Mini-Implant Insertion Using a Guide Manufactured with Computer-Aided Design and Computer-Aided Manufacturing in an Adolescent Patient Suffering from Tooth Eruption Disturbance
Abstract
1. Introduction
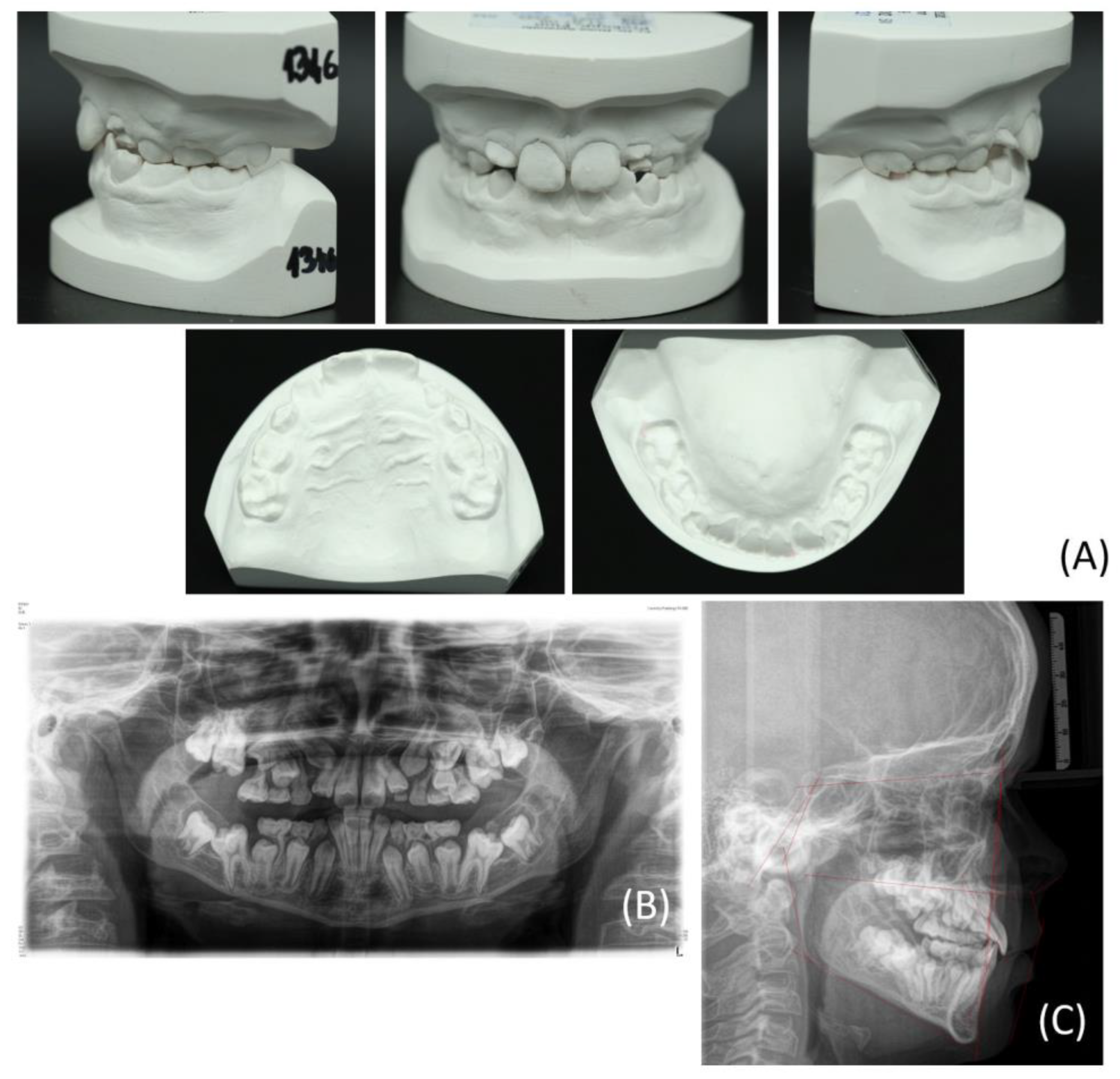
2. Clinical Example Presentation
2.1. Patient Case
2.2. Treatment Methods and Objectives
- Surgical exposure of the displaced and impacted teeth.
- RPE using a skeletal-anchorage Hyrax appliance.
- Resolution of the crossbite through maxillary transversal expansion.
- Alignment of the surgically exposed teeth by using skeletal anchorage, compensating for insufficient dentoalveolar support due to the reduced dentition.
- Eruption control of the displaced permanent teeth after dental arch expansion.
- Correction of the angulation, inclination, and rotation of the malpositioned teeth using a fixed orthodontic appliance.
2.3. Design and Manufacturing of the CAD/CAM Drilling Template
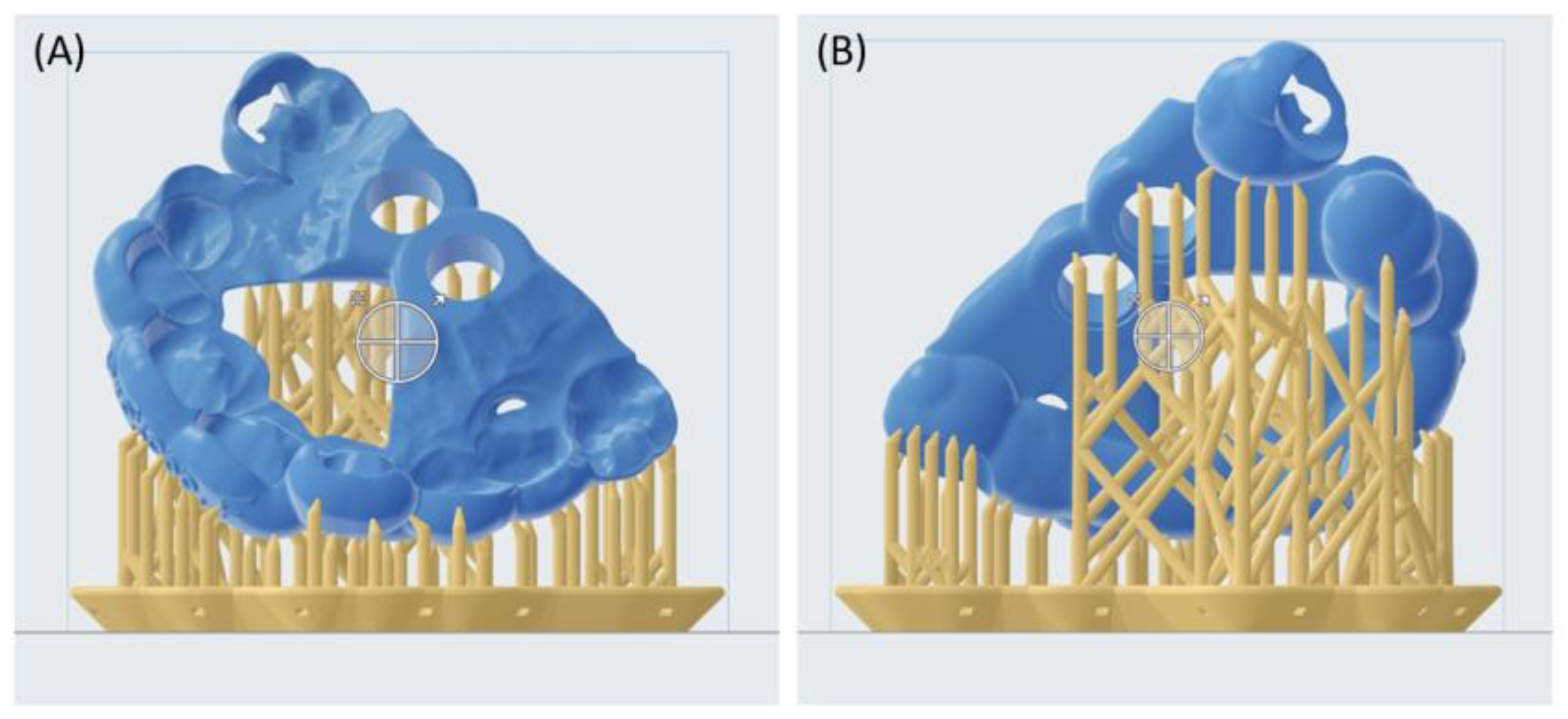
2.3.1. Digital Planning and Template Design
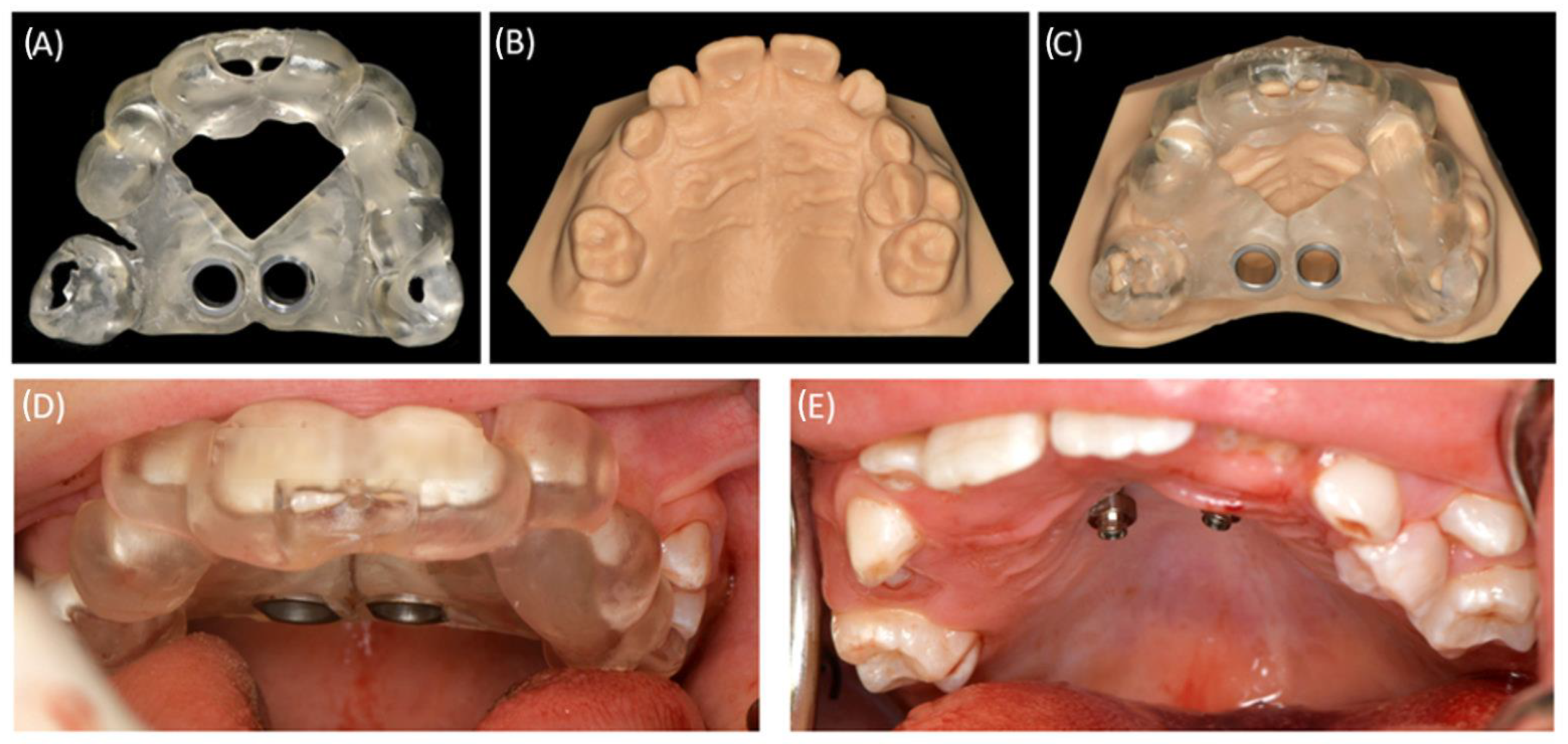
2.3.2. Manufacturing of the Drilling Template
2.3.3. Post-Processing of the Drilling Template
2.3.4. Supplementary CAM of a Model Cast
2.4. Treatment of the Clinical Example
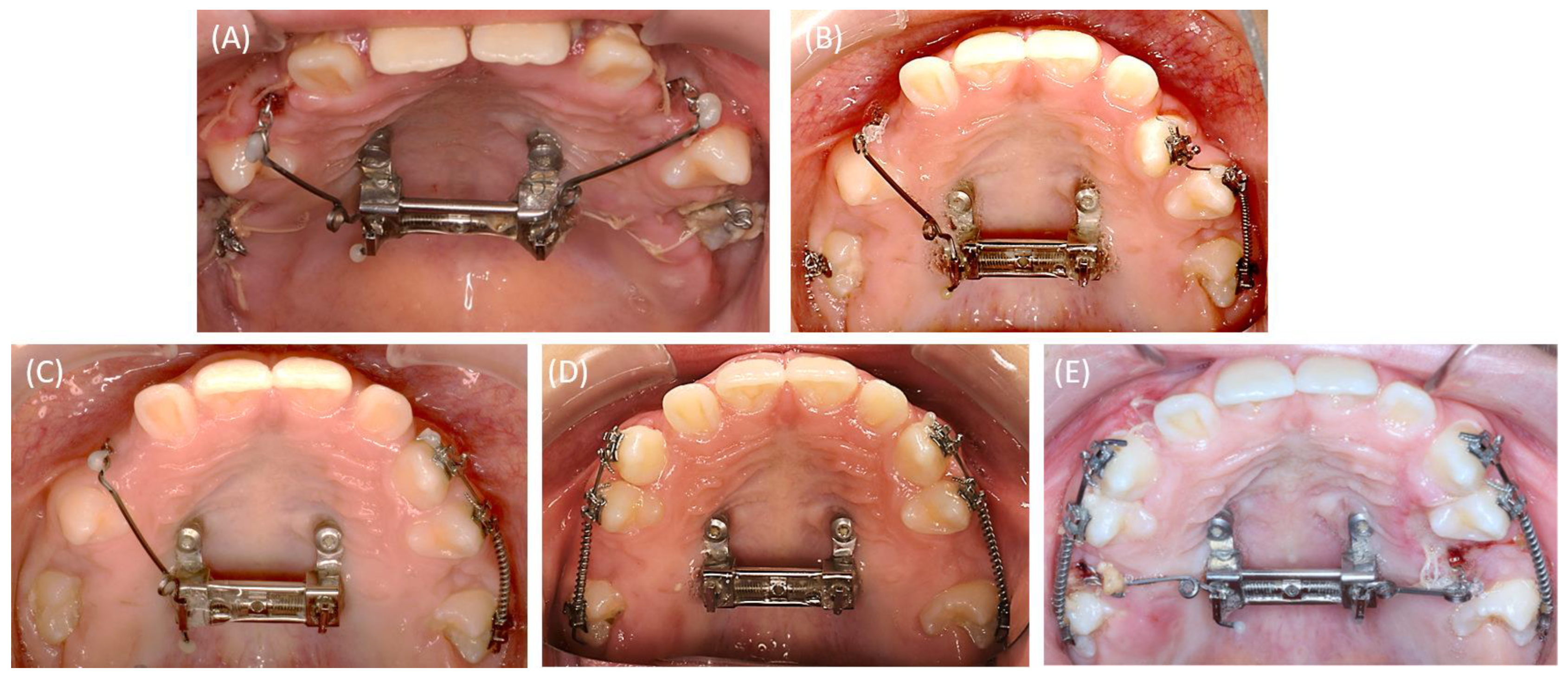
2.4.1. First Surgical Exposure of the Impacted Teeth and Insertion of the Mini-Implants
2.4.2. RPE Using the Skeletal-Anchorage Hyrax Appliance
2.4.3. Alignment of the Surgically Exposed Teeth by Using Skeletal Anchorage
3. Discussion
4. Conclusions
- Computer-aided static navigation techniques, applying IOS and CBCT, support a patient-specific, accurate, and safe planning for orthodontic mini-implant insertion.
- CAD/CAM technologies for the design and manufacturing of the insertion template have proven to be a feasible and efficient solution that can be easily implemented in the clinical routine, even in challenging patient cases.
- The presented protocol using CAD/CAM-based drilling templates might be supportive in the education of inexperienced clinicians.
- The skeletal-anchored Hyrax appliance provides an effective treatment for orthodontic therapy in challenging cases with a reduced dentition, allowing for both maxillary expansion and dental arch alignment in a single approach.
- The simultaneous insertion of mini-implants and the Hyrax appliance in a single intervention can optimize the treatment process.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fekonja, A. Evaluation of the eruption of permanent teeth and their association with malocclusion. Clin. Exp. Dent. Res. 2022, 8, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Bjerklin, K.; Kurol, J.; Valentin, J. Ectopic eruption of maxillary first permanent molars and association with other tooth and developmental disturbances. Eur. J. Orthod. 1992, 14, 369–375. [Google Scholar] [CrossRef]
- Björk, A.; Skieller, V. Facial development and tooth eruption. An implant study at the age of puberty. Am. J. Orthod. 1972, 62, 339–383. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Vig, K.W. Primary failure of eruption: A possible cause of posterior open-bite. Am. J. Orthod. 1981, 80, 173–190. [Google Scholar] [CrossRef]
- Rad, A.S.; Reid, J. Delayed eruption of a permanent molar associated with a complex odontoma: Report of case. ASDC J. Dent. Child. 1996, 63, 299–301. [Google Scholar] [PubMed]
- Raghoebar, G.M.; Boering, G.; Vissink, A.; Stegenga, B. Eruption disturbances of permanent molars: A review. J. Oral Pathol. Med. 1991, 20, 159–166. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Sundström, B.; Ravn, J.J. The effect of traumatic injuries to primary teeth on their permanent successors. I. A clinical and histologic study of 117 injured permanent teeth. Scand. J. Dent. Res. 1971, 79, 219–283. [Google Scholar] [CrossRef]
- Di Biase, D.D. Mucous membrane and delayed eruption. Dent. Pract. Dent. Rec. 1971, 21, 241–250. [Google Scholar]
- Shafer, A.W.; Hine, M.K.; Levy, B.M. Shafer’s Textbook of Oral Pathology, 7th ed.; Elsevier, a division of Reed Elsevier India Private Limited: New Delhi, India, 2012; ISBN 9788131230978. [Google Scholar]
- Jordan, R.C.K.; Sciubba, J.J.; Regezi, J.A. (Eds.) Oral Pathology: Clinical Pathologic Correlations: Clinical Pathologic Correlations, 7th ed.; Elsevier Health Sciences: St. Louis, MO, USA, 2017; ISBN 0323297684. [Google Scholar]
- Andreasen, J.O.; Petersen, J.K.; Laskin, D.M. (Eds.) Textbook and Color Atlas of Tooth Impactions, 1st ed.; Mosby; Munksgaard: St. Louis, MO, USA, 1997; ISBN 0323001467. [Google Scholar]
- Raghoebar, G.M.; Boering, G.; Jansen, H.W.; Vissink, A. Secondary retention of permanent molars: A histologic study. J. Oral Pathol. Med. 1989, 18, 427–431. [Google Scholar] [CrossRef]
- Nolla, C.M. The Development of Permanent Teeth. Ph.D. Thesis, University of Michigan, Ann Arbor, MI, USA, 1960; pp. 254–266. [Google Scholar]
- Suri, L.; Gagari, E.; Vastardis, H. Delayed tooth eruption: Pathogenesis, diagnosis, and treatment. A literature review. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 432–445. [Google Scholar] [CrossRef]
- Houston, W.J.B.; Tulley, W.J. A Textbook of Orthodontics; Wright: Bristol, UK, 1986; ISBN 0723607478. [Google Scholar]
- Costa, A.; Raffainl, M.; Melsen, B. Miniscrews as orthodontic anchorage: A preliminary report. Int. J. Adult Orthodon. Orthognath. Surg. 1998, 13, 201–209. [Google Scholar]
- Clarenbach, T.-H.; Wilmes, B.; Ihssen, B.; Vasudavan, S.; Drescher, D. Hybrid hyrax distalizer and mentoplate for rapid palatal expansion, class III treatment, and upper molar distalization. J. Clin. Orthod. 2017, 51, 317–325. [Google Scholar]
- Wilmes, B.; Ngan, P.; Liou, E.J.W.; Franchi, L.; Drescher, D. Early class III facemask treatment with the hybrid hyrax and Alt-RAMEC protocol. J. Clin. Orthod. 2014, 48, 84–93. [Google Scholar]
- Wilmes, B.; Nienkemper, M.; Ludwig, B.; Kau, C.H.; Drescher, D. Early Class III treatment with a hybrid hyrax-mentoplate combination. J. Clin. Orthod. 2011, 45, 15–21; quiz 39. [Google Scholar] [PubMed]
- MacGinnis, M.; Chu, H.; Youssef, G.; Wu, K.W.; Machado, A.W.; Moon, W. The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex—A finite element method (FEM) analysis. Prog. Orthod. 2014, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Tausche, E.; Hansen, L.; Schneider, M.; Harzer, W. [Bone-supported rapid maxillary expansion with an implant-borne Hyrax screw: The Dresden Distractor]. L’ Orthod. Fr. 2008, 79, 127–135. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Quinzi, V.; Ronsivalle, V.; Farronato, M.; Nicotra, C.; Indelicato, F.; Isola, G. Evaluation of Imaging Software Accuracy for 3-Dimensional Analysis of the Mandibular Condyle. A Comparative Study Using a Surface-to-Surface Matching Technique. Int. J. Environ. Res. Public Health 2020, 17, 4789. [Google Scholar] [CrossRef] [PubMed]
- Ronsivalle, V.; Venezia, P.; Bennici, O.; D’Antò, V.; Leonardi, R.; Lo Giudice, A. Accuracy of digital workflow for placing orthodontic miniscrews using generic and licensed open systems. A 3d imaging analysis of non-native .stl files for guided protocols. BMC Oral Health 2023, 23, 494. [Google Scholar] [CrossRef]
- Cassetta, M.; Altieri, F.; Di Giorgio, R.; Barbato, E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: Description of a technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef]
- Hourfar, J.; Ludwig, B.; Bister, D.; Braun, A.; Kanavakis, G. The most distal palatal ruga for placement of orthodontic mini-implants. Eur. J. Orthod. 2015, 37, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Aretxabaleta, M.; Unkovskiy, A.; Koos, B.; Spintzyk, S.; Xepapadeas, A.B. Accuracy Evaluation of Additively and Subtractively Fabricated Palatal Plate Orthodontic Appliances for Newborns and Infants—An In Vitro Study. Materials 2021, 14, 4103. [Google Scholar] [CrossRef]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Prescher, A.; Hölzle, F.; Modabber, A.; Wolf, M.; Peters, F. Accuracy of orthodontic mini-implants placed at the anterior palate by tooth-borne or gingiva-borne guide support: A cadaveric study. Clin. Oral Investig. 2019, 23, 4425–4431. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Kusnoto, B. Risks and complications of orthodontic miniscrews. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S43–S51. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M.A. Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 577–595.e7. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.-J.; Choi, Y.-J.; Evans, C.A.; Hwang, H.-S. Predictors of initial stability of orthodontic miniscrew implants. Eur. J. Orthod. 2011, 33, 528–532. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, B.; Glasl, B.; Bowman, S.J.; Wilmes, B.; Kinzinger, G.S.M.; Lisson, J.A. Anatomical guidelines for miniscrew insertion: Palatal sites. J. Clin. Orthod. 2011, 45, 433–441. [Google Scholar]
- Wilmes, B.; Ludwig, B.; Vasudavan, S.; Nienkemper, M.; Drescher, D. The T-Zone: Median vs. Paramedian Insertion of Palatal Mini-Implants. J. Clin. Orthod. 2016, 50, 543–551. [Google Scholar] [PubMed]
- Arqub, S.A.; Gandhi, V.; Mehta, S.; Palo, L.; Upadhyay, M.; Yadav, S. Survival estimates and risk factors for failure of palatal and buccal mini-implants. Angle Orthod. 2021, 91, 756–763. [Google Scholar] [CrossRef]
- Brettin, B.T.; Grosland, N.M.; Qian, F.; Southard, K.A.; Stuntz, T.D.; Morgan, T.A.; Marshall, S.D.; Southard, T.E. Bicortical vs monocortical orthodontic skeletal anchorage. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 625–635. [Google Scholar] [CrossRef]
- Hourfar, J.; Bister, D.; Kanavakis, G.; Lisson, J.A.; Ludwig, B. Influence of interradicular and palatal placement of orthodontic mini-implants on the success (survival) rate. Head Face Med. 2017, 13, 14. [Google Scholar] [CrossRef]
- Karagkiolidou, A.; Ludwig, B.; Pazera, P.; Gkantidis, N.; Pandis, N.; Katsaros, C. Survival of palatal miniscrews used for orthodontic appliance anchorage: A retrospective cohort study. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 767–772. [Google Scholar] [CrossRef]
- Zawawi, K.H. Acceptance of orthodontic miniscrews as temporary anchorage devices. Patient Prefer. Adherence 2014, 8, 933–937. [Google Scholar] [CrossRef][Green Version]
- Baumgaertel, S. Temporary skeletal anchorage devices: The case for miniscrews. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 558–564. [Google Scholar] [CrossRef]
- Chaushu, S.; Chaushu, G. Skeletal Implant Anchorage in the Treatment of Impacted Teeth—A Review of the State of the Art. Semin. Orthod. 2010, 16, 234–241. [Google Scholar] [CrossRef]
- Giancotti, A.; Arcuri, C.; Barlattani, A. Treatment of ectopic mandibular second molar with titanium miniscrews. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Nienkemper, M.; Pauls, A.; Ludwig, B.; Wilmes, B.; Drescher, D. Multifunctional use of palatal mini-implants. J. Clin. Orthod. 2012, 46, 679. [Google Scholar]
- McGuire, M.K.; Scheyer, E.T.; Gallerano, R.L. Temporary anchorage devices for tooth movement: A review and case reports. J. Periodontol. 2006, 77, 1613–1624. [Google Scholar] [CrossRef]
- Hodges, R.J.; Atchison, K.A.; White, S.C. Impact of cone-beam computed tomography on orthodontic diagnosis and treatment planning. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 665–674. [Google Scholar] [CrossRef]
- Bae, M.-J.; Kim, J.-Y.; Park, J.-T.; Cha, J.-Y.; Kim, H.-J.; Yu, H.-S.; Hwang, C.-J. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 893–901. [Google Scholar] [CrossRef]
- Qiu, L.; Haruyama, N.; Suzuki, S.; Yamada, D.; Obayashi, N.; Kurabayashi, T.; Moriyama, K. Accuracy of orthodontic miniscrew implantation guided by stereolithographic surgical stent based on cone-beam CT-derived 3D images. Angle Orthod. 2012, 82, 284–293. [Google Scholar] [CrossRef]
- Yu, J.-J.; Kim, G.-T.; Choi, Y.-S.; Hwang, E.-H.; Paek, J.; Kim, S.-H.; Huang, J.C. Accuracy of a cone beam computed tomography-guided surgical stent for orthodontic mini-implant placement. Angle Orthod. 2012, 82, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Unland, J.; Wilmes, B.; Tarraf, N.E.; Drescher, D. Is there an ideal insertion angle and position for orthodontic mini-implants in the anterior palate? A CBCT study in humans. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 345–354. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Pozzan, L.; Contardo, L. Does the planned miniscrew position reflect the achieved one? A clinical study on the reliability of guided miniscrew insertion using lateral cephalogram and maxillary stereolithography file for planning. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e312–e318. [Google Scholar] [CrossRef] [PubMed]
- Wilmes, B.; Tarraf, N.E.; de Gabriele, R.; Dallatana, G.; Drescher, D. CAD/CAM-gefertigte Insertions-Guides für die rein Mini-Implantatgetragene Gaumennahterweiterung. J. Orofac. Orthop. 2022, 83, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Casaña-Ruiz, M.D.; Bellot-Arcís, C.; Paredes-Gallardo, V.; García-Sanz, V.; Almerich-Silla, J.M.; Montiel-Company, J.M. Risk factors for orthodontic mini-implants in skeletal anchorage biological stability: A systematic literature review and meta-analysis. Sci. Rep. 2020, 10, 5848. [Google Scholar] [CrossRef]
- Küffer, M.; Drescher, D.; Becker, K. Application of the Digital Workflow in Orofacial Orthopedics and Orthodontics: Printed Appliances with Skeletal Anchorage. Appl. Sci. 2022, 12, 3820. [Google Scholar] [CrossRef]
- Graf, S.; Vasudavan, S.; Wilmes, B. CAD-CAM design and 3-dimensional printing of mini-implant retained orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 877–882. [Google Scholar] [CrossRef]
- Graf, S.; Cornelis, M.A.; Hauber Gameiro, G.; Cattaneo, P.M. Computer-aided design and manufacture of hyrax devices: Can we really go digital? Am. J. Orthod. Dentofac. Orthop. 2017, 152, 870–874. [Google Scholar] [CrossRef]



| Measurement | Value before Treatment | Measurement | Value before Treatment |
|---|---|---|---|
| SNA (82 ± 3°) | 83.3° | Interincisal angle 1–1 (131 ± 6°) | 131.6° |
| SNB (80 ± 3°) | 81.3° | OK1-NA (22.0 ± 3°) | 30.1° |
| AND (indiv.) | 4.8° | UK1-NB (25.0 ± 3°) | 16.3° |
| SN-Pg (82 ± 3°) | 80.7° | OK1O-NA (4.0 ± 2 mm) | 3.9 mm |
| NS-Ba (130 ± 6°) | 127.6° | UK1O-NB (4.0 ± 2 mm) | 2.9 mm |
| NL-NSL (8.5 ± 3°) | 9.9° | Overjet | 3 mm |
| ML-NSL (32.0 ± 6°) | 33.4° | Overbite | 3 mm |
| ML-NL (23.5 ± 3°) | 23.5° | Mandibular deviation | 1.5 mm right side |
| Wits appraisal (−0.3 ± 0.3 mm) | −1.0 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weismann, C.; Heise, K.; Aretxabaleta, M.; Cetindis, M.; Koos, B.; Schulz, M.C. Mini-Implant Insertion Using a Guide Manufactured with Computer-Aided Design and Computer-Aided Manufacturing in an Adolescent Patient Suffering from Tooth Eruption Disturbance. Bioengineering 2024, 11, 91. https://doi.org/10.3390/bioengineering11010091
Weismann C, Heise K, Aretxabaleta M, Cetindis M, Koos B, Schulz MC. Mini-Implant Insertion Using a Guide Manufactured with Computer-Aided Design and Computer-Aided Manufacturing in an Adolescent Patient Suffering from Tooth Eruption Disturbance. Bioengineering. 2024; 11(1):91. https://doi.org/10.3390/bioengineering11010091
Chicago/Turabian StyleWeismann, Christina, Kathrin Heise, Maite Aretxabaleta, Marcel Cetindis, Bernd Koos, and Matthias C. Schulz. 2024. "Mini-Implant Insertion Using a Guide Manufactured with Computer-Aided Design and Computer-Aided Manufacturing in an Adolescent Patient Suffering from Tooth Eruption Disturbance" Bioengineering 11, no. 1: 91. https://doi.org/10.3390/bioengineering11010091
APA StyleWeismann, C., Heise, K., Aretxabaleta, M., Cetindis, M., Koos, B., & Schulz, M. C. (2024). Mini-Implant Insertion Using a Guide Manufactured with Computer-Aided Design and Computer-Aided Manufacturing in an Adolescent Patient Suffering from Tooth Eruption Disturbance. Bioengineering, 11(1), 91. https://doi.org/10.3390/bioengineering11010091







