1. Introduction
In recent years, scoliosis has become more common in adolescents. If not detected and intervened in a timely manner, it can lead to serious deformities and cause visceral dysfunction [
1]. Scoliosis refers to the curvature of the back spine that deviates from the centerline of the trunk on one or both sides, forming an “S” or “C” shape [
2]. In the clinic, Cobb angle measurement of X-ray images is the “gold standard” to evaluate the severity of scoliosis in patients. The degree of scoliosis is mainly evaluated by doctors’ manual measurement [
3]. However, manual evaluation of the Cobb angle of scoliosis is time-consuming and has errors. The Cobb angle measured manually by the same doctor varies from 3 to 5, while it varies from 5 to 7 among different doctors [
4]. For inexperienced evaluators, the error may be higher. Nevertheless, X-ray examination is relatively simple; patients do not need to accept complicated preparation procedures, and the examination process is fast. Compared with other advanced imaging examination methods, X-ray examination has a lower cost and is more suitable as a preliminary screening tool. This makes it still the mainstream screening method at present. But the size of the Cobb angle is directly related to the choice of patients’ braces or the diagnosis and decision of surgery [
5]. Therefore, accurate automatic calculation and comprehensive evaluation of the Cobb angle are of great value in clinical practice.
Using computer vision technology and deep learning algorithms can effectively lower the threshold of scoliosis evaluation. At present, the spine X-ray image analysis method based on deep learning has made progress in the automatic evaluation of adolescent idiopathic scoliosis. By training a deep convolution neural network to detect vertebrae or segment vertebrae, the Cobb angle measurement can be realized, which greatly improves the evaluation efficiency of scoliosis severity [
6,
7]. However, based on X-ray examination, there is still radiation exposure, and it is not flexible in time and space, which limits its role in early screening of adolescent scoliosis and long-term dynamic evaluation of scoliosis patients.
In addition to X-ray films, there are several imaging methods that are considered relatively reliable. Multi-slice spiral Computed Tomography (CT) is a commonly used diagnostic examination method in clinical practice, and its accuracy is higher than that of the X-ray examination. But this method still produces radiation [
8]. Magnetic resonance imaging (MRI) technology is non-invasive and has high spatial resolution. It can not only clearly display the anatomical structure of bone, find the abnormal development of the vertebral body and its appendages, but also check whether the spinal cord is abnormal. It is of great value for preoperative diagnosis and postoperative review of scoliosis, but the cost is too high [
9]. Three-dimensional (3D) ultrasound technology can conveniently and intuitively display the shape of the spine, realize the visualization of the 3D shape of the spine, and accurately measure the curvature of the coronal plane and sagittal plane, so as to rotate axially to the vertebral body [
10].
Many studies have focused on using 3D scanning equipment to evaluate scoliosis. Fiona et al. developed a 3D measurement system, which consists of several high-precision sensors. By using non-contact 3D scanning technology, the 3D shape data of the back surface can be obtained by projecting a grating or a laser beam on the patient’s back and capturing the position information of the reflected light. Based on the extracted feature points, the system can calculate the key parameters, such as the bending angle and rotation degree of the spine, which provides a basis for subsequent evaluation and treatment [
11]. Alexander et al. designed a 3D body scanner equipped with an infrared sensor and video camera to capture the patient’s body image. Through biomechanical modeling, the biomechanical models of the rib cage and spinal column are simulated based on the finite element method to calculate and compare the specific spinal deformation of patients. It aims to be used as the supplementary information of Cobb angle for daily clinical evaluation of spinal deformation and may reduce the use of X-rays in a follow-up examination [
12].
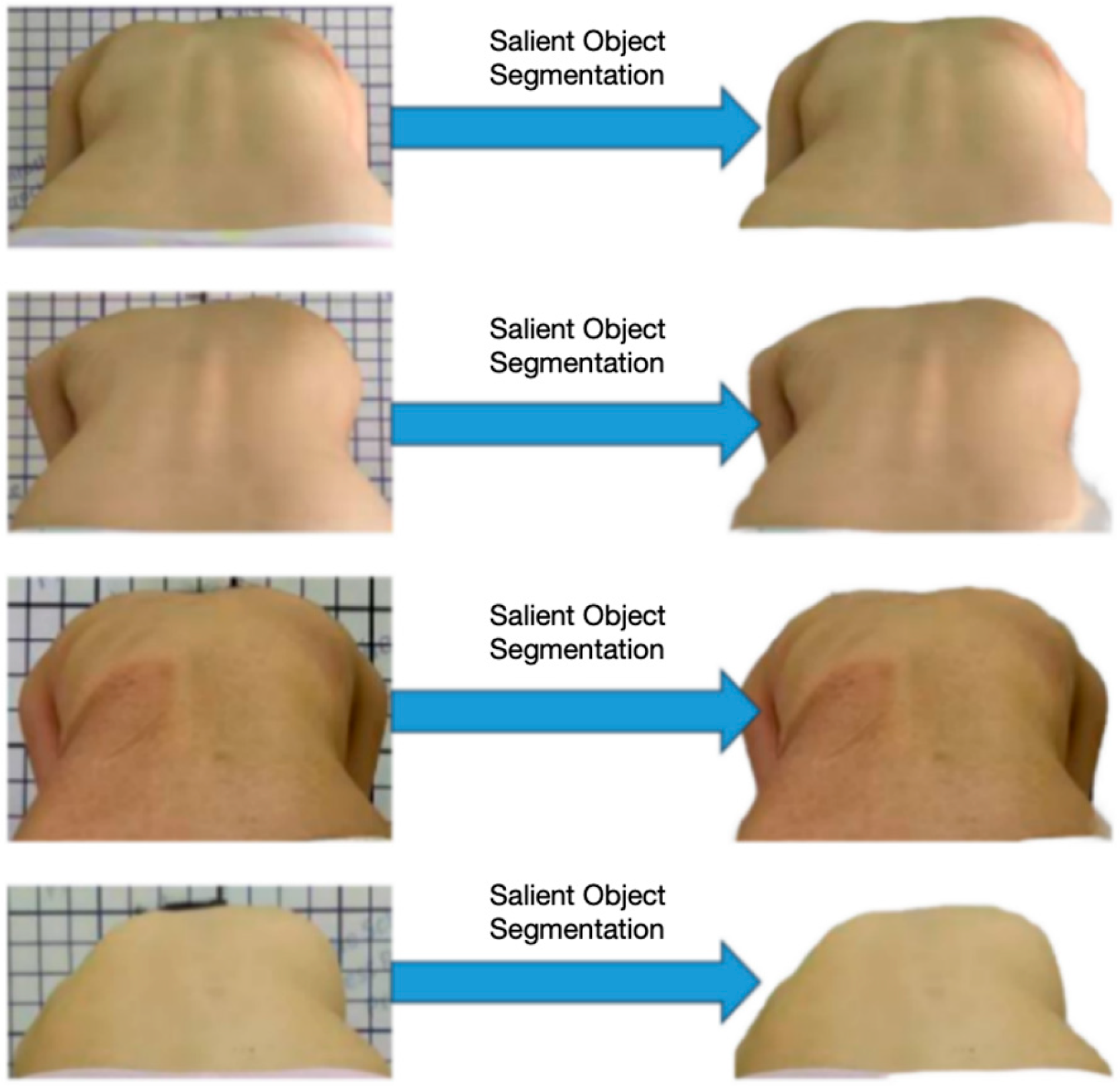
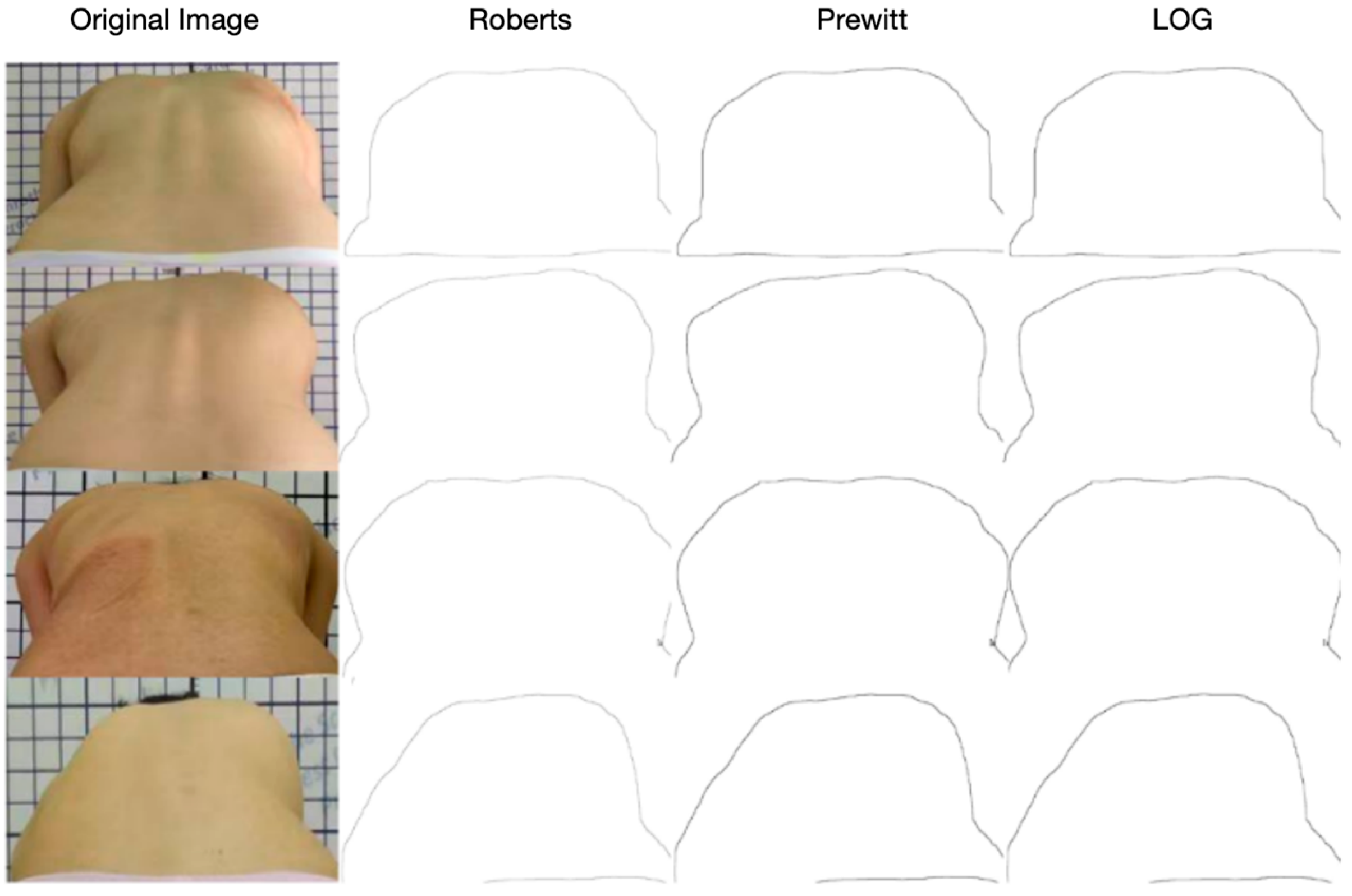
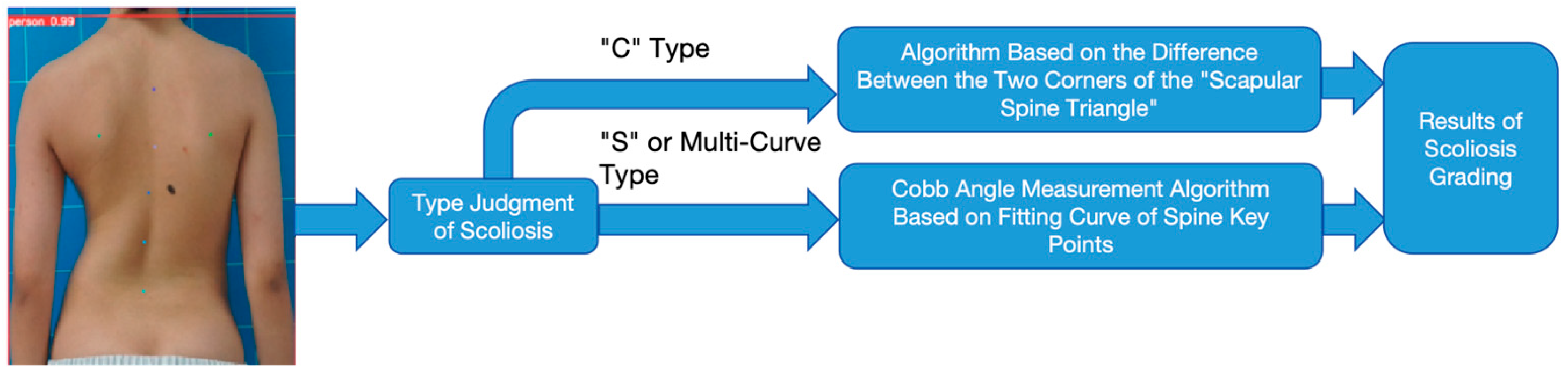
However, most of the above detection methods need to rely on professional equipment, which does not have the real-time and convenience of screening at home. Therefore, this paper aims to design a deep learning algorithm that can evaluate scoliosis without X-rays, only using the back photos in standing position and bare-back photos taken by mobile phones. The goal of this algorithm is to evaluate the severity of scoliosis more accurately than ordinary human doctors when only the image data of patients’ backs are available. This method can not only save medical resources, improve screening efficiency, and reduce radiation caused by routine X-ray follow-up but also realize home automatic identification of back photos taken by mobile phones and make a long-term, dynamic, and remote evaluation of the patient’s spine, which has important medical, economic, and social values.
The University of Hong Kong developed a virtual spine evaluation platform [
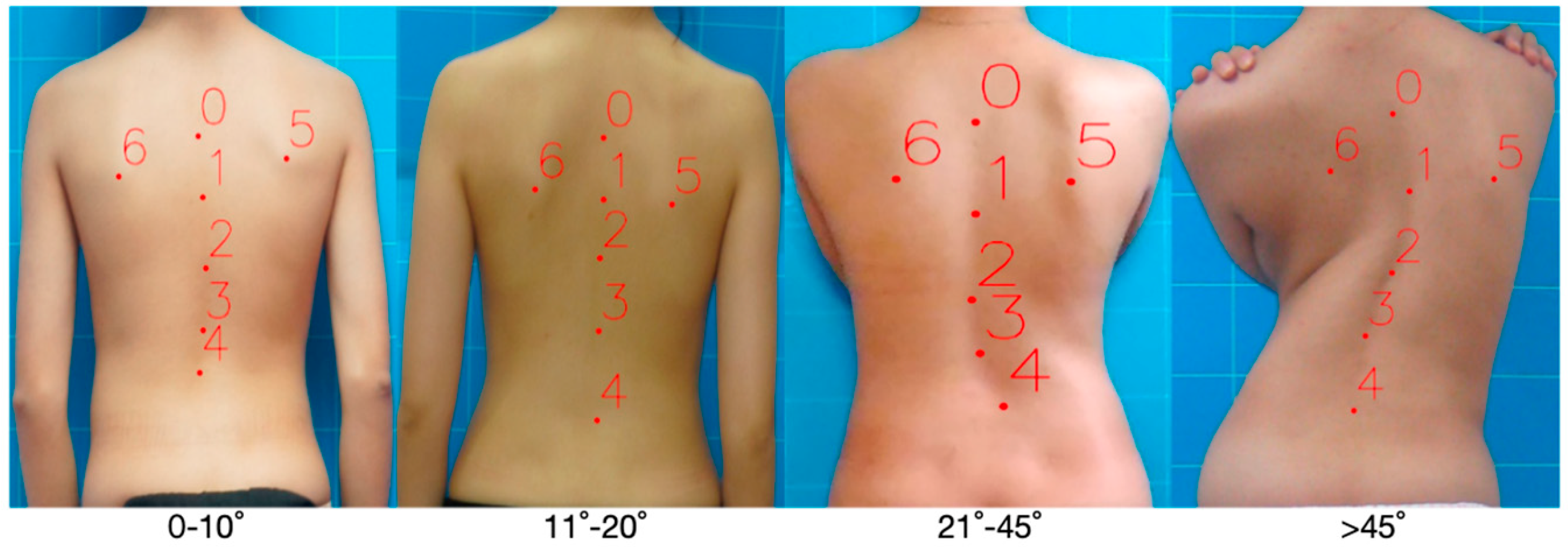
13]. The pictures of the human back collected by the mobile phone are used to evaluate the risk of spinal deformity and judge whether there is any progress in spinal deformity. Through three deep learning frameworks based on Visual Transformer, Residual Network, and Attention Mechanism, the platform receives photos as input to analyze the degree of scoliosis. The three-classification model is trained for severity classification, and the two-classification model is trained for the curve-type classification. Xinhua Hospital Affiliated with the Medical College of Shanghai Jiaotong University, proposed a scoliosis hierarchical depth learning algorithm for back photos. The algorithm flow is as follows: First, train the Faster-RCNN network to locate the key areas of the photographed human back photos. Then, for the photos of key back regions, the ResNet50 network is trained to realize four classifications of scoliosis angles (<10, 10–19, 20–44, ≥45). The accuracy of this method in the four classification tasks of scoliosis is 0.555, which is slightly lower than that of ordinary doctors (56.9%) [
14]. Subsequently, Xidian University improved the classification method of scoliosis on this basis. Three two-classification models of scoliosis are used to replace the traditional four-classification model, thus realizing a more simplified and effective identification of scoliosis diseases [
15].
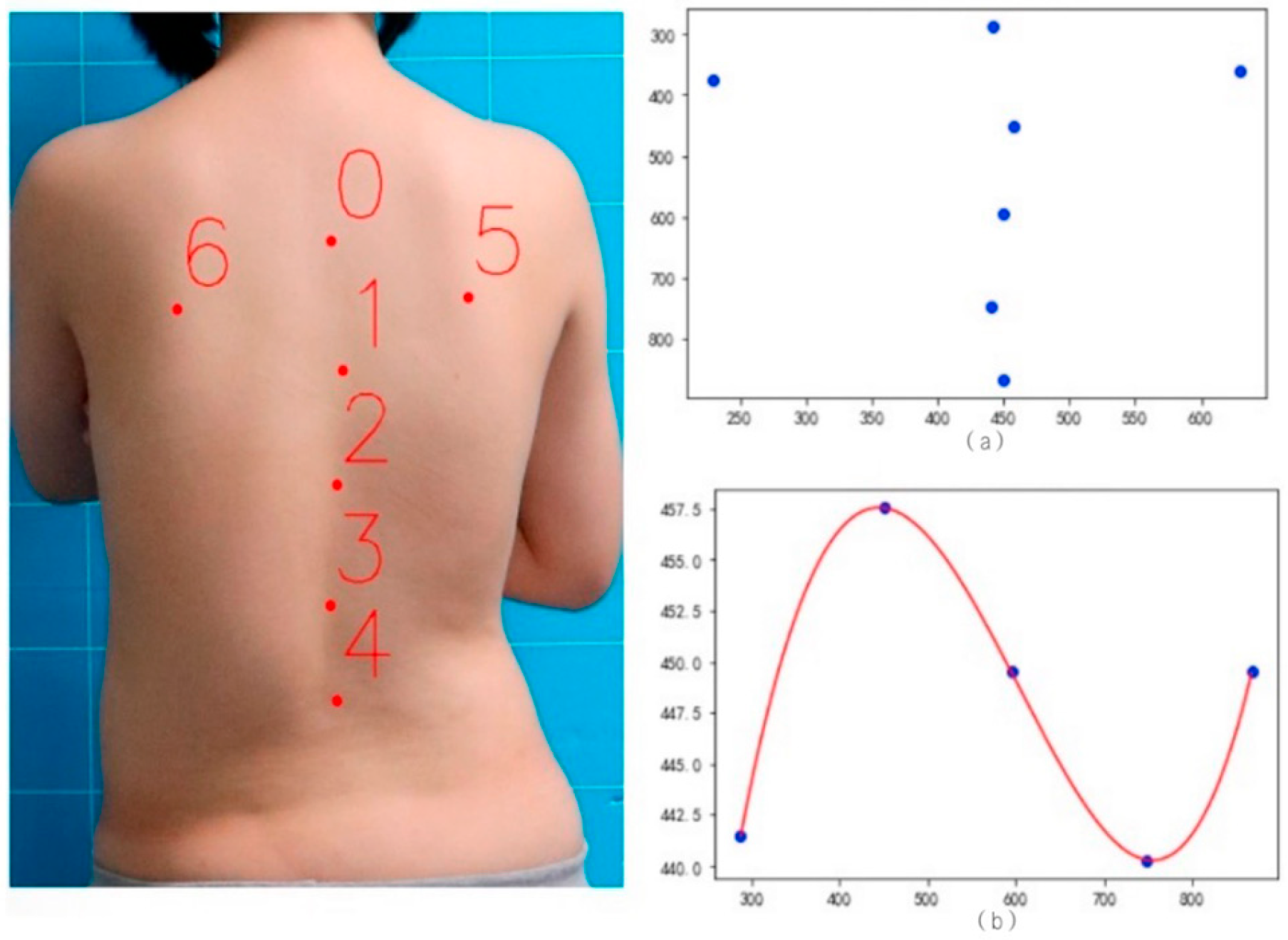
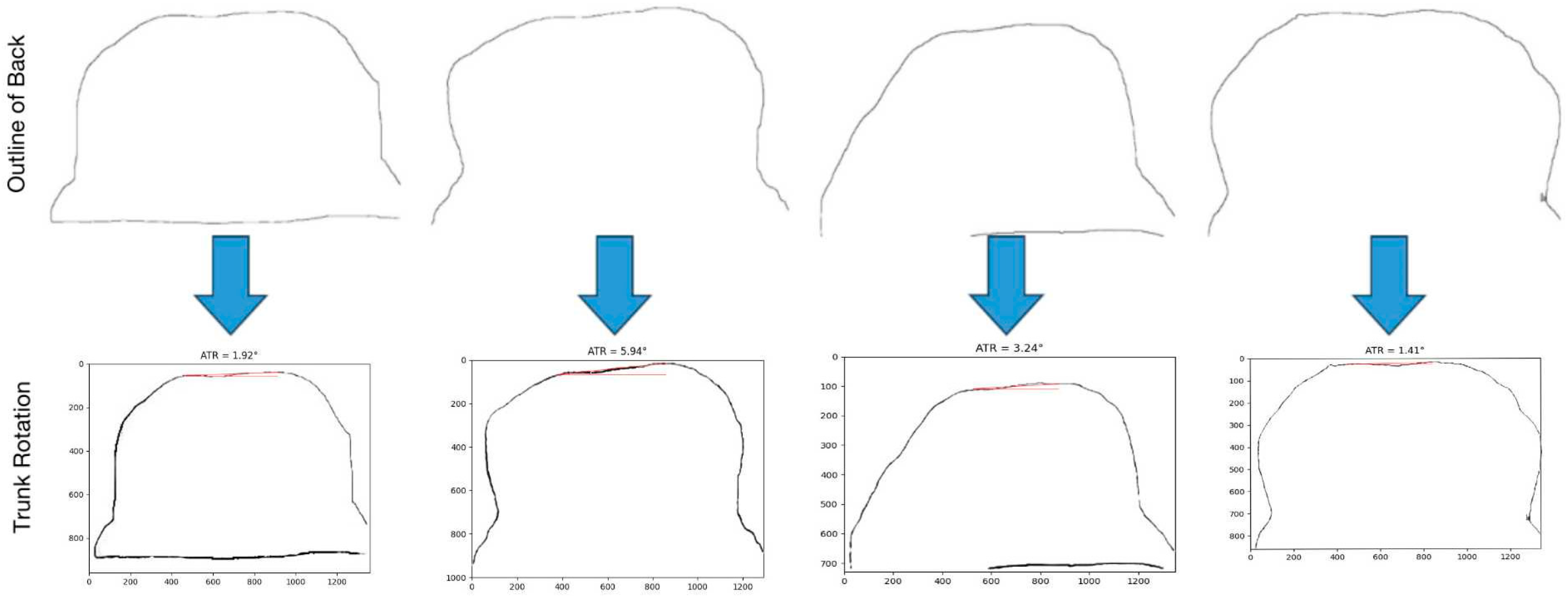
In structural scoliosis, the spine will be offset not only in the coronal plane but also in the sagittal plane [
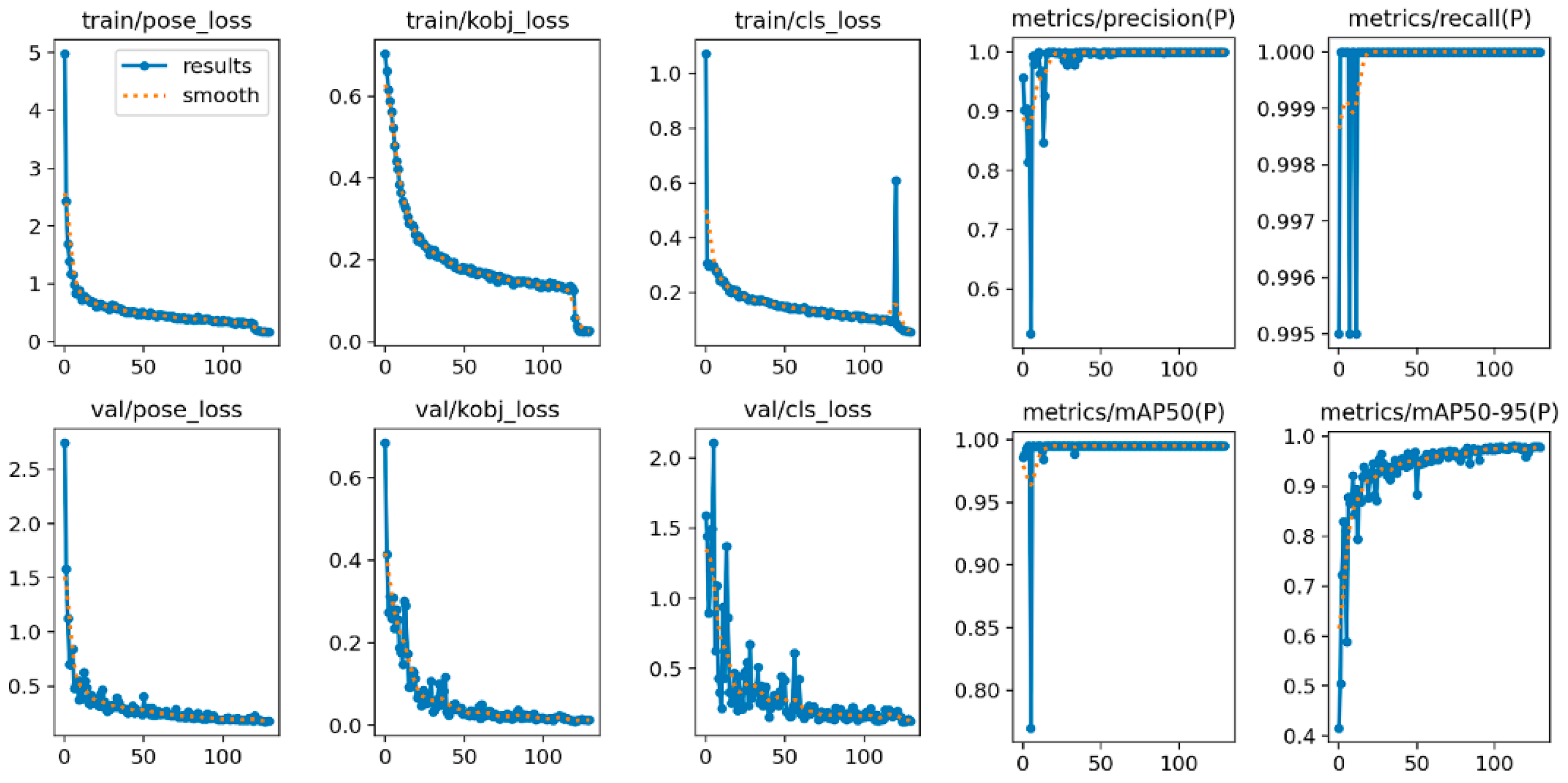
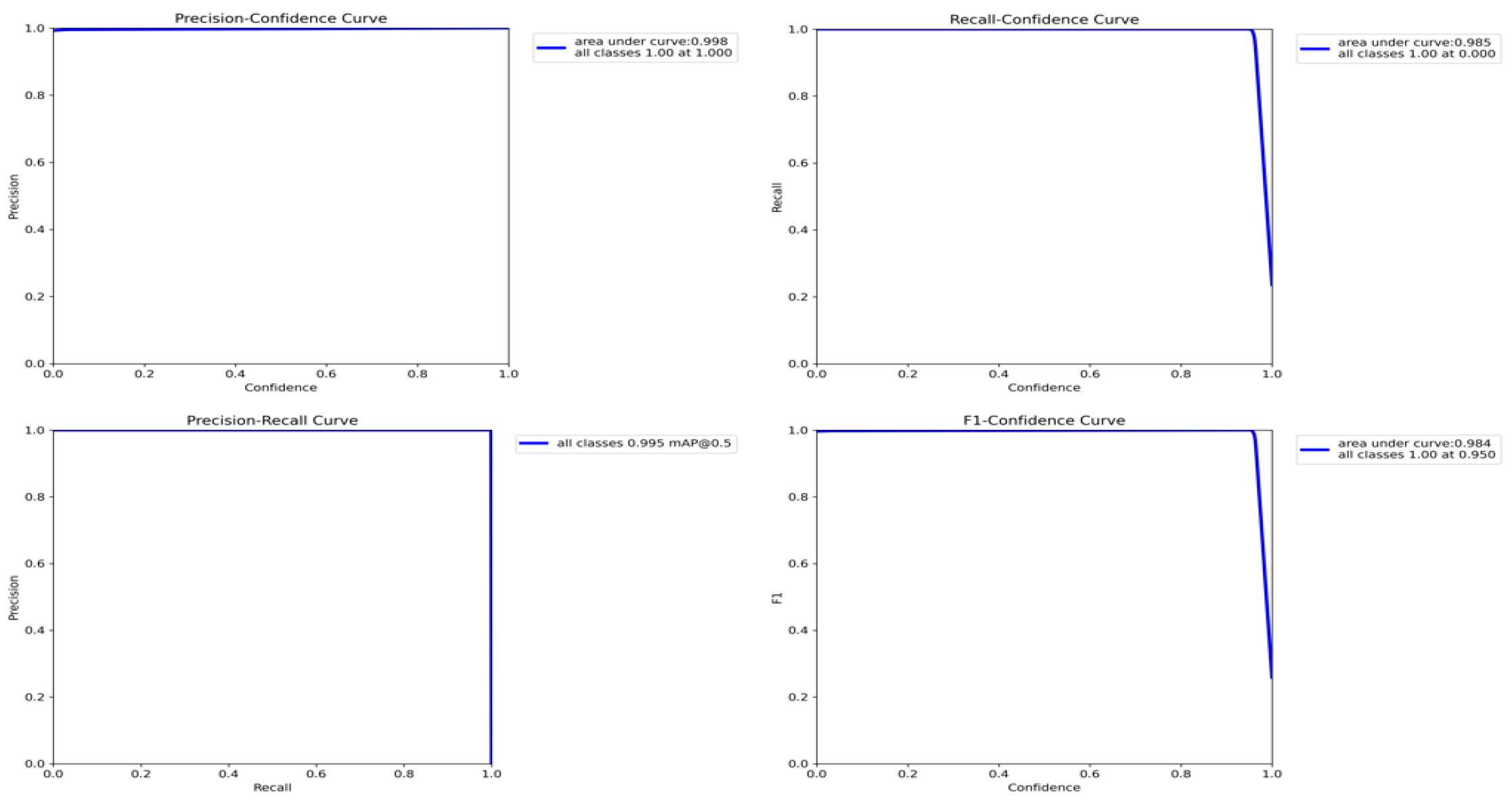
16]. Therefore, scoliosis must be regarded as a three-dimensional deformity of the spine and trunk, which may deteriorate rapidly during rapid growth. However, at present, the research pays more attention to the interval estimation of the deviation angle of the coronal plane of the spine but ignores the research on the types of spinal curvature and the degree of sagittal plane deviation of the spine. In this paper, a multi-dimensional scoliosis evaluation algorithm is designed and implemented using bare-back photos, including a trunk rotation measurement algorithm, spinal curvature type discrimination algorithm, and spinal coronal scoliosis severity classification algorithm, integrating doctors’ knowledge. Compared with the previous algorithms that only evaluated the degree of coronal deviation of the spine, this set of algorithms has higher reliability and improved the classification accuracy, recall rate, and F1-score. It can also be used for the long-term dynamic evaluation of scoliosis and visually show the changes in scoliosis during rehabilitation treatment.
4. Conclusions
For adolescent idiopathic scoliosis, we should find it as soon as possible and cooperate with doctors for conservative intervention when the Cobb angle is the smallest and flexibility is the best. In this paper, a new method, which does not need X-rays, is proposed, and a deep learning algorithm can be used to evaluate scoliosis in multiple dimensions only by taking bare photos of patients’ backs with mobile phones, which can accurately evaluate the severity of scoliosis, even better than the judgment of ordinary doctors. This method can realize automatic assessment of scoliosis at home, which can not only save medical resources but also reduce the frequency of patients receiving X-ray radiation.
The deep learning algorithm for multi-dimensional evaluation of scoliosis using bare-back photos proposed in this paper is different from previous studies that only focus on the coronal offset angle of the spine. In this paper, the trunk rotation measurement algorithm and the spine bending type discrimination algorithm are proposed for the first time. At the same time, combined with the doctor’s evaluation experience of scoliosis, this paper also puts forward an algorithm for grading the degree of scoliosis in the coronal plane. The classification accuracy of this algorithm exceeds the existing methods and is more interpretable.
In the future, the multi-dimensional scoliosis assessment algorithm can be deployed and applied, and an application program can be developed so that patients can upload pictures with one click and obtain scoliosis assessment results. With the continuous development of telemedicine technology, the following research will focus on establishing a remote monitoring and management system based on intelligent technology. Patients can carry out rehabilitation training through smart devices such as mobile phones and communicate with doctors in real time through the remote monitoring system. Doctors can keep abreast of patients’ rehabilitation progress and provide guidance, thus achieving more flexible and convenient rehabilitation management.