Orthognathic Surgery and Relapse: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Processing
2.2. Inclusion and Exclusion Criteria
3. Results
4. Discussion
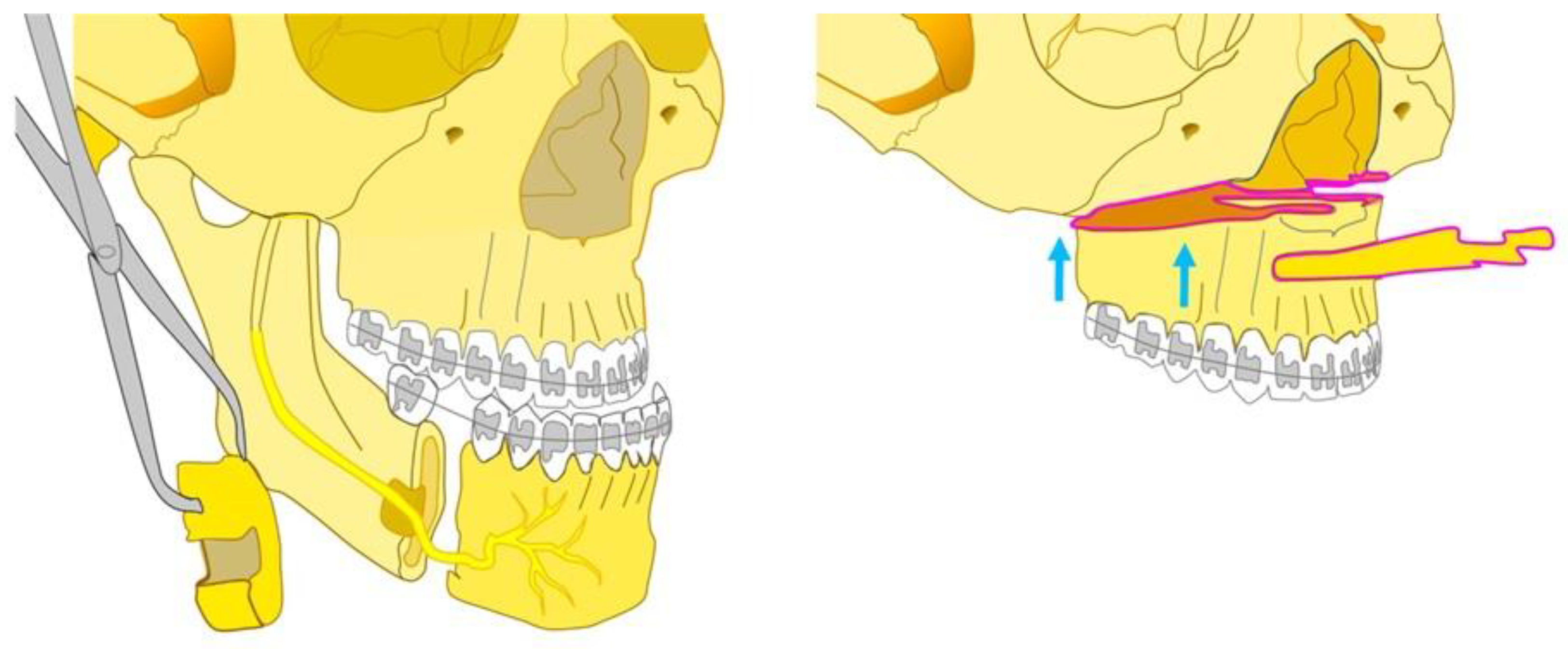
4.1. Le Fort 1 Osteotomy
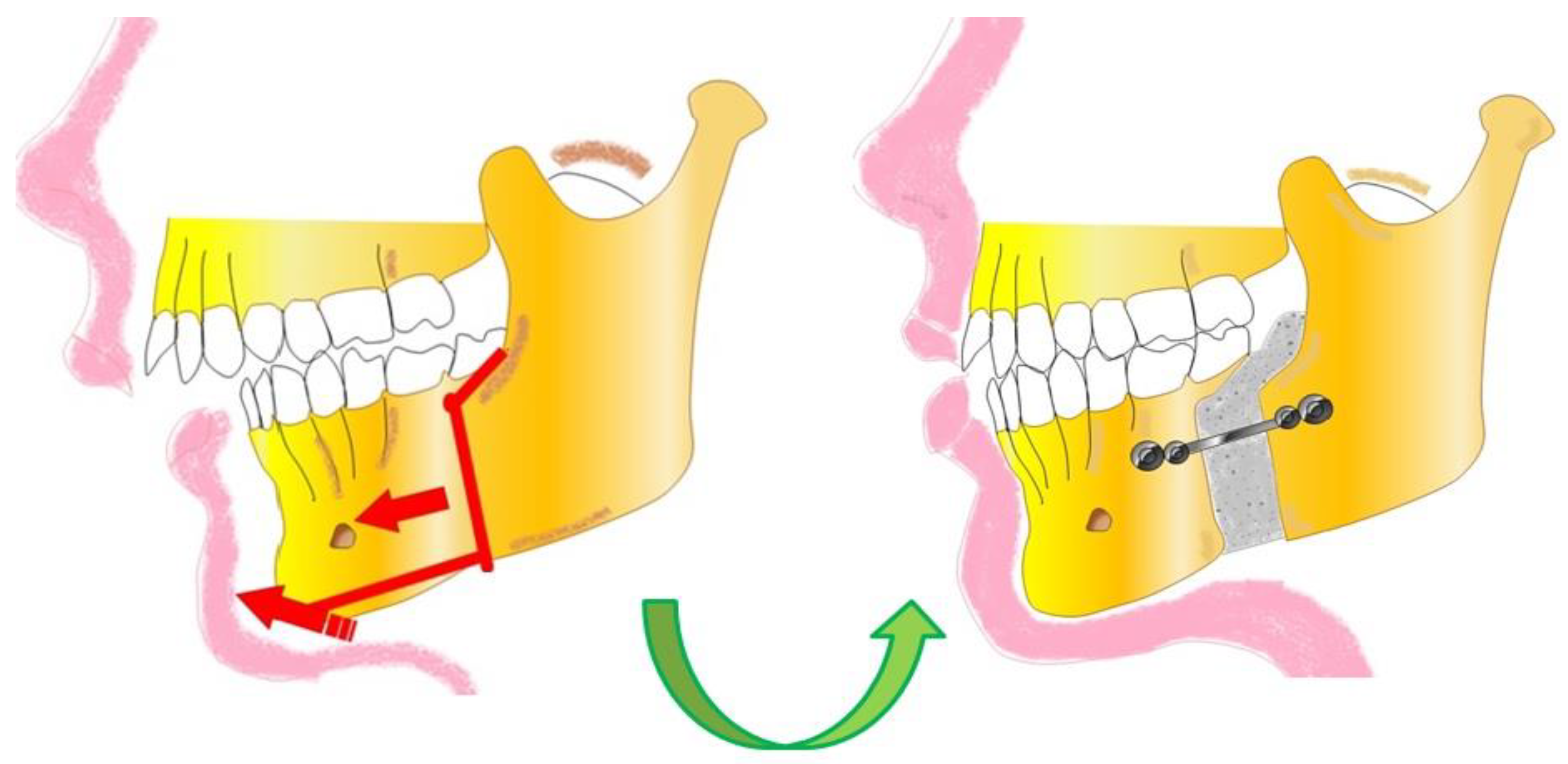
4.2. BSSO (Bilateral Sagittal Split Osteotomy)
4.3. Combined Maxillomandibular Approach
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Van Hemelen, G.; Van Genechten, M.; Renier, L.; Desmedt, M.; Verbruggen, E.; Nadjmi, N. Three-Dimensional Virtual Planning in Orthognathic Surgery Enhances the Accuracy of Soft Tissue Prediction. J. Craniomaxillofac. Surg. 2015, 43, 918–925. [Google Scholar] [CrossRef]
- Hamdy Mahmoud, M.; Ismail Elfaramawi, T. Maxillary Stability in Patients with Skeletal Class III Malocclusion Treated by Bimaxillary Orthognathic Surgery: Comparison of Mandible-First and Maxilla-First Approaches in a Randomised Controlled Study. Br. J. Oral Maxillofac. Surg. 2022, 60, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.-S.; Li, Y.-F. Comprehensive Correction of Maxillofacial Bone Deformity-Consideration and Combined Application of Orthognathic Surgery and Facial Contouring Surgery. Hua Xi Kou Qiang Yi Xue Za Zhi 2021, 39, 255–259. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Gentile, M.; Inchingolo, A.M.; Dipalma, G. Non-Syndromic Multiple Supernumerary Teeth in a Family Unit with a Normal Karyotype: Case Report. Int. J. Med. Sci. 2010, 7, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Brachvogel, P.; Berten, J.L.; Hausamen, J.E. Surgery before orthodontic treatment: A concept for timing the combined therapy of skeletal dysgnathias. Dtsch. Zahn Mund Kieferheilkd. Zentralblatt 1991, 79, 557–563. [Google Scholar]
- Lin, J.-H.; Li, C.; Wong, H.; Chamberland, S.; Le, A.D.; Chung, C.-H. Asymmetric Maxillary Expansion Introduced by Surgically Assisted Rapid Palatal Expansion: A Systematic Review. J. Oral Maxillofac. Surg. 2022, 80, 1902–1911. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Prevalence of Temporomandibular Disorders (TMD) in Pregnancy: A Systematic Review with Meta-analysis. J. Oral Rehabil. 2023, 50, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Bock, N.; Pancherz, H. Herbst Treatment of Class II Division 1 Malocclusions in Retrognathic and Prognathic Facial Types. Angle Orthod. 2006, 76, 930–941. [Google Scholar] [CrossRef]
- Barakat, A.; Alasseri, N.; Assari, A.S.; Koppolu, P.; Al-Saffan, A. A Case Report on Surgical-Orthodontic Correction of Skeletal Class III Malocclusion with Severe Prognathic Mandible and Retrognathic Maxilla. J. Pharm. Bioallied Sci. 2022, 14, S1054–S1058. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. [Google Scholar] [CrossRef]
- Mummolo, S.; Nota, A.; Marchetti, E.; Padricelli, G.; Marzo, G. The 3D Tele Motion Tracking for the Orthodontic Facial Analysis. BioMed Res. Int. 2016, 2016, 4932136. [Google Scholar] [CrossRef]
- Görgülü, S.; Sağdıç, D.; Akin, E.; Karaçay, S.; Bulakbası, N. Tongue Movements in Patients with Skeletal Class III Malocclusions Evaluated with Real-Time Balanced Turbo Field Echo Cine Magnetic Resonance Imaging. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e405–e414. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.M.; Lacerda-Santos, R.; de Oliveira, D.L.; Alves, J.V.; Britto, J.P.; Souza, E.d.S.; Alves, L.P.; Barbosa, G.; Coqueiro, R.d.S.; Santos, A.F.D. Esthetic Perception of Facial Profile after Treatment with the Thurow Appliance. Braz. Oral Res. 2015, 29, S1806-83242015000100220. [Google Scholar] [CrossRef]
- Philippe, F.; Mona, S.G. Surgical Treatment of a Borderline Skeletal Class III Patient: An Interdisciplinary Approach. Med. Arch. 2021, 75, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Coppotelli, E.; Incisivo, V.; Vernucci, R.A.; Mazzoli, V.; Barbato, E.; Silvestri, A. Orthodontic-Orthopedic-Surgical Treatment of Syndromic Third Class: Proposal of a New Craniofacial Cephalometric Method. J. Craniofac. Surg. 2019, 30, 1170–1173. [Google Scholar] [CrossRef] [PubMed]
- Preidl, R.H.M.; Kesting, M.; Rau, A. Perioperative Management in Patients with Cleft Lip and Palate. J. Craniofac. Surg. 2020, 31, 95–101. [Google Scholar] [CrossRef]
- Worley, M.L.; Patel, K.G.; Kilpatrick, L.A. Cleft Lip and Palate. Clin. Perinatol. 2018, 45, 661–678. [Google Scholar] [CrossRef]
- Alfwaress, F.S.D.; Khwaileh, F.A.; Rawashdeh, M.A.; Alomari, M.A.; Nazzal, M.S. Cleft Lip and Palate: Demographic Patterns and the Associated Communication Disorders. J. Craniofac. Surg. 2017, 28, 2117–2121. [Google Scholar] [CrossRef]
- Hong, M.; Kim, H.; Yang, I.-H.; Choi, J.-Y.; Lee, J.-H.; Kim, M.-J.; Chung, J.H.; Kim, S.; Baek, S.-H. Facial Asymmetry Phenotypes in Adult Patients with Unilateral Cleft Lip and Palate and Skeletal Class III Malocclusion Using Principal Component Analysis and Cluster Analysis. J. Craniofac. Surg. 2023, 34, e314–e319. [Google Scholar] [CrossRef]
- Ahn, H.-W.; Baek, S.-H. Skeletal Anteroposterior Discrepancy and Vertical Type Effects on Lower Incisor Preoperative Decompensation and Postoperative Compensation in Skeletal Class III Patients. Angle Orthod. 2011, 81, 64–74. [Google Scholar] [CrossRef]
- Sato, S.; Endo, N.; Yamauchi, M.; Takeuchi, M.; Suzuki, Y. Importance of posterior discrepancy in the development of skeletal Class III malocclusion. Kanagawa Shigaku 1989, 24, 219–229. [Google Scholar]
- Leck, R.; Paul, N.; Rolland, S.; Birnie, D. The Consequences of Living with a Severe Malocclusion: A Review of the Literature. J. Orthod. 2022, 49, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Jeyaraj, P.; Juneja, P. A Case of Extreme Skeletal Class III Malocclusion Beyond the Envelope of Discrepancy, Managed Effectively by a Modified Ortho-Surgical Protocol. J. Maxillofac. Oral Surg. 2021, 20, 201–218. [Google Scholar] [CrossRef] [PubMed]
- Fastuca, R.; Beccarini, T.; Rossi, O.; Zecca, P.A.; Caprioglio, A. Influence of Facial Components in Class III Malocclusion Esthetic Perception of Orthodontists, Patients, and Laypersons. J. Orofac. Orthop. 2022, 83, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-M.; Hsu, H.-J.; Hsu, K.-J.; Tseng, Y.-C. Clinical Significance of Postoperative Skeletal Relapse in the Treatment of Mandibular Prognathism: Receiver Operating Characteristic Curve Analysis. J. Formos. Med. Assoc. 2022, 121, 2593–2600. [Google Scholar] [CrossRef]
- Al-Sebaei, M.O. The Validity of Three Neo-Classical Facial Canons in Young Adults Originating from the Arabian Peninsula. Head Face Med. 2015, 11, 4. [Google Scholar] [CrossRef] [PubMed]
- Chiba, F.Y.; Chiba, E.K.; Moimaz, S.A.S.; Matsushita, D.H.; Garbin, A.J.Í.; Garbin, C.A.S. Malocclusion and Its Relationship with Oral Health-Related Quality of Life in Patients with Eating Disorders. Dent. Press J. Orthod. 2022, 27, e2220305. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, Y. BSSRO Improves Mandibular Morphology Mainly through Correction of Body Length and Volume in Patients with Asymmetric Mandibular Prognathism. J. Clin. Med. 2022, 11, 7131. [Google Scholar] [CrossRef]
- Straughan, D.M.; Yaremchuk, M.J. Improving Male Chin and Mandible Eesthetics. Clin. Plast. Surg. 2022, 49, 275–283. [Google Scholar] [CrossRef]
- Yi, J.S.; Jang, Y.J. Frequency and Characteristics of Facial Asymmetry in Patients with Deviated Noses. JAMA Facial Plast. Surg. 2015, 17, 265–269. [Google Scholar] [CrossRef]
- Prado, D.G.d.A.; Berretin-Felix, G.; Migliorucci, R.R.; Bueno, M.d.R.S.; Rosa, R.R.; Polizel, M.; Teixeira, I.F.; Gavião, M.B.D. Effects of Orofacial Myofunctional Therapy on Masticatory Function in Individuals Submitted to Orthognathic Surgery: A Randomized Trial. J. Appl. Oral Sci. 2018, 26, e20170164. [Google Scholar] [CrossRef] [PubMed]
- Chua, H.D.P.; Hägg, M.B.; Cheung, L.K. Cleft Maxillary Distraction versus Orthognathic Surgery—Which One Is More Stable in 5 Years? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 109, 803–814. [Google Scholar] [CrossRef]
- Dolce, C.; Hatch, J.P.; Van Sickels, J.E.; Rugh, J.D. Rigid versus Wire Fixation for Mandibular Advancement: Skeletal and Dental Changes after 5 Years. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 610–619. [Google Scholar] [CrossRef]
- Fahradyan, A.; Wolfswinkel, E.M.; Clarke, N.; Park, S.; Tsuha, M.; Urata, M.M.; Hammoudeh, J.A.; Yamashita, D.-D.R. Impact of the Distance of Maxillary Advancement on Horizontal Relapse After Orthognathic Surgery. Cleft Palate-Craniofacial J. 2018, 55, 546–553. [Google Scholar] [CrossRef]
- Perez, D.; Ellis, E. Sequencing Bimaxillary Surgery: Mandible First. J. Oral Maxillofac. Surg. 2011, 69, 2217–2224. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef]
- Perez, D.; Ellis, E. Implications of Sequencing in Simultaneous Maxillary and Mandibular Orthognathic Surgery. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2016, 24, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Tondin, G.M.; Leal, M.d.O.C.D.; Costa, S.T.; Grillo, R.; Jodas, C.R.P.; Teixeira, R.G. Evaluation of the Accuracy of Virtual Planning in Bimaxillary Orthognathic Surgery: A Systematic Review. Br. J. Oral Maxillofac. Surg. 2022, 60, 412–421. [Google Scholar] [CrossRef]
- NiÑo-Sandoval, T.C.; Almeida, R.d.A.C.; Vasconcelos, B.C.d.E. Incidence of Condylar Resorption after Bimaxillary, Lefort I, and Mandibular Surgery: An Overview. Braz. Oral Res. 2021, 35, e27. [Google Scholar] [CrossRef]
- Raffaini, M.; Magri, A.; Conti, M.; Arcuri, F. Advanced Facial Rejuvenation After Bimaxillary Surgery in Three Different Facial Types. Aesthetic Plast. Surg. 2022, 46, 183–193. [Google Scholar] [CrossRef]
- Choo, H.; Heo, H.-A.; Yoon, H.-J.; Chung, K.-R.; Kim, S.-H. Treatment Outcome Analysis of Speedy Surgical Orthodontics for Adults with Maxillary Protrusion. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e251–e262. [Google Scholar] [CrossRef]
- Tai, W.; Leung, Y.Y.; Li, D.T.S. What Are the Surgical Risks and 2-Year Stability of Mandibular Anterior Subapical Osteotomy in the Treatment of Dentoalveolar Protrusion? Clin. Oral Investig. 2022, 27, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Trilles, J.; Chaya, B.F.; Daar, D.A.; Anzai, L.; Boczar, D.; Rodriguez Colon, R.; Hirsch, D.L.; Jacobson, A.S.; Levine, J.P. Double-Barrel versus Single-Barrel Fibula Flaps for Mandibular Reconstruction: Safety and Outcomes. Laryngoscope 2022, 132, 1576–1581. [Google Scholar] [CrossRef]
- Wu, G. Commentary on: Assessment of Robot-Assisted Mandibular Contouring Surgery in Comparison With Traditional Surgery: A Prospective, Single-Center, Randomized Controlled Trial. Aesthetic Surg. J. 2022, 42, 580–581. [Google Scholar] [CrossRef] [PubMed]
- Ann, H.-R.; Jung, Y.-S.; Lee, K.-J.; Baik, H.-S. Evaluation of Stability after Pre-Orthodontic Orthognathic Surgery Using Cone-Beam Computed Tomography: A Comparison with Conventional Treatment. Korean J. Orthod. 2016, 46, 301–309. [Google Scholar] [CrossRef]
- Sahoo, N.K.; Agarwal, S.S.; Datana, S.; Bhandari, S.K. Long-Term Study of Relapse After Mandibular Orthognathic Surgery: Advancement Versus Setback. J. Maxillofac. Oral Surg. 2022, 21, 469–480. [Google Scholar] [CrossRef]
- Chung, E.H.; Borzabadi-Farahani, A.; Yen, S.L.-K. Clinicians and Laypeople Assessment of Facial Attractiveness in Patients with Cleft Lip and Palate Treated with LeFort I Surgery or Late Maxillary Protraction. Int. J. Pediatr. Otorhinolaryngol. 2013, 77, 1446–1450. [Google Scholar] [CrossRef] [PubMed]
- Botticelli, S.; Küseler, A.; Marcusson, A.; Mølsted, K.; Nørholt, S.E.; Cattaneo, P.M.; Pedersen, T.K. Do Infant Cleft Dimensions Have an Influence on Occlusal Relations? A Subgroup Analysis Within an RCT of Primary Surgery in Patients With Unilateral Cleft Lip and Palate. Cleft Palate Craniofacial J. 2020, 57, 378–388. [Google Scholar] [CrossRef]
- Verlinden, C.R.A.; van de Vijfeijken, S.E.C.M.; Tuinzing, D.B.; Jansma, E.P.; Becking, A.G.; Swennen, G.R.J. Complications of Mandibular Distraction Osteogenesis for Developmental Deformities: A Systematic Review of the Literature. Int. J. Oral Maxillofac. Surg. 2015, 44, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Neeraj; Reddy, S.G.; Dixit, A.; Agarwal, P.; Chowdhry, R.; Chug, A. Relapse and Temporomandibular Joint Dysfunction (TMD) as Postoperative Complication in Skeletal Class III Patients Undergoing Bimaxillary Orthognathic Surgery: A Systematic Review. J. Oral Biol. Craniofacial Res. 2021, 11, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Yun, I.S.; Park, B.-Y.Y. Outcome of Early Rigid Fixation and Removal of Rigid External Distraction System after Distraction Osteogenesis of the Midface. J. Craniofacial Surg. 2011, 22, 576–580. [Google Scholar] [CrossRef]
- Gassmann, C.J.; Van Sickels, J.E.; Thrash, W.J. Causes, Location, and Timing of Relapse Following Rigid Fixation after Mandibular Advancement. J. Oral Maxillofac. Surg. 1990, 48, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Eggensperger, N.; Smolka, K.; Luder, J.; Iizuka, T. Short- and Long-Term Skeletal Relapse after Mandibular Advancement Surgery. Int. J. Oral Maxillofac. Surg. 2006, 35, 36–42. [Google Scholar] [CrossRef]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Fiorillo, L.; Cervino, G.; Cicciù, M. Economic Inequalities and Temporomandibular Disorders: A Systematic Review with Meta-analysis. J. Oral Rehabil. 2023, 50, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Thiem, D.G.E.; Schneider, D.; Hammel, M.; Saka, B.; Frerich, B.; Al-Nawas, B.; Kämmerer, P.W. Complications or Rather Side Effects? Quantification of Patient Satisfaction and Complications after Orthognathic Surgery—A Retrospective, Cross-Sectional Long-Term Analysis. Clin. Oral Investig. 2021, 25, 3315–3327. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Ji, H.; Du, W.; Xu, C.; Luo, E. Management of Condylar Resorption before or after Orthognathic Surgery: A Systematic Review. J. Craniomaxillofacial Surg. 2019, 47, 1007–1014. [Google Scholar] [CrossRef]
- Gaitan-Romero, L.; Shujaat, S.; Ma, H.; Orhan, K.; Shaheen, E.; Mulier, D.; Willems, G.; Politis, C.; Jacobs, R. Evaluation of Long-Term Hard Tissue Relapse Following Surgical–Orthodontic Treatment in Skeletal Class II Patients: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Damrongsirirat, N.; Kaboosaya, B.; Siriwatana, K.; Subbalekha, K.; Jansisyanont, P.; Pimkhaokham, A. Complications Related to Orthognathic Surgery: A 10-Year Experience in Oral and Maxillofacial Training Center. J. Cranio-Maxillofac. Surg. 2022, 50, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kim, H.; Cha, K.-S. Evaluation of the Stability of Maxillary Expansion Using Cone-Beam Computed Tomography after Segmental Le Fort I Osteotomy in Adult Patients with Skeletal Class III Malocclusion. Korean J. Orthod. 2018, 48, 63. [Google Scholar] [CrossRef]
- da Costa Senior, O.; De Temmerman, G.; Falter, B.; Politis, C. Modified Intraoral C-Osteotomy. J. Craniofacial Surg. 2021, 32, 2202–2204. [Google Scholar] [CrossRef]
- da Silva, W.S.; de Almeida, A.L.P.F.; Pucciarelli, M.G.R.; Neppelenbroek, K.H.; da Silva de Menezes, J.D.; Yaedú, R.Y.F.; Oliveira, T.M.; Cintra, F.M.R.N.; Soares, S. Relapse after Le Fort I Surgery in Oral Cleft Patients: A 2-Year Follow-up Using Digitized and 3D Models. Odontology 2018, 106, 445–453. [Google Scholar] [CrossRef]
- Al-Delayme, R.M.A.; Alsagban, A.A.R.; Ahmed, F.T.; Farag, A.; Al-Allaq, T.; Virdee, P.; Alnajjar, Z.; Alsamaraie, S.A.I.; Elnashef, S.; Arab, L.; et al. The Direction of Double-Jaw Surgery Relapse for Correction of Skeletal Class III Deformity: Bilateral Sagittal Split Versus Intraoral Vertical Ramus Setback Osteotomies. J. Maxillofac. Oral Surg. 2019, 18, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Politis, C.; Jacobs, R.; De Laat, A.; De Grauwe, A. TMJ Surgery Following Orthognathic Surgery: A Case Series. Oral Maxillofac. Surg. Cases 2018, 4, 39–52. [Google Scholar] [CrossRef]
- Peleg, O.; Mahmoud, R.; Shuster, A.; Arbel, S.; Kleinman, S.; Mijiritsky, E.; Ianculovici, C. Vertical Ramus Osteotomy, Is It Still a Valid Tool in Orthognathic Surgery? IJERPH 2022, 19, 10171. [Google Scholar] [CrossRef]
- Antonarakis, G.S.; Herzog, G.; Kiliaridis, S. Vertical Relapse after Orthodontic and Orthognathic Surgical Treatment in a Patient with Myotonic Dystrophy. Eur. J. Paediatr. Dent. 2019, 20, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Ronsivalle, V.; Shapira, I.; Cicciù, M. Prevalence of Temporomandibular Disorders in Subjects Affected by Parkinson Disease: A Systematic Review and Metanalysis. J. Oral Rehabil. 2023, 50, 877–885. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Crimi, S.; Badnjević, A.; Cervino, G.; Bianchi, A.; Cicciù, M. Correlation between Temporomandibular Disorders (TMD) and Posture Evaluated Trough the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD): A Systematic Review with Meta-Analysis. J. Clin. Med. 2023, 12, 2652. [Google Scholar] [CrossRef]
- Park, Y.-W.; Kang, H.-S.; Lee, J.-H. Comparative Study on Long-Term Stability in Mandibular Sagittal Split Ramus Osteotomy: Hydroxyapatite/Poly-l-Lactide Mesh versus Titanium Miniplate. Maxillofac. Plast. Reconstr. Surg. 2019, 41, 8. [Google Scholar] [CrossRef]
- Aich, S.; Singarapu, R.; Shetty, A.; Rathna, K.; Purvey, P.K.; Shaju, A. Evaluation of Sagittal Curving Osteotomy vs Conventional Advancement Genioplasty in Retrogenia Patients: A Randomized Control Trial. J. Maxillofac. Oral Surg. 2022, 21, 1244–1258. [Google Scholar] [CrossRef] [PubMed]

| Authors and Year | Type | Aim | Materials and Methods | Results |
|---|---|---|---|---|
| Kim et al., 2018 [61] | Randomized clinical study | In adult patients with skeletal class III malocclusion who need maxillary expansion, to use cone-beam computed tomography (CBCT) to assess the stability of the skeletal and dental widths after segmental Le Fort 1 osteotomy. | Le Fort 1 osteotomies (control group) and segmental Le Fort 1 osteotomies (experimental group) were performed on 25 and 36 patients with skeletal class III malocclusion, respectively. The skeletal and dental widths were measured on CBCT pictures (T1, T2, and T3) before, after, and at the end of the course of therapy. It was shown that the degree of relapse in the experimental group and the extent of surgery were correlated. | In the experimental group, the amount of segmental Le Fort 1 skeletal expansion was inversely correlated with the degree of postoperative skeletal relapse. |
| Fahradyan et al., 2018 [35] | Prospective study | Examine the relationship between the degree of maxillary advancement and relapse. | Between 2008 and 2015, bimaxillary surgery and either a Le Fort 1 or a Le Fort 1 with mandibular setback were performed on individuals with class III skeletal malocclusions. | The horizontal relapse was 1.8 mm and the mean maxillary advancement was 6.3 mm for a relapse of 28.6%. |
| Sahoo. et al., 2020 [47] | Study in vivo | Think about relapse in the long term compared to the short term. | 46 patients who underwent mandibular orthognathic surgery had their medical records split into two categories, surgery for mandibular advancement and surgery for mandibular setback. | The amount of surgical movement and the intraoperative change in mandibular plane angle were substantially linked with relapse in both groups (p values for each were 0.05). |
| da Costa Senior et al., 2021 [62] | Study in vivo | This study’s objective was to assess how well the surgical technique addresses condilar relapse. | 7 patients underwent bilateral sagittal split osteotomies, and 2 additional Le fort 1 osteotomies and TMJ surgeries were performed in 2 cases. | Patients who require additional orthognathic surgery and those who experience malocclusion after condylar resorption may find relief with the modified C-osteotomy. |
| da Silva et al., 2018 [63] | Retrospective study | To evaluate and find relapse after orthognathic surgery for maxillary advancement (Le Fort 1 maxillary osteotomy in oral cleft patients two years later); to analyze digital cephalograms and three-dimensional dental models. | Dental casts and lateral cephalograms were performed on 17 people. The digital cephalometric tracings were assessed in T1 (before surgery), T2 (immediately after surgery), and T3–6 months to 1 year after surgery. The dental casts are displayed in F1, F2, and F3. | While the other parameters under investigation were unaffected, cephalometry revealed a relapse in the vertical movement following maxillary advancement utilizing orthognathic surgery. |
| Al-Delayme et al, 2018 [64] | Prospective comparative clinical trial | Assess the postoperative stability of the double-jaw surgical treatment of skeletal class III deformities, and compare the two distinct mandibular surgical procedures. | 12 patients with skeletal class III malocclusions were included in this study. The patients underwent BSSO or IVRO in addition to a Le Fort 1 osteotomy for double-jaw surgery. Prior to T0, immediately after the procedure (T1), and one year later, lateral cephalograms were performed. | The average mandibular setback and maxillary advancement in the BSSO group were respectively 6.22 mm at B point and 2.93 mm at point A, with relapse rates of 24.9 and 26.6. |
| Politis et al., 2018 [65] | Retrospective cohort study | After orthognathic surgery, assess the need for TMJ surgery. | 630 patients underwent Le Fort 1 osteotomies or sagittal split osteotomies between January 2013 and December 2016. | Individuals with internal derangement only showed severe occlusal anomalies in one case, unlike those with bilateral condylar resorption, where the skeletal relapse persisted as a problem. |
| Peleg et al., 2022 [66] | Retrospective cohort study | During orthognathic surgery, look into mandibular operations, paying close attention to the two most common procedures between January 2010 and December 2019: IVRO and SSO. | There were 144 patients altogether. IVRO:SSO procedures were 118:26 in number. | Overall, there were 53 problems/issues following surgery, such as skeletal relapse, temporomandibular joint dysfunction, etc. |
| Antonarakis., et al., 2019 [67] | Case report | To provide the first case of combined orthodontic and orthognathic surgical therapy for a patient with MD who has had a lengthy, well-documented follow-up using radiography. | Orthognathic and orthodontic surgery were performed on a 17-year-old male patient who had a significant open bite, a long, tapering face, and MD type 1. | Long-term stability issues in a patient with MD who underwent orthognathic surgery and orthodontic treatment to close his anterior open bite are discussed. |
| Tai Wayne et al., 2022 [43] | Retrospective study | To assess the stability and negative consequences of mandibular anterior subapical osteotomy (ASO) as a therapy for bimaxillary dentoalveolar protrusion. | Between 2008 and 2017, 120 individuals who underwent orthognathic surgery at a single hospital were included. Serial lateral cephalogram traces were taken prior to surgery (T1), six weeks after surgery (T2), and two years following surgery in order to evaluate relapse. | L1-MP increased on average by 12, 7°. At 2 years following surgery, 96.7% of patients had a mean L1-MP relapse of 2.9°. There was no clear factor that enhanced the chance of relapse and the degree of surgical repositioning was only sporadically connected with that of relapse, etc. |
| Peleg et al., 2022 [66] | Retrospective cohort study | During orthognathic surgery, look into mandibular operations, paying attention to the two most common procedures between January 2010 and December 2019: IVRO and SSO. | There were 144 patients altogether. IVRO:SSO procedures were 118:26 in number. | Overall, there were 53 problems/issues following surgery, such as skeletal relapse, temporomandibular joint dysfunction, etc. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.M.; Patano, A.; Piras, F.; Ruvo, E.d.; Ferrante, L.; Noia, A.D.; Dongiovanni, L.; Palermo, A.; Inchingolo, F.; Inchingolo, A.D.; et al. Orthognathic Surgery and Relapse: A Systematic Review. Bioengineering 2023, 10, 1071. https://doi.org/10.3390/bioengineering10091071
Inchingolo AM, Patano A, Piras F, Ruvo Ed, Ferrante L, Noia AD, Dongiovanni L, Palermo A, Inchingolo F, Inchingolo AD, et al. Orthognathic Surgery and Relapse: A Systematic Review. Bioengineering. 2023; 10(9):1071. https://doi.org/10.3390/bioengineering10091071
Chicago/Turabian StyleInchingolo, Angelo Michele, Assunta Patano, Fabio Piras, Elisabetta de Ruvo, Laura Ferrante, Angela Di Noia, Leonardo Dongiovanni, Andrea Palermo, Francesco Inchingolo, Alessio Danilo Inchingolo, and et al. 2023. "Orthognathic Surgery and Relapse: A Systematic Review" Bioengineering 10, no. 9: 1071. https://doi.org/10.3390/bioengineering10091071
APA StyleInchingolo, A. M., Patano, A., Piras, F., Ruvo, E. d., Ferrante, L., Noia, A. D., Dongiovanni, L., Palermo, A., Inchingolo, F., Inchingolo, A. D., & Dipalma, G. (2023). Orthognathic Surgery and Relapse: A Systematic Review. Bioengineering, 10(9), 1071. https://doi.org/10.3390/bioengineering10091071












