Assessment of Thermal Influence on an Orthodontic System by Means of the Finite Element Method
Abstract
1. Introduction
2. Materials and Methods
- -
- Direct engineering methods, which are included, in particular, in the SolidWorks program, which allow the generation of virtual objects similar to reality models, such as orthodontic wires or brackets and tube-type elements;
- -
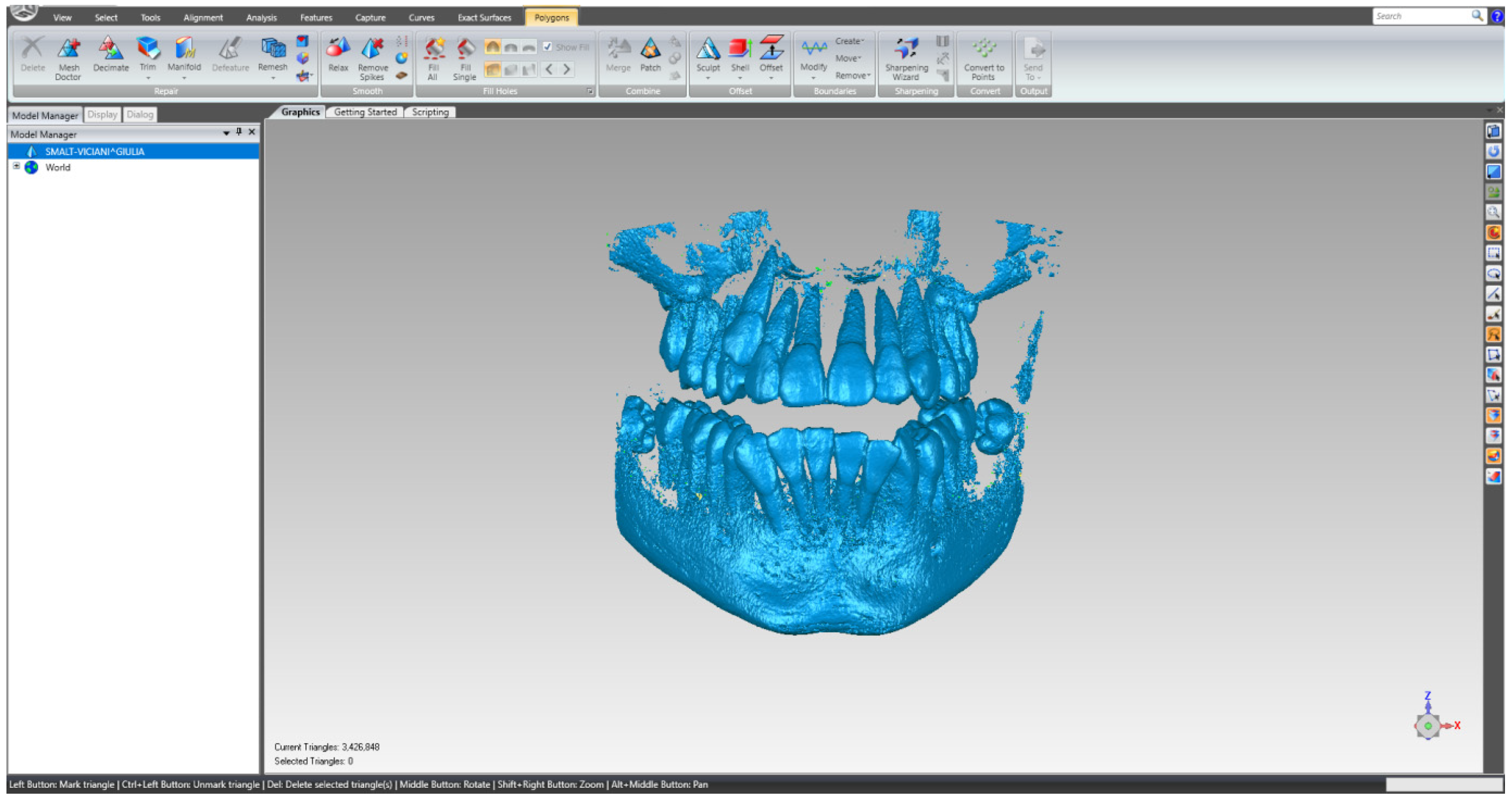
- Reverse Engineering methods, which are the basis of the Geomagic program, used for editing and preparing models that, initially, were composed of the so-called “clouds of points”;
- -
- Thermodynamics methods that were used to define the simulations made in Ansys Workbench;
- -
- Techniques specific to the finite element method that are the basis of the algorithms contained in the thermal modules of the Ansys program.
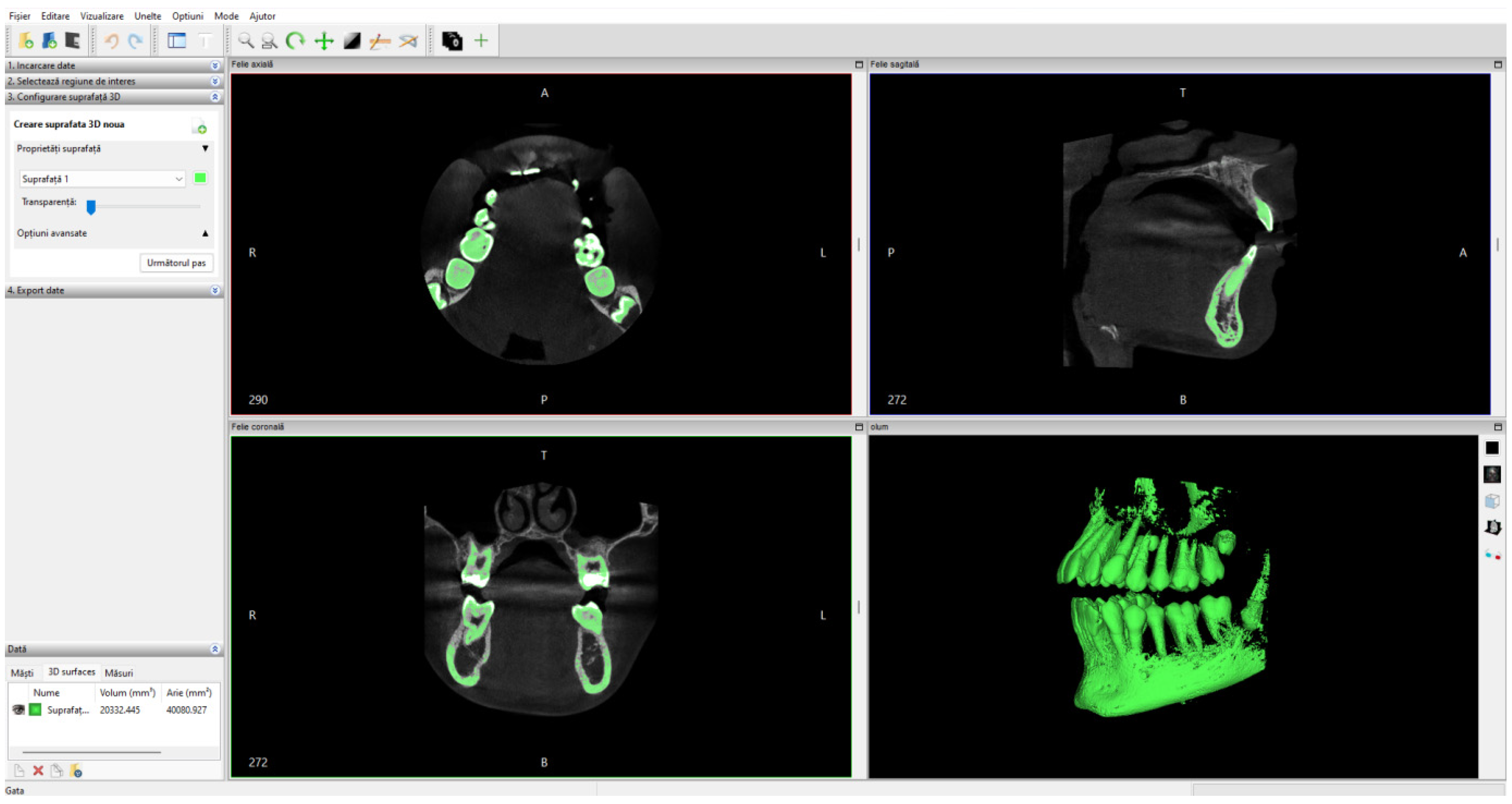
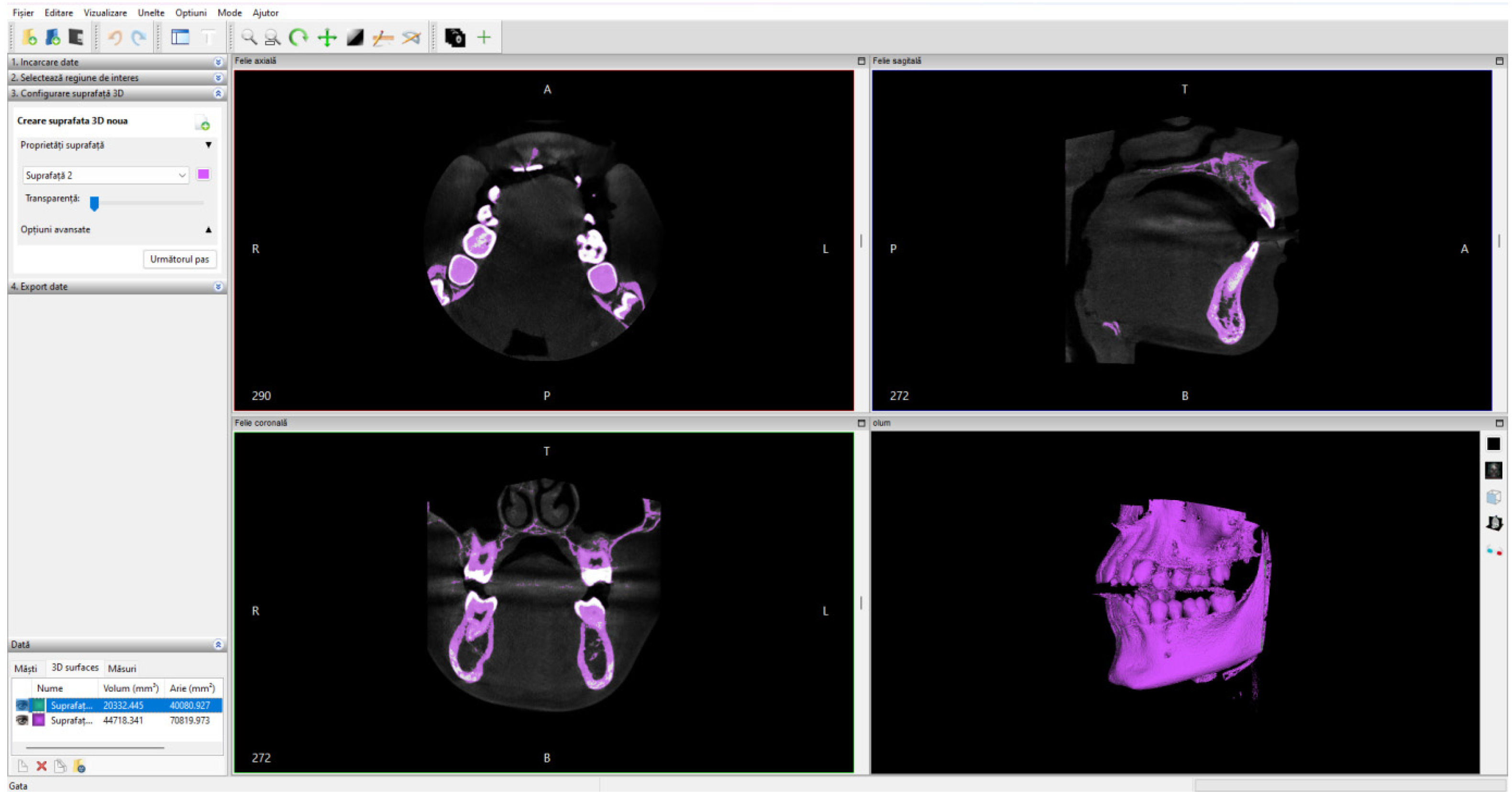
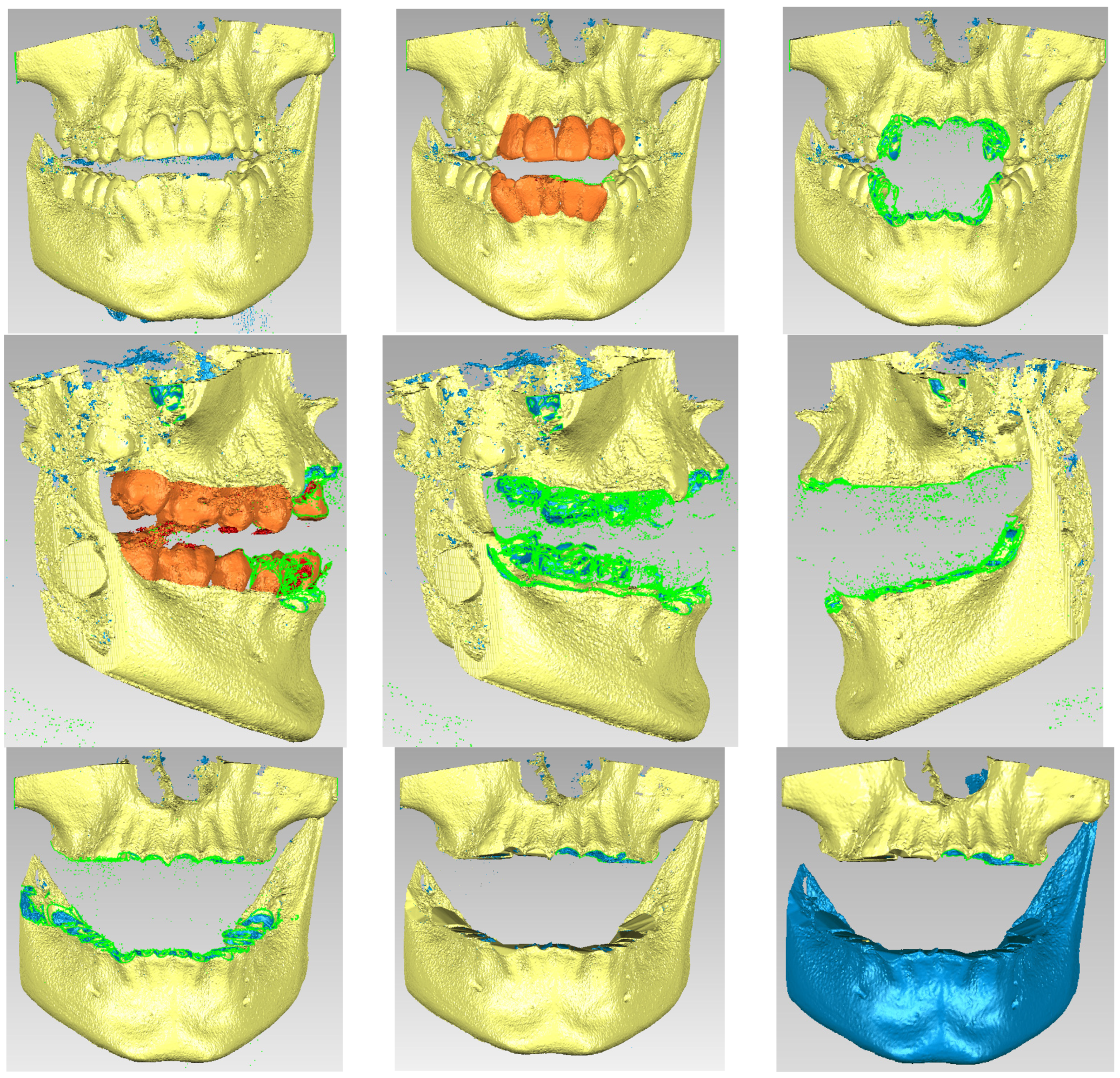
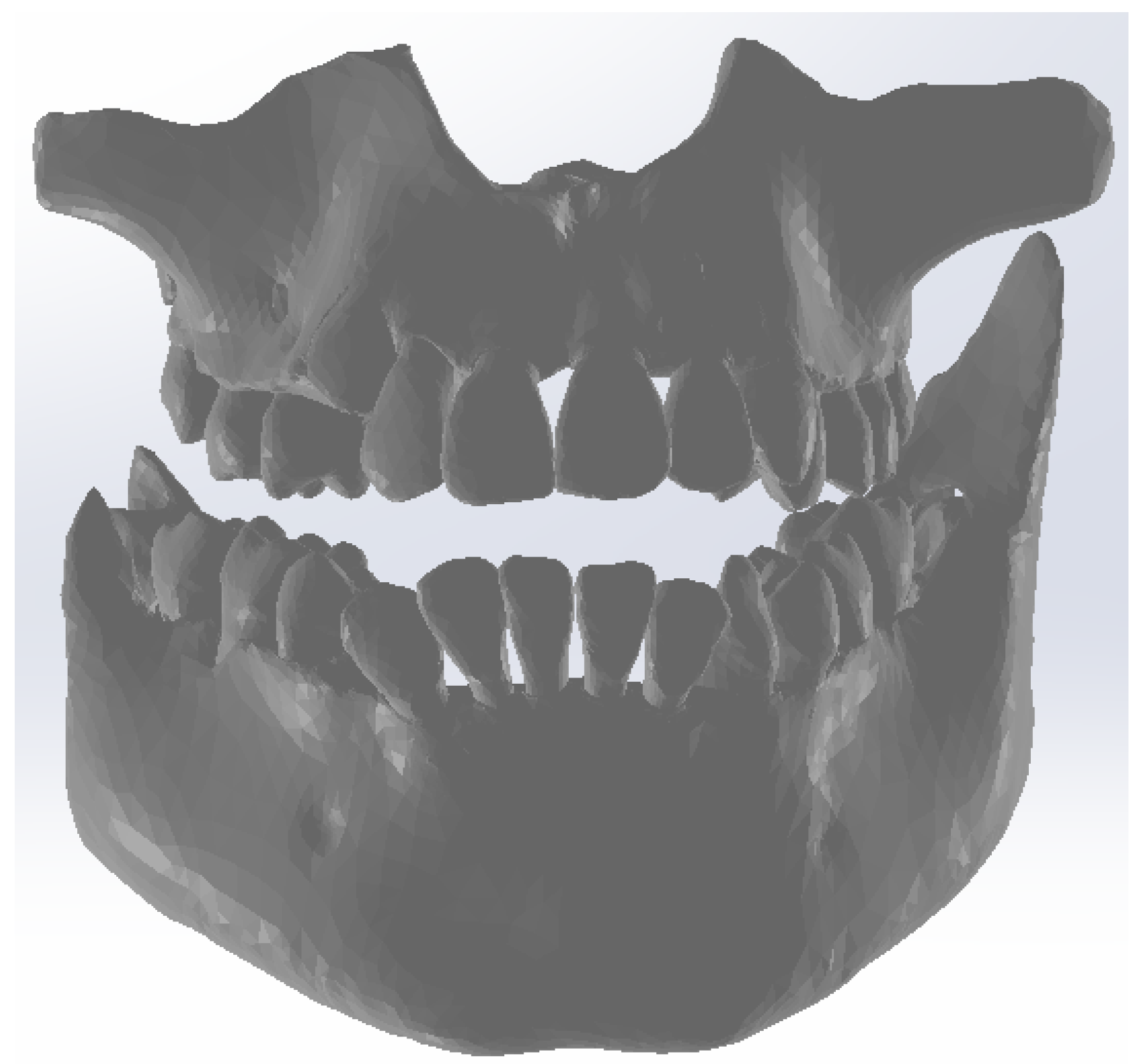
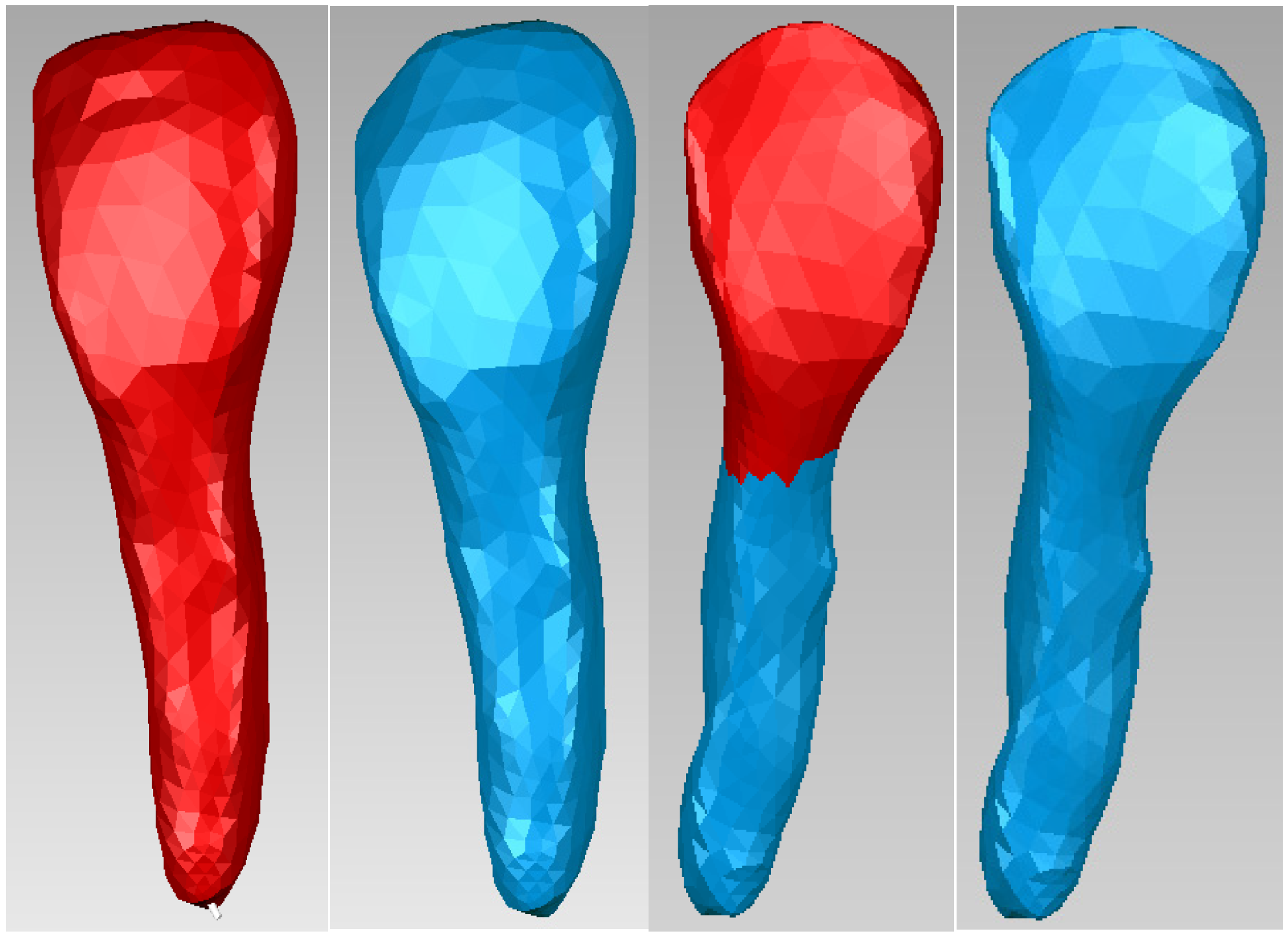
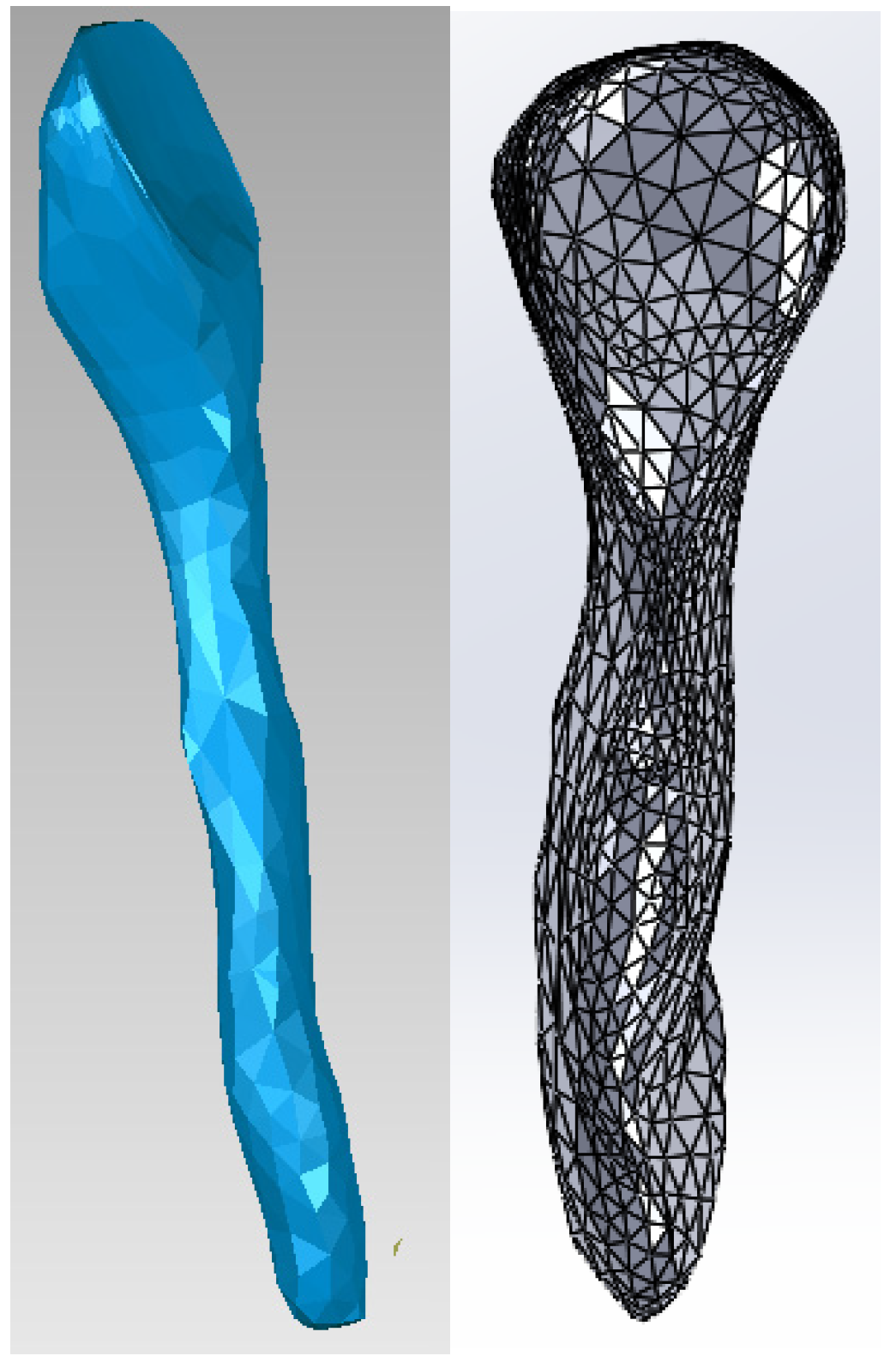
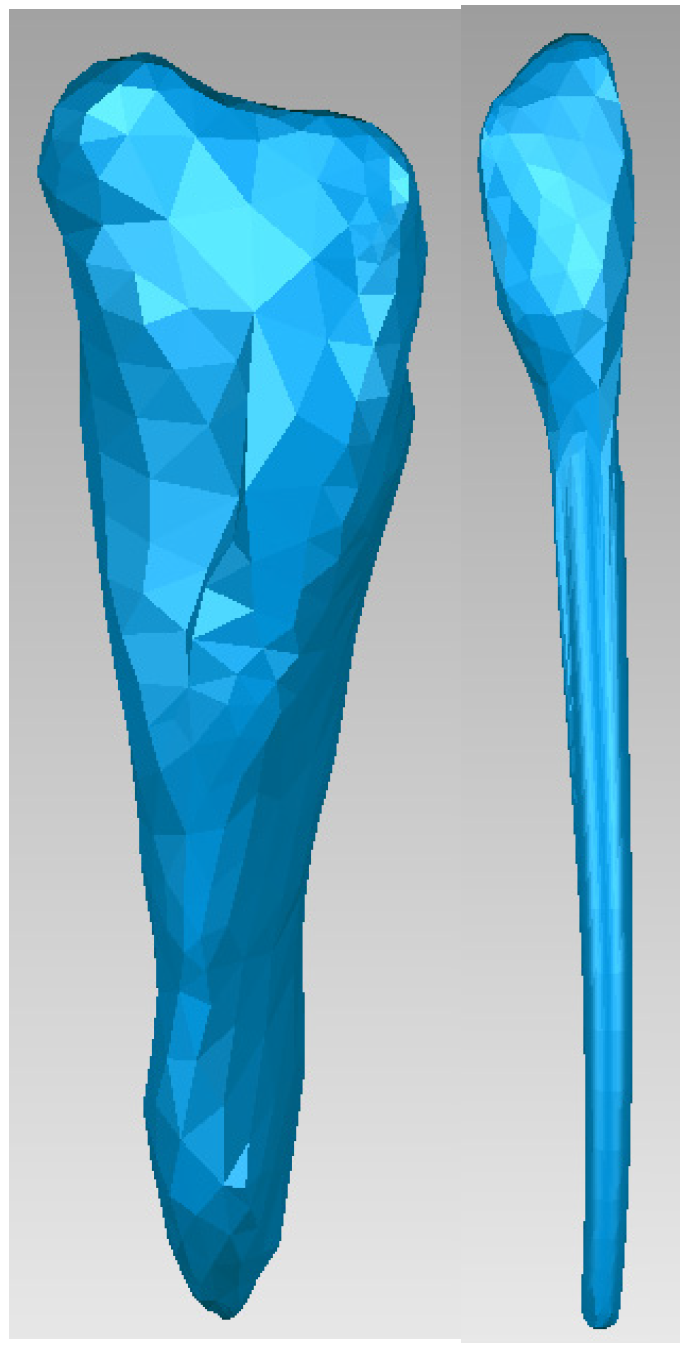
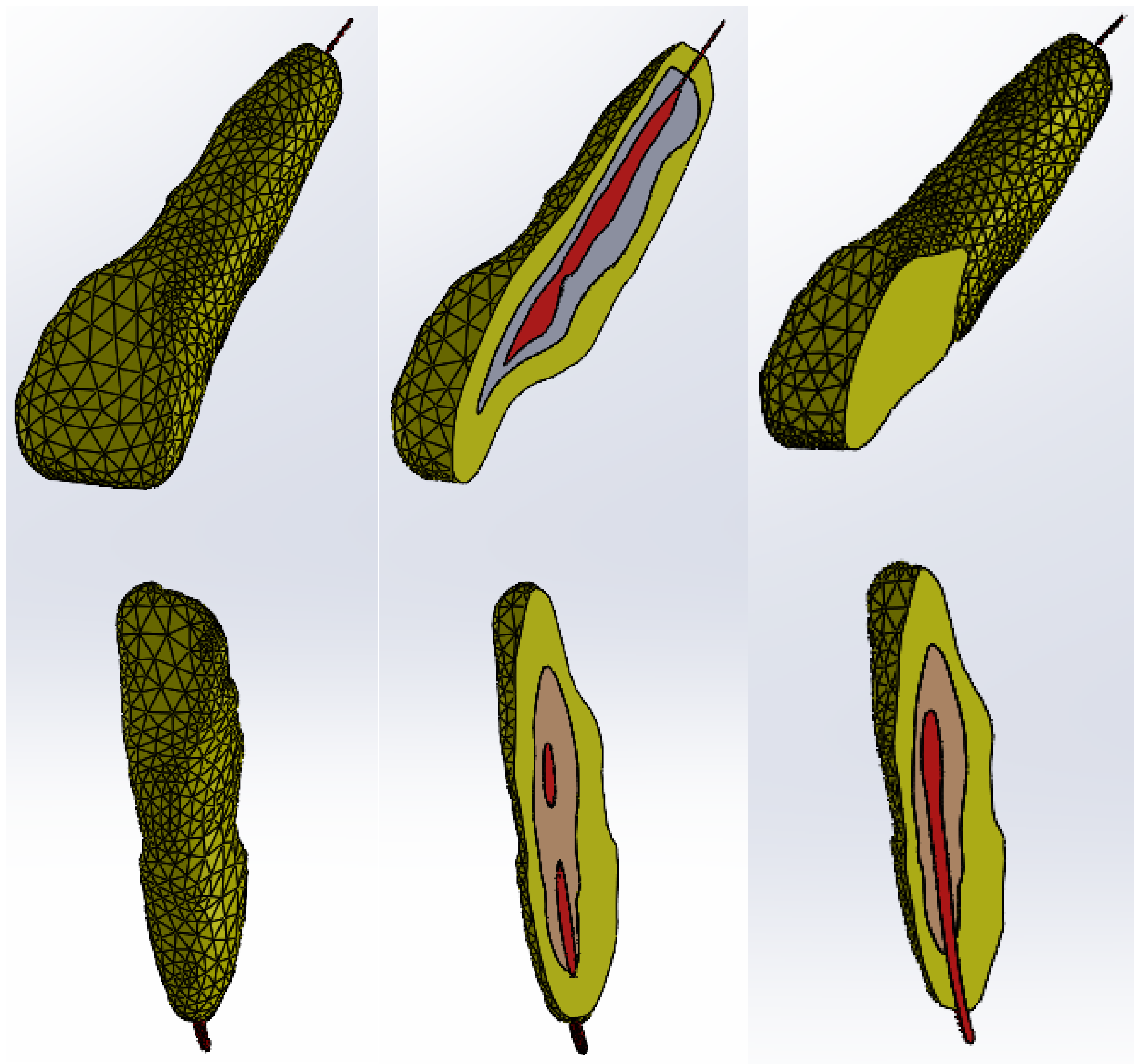
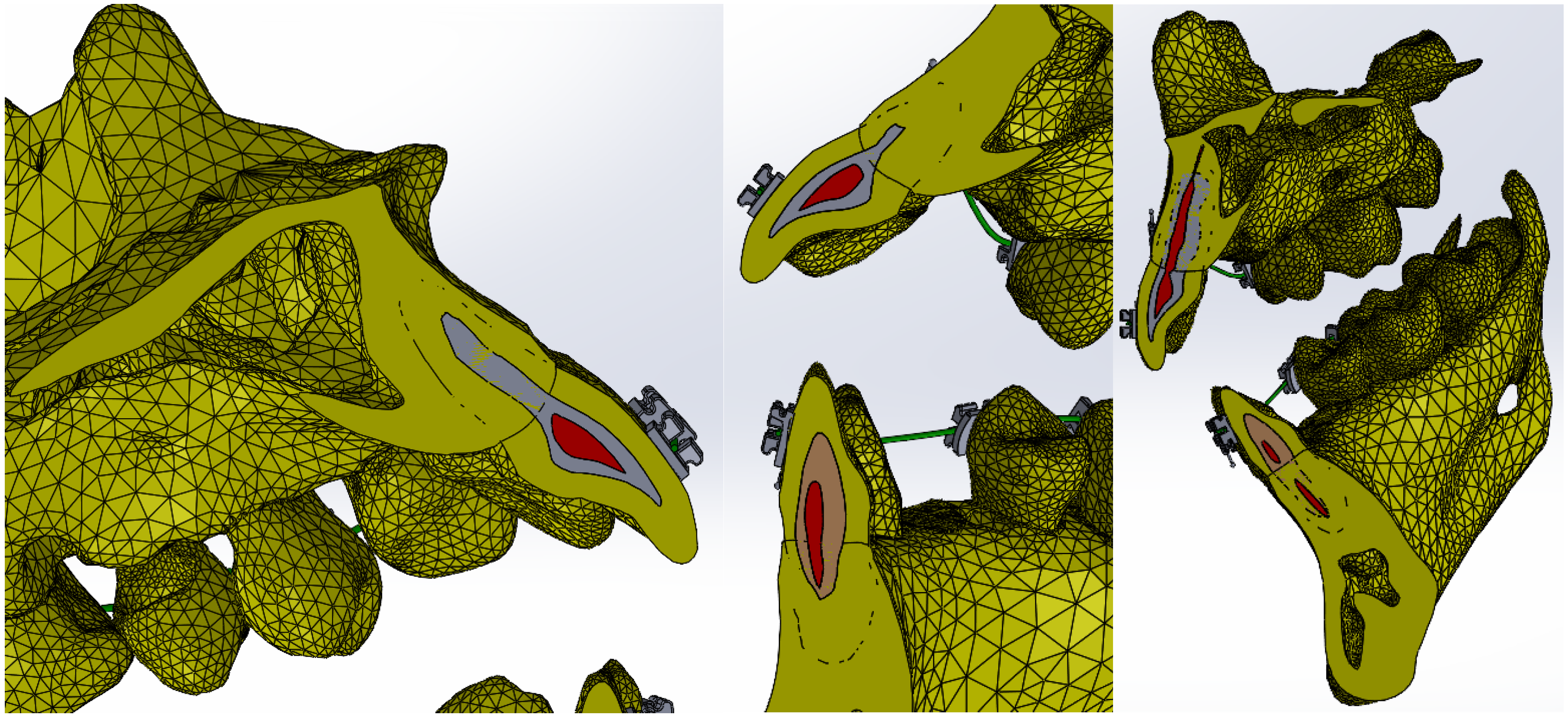
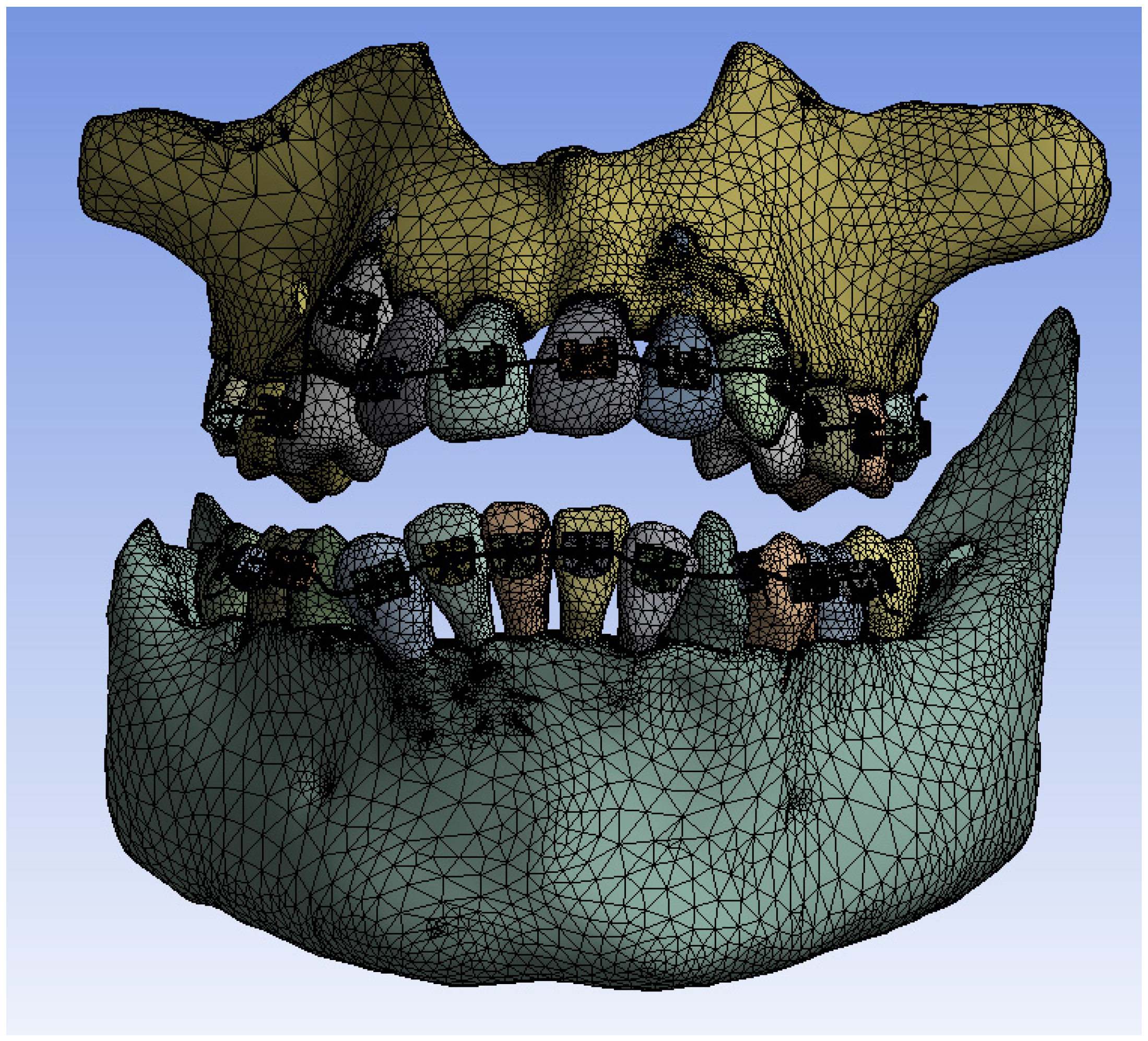
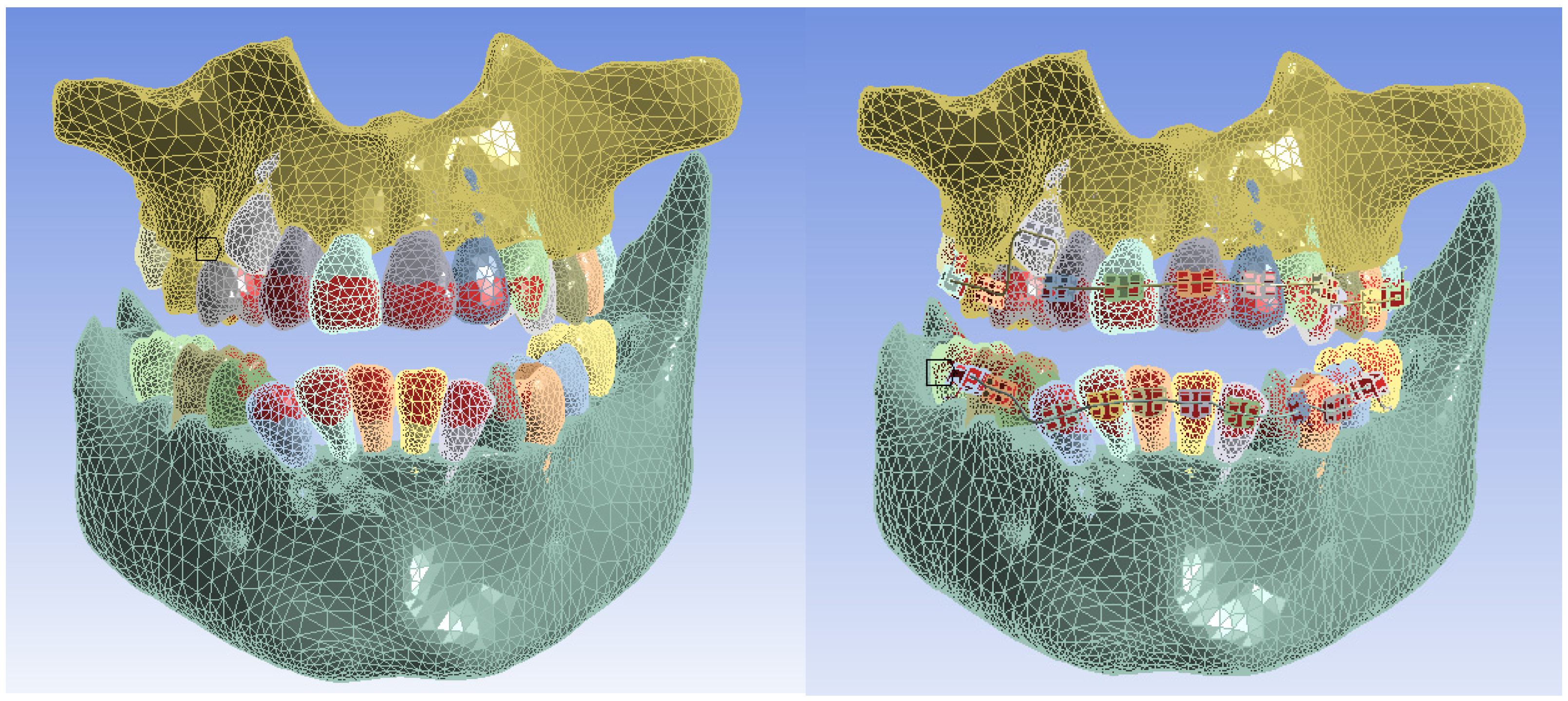
2.1. Elaboration of the Three-Dimensional Model of a Stomatognathic System Quasi-Identical to the Patient’s
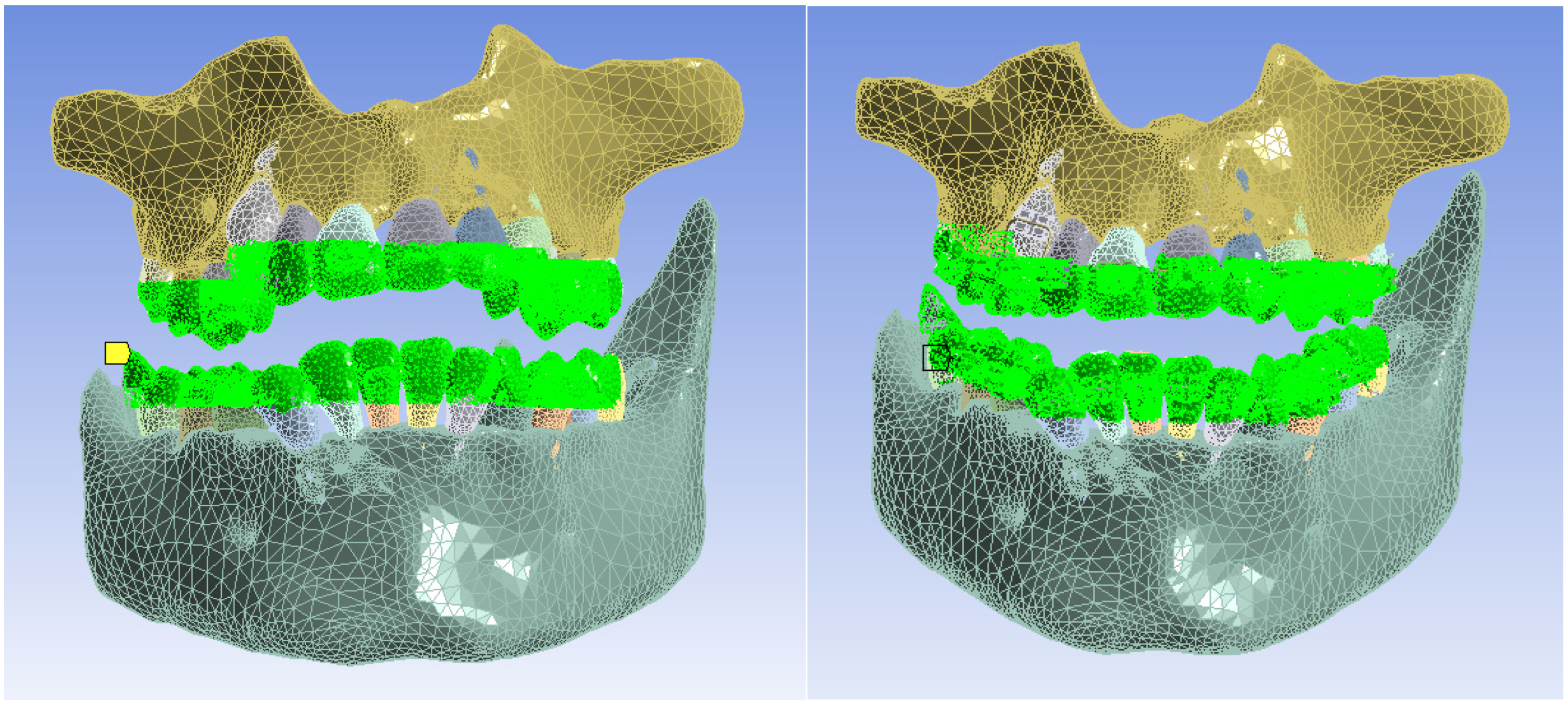
2.2. Preparation of Thermal Simulations
- -
- The model of the control stomatognathic apparatus (in the obtained model, the bracket and tube-type elements and the orthodontic wires were suppressed);
- -
- The model of the stomatognathic apparatus with a fixed metallic orthodontic appliance.
- -
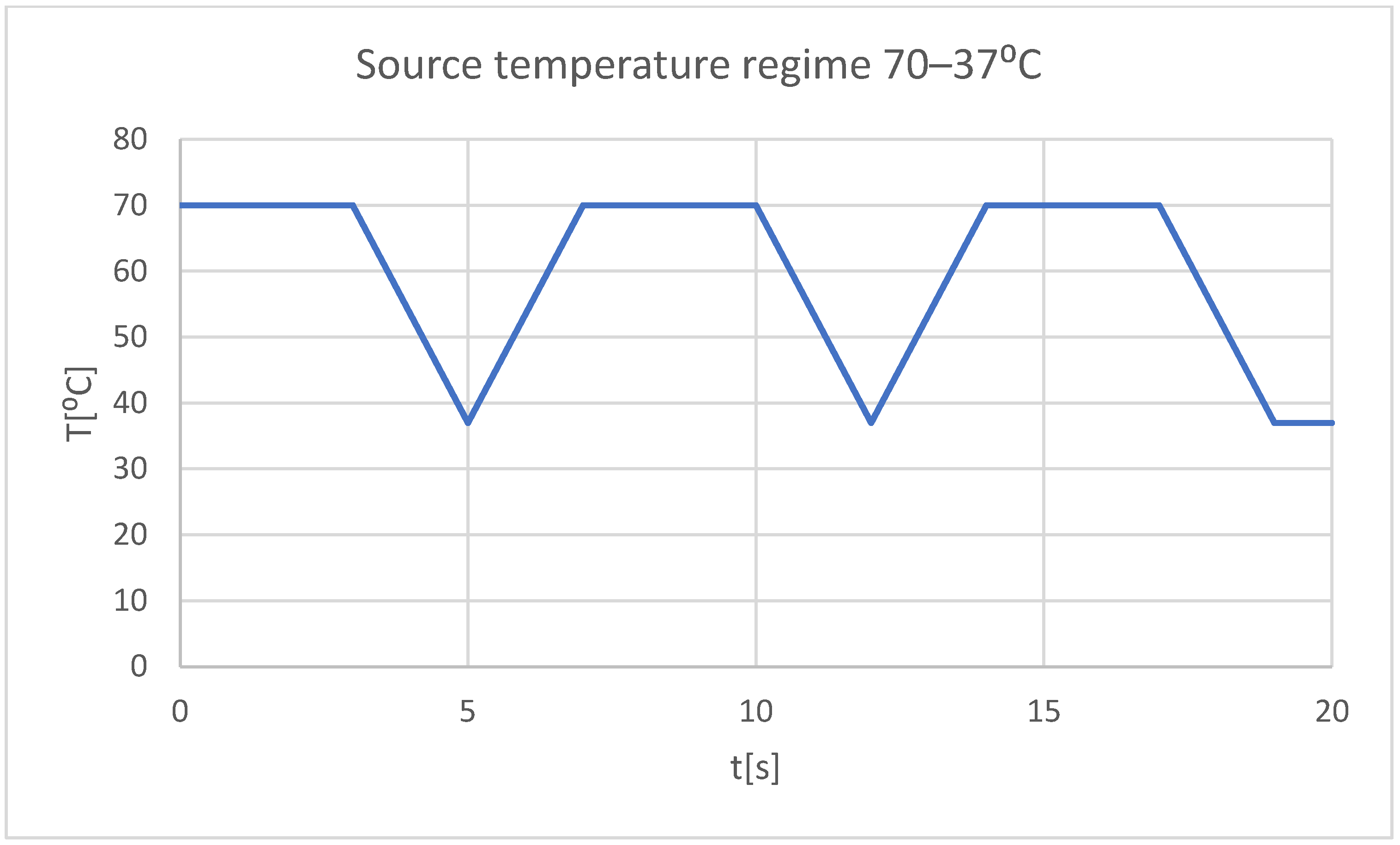
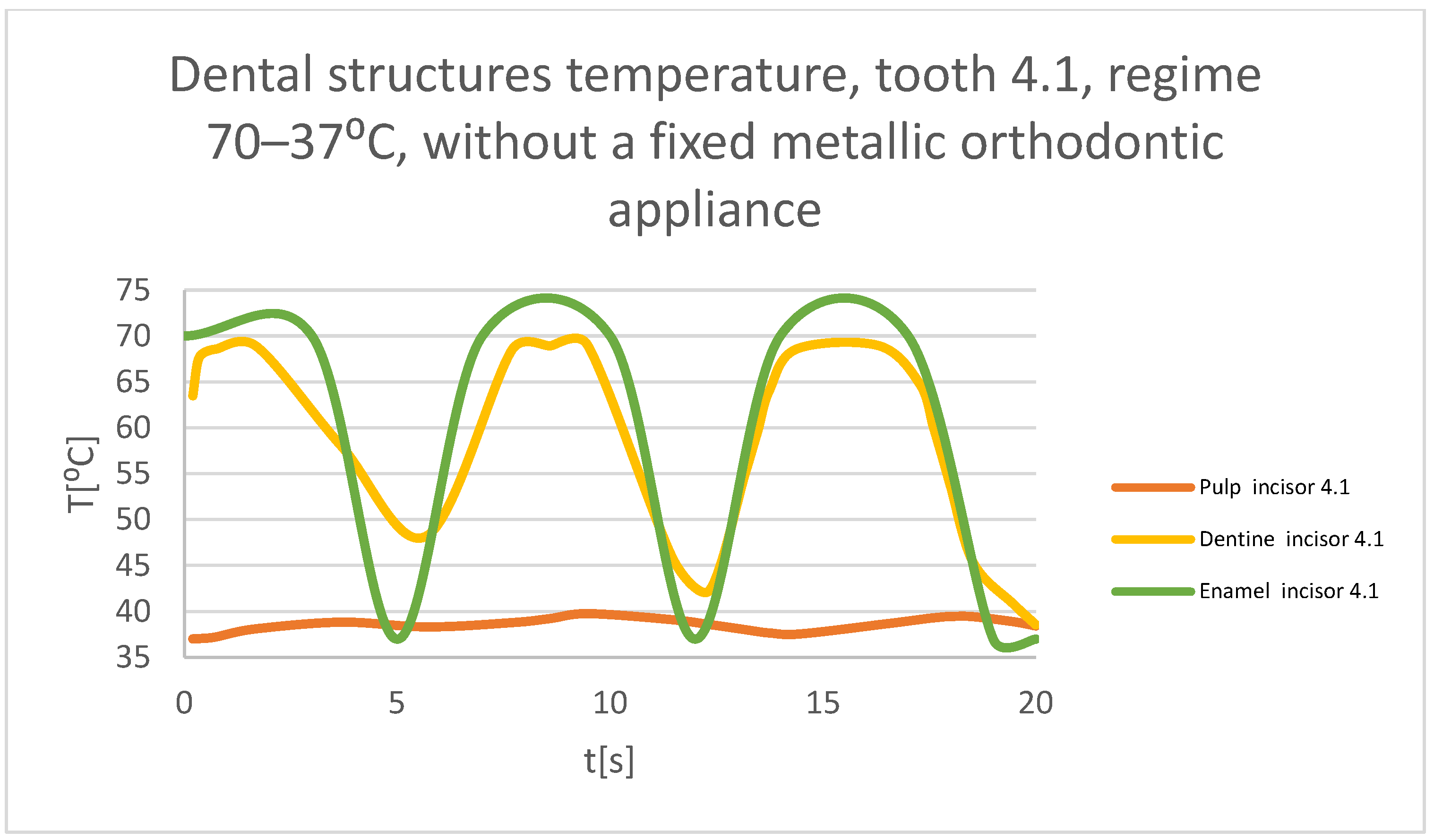
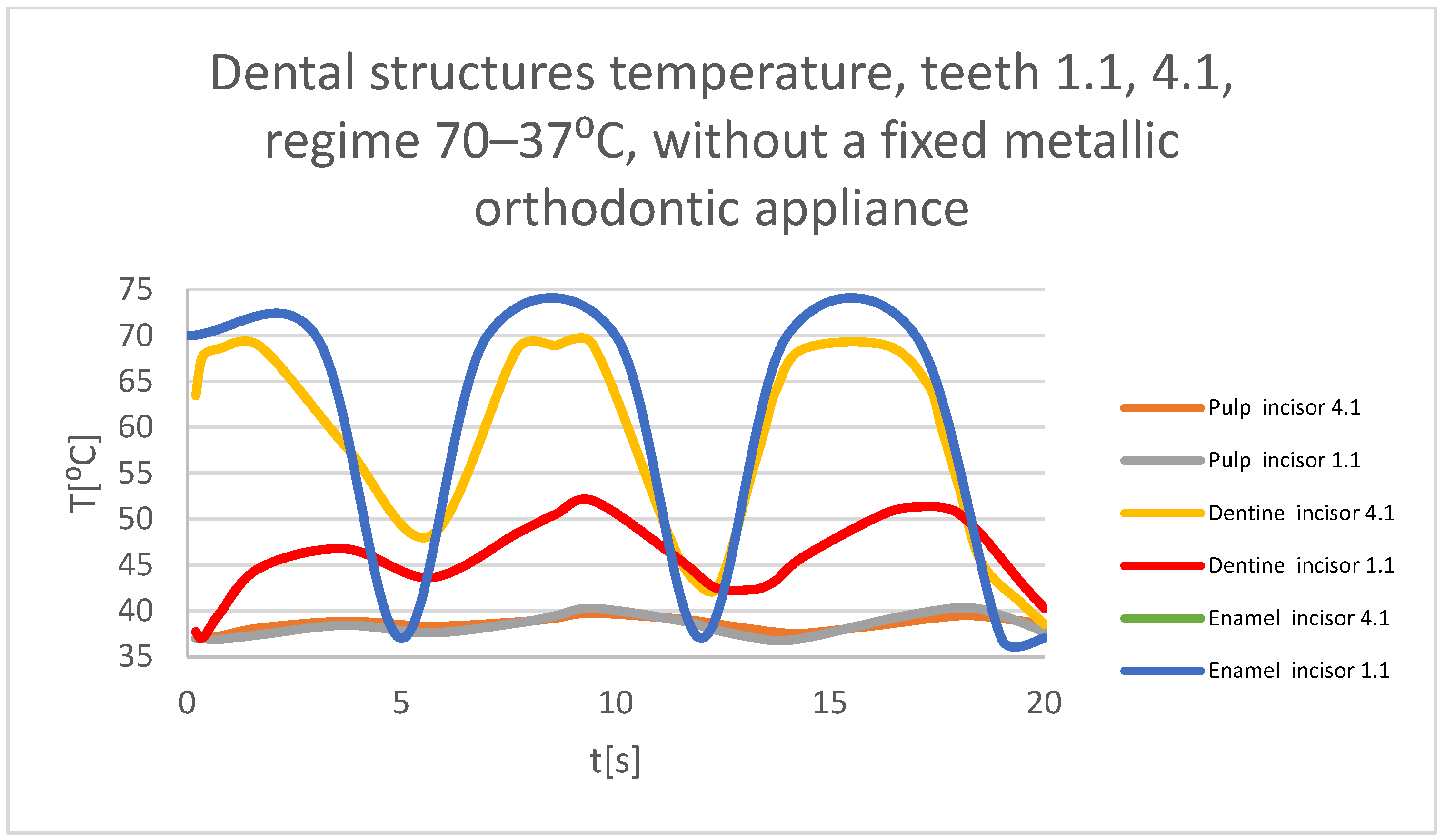
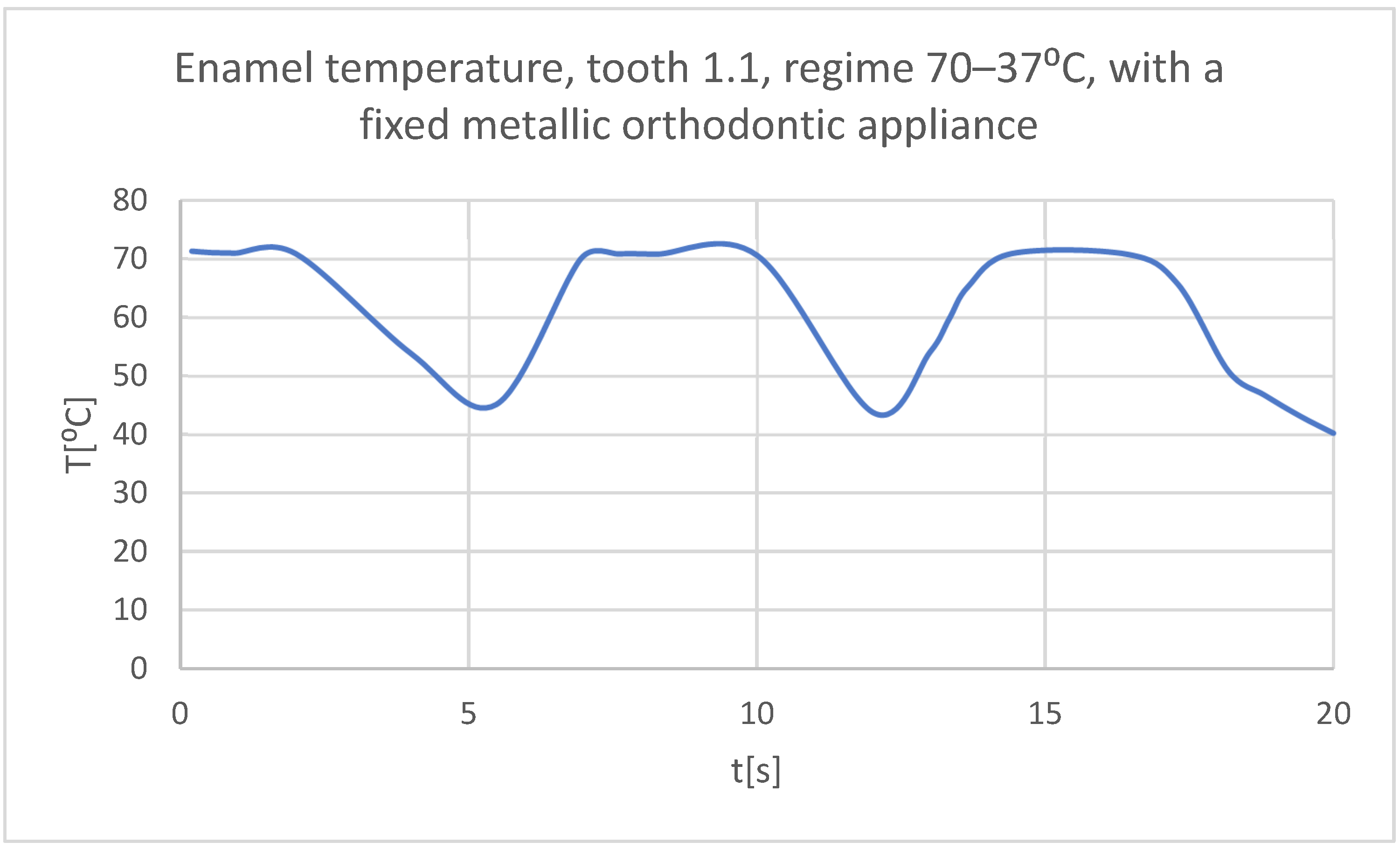
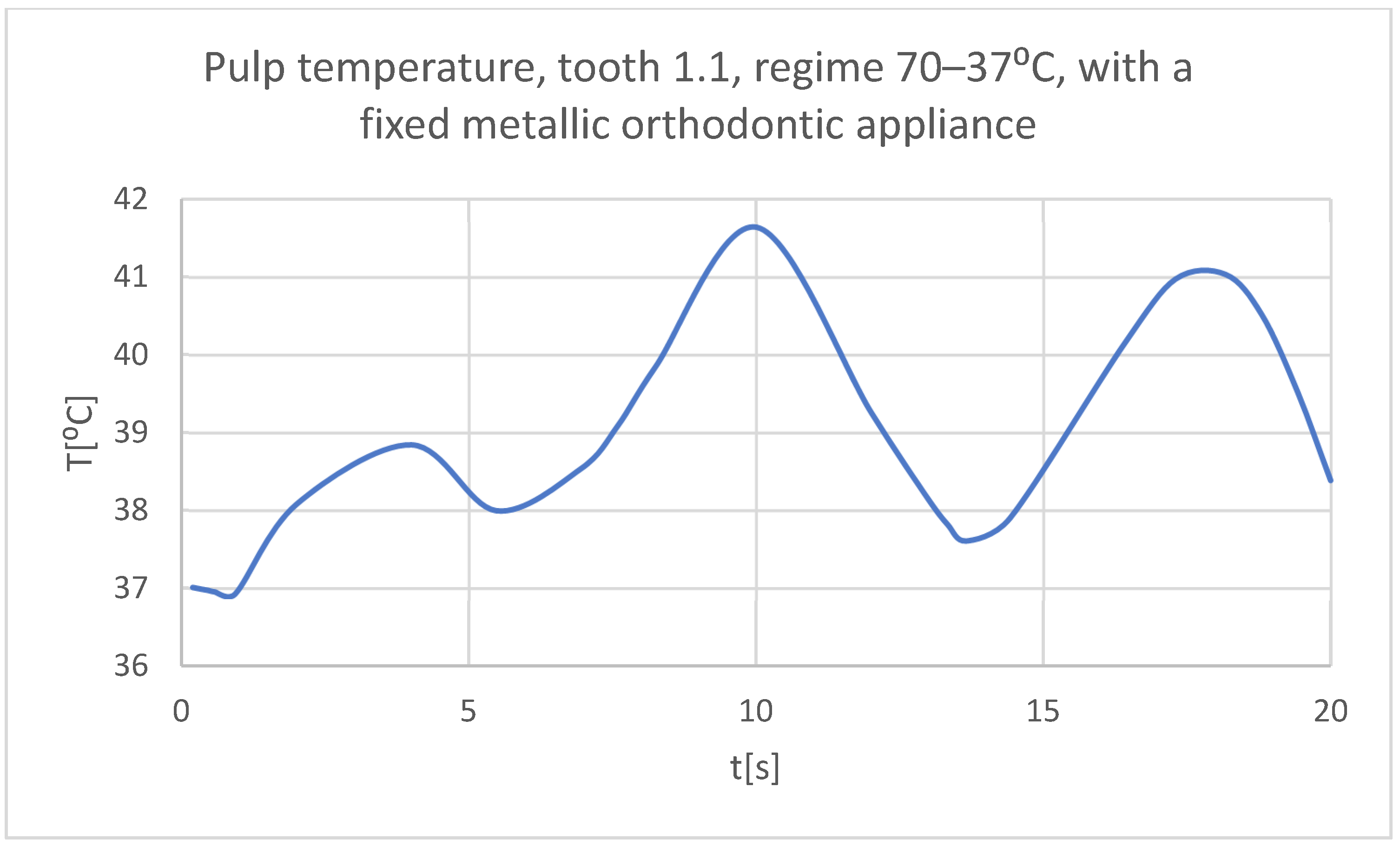
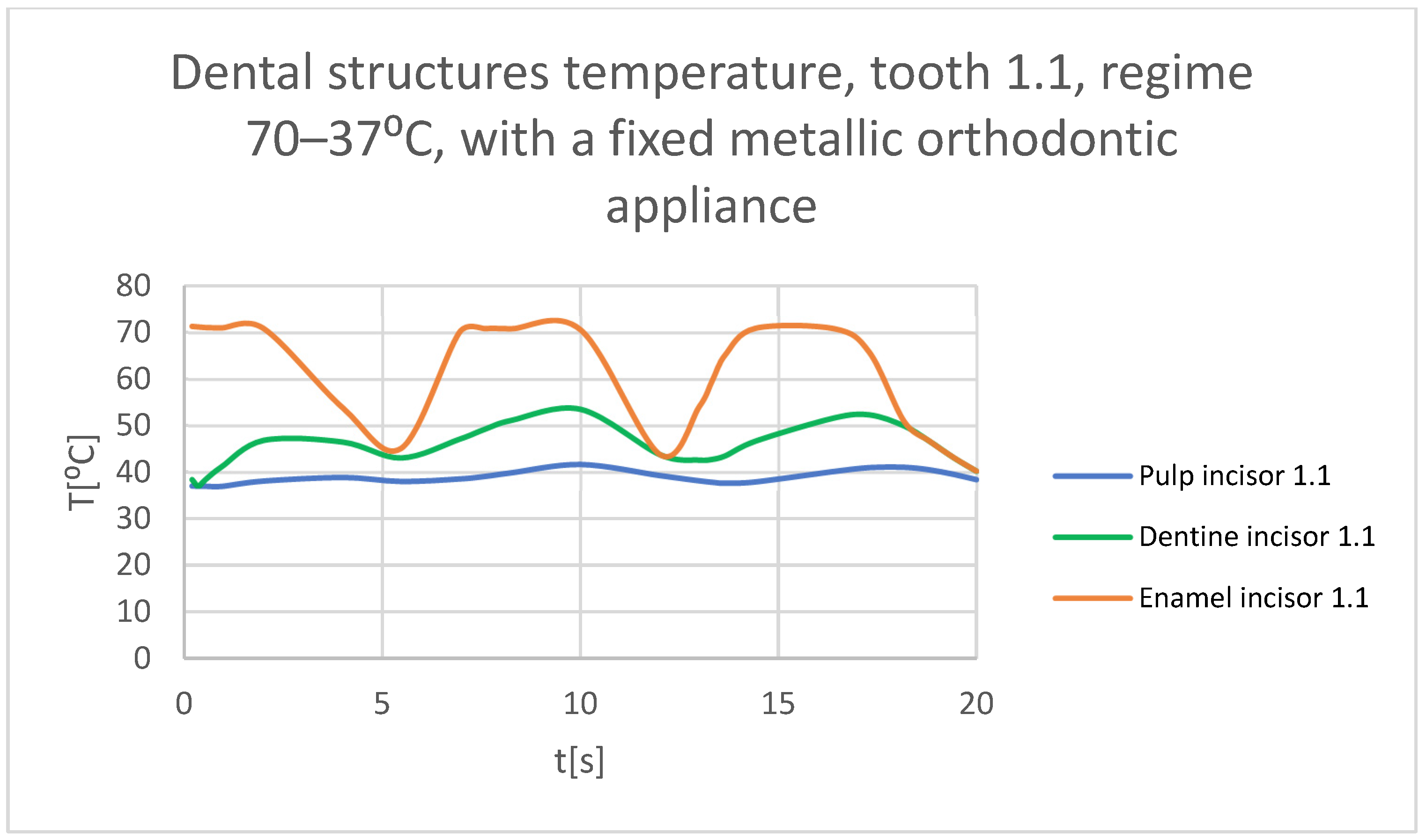
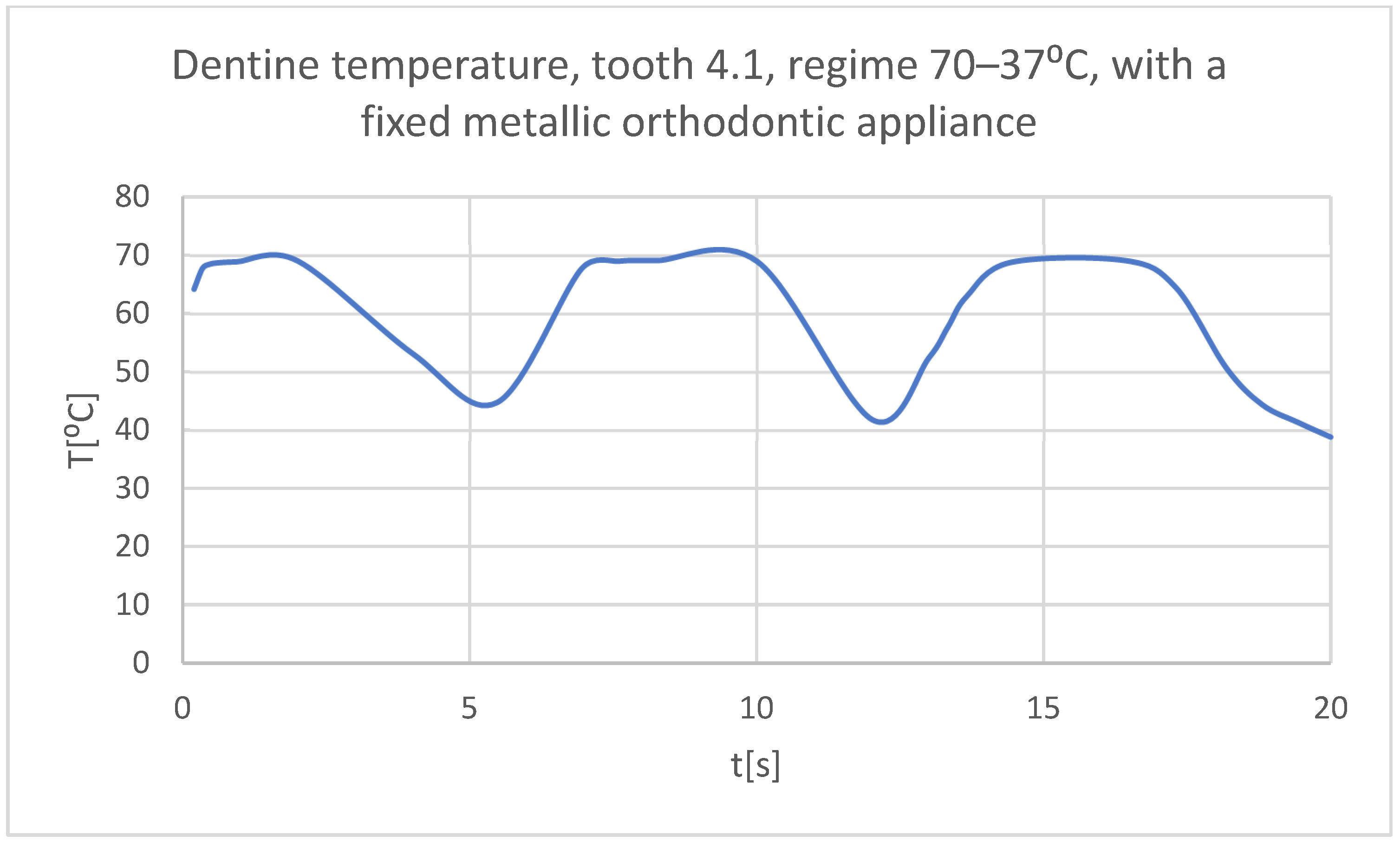
- Very hot food (70 °C) that acts for 3 s, then the temperature tends to 37 °C, and the cycle is repeated two more times; the whole regime lasts 20 s (Figure 22);
- -
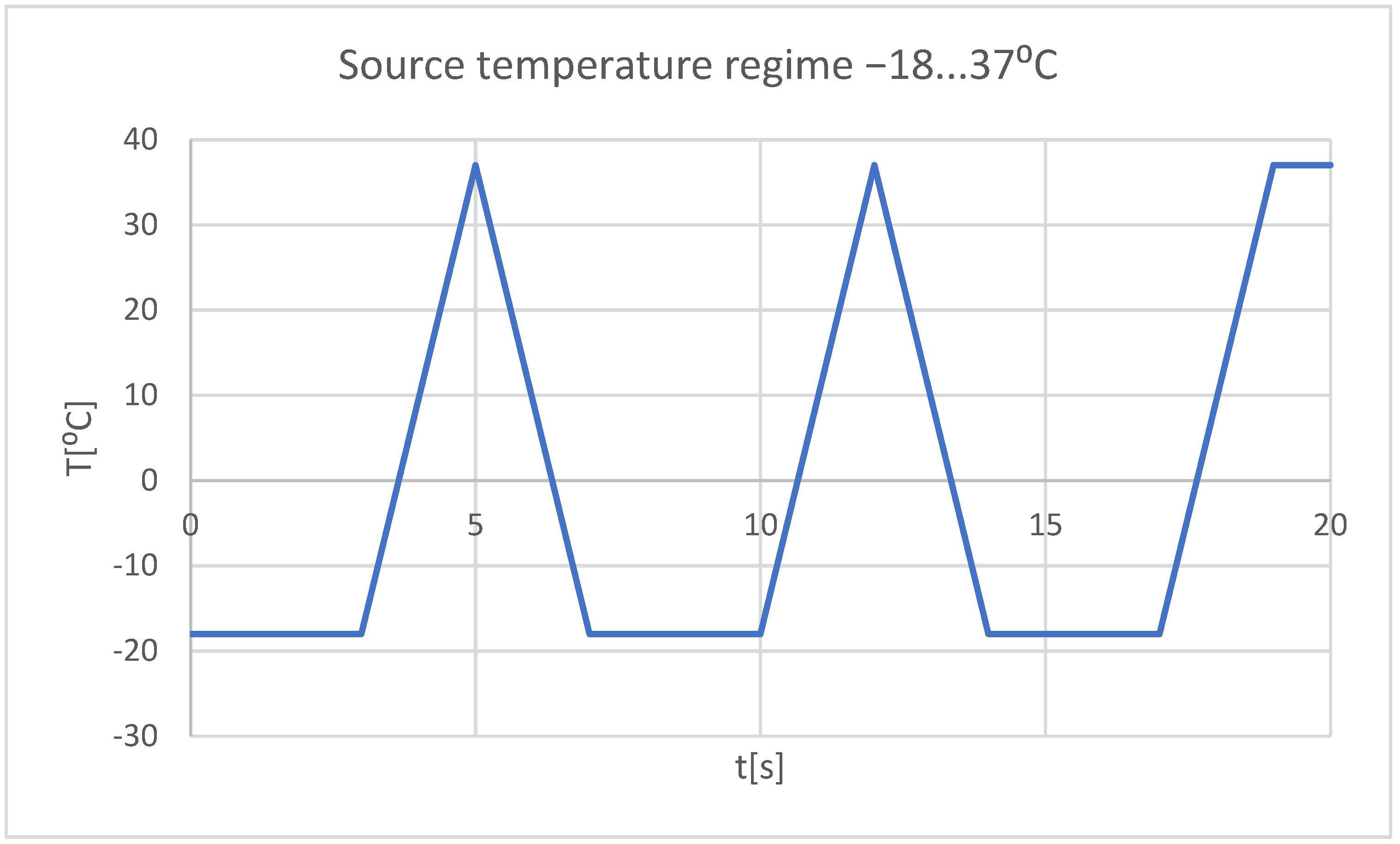
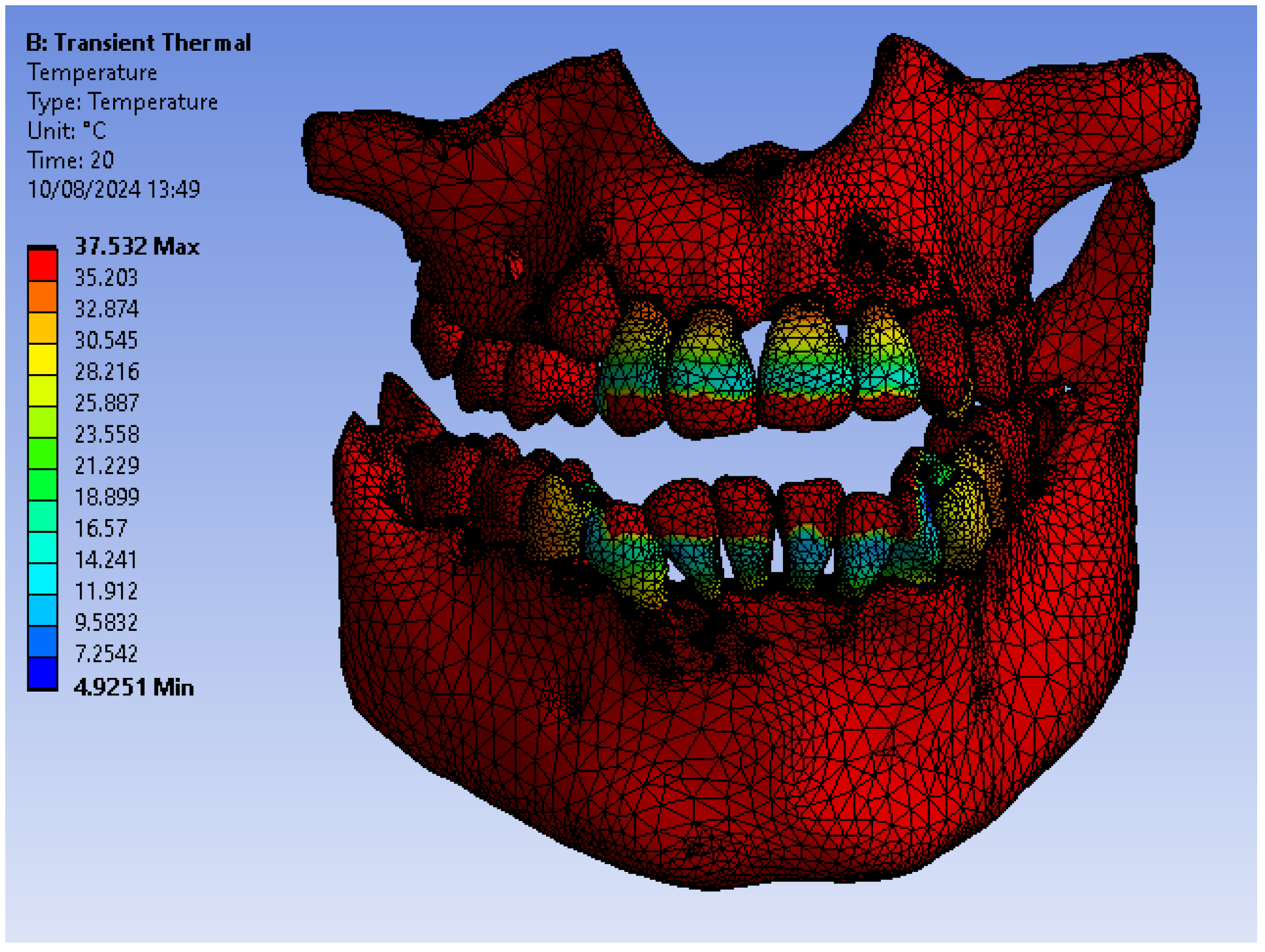
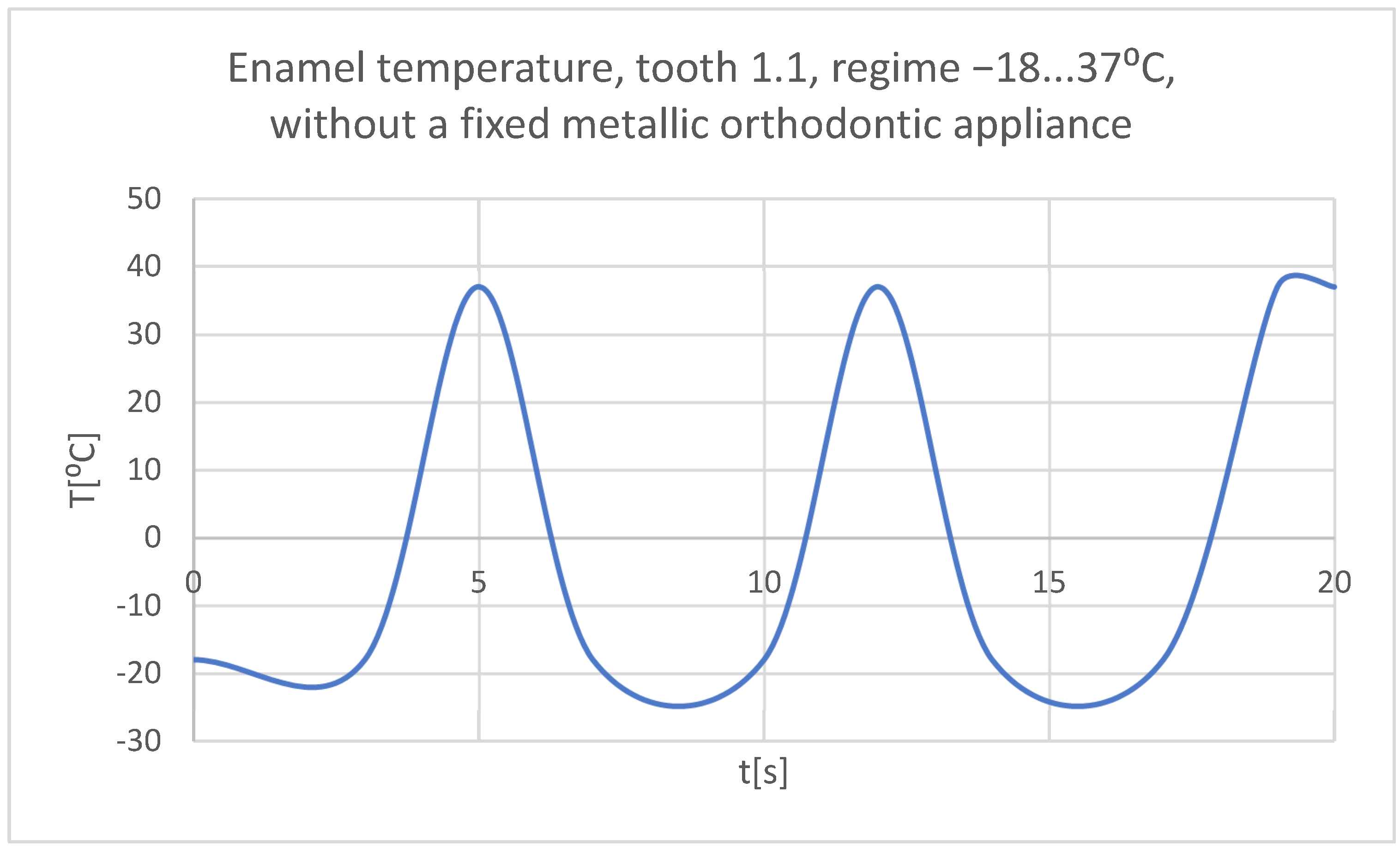
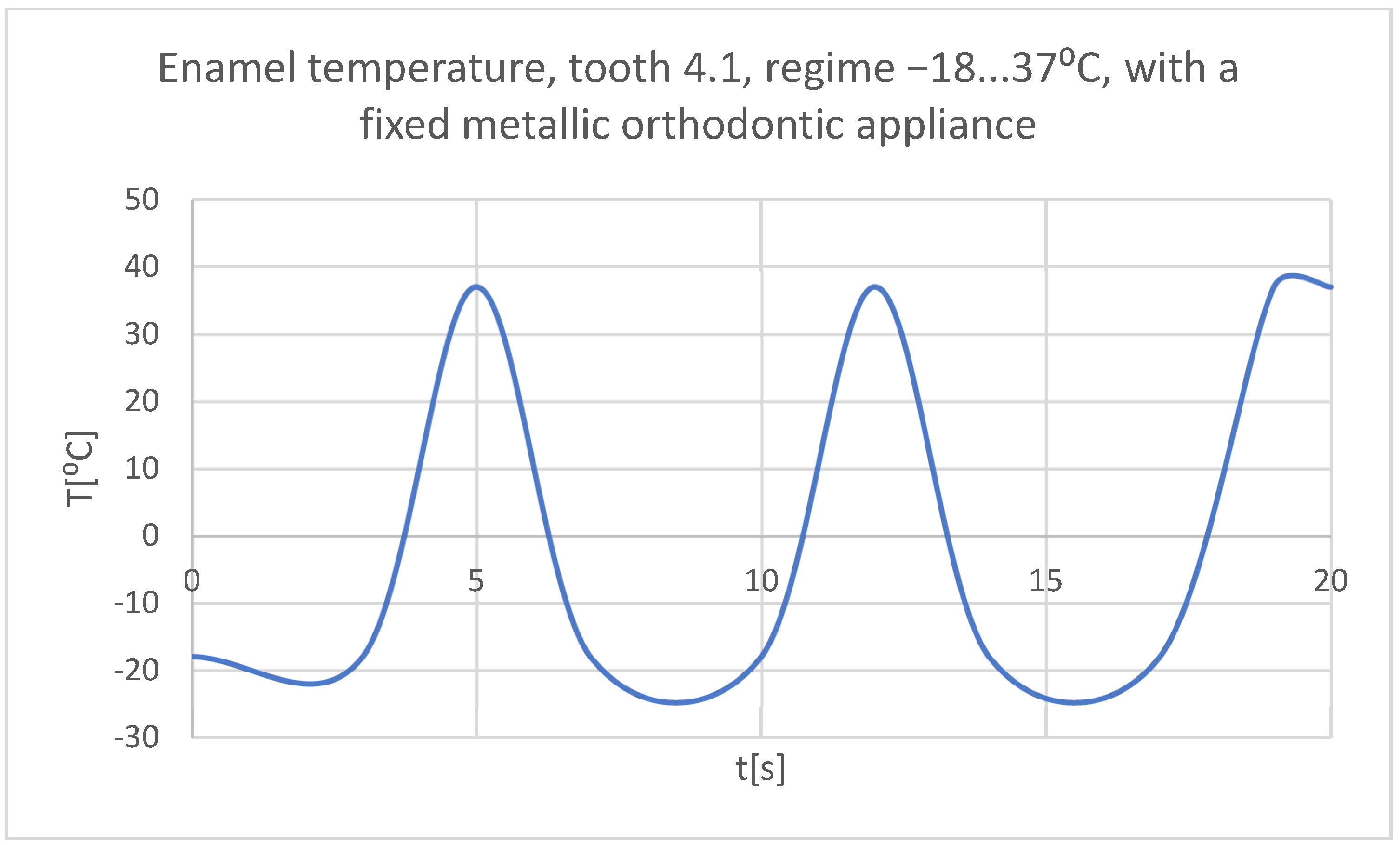
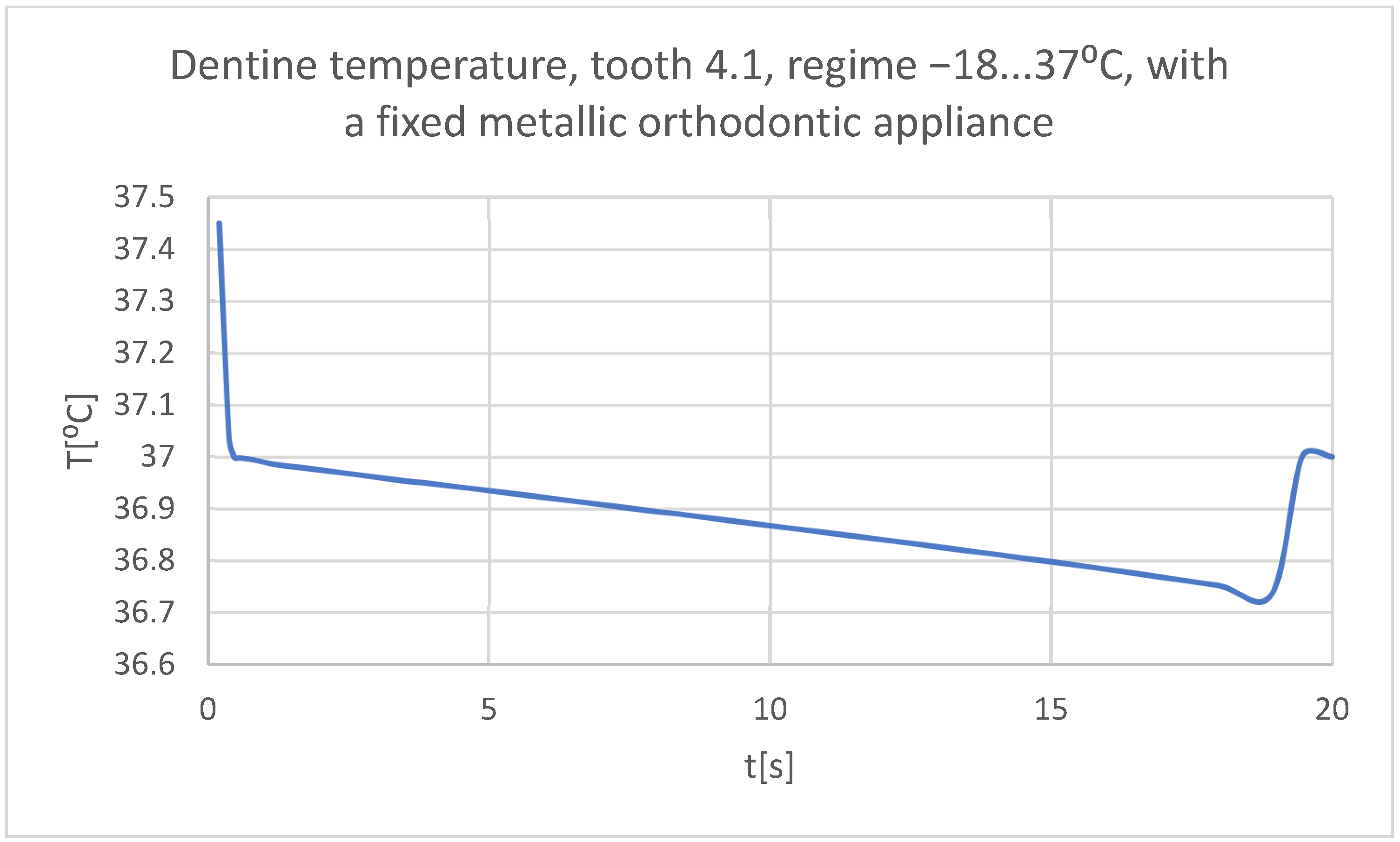
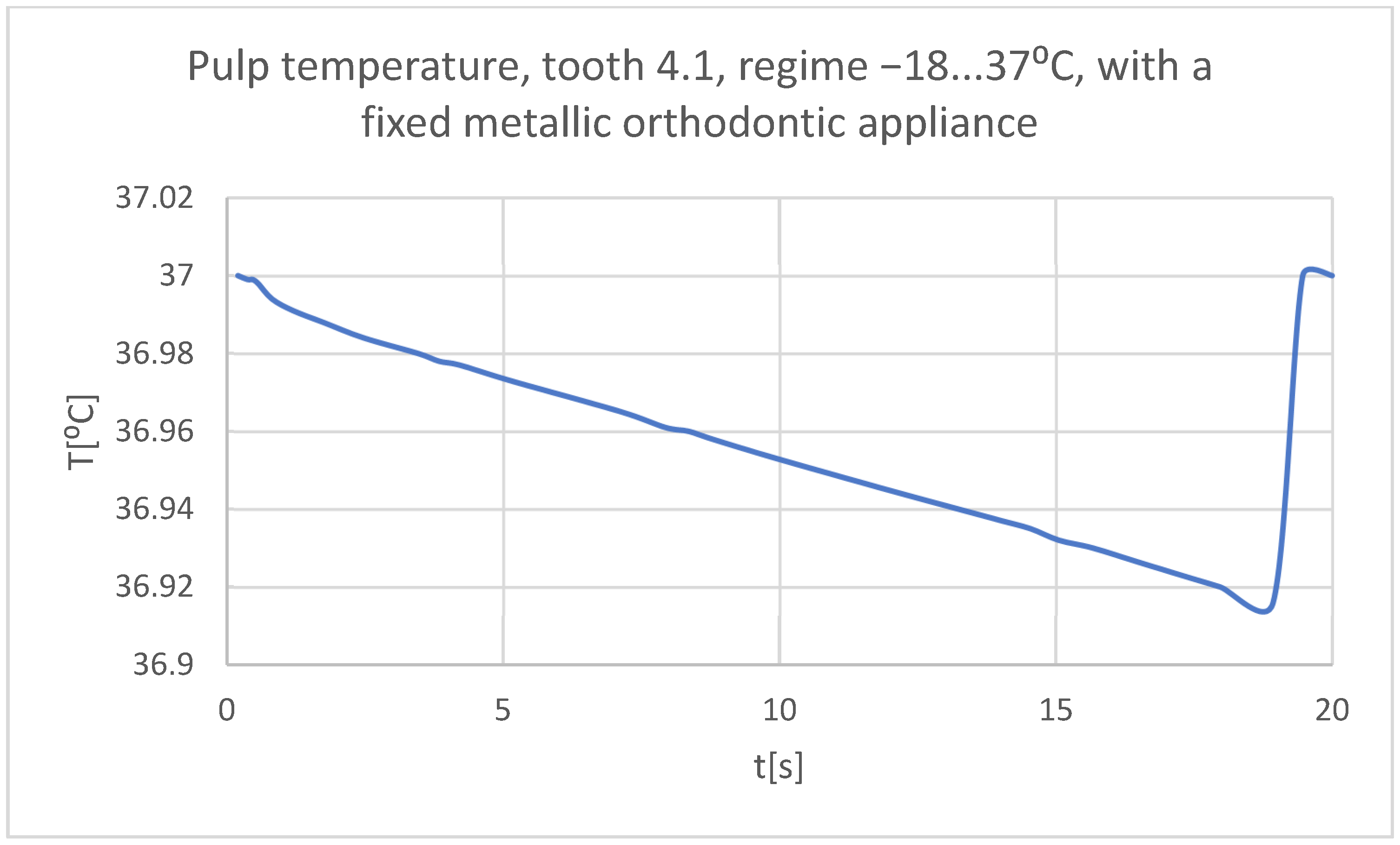
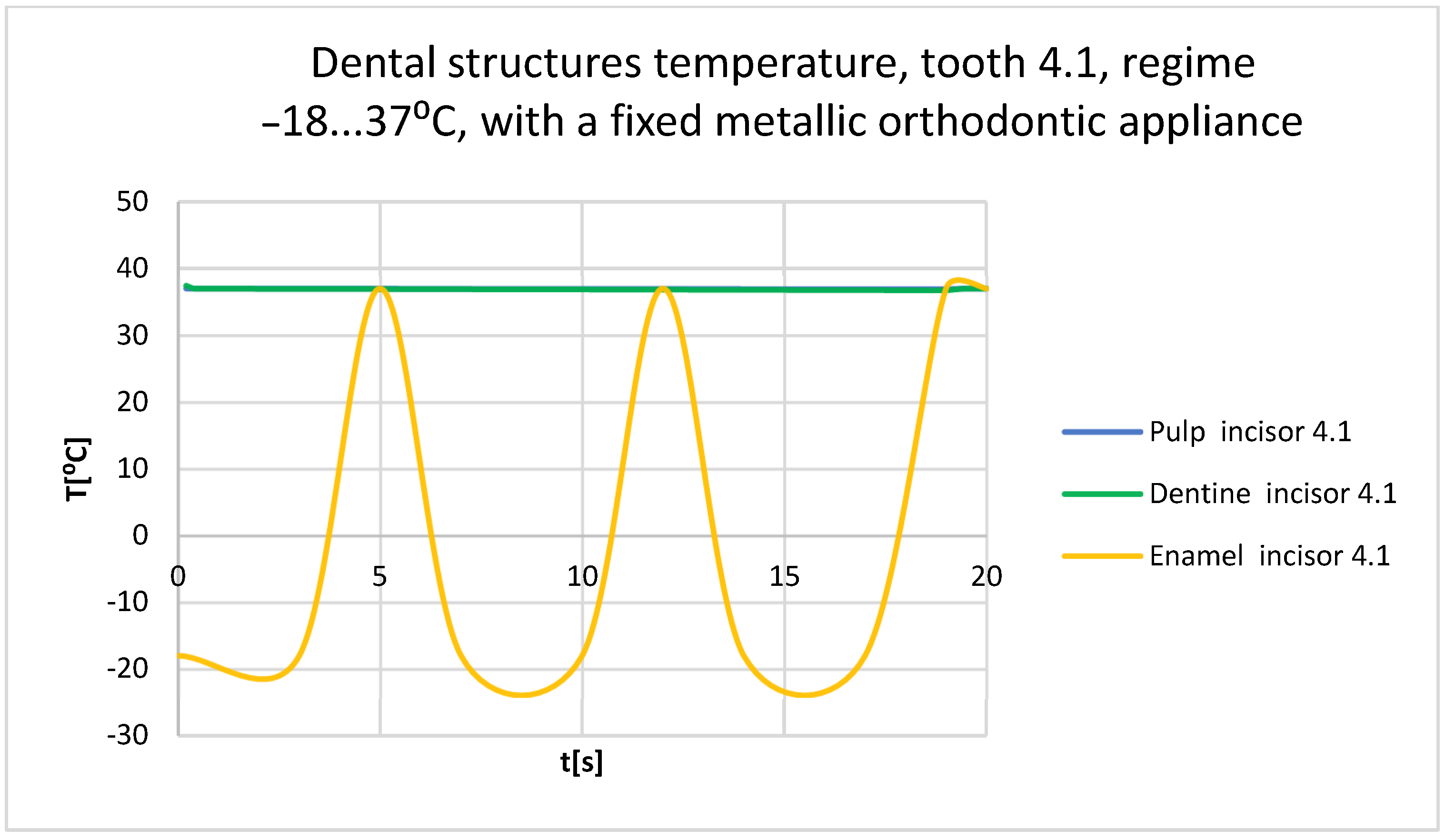
- Very cold food (−18 °C) that acts for 3 s, then the temperature tends to 37 °C, and the cycle is repeated two more times; the whole regime lasts 20 s (Figure 23);
3. Results
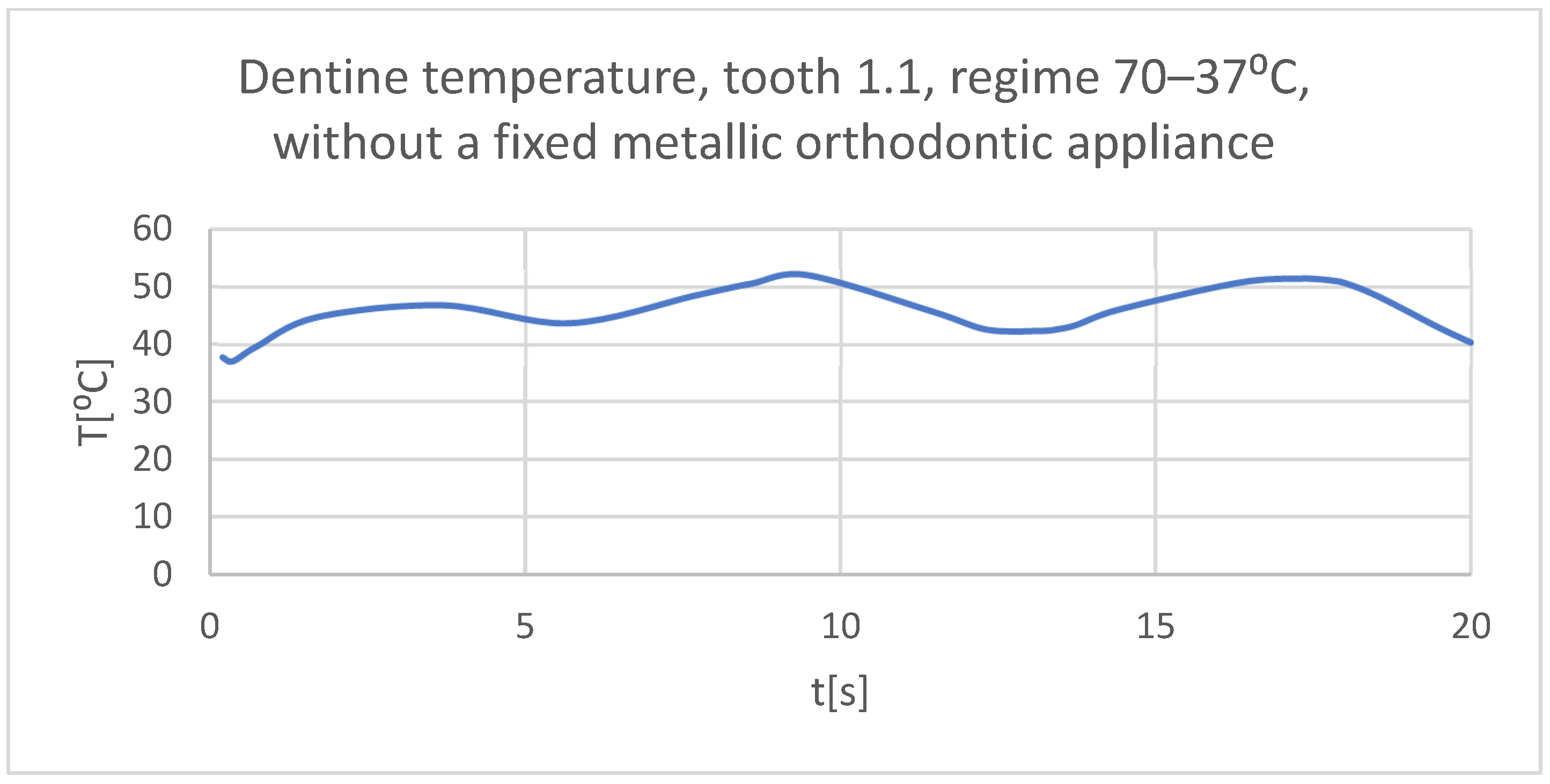
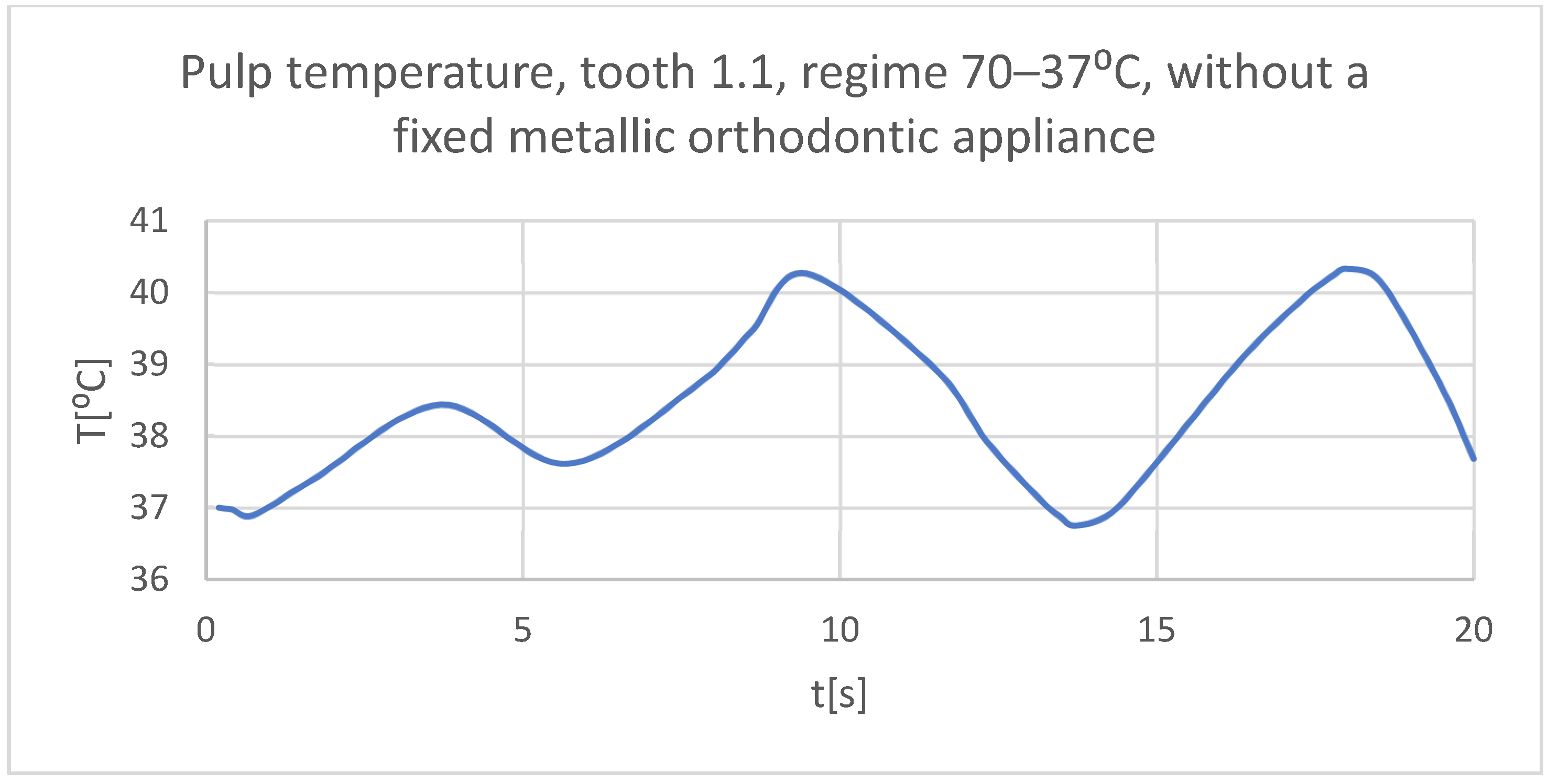
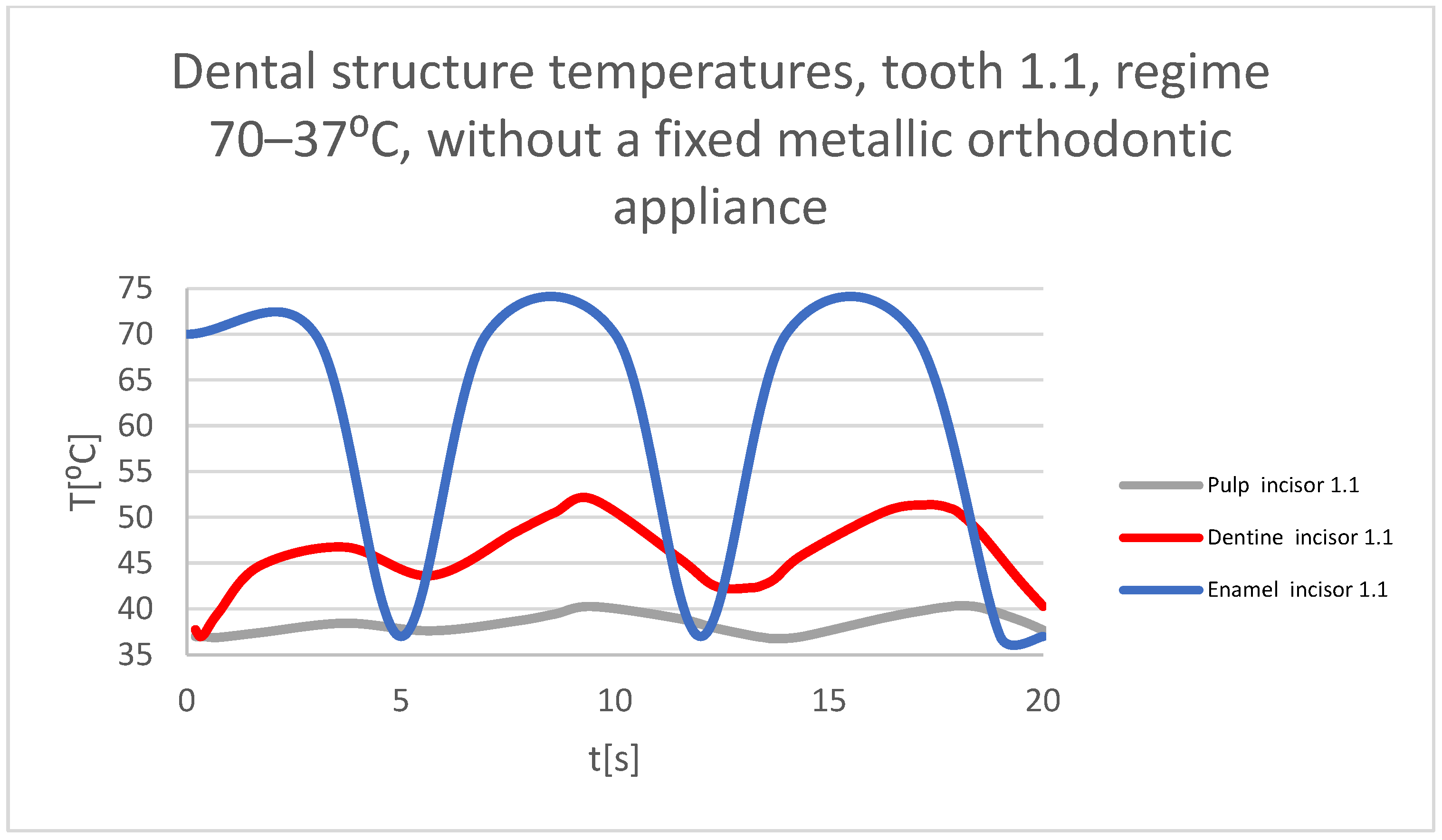
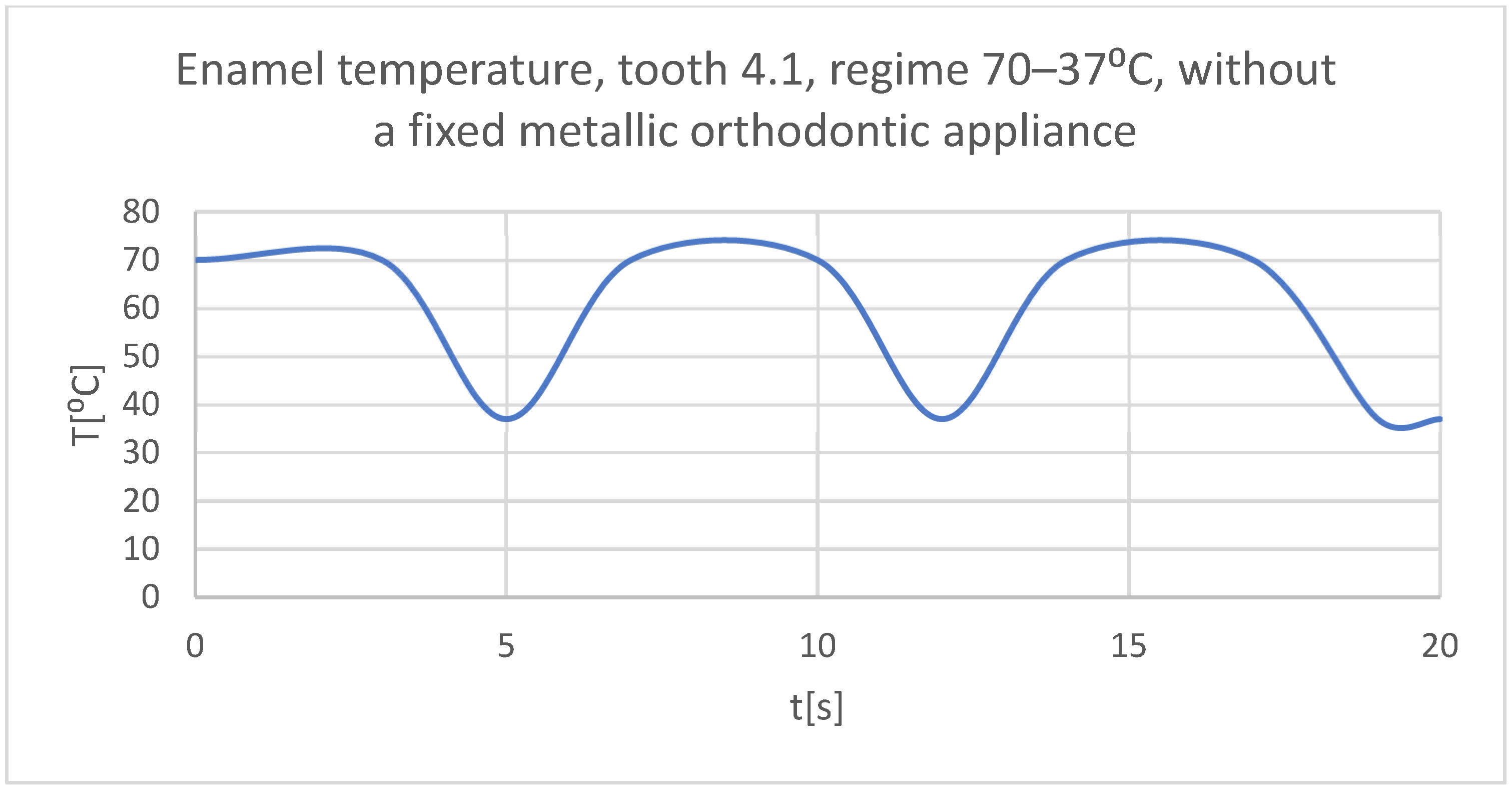
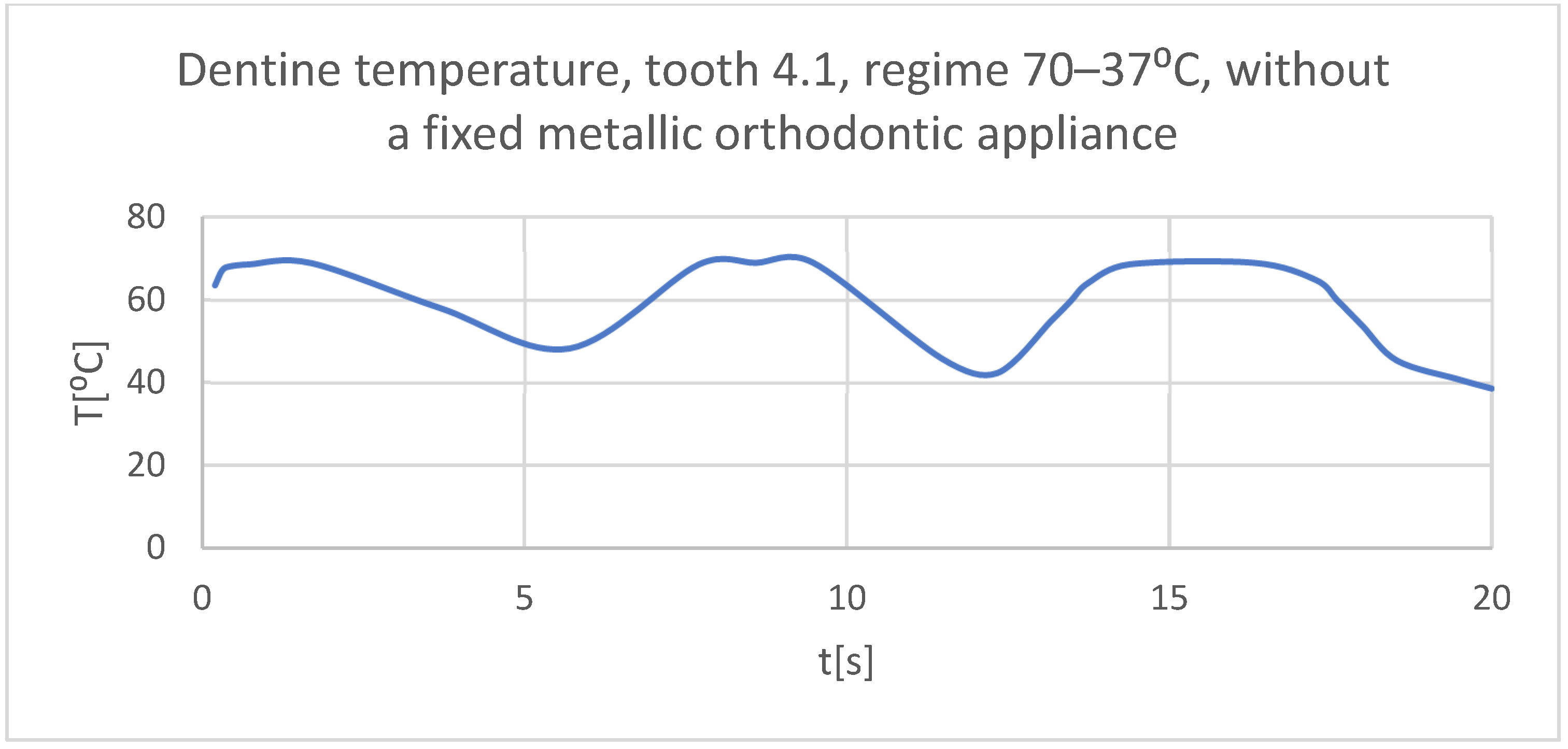
3.1. Thermal Simulation Results for the Stomatognathic Control System with a Hot Temperature Source
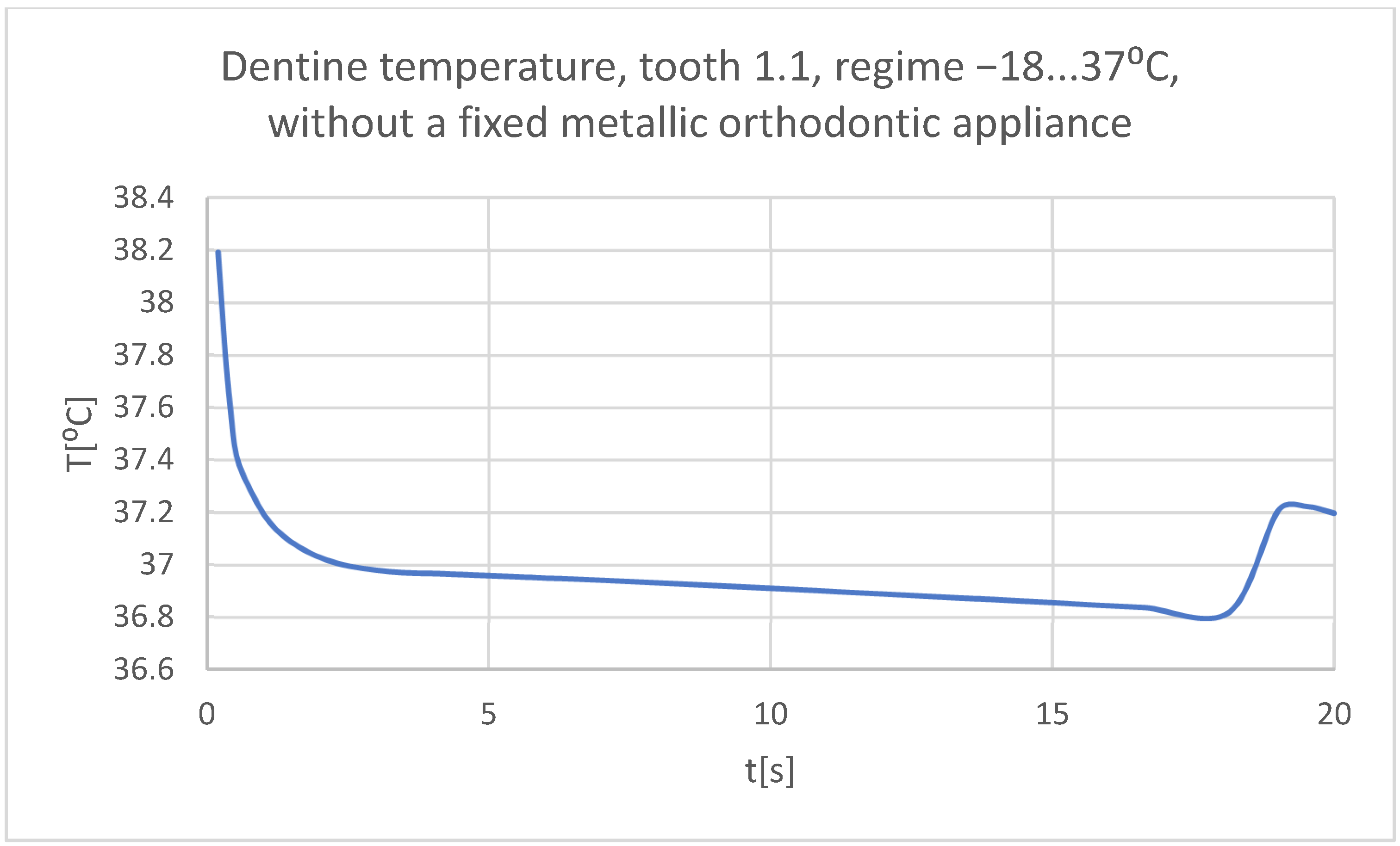
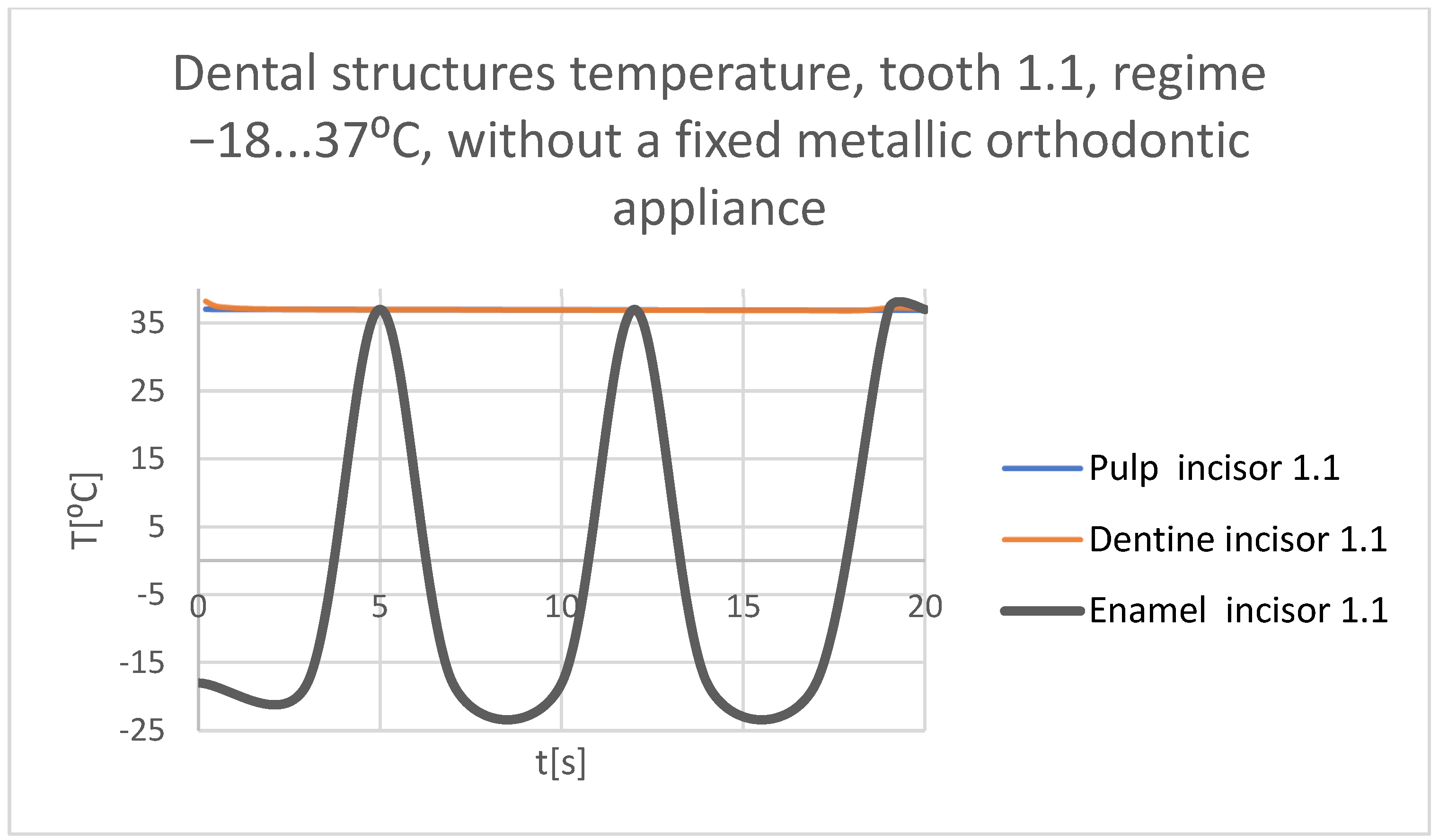
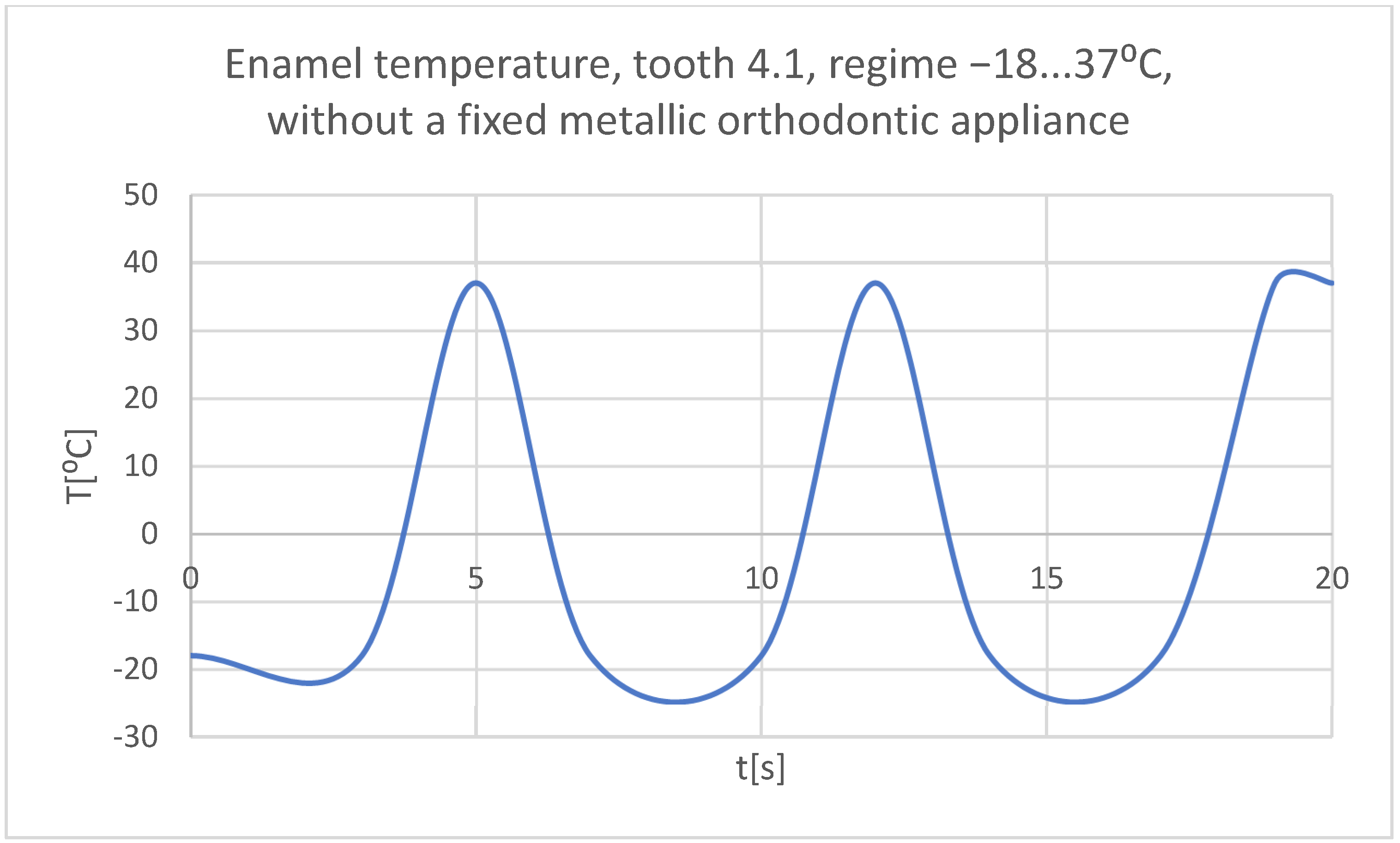
3.2. Thermal Simulation Results for the Stomatognathic Control System with a Cold Temperature Source
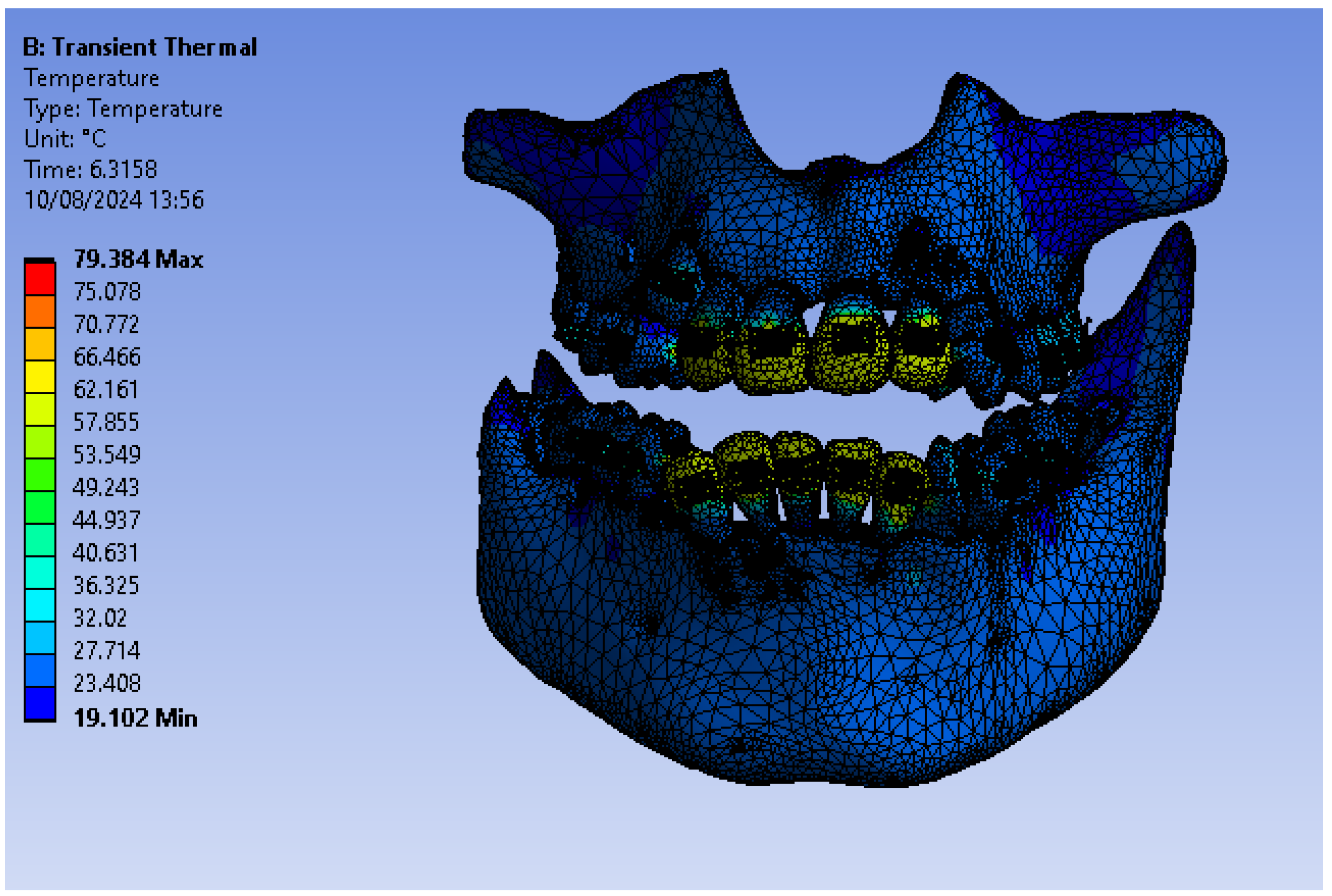
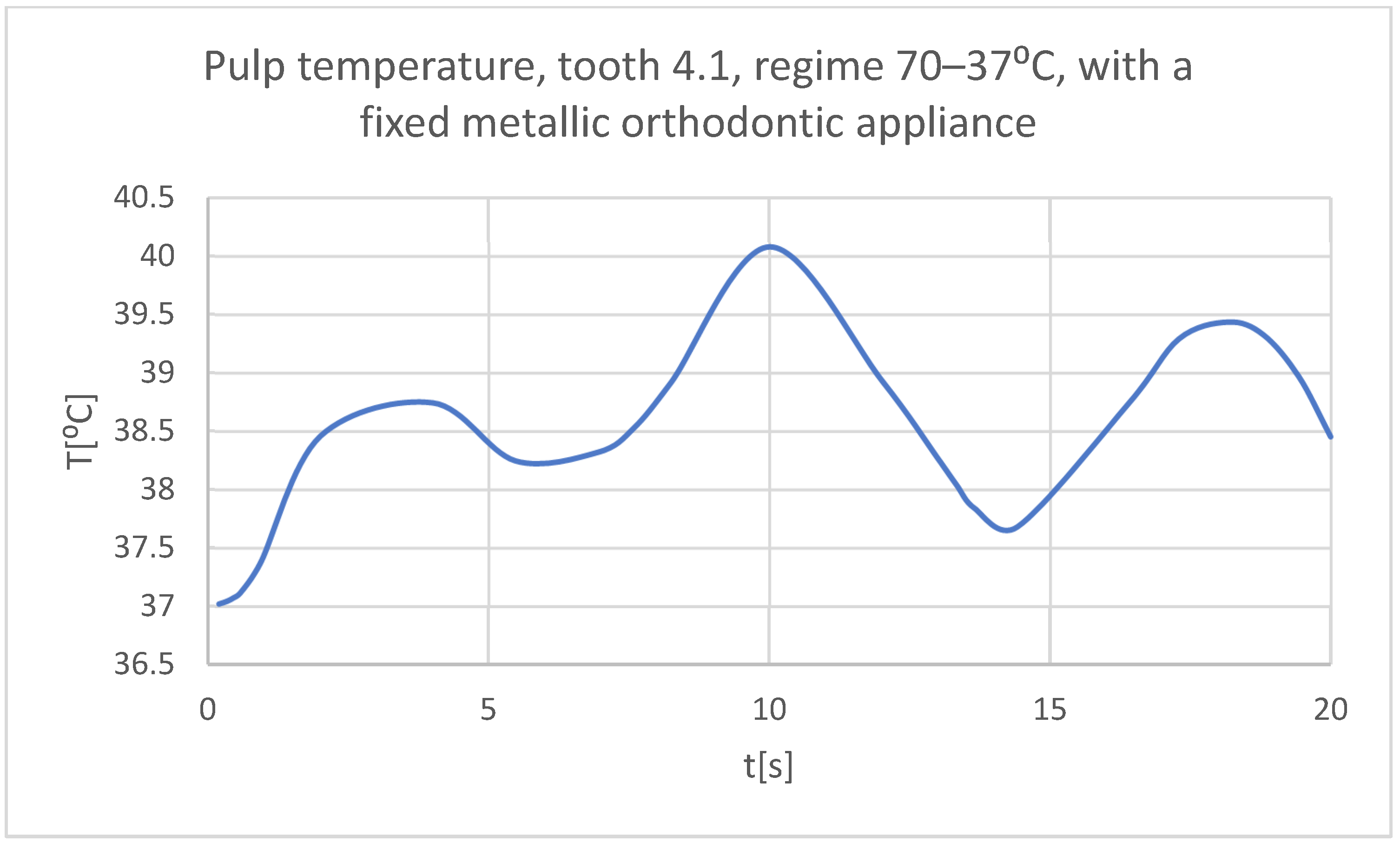
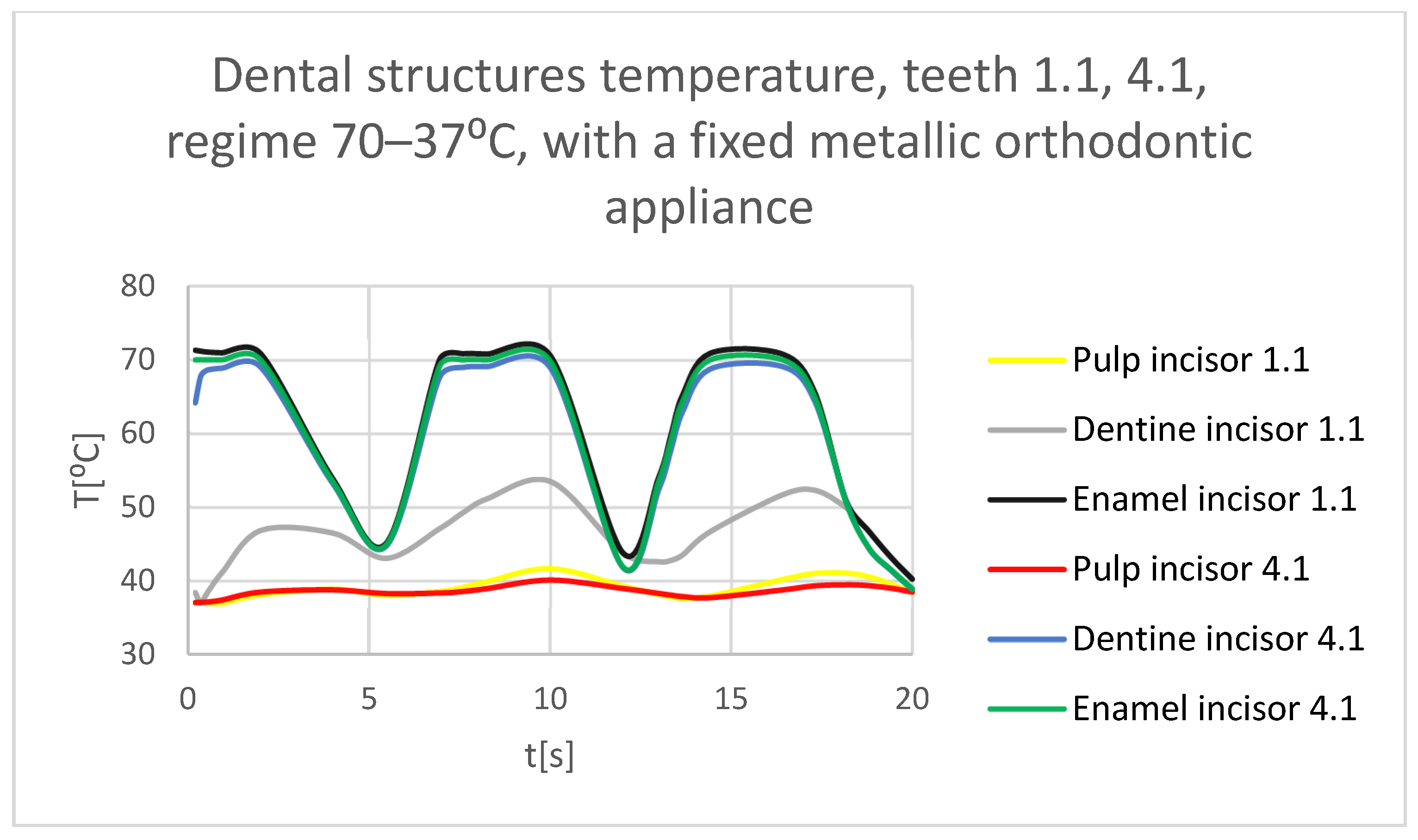
3.3. The Results of the Thermal Simulation for the Stomatognathic System with a Fixed Metallic Orthodontic Appliance Having a Hot Temperature Source
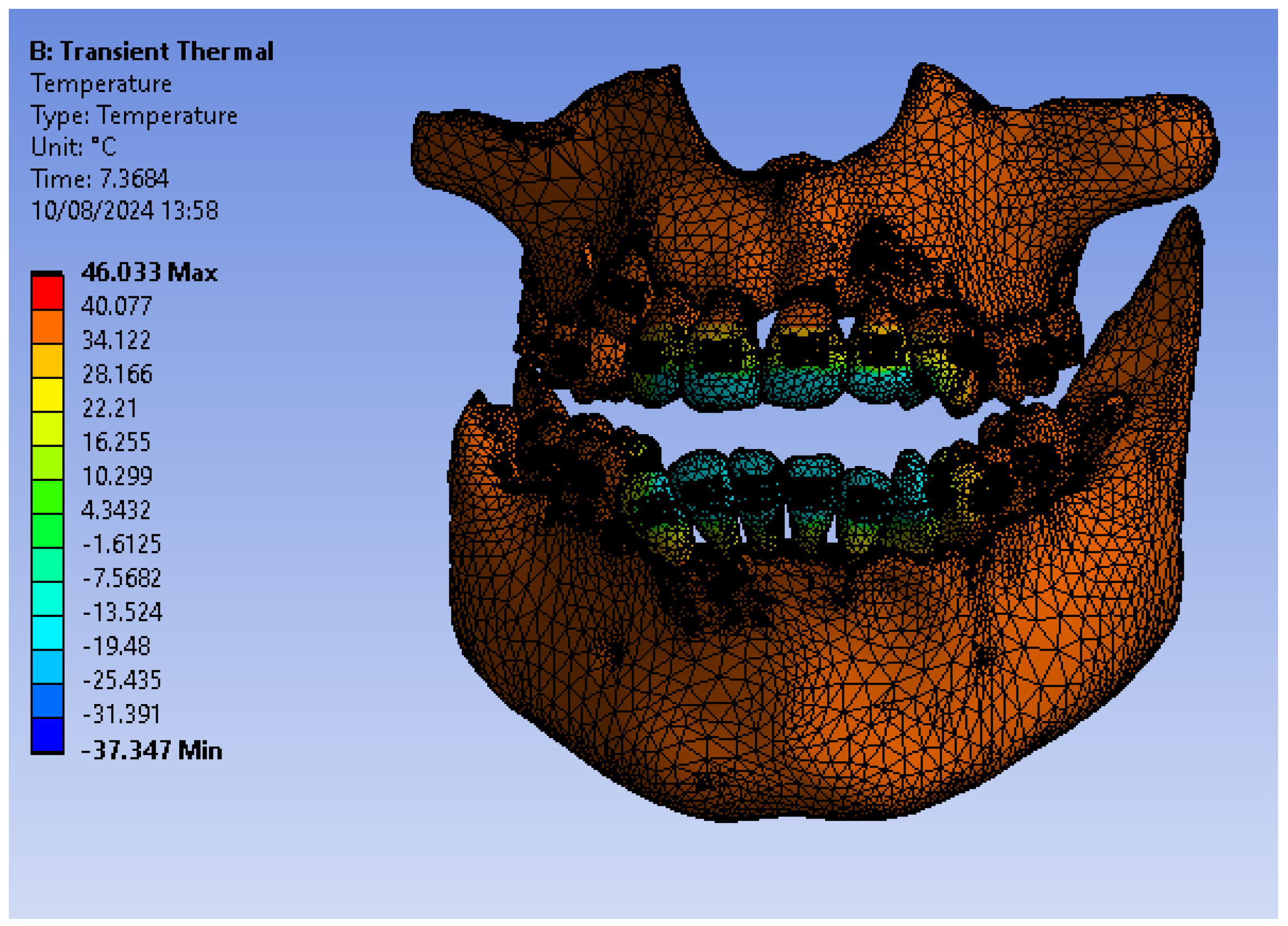
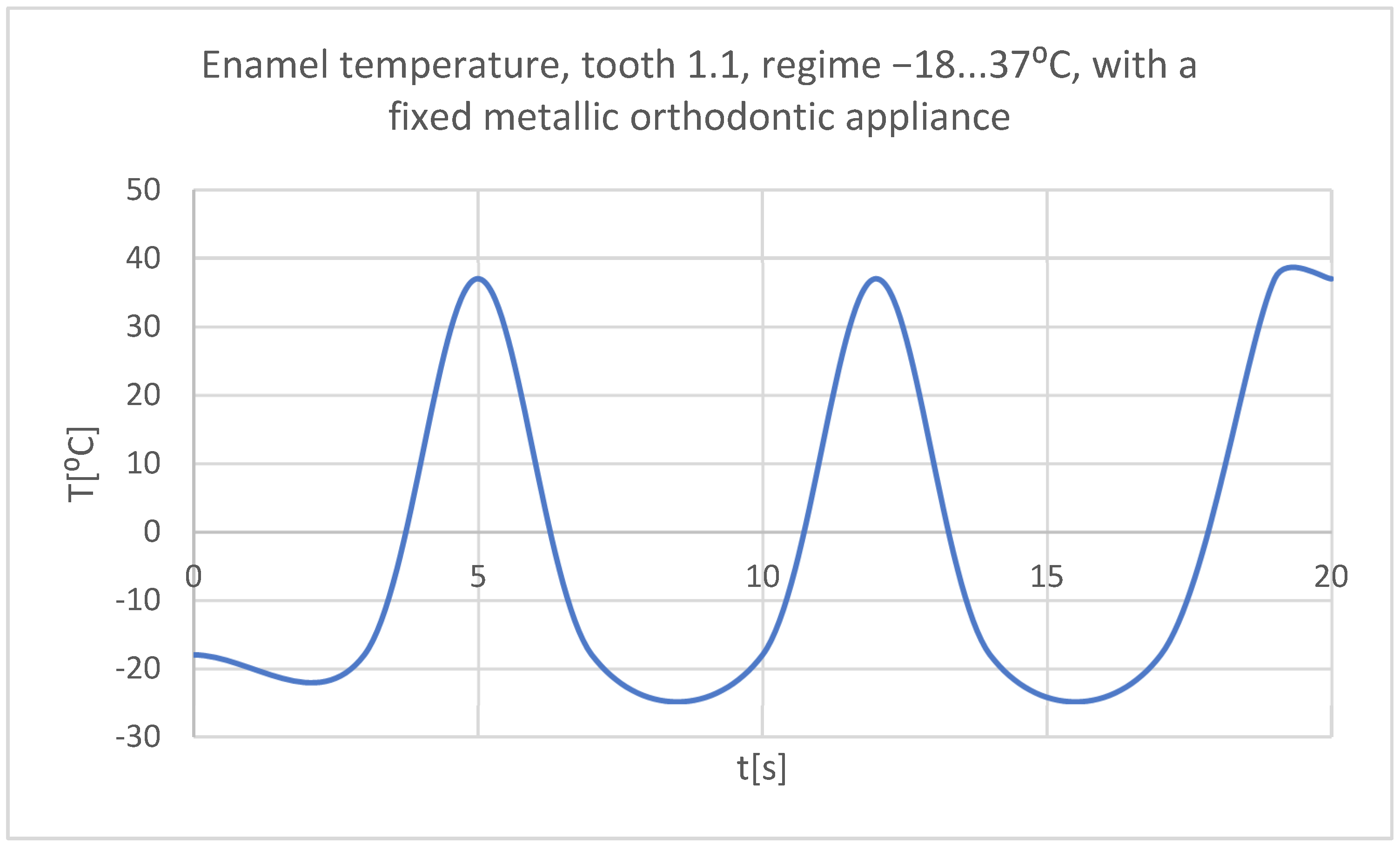
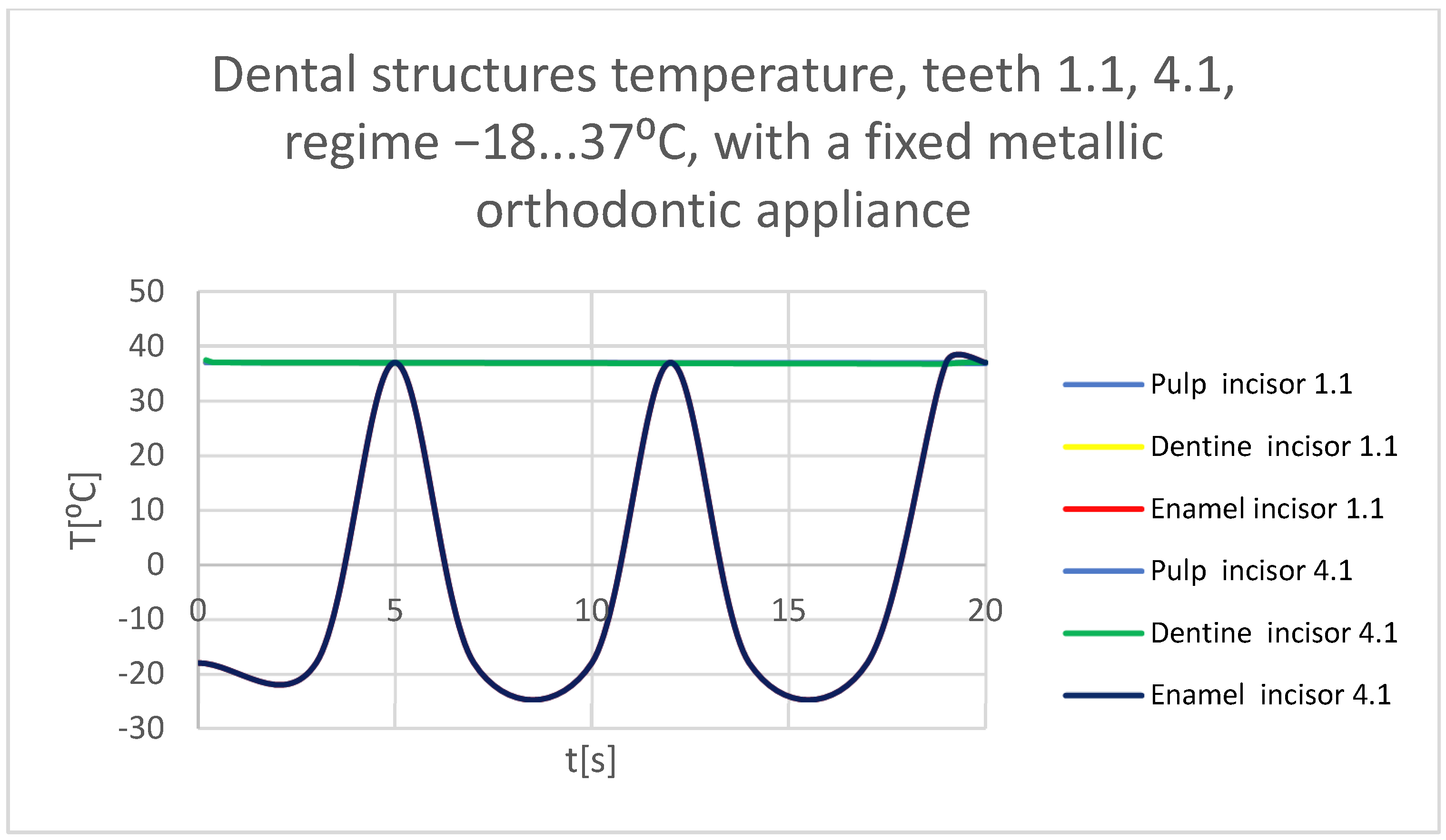
3.4. Thermal Simulation Results for the Stomatognathic System with a Fixed Metallic Orthodontic Appliance Having a Cold Temperature Source
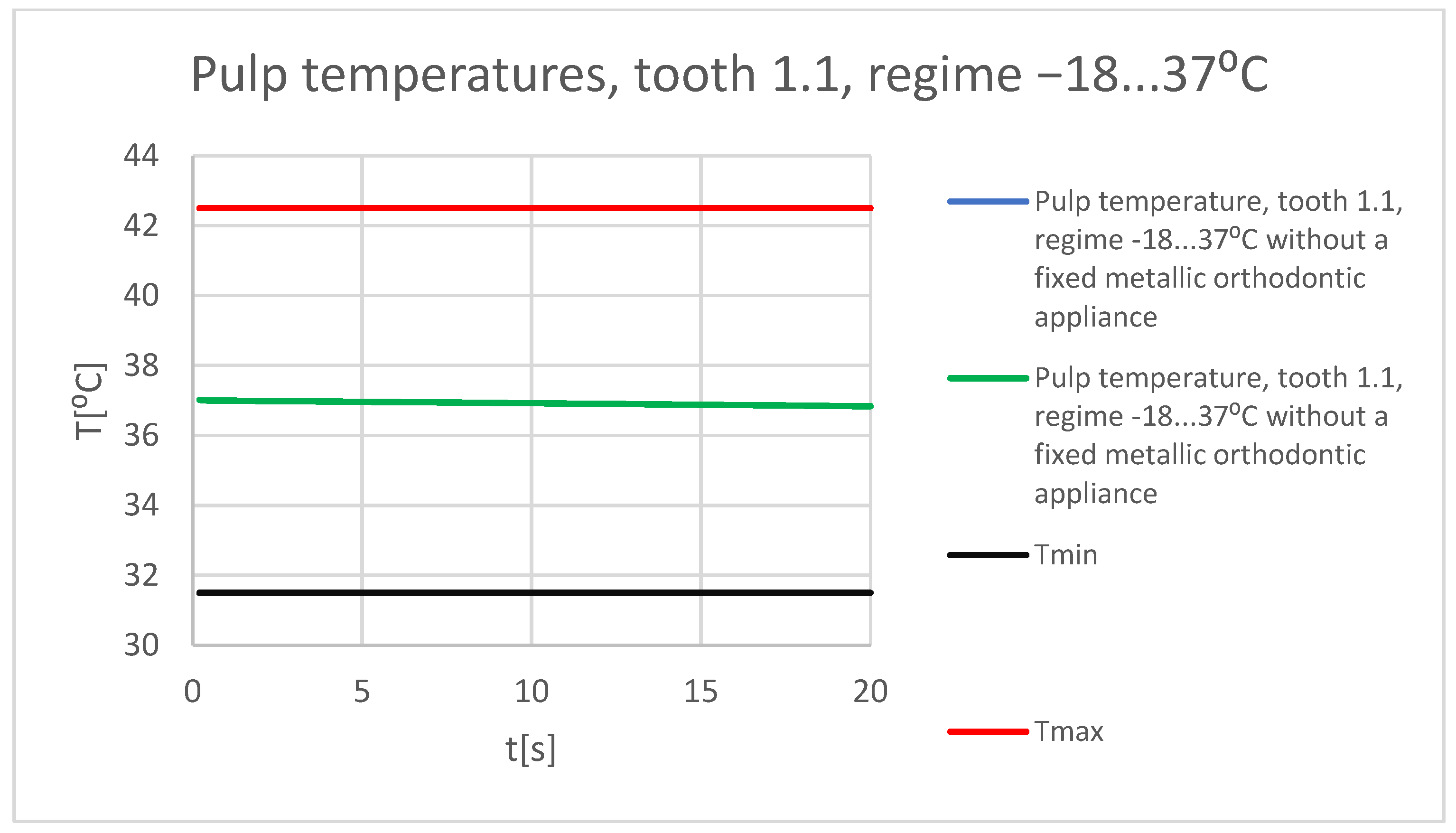
3.5. Comparative Diagrams
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Devi, L.B.; Keisam, A.; Singh, H.P. Malocclusion and occlusal traits among dental and nursing students of Seven North-East states of India. J. Oral Biol. Craniofac. Res. 2022, 12, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Alhammadi, M.; Halboub, E.; Salah-Fayed, M.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef] [PubMed]
- Friedlander-Barenboim, S.; Hamed, W.; Zini, A.; Yarom, N.; Abramovitz, I.; Chweidan, H.; Finkelstein, T.; Almoznino, G. Patterns of Cone-Beam Computed Tomography (CBCT) Utilization by Various Dental Specialties: A 4-Year Retrospective Analysis from a Dental and Maxillofacial Specialty Center. Healthcare 2021, 9, 1042. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Khoudhary, K.; Nagi, R.; Shukla, S.; Kaur, N.; Grover, D. New evolution of cone-beam computed tomography in dentistry: Combining digital technologies. Imaging Sci. Dent. 2019, 49, 179–190. [Google Scholar] [CrossRef]
- Petrescu, S.-M.-S.; Țuculină, M.J.; Popa, D.L.; Duță, A.; Sălan, A.I.; Voinea-Georgecu, R.; Diaconu, O.A.; Turcu, A.A.; Mocanu, H.; Nicola, A.G.; et al. Modeling and Simulating an Orthodontic System Using Virtual Methods. Diagnostics 2022, 12, 1296. [Google Scholar] [CrossRef]
- Katta, M.; Petrescu, S.-M.-S.; Dragomir, L.P.; Popescu, M.R.; Voinea-Georgescu, R.; Țuculină, M.J.; Popa, D.L.; Duță, A.; Diaconu, O.A.; Dascalu, I.T. Using the Finite Element Method to Determine the Odonto-Periodontal Stress for a Patient with Angle Class II Division 1 Malocclusion. Diagnostics 2023, 13, 1567. [Google Scholar] [CrossRef]
- Maya-Anaya, D.; Urriolagoitia-Sosa, G.; Romero-Ángeles, B.; Martinez-Mondragon, M.; German-Carcaño, J.M.; Correa-Corona, M.I.; Trejo-Enríquez, A.; Sánchez-Cervantes, A.; Urriolagoitia-Luna, A.; Urriolagoitia-Calderón, G.M. Numerical Analysis Applying the Finite Element Method by Developing a Complex Three-Dimensional Biomodel of the Biological Tissues of the Elbow Joint Using Computerized Axial Tomography. Appl. Sci. 2023, 13, 8903. [Google Scholar] [CrossRef]
- Zach, L.; Cohen, G. Pulp response to external heat. Oral Surg. 1965, 19, 515–530. [Google Scholar] [CrossRef]
- Korioth, T.W.; Versluis, A. Modeling the mechanical behavior of the jaws and their related structures by finite element (FE) analysis. Crit. Rev. Oral Biol. Med. 1997, 8, 90–104. [Google Scholar] [CrossRef]
- Rees, J.S.; Jacobsen, P.H. The effect of cuspal flexure on a buccal Class V restoration: A finite element study. J. Dent. 1998, 26, 361–367. [Google Scholar] [CrossRef]
- Toparli, M.; Gökay, N.; Aksoy, T. An investigation of temperature and stress distribution on a restored maxillary second premolar tooth using a three-dimensional finite element method. J. Oral Rehabil. 2000, 27, 1077–1081. [Google Scholar] [PubMed]
- Masouras, K.; Silikas, N.; Watts, D.C. Correlation of filler content and elastic properties of resin-composites. Dent. Mater. 2008, 24, 932–939. [Google Scholar] [CrossRef] [PubMed]
- Nica, I.; Rusu, V.; Păun, A.; Ștefănescu, C.; Vizureanu, P.; Alugulesei, A. Thermal properties of nanofilled and microfilled restorative composites. Mater. Plast. 2009, 18, 20. [Google Scholar]
- Hashemipour, M.A.; Mohammadpour, A.; Nassab, S.A. Transient thermal and stress analysis of maxillary second premolar tooth using an exact three-dimensional model. Indian J. Dent. Res. 2010, 21, 158–164. [Google Scholar] [CrossRef]
- Ausiello, P.; Franciosa, P.; Martorelli, M.; Watts, D.C. Numerical fatigue 3D-FE modeling of indirect composite-restored posterior teeth. Dent. Mater. 2011, 27, 423–430. [Google Scholar] [CrossRef]
- Alnazzawi, A.; Watts, D.C. Simultaneous determination of polymerization shrinkage, exotherm and thermal expansion coefficient for dental resin-composites. Dent. Mater. 2012, 28, 1240–1249. [Google Scholar] [CrossRef]
- Xie, H.; Deng, S.; Zhang, Y.; Zhang, J. Simulation study on convective heat transfer of the tongue in closed mouth. In Proceedings of the 8th IEEE International Conference on Software Engineering and Service Science (ICSESS), Beijing, China, 24–26 November 2017; pp. 802–805. [Google Scholar]
- Stănuşi, A.Ş.; Popa, D.L.; Ionescu, M.; Cumpătă, C.N.; Petrescu, G.S.; Ţuculină, M.J.; Dăguci, C.; Diaconu, O.A.; Gheorghiță, L.M.; Stănuşi, A. Analysis of Temperatures Generated During Conventional Laser Irradiation of Root Canals–A Finite Element Study. Diagnostics 2023, 13, 1757. [Google Scholar] [CrossRef]
- Huiskes, R.; Chao, E.Y.S. A Survey of Finite Element Analysis in Orthopedic Biomechanics: The First Decade. J. Biomech. 1983, 16, 385–409. [Google Scholar] [CrossRef]
- Shivakumar, S.; Kudagi, V.S.; Talwade, P. Applications of Finite Element Analysis in Dentistry: A Review. J. Int. Oral Health 2021, 13, 415–422. [Google Scholar]
- Rastegari, S.; Hosseini, S.M.; Hasani, M.; Jamilian, A. An Overview of Basic Concepts of Finite Element Analysis and Its Applications in Orthodontics. J. Dent. 2023, 11, 23–30. [Google Scholar] [CrossRef]
- Luchian, I.; Mârțu, M.A.; Tatarciuc, M.; Scutariu, M.M.; Ioanid, N.; Pasarin, L.; Kappenberg-Nițescu, D.C.; Sioustis, I.A.; Solomon, S.M. Using FEM to Assess the Effect of Orthodontic Forces on Affected Periodontium. Appl. Sci. 2021, 11, 7183. [Google Scholar] [CrossRef]
- Hetzler, S.; Rues, S.; Zenthöfer, A.; Rammelsberg, P.; Lux, C.J.; Roser, C.J. Finite Element Analysis of Fixed Orthodontic Retainers. Bioengineering 2024, 11, 394. [Google Scholar] [CrossRef] [PubMed]


























| Component | Density [kg/m3] | Isotropic Thermal Conductivity [W · m/°C] | Specific Heat [J · kg/°C] |
|---|---|---|---|
| Enamel | 2958 | 0.93 | 710 |
| Dentine | 2140 | 0.36 | 1302 |
| Dental pulp | 1000 | 0.0418 | 4200 |
| Mandible, maxillary | 2310 | 1 | 2650 |
| Bracket and tube-type elements, Ni + Cr alloy | 8500 | 13 | 460 |
| Orthodontic wires, Ni + Ti alloy | 6450 | 60 | 457 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrescu, S.-M.-S.; Rauten, A.-M.; Popescu, M.; Popescu, M.R.; Popa, D.L.; Ilie, D.; Duță, A.; Răcilă, L.D.; Vintilă, D.D.; Buciu, G. Assessment of Thermal Influence on an Orthodontic System by Means of the Finite Element Method. Bioengineering 2024, 11, 1002. https://doi.org/10.3390/bioengineering11101002
Petrescu S-M-S, Rauten A-M, Popescu M, Popescu MR, Popa DL, Ilie D, Duță A, Răcilă LD, Vintilă DD, Buciu G. Assessment of Thermal Influence on an Orthodontic System by Means of the Finite Element Method. Bioengineering. 2024; 11(10):1002. https://doi.org/10.3390/bioengineering11101002
Chicago/Turabian StylePetrescu, Stelian-Mihai-Sever, Anne-Marie Rauten, Mihai Popescu, Mihai Raul Popescu, Dragoș Laurențiu Popa, Dumitru Ilie, Alina Duță, Laurențiu Daniel Răcilă, Daniela Doina Vintilă, and Gabriel Buciu. 2024. "Assessment of Thermal Influence on an Orthodontic System by Means of the Finite Element Method" Bioengineering 11, no. 10: 1002. https://doi.org/10.3390/bioengineering11101002
APA StylePetrescu, S.-M.-S., Rauten, A.-M., Popescu, M., Popescu, M. R., Popa, D. L., Ilie, D., Duță, A., Răcilă, L. D., Vintilă, D. D., & Buciu, G. (2024). Assessment of Thermal Influence on an Orthodontic System by Means of the Finite Element Method. Bioengineering, 11(10), 1002. https://doi.org/10.3390/bioengineering11101002







