Morphological Study of the Mandibular Lingula and Antilingula by Cone-Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Conditions
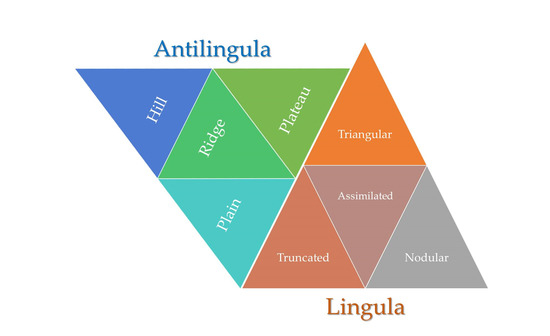
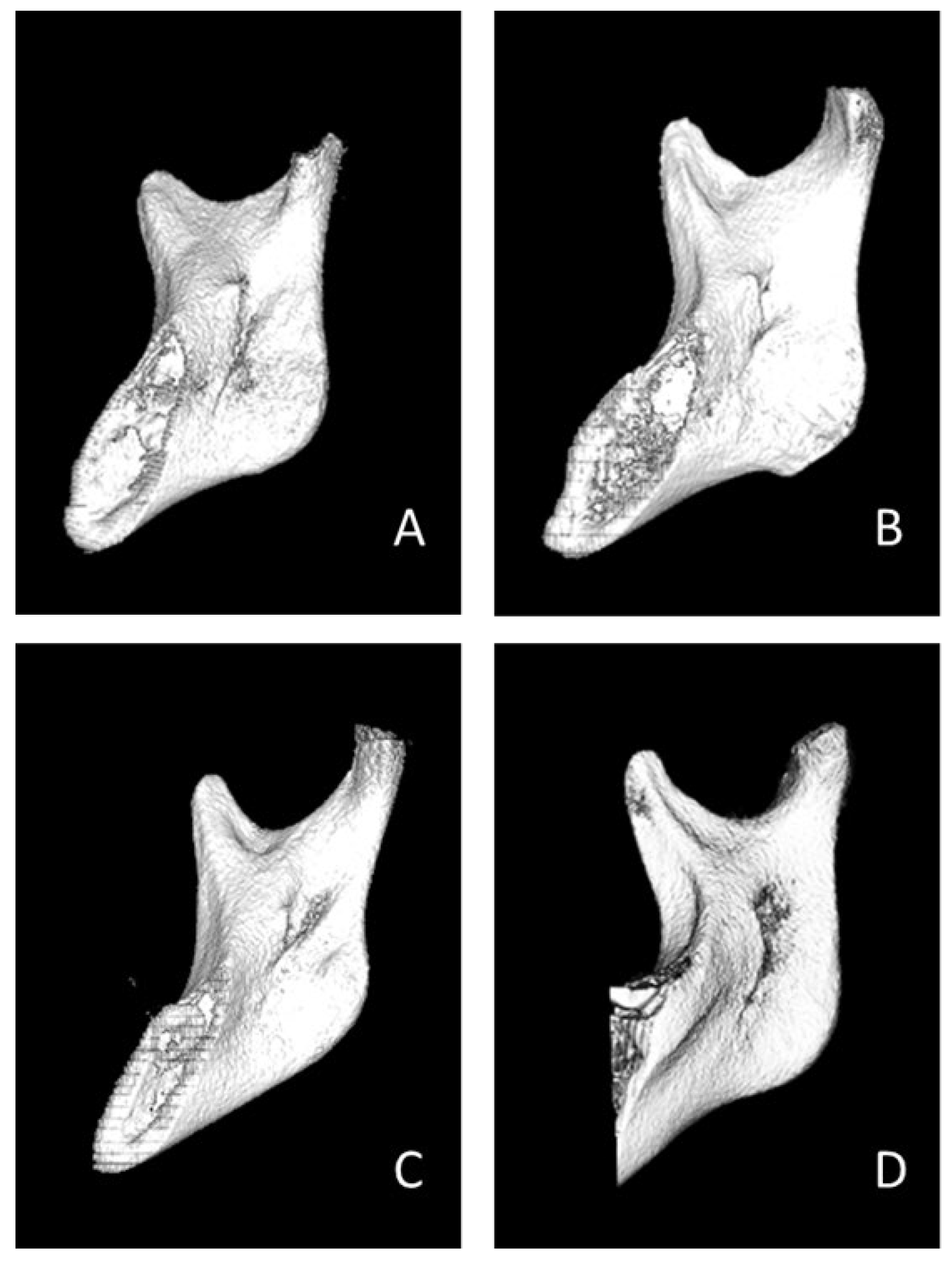
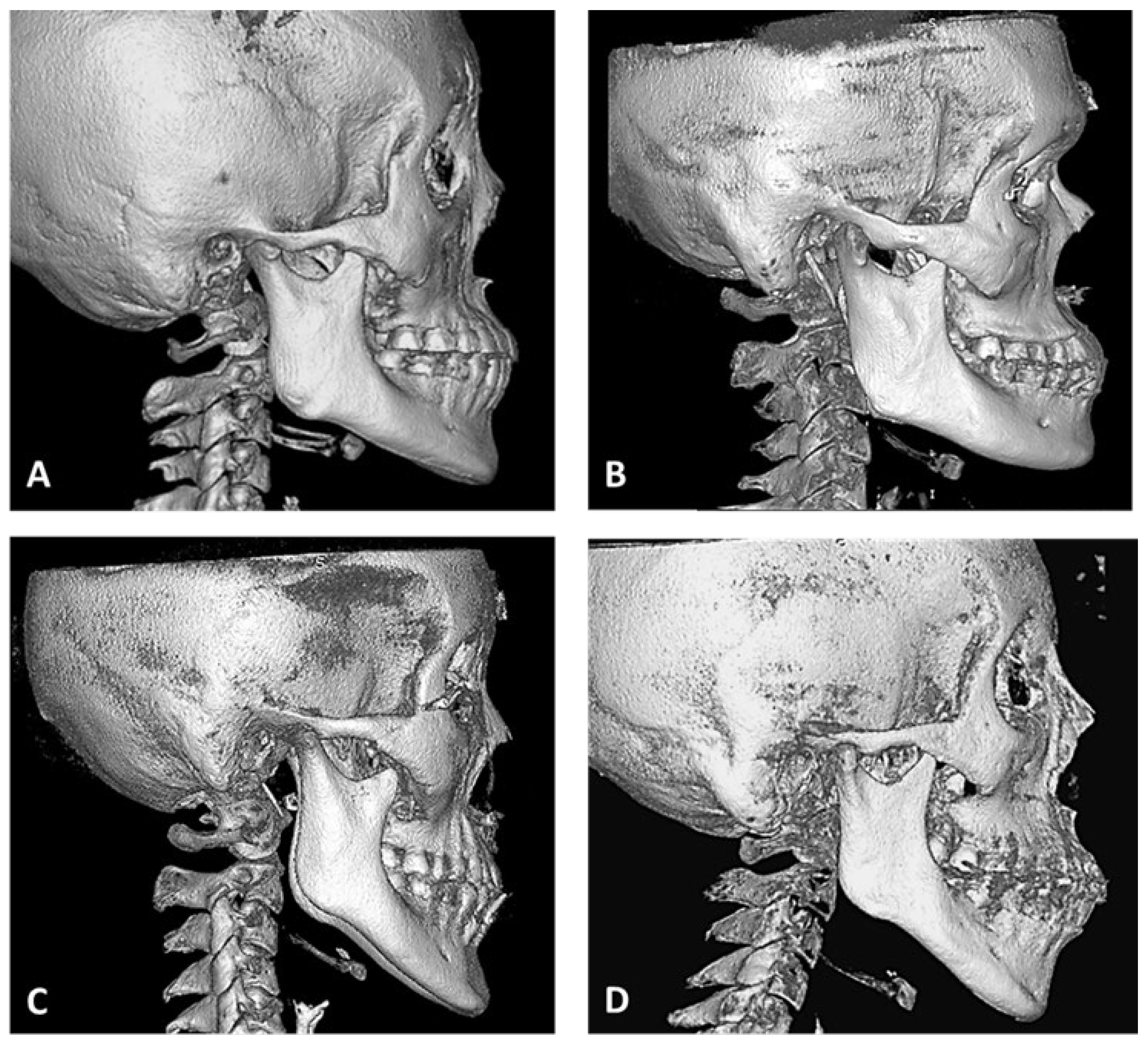
2.2. Image Investigation and Analysis
2.3. Statistical Analysis
3. Results
3.1. Morphological Parameters of Sex and Skeletal Patterns
3.2. Morphological Parameters on the Right and Left Sides for Each Sex
3.3. Morphological Parameters in the Bilateral and Unilateral Sides
3.4. Morphological Parameters on the Right and Left Sides for Skeletal Patterns
3.5. Morphological Parameters in the Bilateral and Unilateral Sides of the Skeletal Patterns
3.6. Distribution Correlation between the Lingula and Antilingula Shapes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Monnazzi, M.S.; Passeri, L.A.; Gabrielli, M.F.; Bolini, P.D.; de Carvalho, W.R.; da Costa Machado, H. Anatomic study of the mandibular foramen, lingula and antilingula in dry mandibles, and its statistical relationship between the true lingula and the antilingula. Int. J. Oral Maxillofac. Surg. 2012, 41, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Hou, Y.; Zhang, B.; Wang, R.; Yuan, H. CBCT study on the relationship between lingula and antilingula position in a Chinese Han population. Surg. Radiol. Anat. 2019, 41, 663–667. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.J.; Chen, Y.S.; Chen, P.H.; Chen, H.S.; Chen, C.M. The correlation between surgical reference points: Antilingula, lingula, and mandibular foramen. J. Stomatol. Oral Maxillofac Surg. 2021, 122, 535–538. [Google Scholar] [CrossRef]
- Hsu, K.J.; Tseng, Y.C.; Liang, S.W.; Hsiao, S.Y.; Chen, C.M. Dimension and Location of the Mandibular Lingula: Comparisons of Gender and Skeletal Patterns Using Cone-Beam Computed Tomography. BioMed Res. Int. 2020, 2020, 2571534. [Google Scholar] [CrossRef] [PubMed]
- Aziz, S.R.; Dorfman, B.J.; Ziccardi, V.B.; Janal, M. Accuracy of Using the Antilingula as a Sole Determinant of Vertical Ramus Osteotomy Position. J. Oral Maxillofac. Surg. 2007, 65, 859–862. [Google Scholar] [CrossRef]
- Jansisyanont, P.; Apinhasmit, W.; Chompoopong, S. Shape, height, and location of the lingula for sagittal ramus osteotomy in Thais. Clin. Anat. 2009, 22, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Akcay, H.; Kalabalık, F.; Tatar, B.; Ulu, M. Location of the mandibular lingula: Comparison of skeletal Class I and Class III patients in relation to ramus osteotomy using cone-beam computed tomography. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 504–508. [Google Scholar] [CrossRef]
- Pogrel, M.A.; Schmidt, B.L.; Ammar, A. The presence of the antilingula and its relationship to the true lingula. Br. J. Oral Maxillofac. Surg. 1995, 33, 235–238. [Google Scholar] [CrossRef]
- Tuli, A.; Choudhry, R.; Choudhry, S.; Raheja, S.; Agarwal, S. Variation in shape of the lingula in the adult human mandible. J. Anat. 2000, 197, 313–317. [Google Scholar] [CrossRef]
- Hogan, G.; Ellis, E., 3rd. The “Antilingula”—Fact or Fiction? J. Oral Maxillofac. Surg. 2006, 64, 1248–1254. [Google Scholar] [CrossRef]
- Lopes, P.T.; Pereira, G.A.; Santos, A.M. Morphological analysis of the lingula in dry mandibles of individuals on Southern Brazil. J. Morphol. Sci. 2010, 27, 136–138. [Google Scholar]
- Senel, B.; Ozkan, A.; Altug, H.A. Morphological evaluation of the mandibular lingula using cone-beam computed tomography. Folia Morphol. 2015, 74, 497–502. [Google Scholar] [CrossRef]
- Jung, Y.H.; Cho, B.H.; Hwang, J.J. Location and shape of the mandibular lingula: Comparison of skeletal class I and class III patients using panoramic radiography and cone-beam computed tomography. Imaging Sci. Dent. 2018, 48, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, S.Y.; Hsu, K.J.; Liang, S.W.; Tseng, Y.C.; Chen, C.M. The presence probability of mandibular lingla and antilingula. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 621–625. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D cephalometry on reduced FOV CBCT: Skeletal class assessment through AF-BF on Frankfurt plane—Validity and reliability through comparison with 2D measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef]
- Farronato, M.; Baselli, G.; Baldini, B.; Favia, G.; Tartaglia, G.M. 3D Cephalometric Normality Range: Auto Contractive Maps (ACM) Analysis in Selected Caucasian Skeletal Class I Age Groups. Bioengineering 2022, 9, 216. [Google Scholar] [CrossRef] [PubMed]
- Sekerci, A.E.; Sisman, Y. Cone-beam computed tomography analysis of the shape, height, and location of the mandibular lingula. Surg. Radiol. Anat. 2014, 36, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Kositbowornchai, S.; Siritapetawee, M.; Damrongrungruang, T.; Khongkankong, W.; Chatrchaiwiwatana, S.; Khamanarong, K.; Chanthaooplee, T. Shape of the lingula and its localization by panoramic radiograph versus dry mandibular measurement. Surg. Radiol. Anat. 2007, 29, 689–694. [Google Scholar] [CrossRef]
- Murlimanju, B.V.; Prabhu, L.V.; Pai, M.M.; Paul, M.T.; Saralaya, V.V.; Kumar, C.G. Morphological study of lingula of the mandibles in South Indian population. Morphologie 2012, 96, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Alves, N.; Deana, N.F. Morphological study of the lingula in adult human mandibles of Brazilians individuals and clinical implications. BioMed Res. Int. 2015, 2015, 873751. [Google Scholar] [CrossRef]
- Asdullah, M.; Ansari, A.A.; Khan, M.H.; Salati, N.A.; Khawja, K.J.; Sachdev, A.S. Morphological variations of lingula and prevalence of accessory mandibular foramina in mandibles: A study. Natl. J. Maxillofac. Surg. 2018, 9, 129–133. [Google Scholar] [PubMed]
- Ahn, B.S.; Oh, S.H.; Heo, C.K.; Kim, G.T.; Choi, Y.S.; Hwang, E.H. Cone-beam computed tomography of mandibular foramen and lingula for mandibular anesthesia. Imaging Sci. Dent. 2020, 50, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Stipo, A.R.; Bertoglio, B.; Biehler-Gomez, L.; Cattaneo, C.; De Angelis, D. Morphological analysis of lingula shape in a modern Italian cemeterial population: Clinical and forensic considerations. Leg. Med. 2022, 55, 102027. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.Y.; Hur, M.S. Anatomical review of the mandibular lingula for inferior alveolar nerve block. Folia Morphol. 2021, 80, 786–791. [Google Scholar] [CrossRef]
- Zhou, C.; Jeon, T.H.; Jun, S.H.; Kwon, J.J. Evaluation of mandibular lingula and foramen location using 3-dimensional mandible models reconstructed by cone-beam computed tomography. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 30. [Google Scholar] [CrossRef]
- Lupi, S.M.; Landini, J.; Olivieri, G.; Todaro, C.; Scribante, A.; Rodriguez y Baena, R. Correlation between the Mandibular Lingula Position and Some Anatomical Landmarks in Cone Beam CT. Healthcare 2021, 9, 1747. [Google Scholar] [CrossRef]
- Lima, F.J.C.; Oliveira Neto, O.B.; Barbosa, F.T.; Sousa-Rodrigues, C.F. Location, shape and anatomic relations of the mandibular foramen and the mandibular lingula: A contribution to surgical procedures in the ramus of the mandible. Oral Maxillofac. Surg. 2016, 20, 177–182. [Google Scholar] [CrossRef]
- Samanta, P.; Kharb, P. Morphological analysis of the lingula in dry adult human mandibles of north Indian population. J. Cranio-Maxillary Dis. 2012, 1, 7. [Google Scholar] [CrossRef]
- Woo, S.S.; Cho, J.Y.; Park, W.H.; Yoo, I.H.; Lee, Y.S.; Shim, K.S. A study of mandibular anatomy for orthognathic surgery in Koreans. J. Korean Assoc. Oral Maxillofac. Surg. 2002, 28, 126–131. [Google Scholar]
- Levine, B.; Topazian, D.S. The intraoral inverted-L double-oblique osteotomy of the mandibualr ramus: A new technique for the correction of mandibular prognathism. J. Oral Surg. 1976, 34, 522–525. [Google Scholar]
- Park, J.H.; Jung, H.D.; Kim, H.J.; Jung, Y.S. Anatomical study of the location of the antilingula, lingula, and mandibular foramen for vertical ramus osteotomy. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 15. [Google Scholar] [CrossRef] [PubMed]
- Reitzik, M.; Griffiths, R.R.; Mirels, H. Surgical anatomy of the ascending ramus of the mandible. Br. J. Oral Surg. 1976, 14, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, T.; Suzuki, T. The comparative anatomical study of the masseter of the mamma (III). Anat. Anz. 1969, 125, 363–387. [Google Scholar] [PubMed]
| Shape | Gender | Skeletal Pattern | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 180) | Male (n = 60) | Female (n = 120) | Chi-Square p Value | Class I (n = 60) | Class II (n = 60) | Class III (n= 60) | Chi-Square p Value | |||||||
| Lingula | ||||||||||||||
| Triangular | 44 | 24.4% | 13 | 7.2% | 31 | 17.2% | 0.366 | 17 | 9.4% | 10 | 5.6% | 17 | 9.4% | 0.232 |
| Truncated | 59 | 32.8% | 22 | 12.2% | 37 | 20.6% | 24 | 13.3% | 17 | 9.4% | 18 | 10.0% | ||
| Nodular | 68 | 37.8% | 20 | 11.1% | 48 | 26.7% | 16 | 8.9% | 29 | 16.1% | 23 | 12.8% | ||
| Assimilated | 9 | 5.0% | 5 | 2.8% | 4 | 2.2% | 3 | 1.7% | 4 | 2.2% | 2 | 1.1% | ||
| Total | 180 | 100.0% | 60 | 33.3% | 120 | 66.7% | 60 | 33.3% | 60 | 33.3% | 60 | 33.3% | ||
| Antilingula | ||||||||||||||
| Hill | 113 | 62.8% | 43 | 23.9% | 70 | 38.9% | 0.101 | 39 | 21.7% | 35 | 19.4% | 39 | 21.7% | 0.200 |
| Ridge | 8 | 4.4% | 4 | 2.2% | 4 | 2.2% | 5 | 2.8% | 1 | 0.6% | 2 | 1.1% | ||
| Plateau | 25 | 13.9% | 4 | 2.2% | 21 | 11.7% | 10 | 5.6% | 8 | 4.4% | 7 | 3.9% | ||
| Plain | 34 | 18.9% | 9 | 5.0% | 25 | 13.9% | 6 | 3.3% | 16 | 8.9% | 12 | 6.7% | ||
| Total | 180 | 100.0% | 60 | 33.3% | 120 | 66.7% | 60 | 33.3% | 60 | 33.3% | 60 | 33.3% | ||
| Shape | Total (n = 180) | McNemar– | Male (n = 60) | Female (n = 120) | |||
|---|---|---|---|---|---|---|---|
| Right | Left | Bowker Test | Right | Left | Right | Left | |
| Lingula | p < 0.001 * | ||||||
| Triangular | 27 | 17 | 8 | 5 | 19 | 12 | |
| Truncated | 19 | 40 | 9 | 13 | 10 | 27 | |
| Nodular | 37 | 31 | 9 | 11 | 28 | 20 | |
| Assimilated | 7 | 2 | 4 | 1 | 3 | 1 | |
| Total | 90 | 90 | 30 | 30 | 60 | 60 | |
| Antilingula | p = 0.047 * | ||||||
| Hill | 65 | 48 | 25 | 18 | 40 | 30 | |
| Ridge | 5 | 17 | 1 | 3 | 4 | 14 | |
| Plateau | 9 | 2 | 2 | 2 | 7 | 0 | |
| Plain | 11 | 23 | 2 | 7 | 9 | 16 | |
| Total | 90 | 90 | 30 | 30 | 60 | 60 | |
| Shape | Total (n = 180) | Male (n = 60) | Female (n = 120) | |||
|---|---|---|---|---|---|---|
| Bilateral | Unilateral | Bilateral | Unilateral | Bilateral | Unilateral | |
| Lingula | ||||||
| Triangular | 24 | 20 | 6 | 7 | 18 | 13 |
| Truncated | 28 | 31 | 14 | 8 | 14 | 23 |
| Nodular | 40 | 28 | 12 | 8 | 28 | 20 |
| Assimilated | 2 | 7 | 0 | 5 | 2 | 2 |
| Total | 94 | 86 | 32 | 28 | 62 | 58 |
| Antilingula | ||||||
| Hill | 76 | 37 | 30 | 13 | 46 | 24 |
| Ridge | 2 | 6 | 2 | 2 | 0 | 4 |
| Plateau | 4 | 43 | 0 | 4 | 4 | 17 |
| Plain | 10 | 45 | 0 | 9 | 10 | 15 |
| Total | 92 | 88 | 32 | 28 | 60 | 60 |
| Shape | Class I (n = 60) | Class II (n = 60) | Class III (n = 60) | |||
|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |
| Lingula | ||||||
| Triangular | 8 | 7 | 8 | 2 | 9 | 8 |
| Truncated | 9 | 17 | 5 | 12 | 7 | 11 |
| Nodular | 9 | 5 | 14 | 15 | 12 | 11 |
| Assimilated | 4 | 1 | 3 | 1 | 2 | 0 |
| Total | 30 | 30 | 30 | 30 | 30 | 30 |
| Antilingula | ||||||
| Hill | 21 | 18 | 21 | 14 | 23 | 16 |
| Ridge | 4 | 1 | 0 | 1 | 1 | 1 |
| Plateau | 4 | 6 | 3 | 5 | 2 | 5 |
| Plain | 1 | 5 | 6 | 10 | 4 | 8 |
| Total | 30 | 30 | 30 | 30 | 30 | 30 |
| Shape | Class I (n = 60) | Class II (n = 60) | Class III (n = 60) | |||
|---|---|---|---|---|---|---|
| Bilateral | Unilateral | Bilateral | Unilateral | Bilateral | Unilateral | |
| Lingula | ||||||
| Triangular | 8 | 9 | 4 | 6 | 12 | 5 |
| Truncated | 14 | 10 | 8 | 9 | 6 | 12 |
| Nodular | 6 | 10 | 24 | 5 | 10 | 13 |
| Assimilated | 0 | 3 | 2 | 2 | 0 | 2 |
| Total | 28 | 32 | 38 | 22 | 28 | 32 |
| Antilingula | ||||||
| Hill | 30 | 9 | 24 | 11 | 22 | 17 |
| Ridge | 2 | 3 | 0 | 1 | 0 | 2 |
| Plateau | 2 | 8 | 2 | 6 | 0 | 7 |
| Plain | 2 | 4 | 8 | 8 | 0 | 12 |
| Total | 36 | 24 | 34 | 26 | 22 | 38 |
| Lingula (n) | Chi-Square | |||||
|---|---|---|---|---|---|---|
| Shape | Triangular | Truncated | Nodular | Assimilated | Total | p Value |
| Antilingula (n) | ||||||
| Hill | 22 | 39 | 45 | 7 | 113 | 0.197 |
| Ridge | 4 | 1 | 3 | 0 | 8 | |
| Plateau | 10 | 10 | 5 | 0 | 25 | |
| lain | 8 | 9 | 15 | 2 | 34 | |
| Total | 44 | 59 | 68 | 9 | 180 | |
| Author | Material | Patients (Sides) | Age (years) | Shape of Lingula (%) | |||
|---|---|---|---|---|---|---|---|
| Year, Country | Female (F)/Male (M) | Mean, Range | Triangular | Truncated | Nodular | Assimilated | |
| Tuli et al. [9] | Dry | n = 165 (330) | NA | 68.5% | 15.8% | 10.9% | 4.8% |
| 2000, India | mandible | 34 F/131 M | |||||
| Kositbowornchai et al. [18] | Dry | n = 72 (144) | 27–87 years | 16.66% | 47.22% | 22.92% | 13.19% |
| 2007, Thailand | mandible | 20 F/52 M | |||||
| Jansisyanont et al. [6] | Dry | n = 92 (184) | 42.4 | 29.9% | 46.2% | 19.6% | 4.3% |
| 2009, Thailand | mandible | 34 F/58 M | 18–83 | ||||
| Murlimanju et al. [19] | Dry | n = 67 (134) | Adult | 29.9% | 27.6% | 29.9% | 12.6% |
| 2012, India | mandible | 30 F/37 M | |||||
| Sekerci and Sisman [17] | CBCT | n = 412 (824) | Adult | 14.1% | 32.0% | 51.2% | 2.7% |
| 2014, Turkey | 199 F/213 M | ||||||
| Senel et al. [12] | CBCT | n = 63 (126) | 46 | 22.2% | 19.0% | 32.5% | 26.2% |
| 2015, Turkey | 28 F/35 M | 25–70 | |||||
| Alves and Deana [20] | Dry | n = 132 (253) | Adult | 23.3% | 49.0% | 26.5% | 1.2% |
| 2016, Brazil | mandible | ||||||
| Asdullah et al. [21] | Dry | n = 50 (100) | Adult | 42.0% | 32.0% | 20.0% | 6.0% |
| 2018, India | mandible | 25 F/25 M | |||||
| Jung et al. [13] | CBCT | n = 347 (694) | 27 | 14.3% | 29.3% | 54.0% | 2.4% |
| 2018, Korea | 166 F/181 M | 19–50 | |||||
| Akcay et al. [7] | CBCT | n = 60 (120) | 18–37 | 20.0% | 21.7% | 45.0% | 13.3% |
| 2019, Turkey | 30 F/30 M | ||||||
| Ahn et al. [22] | CBCT | n = 30 (58) | NA | 31.0% | 25.9% | 32.8% | 10.3% |
| 2020, Korea | |||||||
| Stipo et al. [23] | Dry | n = 235 (453) | 69.4 | 10.8% | 38.6% | 26.3% | 4.0% * |
| 2022, Italy | mandible | 114 F/121 M | 20–101 | ||||
| Present study | CBCT | n = 90 (180) | 25.3 | 24.4% | 32.8% | 37.8% | 5.0% |
| 2023, Taiwan | 60 F/30 M | 16–46 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-M.; Lee, H.-N.; Liang, S.-W.; Hsu, K.-J. Morphological Study of the Mandibular Lingula and Antilingula by Cone-Beam Computed Tomography. Bioengineering 2023, 10, 170. https://doi.org/10.3390/bioengineering10020170
Chen C-M, Lee H-N, Liang S-W, Hsu K-J. Morphological Study of the Mandibular Lingula and Antilingula by Cone-Beam Computed Tomography. Bioengineering. 2023; 10(2):170. https://doi.org/10.3390/bioengineering10020170
Chicago/Turabian StyleChen, Chun-Ming, Hui-Na Lee, Shih-Wei Liang, and Kun-Jung Hsu. 2023. "Morphological Study of the Mandibular Lingula and Antilingula by Cone-Beam Computed Tomography" Bioengineering 10, no. 2: 170. https://doi.org/10.3390/bioengineering10020170
APA StyleChen, C.-M., Lee, H.-N., Liang, S.-W., & Hsu, K.-J. (2023). Morphological Study of the Mandibular Lingula and Antilingula by Cone-Beam Computed Tomography. Bioengineering, 10(2), 170. https://doi.org/10.3390/bioengineering10020170