Carotid Artery Bypass Surgery of In-Body Tissue Architecture-Induced Small-Diameter Biotube in a Goat Model: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
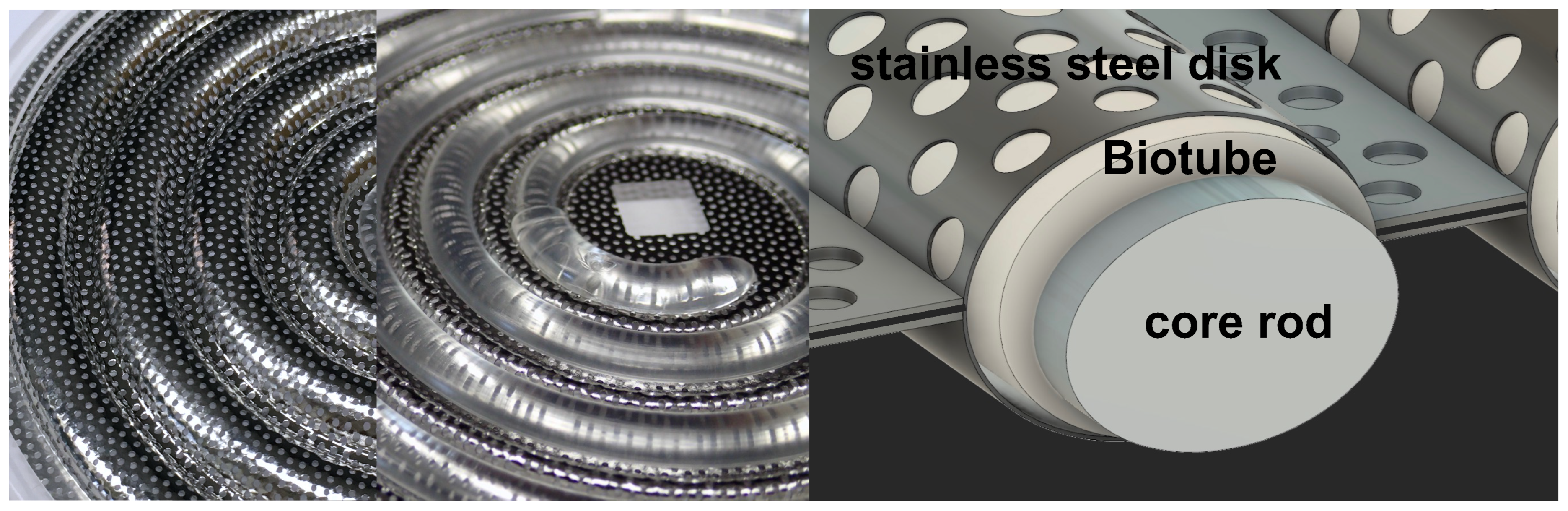
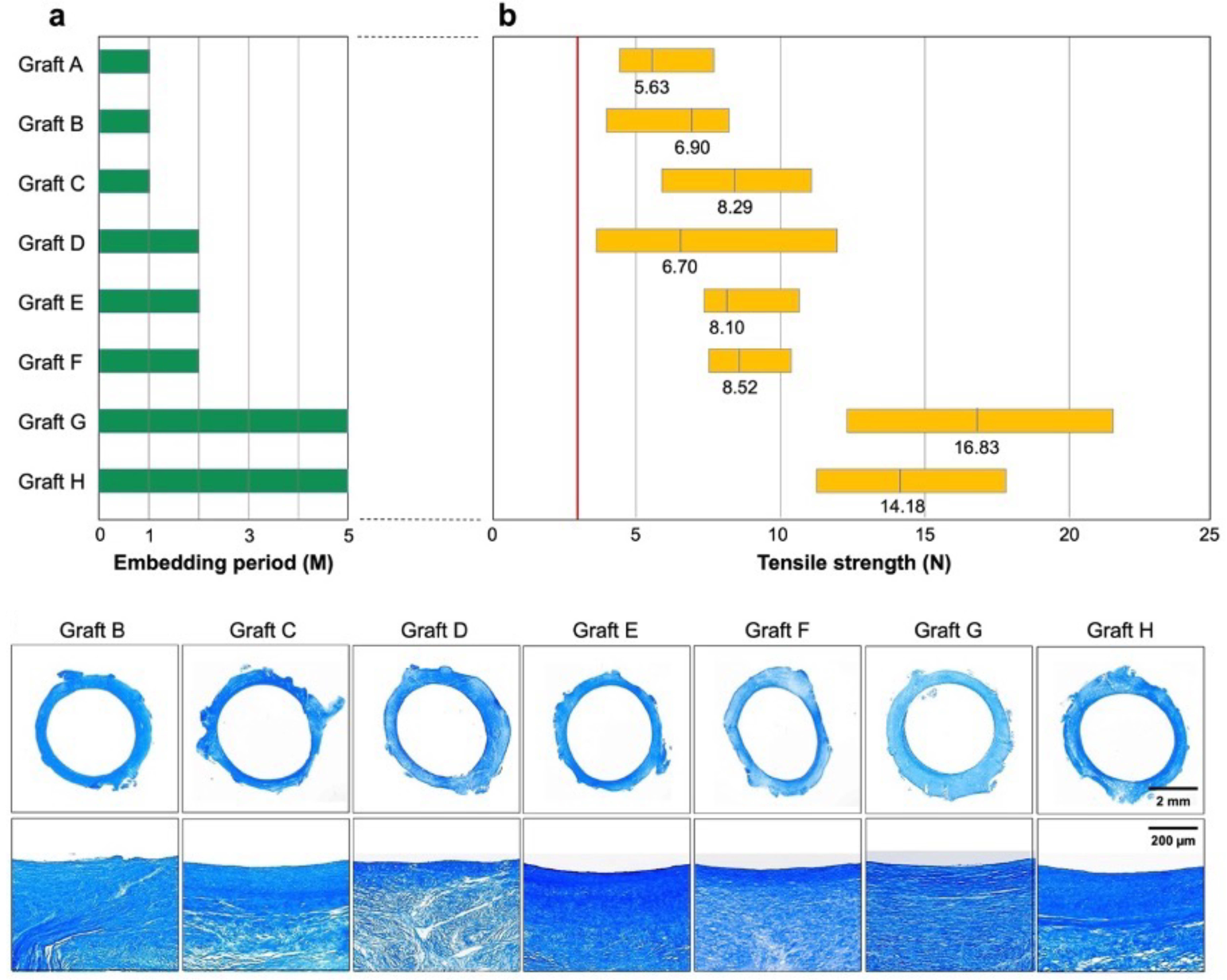
2.2. Preparation of Biotube
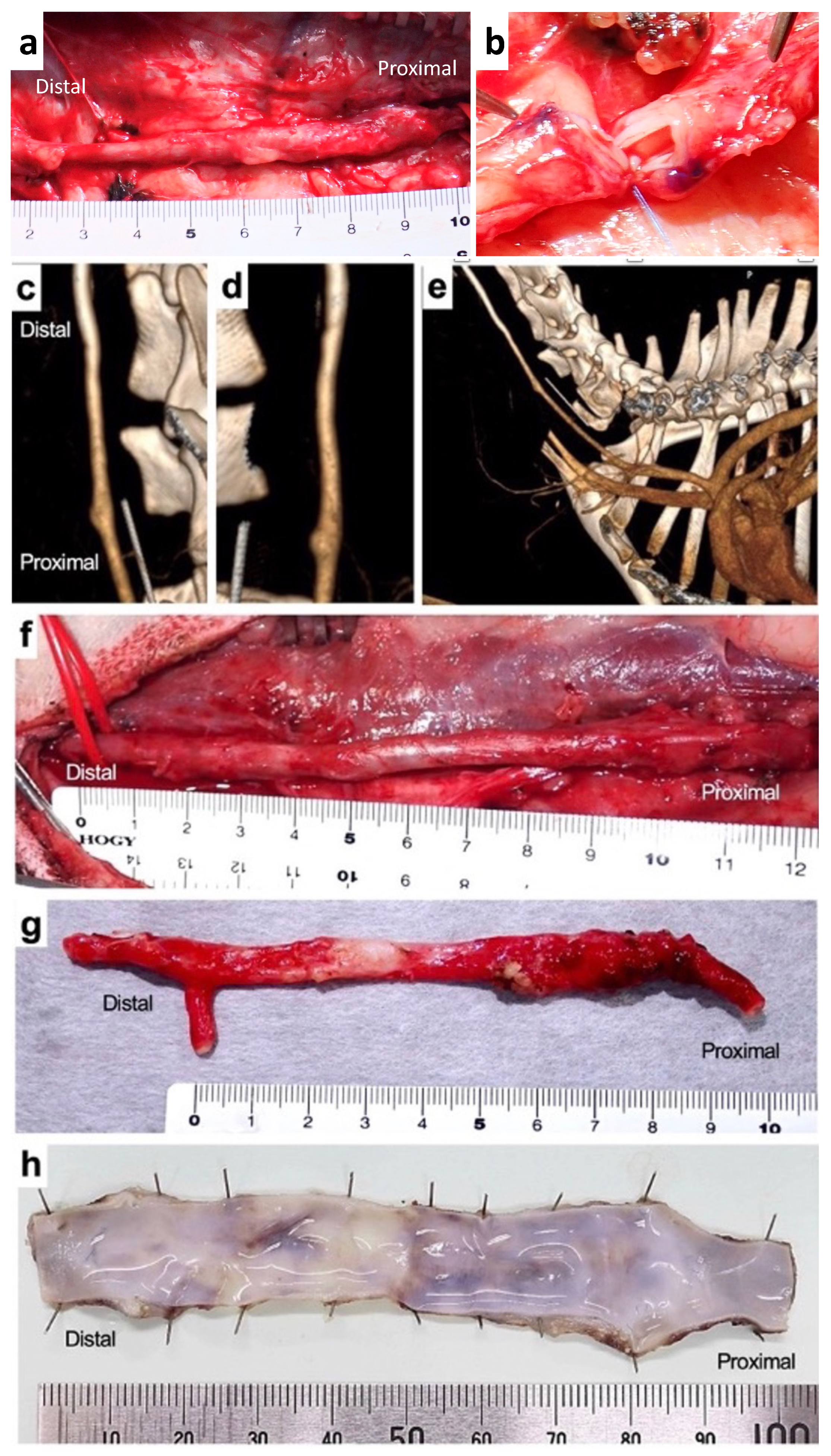
2.3. Surgical Procedures
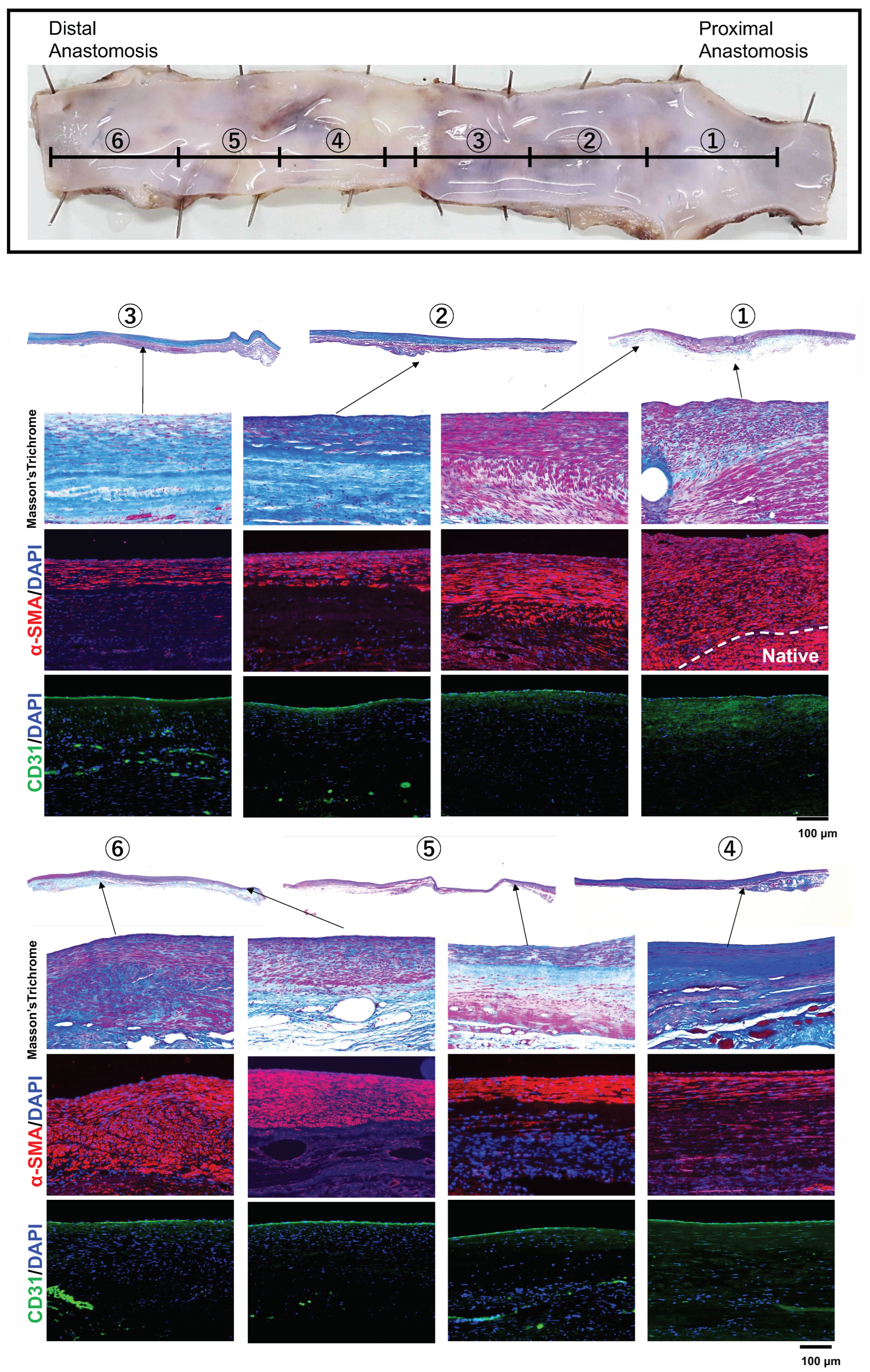
2.4. Histological Examination
3. Results
3.1. Preparation of Biotube
3.2. Implantation of Biotube
3.3. Histological Examination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017, 135, e726–e779. [Google Scholar]
- Bradbury, A.W.; Adam, D.J.; Bell, J.; Forbes, J.F.; Fowkes, F.G.R.; Gillespie, I.; Ruckley, C.V.; Raab, G.M.; BASIL Trial Participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL) trial: Analysis of amputation free and overall survival by treatment received. J. Vasc. Surg. 2010, 51, 18S–31S. [Google Scholar] [CrossRef]
- Pereira, C.E.; Albers, M.; Romiti, M.; Brochado-Neto, F.C.; Pereira, C.A. Meta-analysis of femoropopliteal bypass grafts for lower extremity arterial insufficiency. J. Vasc. Surg. 2006, 44, 510–517. [Google Scholar] [CrossRef]
- Sharrock, M.; Antoniou, S.A.; Antoniou, G.A. Vein versus prosthetic graft for femoropopliteal bypass above the knee: A systematic review and meta-analysis of randomized controlled trials. Angiology 2019, 70, 649–661. [Google Scholar] [CrossRef]
- Twine, C.P.; McLain, A.D. Graft type for femoro-popliteal bypass surgery. Cochrane Database Syst. Rev. 2010, 5, CD001487. [Google Scholar] [CrossRef] [PubMed]
- TASC Steering Committee; Jaff, M.R.; White, C.J.; Hiatt, W.R.; Fowkes, G.R.; Dormandy, J.; Razavi, M.; Reekers, J.; Norgren, L. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: A supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II). J. Endovasc. Ther. 2015, 22, 663–677. [Google Scholar] [CrossRef]
- Nakayama, Y.; Iwai, R.; Terazawa, T.; Tajikawa, T.; Umeno, T.; Kawashima, T.; Nakashima, Y.; Shiraishi, Y.; Yamada, A.; Higashita, R.; et al. Pre-implantation evaluation of a small-diameter, long vascular graft (Biotube®) for below-knee bypass surgery in goats. J. Biomed. Mater. Res. 2022, 110, 2387–2398. [Google Scholar] [CrossRef]
- Higashita, R.; Nakayama, Y.; Shiraishi, Y.; Iwai, R.; Inoue, Y.; Yamada, A.; Terazawa, T.; Tajikawa, T.; Miyazaki, M.; Ohara, M.; et al. Acute phase pilot evaluation of small diameter long iBTA induced vascular graft “Biotube” in a goat model. EJVES Vasc. Forum 2022, 54, 27–35. [Google Scholar] [CrossRef]
- Gutowski, P.; Gage, S.M.; Guziewicz, M.; Ilzecki, M.; Kazimierczak, A.; Kirkton, R.D.; Niklason, L.E.; Pilgrim, A.; Prichard, H.L.; Przywara, S.; et al. Arterial reconstruction with human bioengineered acellular blood vessels in patients with peripheral arterial disease. J. Vasc. Surg. 2020, 72, 1247–1258. [Google Scholar] [CrossRef]
- Kitsuka, T.; Hama, R.; Ulziibayar, A.; Matsuzaki, Y.; Kelly, J.; Shinoka, T. Clinical application for tissue engineering focused on materials. Biomedicines 2022, 10, 1439. [Google Scholar] [CrossRef]
- Nakayama, Y.; Kaneko, Y.; Takewa, Y.; Okumura, N. Mechanical properties of human autologous tubular connective tissues (human biotubes) obtained from patients undergoing peritoneal dialysis. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 104, 1431–1437. [Google Scholar] [CrossRef]
- Nakayama, Y.; Furukoshi, M.; Terazawa, T.; Iwai, R. Development of long in vivo tissue-engineered “Biotube” vascular grafts. Biomaterials 2018, 185, 232–239. [Google Scholar] [CrossRef]
- Fang, S.; Ellman, D.G.; Andersen, D.C. Review: Tissue engineering of small-diameter vascular grafts and their in vivo evaluation in large animals and humans. Cells 2021, 10, 713. [Google Scholar] [CrossRef]
- Skovrind, I.; Harvald, E.B.; Belling, H.J.; Jørgensen, C.D.; Lindholt, J.S.; Andersen, D.C. Concise review: Patency of small-diameter tissue-engineered vascular grafts: A meta-analysis of preclinical trials. Stem Cells Transl. Med. 2019, 8, 671–680. [Google Scholar] [CrossRef]
- Sakaue, T.; Koyama, T.; Nakamura, Y.; Okamoto, K.; Kawashima, T.; Umeno, T.; Nakayama, Y.; Miyamoto, S.; Shikata, F.; Hamaguchi, M.; et al. Bioprosthetic valve deterioration: Accumulation of circulating proteins and macrophages in the valve interstitium. JACC Basic Transl. Sci. 2023, 8, 862–880. [Google Scholar] [CrossRef]
- Rodriguez-Soto, M.A.; Vargas, N.S.; Riveros, A.; Camargo, C.M.; Cruz, J.C.; Sandoval, N.; Briceño, J.C. Failure analysis of TEVG’s I: Overcoming the initial stages of blood material interaction and stabilization of the immune response. Cells 2021, 10, 3140. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Soto, M.A.; Riveros, A.; Vargas, N.S.; Garcia-Brand, A.J.; Camatgo, C.M.; Cruz, J.C.; Sandval, N.; Briceño, J.C. Failure analysis of TEVG’s II: Late failure and entering the regeneration pathway. Cells 2022, 11, 939. [Google Scholar] [CrossRef] [PubMed]
- Beugels, J.; Molin, D.G.M.; Ophelders, D.R.M.G.; Rutten, T.; Kessels, L.; Kloosterboer, N.; Piatkowski de Grzymala, A.A.; Kramer, B.W.W.; van der Hulst, R.R.W.J.; Wolfs, T.G.A.M. Electrical stimulation promotes the angiogenic potential of adipose-derived stem cells. Sci. Rep. 2019, 9, 12076. [Google Scholar] [CrossRef] [PubMed]
- Zizhou, R.; Wang, X.; Houshyar, S. Review of polymeric biomimetic small-diameter vascular grafts to tackle intimal hyperplasia. ACS Omega 2022, 7, 22125–22148. [Google Scholar] [CrossRef] [PubMed]
- Donadoni, F.; Pichardo-Almarza, C.; Bartlett, M.; Dardik, A.; Homer-Vanniasinkam, S.; Díaz-Zuccarini, V. Patient-specific, multi-scale modeling of neointimal hyperplasia in vein grafts. Front. Physiol. 2017, 8, 226. [Google Scholar] [CrossRef] [PubMed]
- Donadoni, F.; Pichardo-Almarza, C.; Homer-Vanniasinkam, S.; Dardik, A.; Díaz-Zuccarini, V. Multiscale, patient-specific computational fluid dynamics models predict formation of neointimal hyperplasia in saphenous vein grafts. J. Vasc. Surg. Cases Innov. Tech. 2020, 6, 292–306. [Google Scholar] [CrossRef] [PubMed]
- Ivanova, Y.; Yukhnev, A.; Tikhomolova, L.; Smirnov, E.; Vrabiy, A.; Suprunovich, A.; Morozov, A.; Khubulava, G.; Vavilov, V. Experience of patient-specific CFD simulation of blood flow in proximal anastomosis for femoral-popliteal bypass. Fluids 2022, 7, 314. [Google Scholar] [CrossRef]
- Haruguchi, H.; Teraoka, S. Intimal hyperplasia and hemodynamic factors in arterial bypass and arteriovenous grafts: A review. J. Artif. Organs 2003, 6, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Sho, E.; Nanjo, H.; Sho, M.; Kobayashi, M.; Komatsu, M.; Kawamura, K.; Xu, C.; Zarins, C.K.; Masuda, H. Arterial enlargement, tortuosity, and intimal thickening in response to sequential exposure to high and low wall shear stress. J. Vasc. Surg. 2004, 39, 601–612. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Umeno, T.; Mori, K.; Iwai, R.; Kawashima, T.; Shuto, T.; Nakashima, Y.; Tajikawa, T.; Nakayama, Y.; Miyamoto, S. Carotid Artery Bypass Surgery of In-Body Tissue Architecture-Induced Small-Diameter Biotube in a Goat Model: A Pilot Study. Bioengineering 2024, 11, 203. https://doi.org/10.3390/bioengineering11030203
Umeno T, Mori K, Iwai R, Kawashima T, Shuto T, Nakashima Y, Tajikawa T, Nakayama Y, Miyamoto S. Carotid Artery Bypass Surgery of In-Body Tissue Architecture-Induced Small-Diameter Biotube in a Goat Model: A Pilot Study. Bioengineering. 2024; 11(3):203. https://doi.org/10.3390/bioengineering11030203
Chicago/Turabian StyleUmeno, Tadashi, Kazuki Mori, Ryosuke Iwai, Takayuki Kawashima, Takashi Shuto, Yumiko Nakashima, Tsutomu Tajikawa, Yasuhide Nakayama, and Shinji Miyamoto. 2024. "Carotid Artery Bypass Surgery of In-Body Tissue Architecture-Induced Small-Diameter Biotube in a Goat Model: A Pilot Study" Bioengineering 11, no. 3: 203. https://doi.org/10.3390/bioengineering11030203
APA StyleUmeno, T., Mori, K., Iwai, R., Kawashima, T., Shuto, T., Nakashima, Y., Tajikawa, T., Nakayama, Y., & Miyamoto, S. (2024). Carotid Artery Bypass Surgery of In-Body Tissue Architecture-Induced Small-Diameter Biotube in a Goat Model: A Pilot Study. Bioengineering, 11(3), 203. https://doi.org/10.3390/bioengineering11030203






