A Study on the Biofilm Removal Efficacy of a Bioelectric Toothbrush
Abstract
:1. Introduction
2. Materials and Methods
2.1. Tested Toothbrushes and Design of BE Toothbrush
2.2. Development of Brushing Simulator
2.3. Plaque Culture
2.4. Experiment of Plaque Removal
- Only saline was applied.
- A toothpaste slurry (toothpaste–saline at a ratio of 1:3) was applied.
2.5. Statistical Analysis
3. Results
3.1. Experiment Using Only Saline
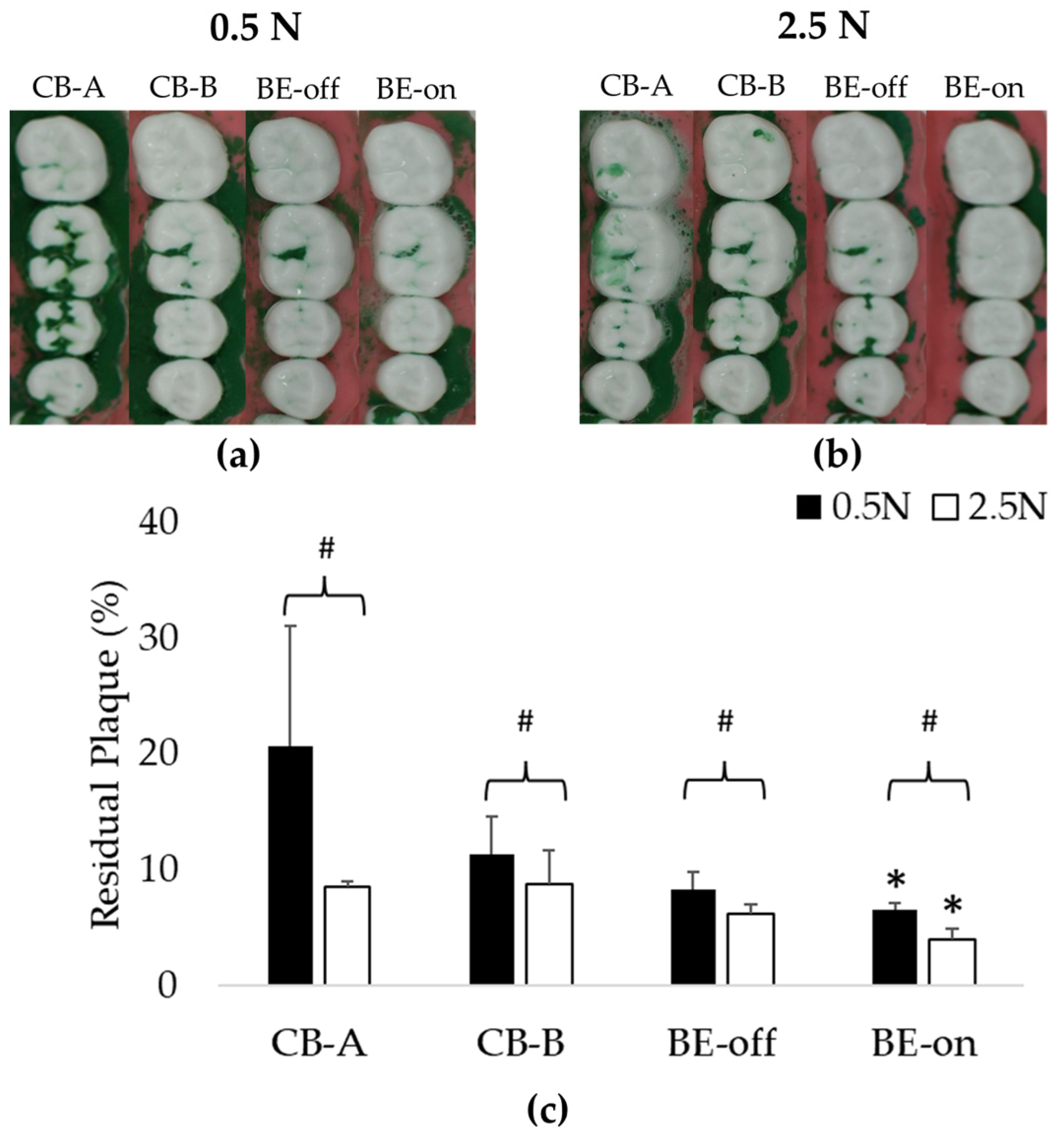
3.2. Experiment Appling a Toothpaste Slurry
3.3. Comparison of Residual Plaque in Applied Saline with BE versus Toothpaste Slurry without BE
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lorenzo-Pouso, A.I.; Pérez-Sayáns, M.; Bravo, S.B.; López-Jornet, P.; García-Vence, M.; Alonso-Sampedro, M.; Carballo, J.; García-García, A. Protein-Based Salivary Profiles as Novel Biomarkers for Oral Diseases. Dis. Mrk. 2018, 2018, 6141845. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/health-topics/oral-health#tab=tab_1 (accessed on 8 September 2023).
- Allaker, R.P.; Douglas, C.I. Novel anti-microbial therapies for dental plaque-related diseases. Int. J. Antimicrob. Agents 2009, 33, 8–13. [Google Scholar] [CrossRef]
- Marsh, P.D. Dental plaque: Biological significance of a biofilm and community life-style. J. Clin Periodontol. 2005, 32, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Abebe, G.M. Oral Biofilm and Its Impact on Oral Health, Psychological and Social Interaction. Int. J. Oral Dent. Health 2021, 7, 127. [Google Scholar]
- Löe, H.; Theilade, E.; Jensen, S.B. Experimental Gingivitis in Man. J. Periodontol. 1965, 36, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Lovdal, A.; Arno, A.; Waerhaug, J. Incidence of clinical manifestations of periodontal disease in light of oral hygiene and calculus formation. J. Amer. Dent. Assoc. 1958, 56, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.W.; Lee, J.; Lee, T.H. Bioelectric effect utilized a healthcare device for effective management of dental biofilms and gingivitis. Med. Eng. Phys. 2022, 104, 103804. [Google Scholar] [CrossRef]
- Alhadainy, H.A.; Keefe, T.; Abdel-Karim, A.H.; Abdulrab, S.; Halboub, E. Association between dental diseases and history of stroke in the United States. Clin. Exp. Dent. Res. 2021, 7, 845–851. [Google Scholar] [CrossRef]
- Albert, D.A.; Ward, A.; Allweiss, P. Diabetes and oral disease: Implications for health professionals. Ann. N. Y. Acad. Sci. 2012, 1255, 1–15. [Google Scholar] [CrossRef]
- Kotronia, E.; Brown, H.; Papacosta, A.O.; Lennon, L.T.; Weyant, R.J.; Whincup, P.H.; Wannamethee, S.G.; Ramsay, S.E. Oral health and all-cause, cardiovascular disease, and respiratory mortality in older people in the UK and USA. Sci. Rep. 2021, 11, 16452. [Google Scholar] [CrossRef]
- Ming, Y.; Hsu, S.W.; Yen, Y.; Lan, S.J. Association of oral health–related quality of life and Alzheimer disease: A systematic review. J. Prosthet. Dent. 2020, 124, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Sälzer, S.; Slot, D.E.; Van der Weijden, F.A.; Dörfer, C.E. Efficacy of inter-dental mechanical plaque control in managing gingivitis—A meta-review. J. Clin. Periodontol. 2015, 42, 92–105. [Google Scholar] [CrossRef] [PubMed]
- Westfelt, E. Rationale of mechanical plaque control. J. Clin. Periodontol. 1996, 23, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Jepsen, S. Role of m toothbrushes in effective plaque control: Advantages and limitations. In Proceedings of European Workship on Mechanical Plaque Control, 1st ed.; Lang, N.P., Attstrom, R., Love, H., Eds.; Quintessence Publishing: Batavia, IL, USA; pp. 121–137.
- Hara, A.T.; Turssi, C.P. Baking soda as an abrasive in toothpastes: Mechanism of action and safety and effectiveness considerations. J. Am. Dent. Assoc. 2017, 148, 27–33. [Google Scholar] [CrossRef]
- Stovell, A.G.; Newton, B.M.; Lynch, R.J.M. Important considerations in the development of toothpaste formulations for children. Int. Dent. J. 2013, 63, 57–63. [Google Scholar] [CrossRef]
- Ullah, R.; Zafar, M.S.; Shahani, N. Potential fluoride toxicity from oral medicaments: A review. Iran. J. Basic Med. Sci. 2017, 20, 841–848. [Google Scholar]
- Mohideen, H.; Dahiya, D.S.; Parsons, D.; Hussain, H.; Ahmed, R.S. Skeletal Fluorosis: A Case of Inhalant Abuse Leading to a Diagnosis of Colon Cancer. J. Investig. Med. High Impact Case Rep. 2022, 10, 23247096221084919. [Google Scholar] [CrossRef]
- Pashley, D.H.; Allison, N.B.; Easmann, R.P.; McKinney, R.V.; Horner, J.A.; Whitford, G.M. The effects of fluoride on the gastric mucosa of the rat. J. Oral Path. Med. 1984, 13, 535–545. [Google Scholar] [CrossRef]
- Wang, Y.; Jiang, L.; Zhao, Y. Awareness of the Benefits and Risks Related to Using Fluoridated Toothpaste Among Doctors: A Population-Based Study. Med. Sci. Monit 2019, 25, 6397–6404. [Google Scholar] [CrossRef]
- Basch, C.H.; Rajan, S. Marketing strategies and warning labels on children’s toothpaste. J. Am. Dent. Hyg. Assoc. 2014, 88, 316–319. [Google Scholar]
- Buzalaf, M.A.; Levy, S.M. Fluoride intake of children:considerations for dental caries and dental fluorosis. Monogr. Oral. Sci. 2011, 22, 1–19. [Google Scholar] [PubMed]
- Hathroubi, S.; Mekni, M.A.; Domenico, P.; Nguyen, D.; Jacques, M. Biofilms: Microbial shelters against antibiotics. Microb. Drug Resist. 2017, 23, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Costerton, J.W.; Ellis, B.; Lam, K.; Johnson, F.; Khoury, A.E. Mechanism of electrical enhancement of efficacy of antibiotics in killing biofilm bacteria. Antimicrob. Agents Chemother. 1994, 38, 2803–2809. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, Y.-G.; Um, H.-S.; Lee, S.Y.; Lee, J.-K.; Chang, B.-S. Antimicrobial effect of toothbrush with light emitting diode on dental biofilm attached to zirconia surface: An in vitro study. J. Dent. Rehabil. Appl. Sci. 2019, 35, 160–169. [Google Scholar] [CrossRef]
- Bagchi, D.; Rathnam, V.S.; Lemmens, P.; Banerjee, I.; Pal, S.K. NIR-light-active ZnO-based nanohybrids for bacterial biofilm treatment. ACS Omega 2018, 3, 10877–10885. [Google Scholar] [CrossRef]
- Pérez-Pérez, L.; García-Gavín, J.; Gilaberte, Y. Daylight-mediated photodynamic therapy in Spain: Advantages and disadvantages. Actas Dermosifiliogr. 2014, 105, 663–674. [Google Scholar] [CrossRef]
- Costerton, J.W.; Stewart, P.S.; Greenberg, E.P. Bacterial biofilms: A common cause of persistent infections. Science 1999, 284, 1318–1322. [Google Scholar] [CrossRef]
- Daubert, D.M.; Weinstein, B.F. Biofilm as a risk factor in implant treatment. Periodontology 2000 2019, 81, 29–40. [Google Scholar] [CrossRef]
- Kim, Y.W.; Subramanian, S.; Gerasopoulos, K.; Ben-Yoav, H.; Wu, H.C.; Quan, D.; Carter, K.; Meyer, M.T.; Bentley, W.E.; Ghodssi, R. Effect of Electrical Energy on the Efficacy of Biofilm Treatment Using the Bioelectric Effect. NPJ Biofilms Microbiomes 2015, 1, 15016. [Google Scholar] [CrossRef]
- Kim, Y.W.; Meyer, M.T.; Berkovich, A.; Subramanian, S.; Iliadis, A.A.; Bentley, W.E.; Ghodssi, R. A surface acoustic wave biofilm sensor integrated with a treatment method based on the bioelectric effect. Sens. Actuators A Phys. 2016, 238, 140–149. [Google Scholar] [CrossRef]
- Pareilleux, A.; Sicard, N. Lethal effects of electric current on Escherichia coli. Appl. Microbiol. 1970, 19, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Blenkinsopp, S.A.; Khoury, A.; Costerton, J. Electrical enhancement of biocide efficacy against Pseudomonas aeruginosa biofilms. Appl. Environ. Microbiol. 1992, 58, 3770–3773. [Google Scholar] [CrossRef] [PubMed]
- Caubet, R.; Pedarros-Caubet, F.; Chu, M.; Freye, E.; de Belém Rodrigues, M.; Moreau, J.M.; Ellison, W.J. A radio frequency electric current enhances antibiotic efficacy against bacterial biofilms. Antimicrob. Agents Chemother. 2004, 48, 4662–4664. [Google Scholar] [CrossRef] [PubMed]
- del Pozo, J.L.; Rouse, M.S.; Mandrekar, J.N.; Steckelberg, J.M.; Patel, R. The electricidal effect: Reduction of staphylococcus and pseudomonas biofilms by prolonged exposure to low-intensity electrical current. Antimicrob. Agents Chemother. 2009, 53, 41–45. [Google Scholar] [CrossRef]
- Stoodley, P.; DeBeer, D.; Lappin-Scott, H.M. Influence of Electric Fields and pH on Biofilm Structure as Related to the Bioelectric Effect. Antimicrob. Agents Chemother. 1997, 41, 1876–1879. [Google Scholar] [CrossRef]
- Park, H.M.; Chang, K.H.; Moon, S.H.; Park, B.J.; Yoo, S.K.; Nam, K.C. In vitro delivery efficiencies of nebulizers for different breathing patterns. Biomed. Eng. OnLine 2021, 20, 59. [Google Scholar] [CrossRef]
- Wisotzki, M.; Mair, A.; Schlett, P.; Lindner, B.; Oberhardt, M.; Bernhard, S. In Vitro Major Arterial Cardiovascular Simulator to Generate Benchmark Data Sets for In Silico Model Validation. Data 2022, 7, 145. [Google Scholar] [CrossRef]
- Szalma, J.; Lovasz, B.V.; Vajta, L.; Soos, B.; Lempel, E.; Mohlhenrich, S.C. The influence of the chosen in vitro bone simulation model on intraosseous temperatures and drilling times. Sci. Rep. 2019, 9, 11817. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, S.-H.; Han, J.-S.; Yeo, I.-S.L.; Yoon, H.-I. Optical and Surface Properties of Monolithic Zirconia after Simulated Toothbrushing. Materials 2019, 12, 1158. [Google Scholar] [CrossRef]
- Bizhang, M.; Schmidt, I.; Chun, Y.P.; Arnold, W.H.; Zimmer, S. Toothbrush abrasivity in a long-term simulation on human dentin depends on brushing mode and bristle arrangement. PLoS ONE 2017, 12, e0172060. [Google Scholar] [CrossRef]
- Ledder, R.G.; Latimer, J.; Forbes, S.; Penney, J.L.; Sreenivasan, P.K.; Mcbain, A.J. Visualization and quantification of the oral hygiene effects of brushing, dentifrice use, and brush wear using a tooth brushing stimulator. Front. Public Health 2019, 7, 91. [Google Scholar] [CrossRef] [PubMed]
- Lang, T.; Staufer, S.; Jennes, B.; Gaengler, P. Clinical validation of robot simulation of toothbrushing-comparative plaque removal efficacy. BMC Oral Health 2014, 14, 82. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.W.; Lee, J.; Han, S.K.; Koo, B.-S.; Park, T.; Park, H.M.; Lee, B. A Non-Electrolysis Bioelectric Effect for Gingivitis and Hygiene Contamination Biofilm Removal. Appl. Microbiol. 2023, 3, 675–686. [Google Scholar] [CrossRef]
- Kim, Y.-J.; Lee, S.G.; Go, S.J.; An, S.; Kim, Y.E.; Kim, Y.I.; Hyun, K.-Y.; Cho, D.S.; Choi, G.E. Anti-inflammatory Effects of Low-frequency Stimulator using Superposition of Alternating Microcurrent Wave in the Animal Models. Biomed. Sci. Lett. 2021, 27, 99–104. [Google Scholar] [CrossRef]
- Hao, L.; Li, C.; Wang, L.; Bai, B.; Zhao, Y.; Luo, C. Design and Fabrication of a High-Temperature SOI Pressure Sensor with Optimized Crossbeam Membrane. Micromachines 2023, 14, 1045. [Google Scholar] [CrossRef]
- ISO TR 14569-1; Dental Materials-Guidance on Testing of Wear Resistance. Part 1: Wear by Tooth Brushing; International Organization for Standardization: Geneva, Switzerland, 2007.
- van Leeuwen, M.P.C.; van der Weijden, F.A.; Slot, D.E.; Rosema, M.A.M. Toothbrush wear in relation to toothbrushing effectiveness. Int. J. Dent. Hyg. 2019, 17, 77–84. [Google Scholar] [CrossRef]
- García-Godoy, F.; Villalta, P.; Bartizek, R.D.; Barker, M.L.; Biesbrock, A.R. Tooth whitening effects of an experimental power whitening toothbrush relative to an 8.7% hydrogen peroxide paint-on gel control. Am. J. Dent. 2004, 17, 25A–30A. [Google Scholar]
- Addy, M.; Jenkins, S.; Newcombe, R. The effect of triclosan, stannous fluoride and chlorhexidine products on: (I) Plaque regrowth over a 4-day period. J. Clin. Periodontol. 1990, 17, 693–697. [Google Scholar] [CrossRef]
- Binney, A.; Addy, M.; McKeown, S.; Everatt, L. The effect of a commercially available triclosan-containing toothpaste compared to a sodium-fluoride-containing toothpaste and a chlorhexidine rinse on 4-day plaque regrowth. J. Clin. Periodontol. 1995, 22, 693–697. [Google Scholar] [CrossRef]
- Sripriya, N.; and Shaik Hyder Ali, K.H. A comparative study of the efficacy of four different bristle designs of tooth brushes in plaque removal. J. Indian Soc. Pedod. Prev. Dent. 2007, 25, 76–81. [Google Scholar] [CrossRef]
- Pujarern, P.; Rodanant, P.; Warinsiriruk, E.; Rattanasuwan, K. Evaluation of the optimum brushing force on dental plaque removal: An in vitro study. M. Dent. J. 2021, 41, 75–82. [Google Scholar]
- Mankodi, S.; Berkowitz, H.; Durbin, K.; Nelson, B. Evaluation of the effects of brushing on the removal of dental plaque. J. Clin. Dent. 1998, 9, 57–60. [Google Scholar] [PubMed]
- Ozdemir, A.; Mas, M.R.; Sahin, S.; Sağlamkaya, U.; Ateşkan, U. Detection of Helicobacter pylori colonization in dental plaques and tongue scrapings of patients with chronic gastritis. Quintessence Int. 2001, 32, 131–134. [Google Scholar] [PubMed]
- Pérez-Serrano, R.M.; Domínguez-Pérez, R.A.; Ayala-Herrera, J.L.; Luna-Jaramillo, A.E.; De Larrea, G.Z.-L.; Solís-Sainz, J.C.; García-Solís, P.; Loyola-Rodríguez, J.P. Dental plaque microbiota of pet owners and their dogs as a shared source and reservoir of antimicrobial resistance genes. J. Glob. Antimicrob. Resist. 2020, 21, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Essalat, M.; Morrison, D.; Kak, S.; Chang, E.J.; Penso, I.R.; Kulchar, R.J.; Padilla, O.H.M.; Shetty, V. A Naturalistic Study of Brushing Patterns Using Powered Toothbrushes. PLoS ONE 2022, 17, e0263638. [Google Scholar] [CrossRef]
- Collins, L.M.; Dawes, C. The surface area of the adult human mouth and thickness of the salivary film covering the teeth and oral mucosa. J. Dent. Res. 1987, 66, 1300–1302. [Google Scholar] [CrossRef]








| Abbreviations | Toothbrushes | BE Applied |
|---|---|---|
| CB-A | 2080 Original Toothbrush, Aekyung Co., Ltd., Seoul, Republic of Korea | X |
| CB-B | Oral-B Ultra-fine, Oral-B Laboratories, Boston, MA, USA | X |
| BE-Off | Non-bioelectric effect | X |
| BE-On | 0.7 V amplitude of 10 MHz with 0.7 V offset | O |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.M.; Ryu, S.; Jo, E.; Yoo, S.K.; Kim, Y.W. A Study on the Biofilm Removal Efficacy of a Bioelectric Toothbrush. Bioengineering 2023, 10, 1184. https://doi.org/10.3390/bioengineering10101184
Park HM, Ryu S, Jo E, Yoo SK, Kim YW. A Study on the Biofilm Removal Efficacy of a Bioelectric Toothbrush. Bioengineering. 2023; 10(10):1184. https://doi.org/10.3390/bioengineering10101184
Chicago/Turabian StylePark, Hyun Mok, Seungjae Ryu, Eunah Jo, Sun Kook Yoo, and Young Wook Kim. 2023. "A Study on the Biofilm Removal Efficacy of a Bioelectric Toothbrush" Bioengineering 10, no. 10: 1184. https://doi.org/10.3390/bioengineering10101184
APA StylePark, H. M., Ryu, S., Jo, E., Yoo, S. K., & Kim, Y. W. (2023). A Study on the Biofilm Removal Efficacy of a Bioelectric Toothbrush. Bioengineering, 10(10), 1184. https://doi.org/10.3390/bioengineering10101184







