.; Giro, G.; Mendoza Marin, D.; Pero, A. Impact of Replacing Conventional Complete Dentures with Implant-Supported Fixed Complete Dentures. Int. J. Periodontics Restor. Dent. 2014, 34, 833–839. [Google Scholar] [CrossRef] [PubMed]



| Distances between Pairs of Sensors in Prostheses (mm) | |||
|---|---|---|---|
| Sensor 1 | Sensor 2 | Mean Distance | Standard Deviation |
| ur | uc | 34.93 ± 0.05 | 0.02 ± 0.00 |
| uc | ul | 34.36 ± 0.09 | 0.02 ± 0.00 |
| ur | ul | 52.61 ± 0.03 | 0.02 ± 0.00 |
| lr | ll | 51.98 ± 0.03 | 0.02 ± 0.00 |
| Distances between Pairs of Sensors in Prostheses (mm) | |||
|---|---|---|---|
| Sensor 1 | Sensor 2 | Mean Distance | Standard Deviation |
| ur | uc | 34.86 ± 0.06 | 0.03 ± 0.01 |
| uc | ul | 34.46 ± 0.04 | 0.05 ± 0.02 |
| ur | ul | 52.62 ± 0.05 | 0.03 ± 0.01 |
| lr | ll | 52.02 ± 0.12 | 0.05 ± 0.02 |
| Micromovement of Upper Prosthesis (mm) | |
|---|---|
| Sensor | Standard Deviation of Sensor Position |
| ur | 0.74 ± 0.12 * |
| uc | 1.02 ± 0.13 * |
| ul | 0.63 ± 0.11 * |
| Micromovement of Upper Prosthesis (mm) | |
|---|---|
| Sensor | Standard Deviation of Sensor Position |
| il | 0.11 ± 0.03 |
| id | 0.12 ± 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marinelli, F.; Venegas, C.; Ruiz, J.V.; Farfán-Beltrán, N.; Staub, E.; Navarro, P.; Alarcón-Apablaza, J.; Fuentes, R. Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography. Bioengineering 2024, 11, 229. https://doi.org/10.3390/bioengineering11030229
Marinelli F, Venegas C, Ruiz JV, Farfán-Beltrán N, Staub E, Navarro P, Alarcón-Apablaza J, Fuentes R. Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography. Bioengineering. 2024; 11(3):229. https://doi.org/10.3390/bioengineering11030229
Chicago/Turabian StyleMarinelli, Franco, Camila Venegas, Joaquin Victorio Ruiz, Nicole Farfán-Beltrán, Erwin Staub, Pablo Navarro, Josefa Alarcón-Apablaza, and Ramón Fuentes. 2024. "Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography" Bioengineering 11, no. 3: 229. https://doi.org/10.3390/bioengineering11030229
APA StyleMarinelli, F., Venegas, C., Ruiz, J. V., Farfán-Beltrán, N., Staub, E., Navarro, P., Alarcón-Apablaza, J., & Fuentes, R. (2024). Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography. Bioengineering, 11(3), 229. https://doi.org/10.3390/bioengineering11030229






