Impact of Palliative Care Services on Treatment and Resource Utilization for Hepatorenal Syndrome in the United States
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
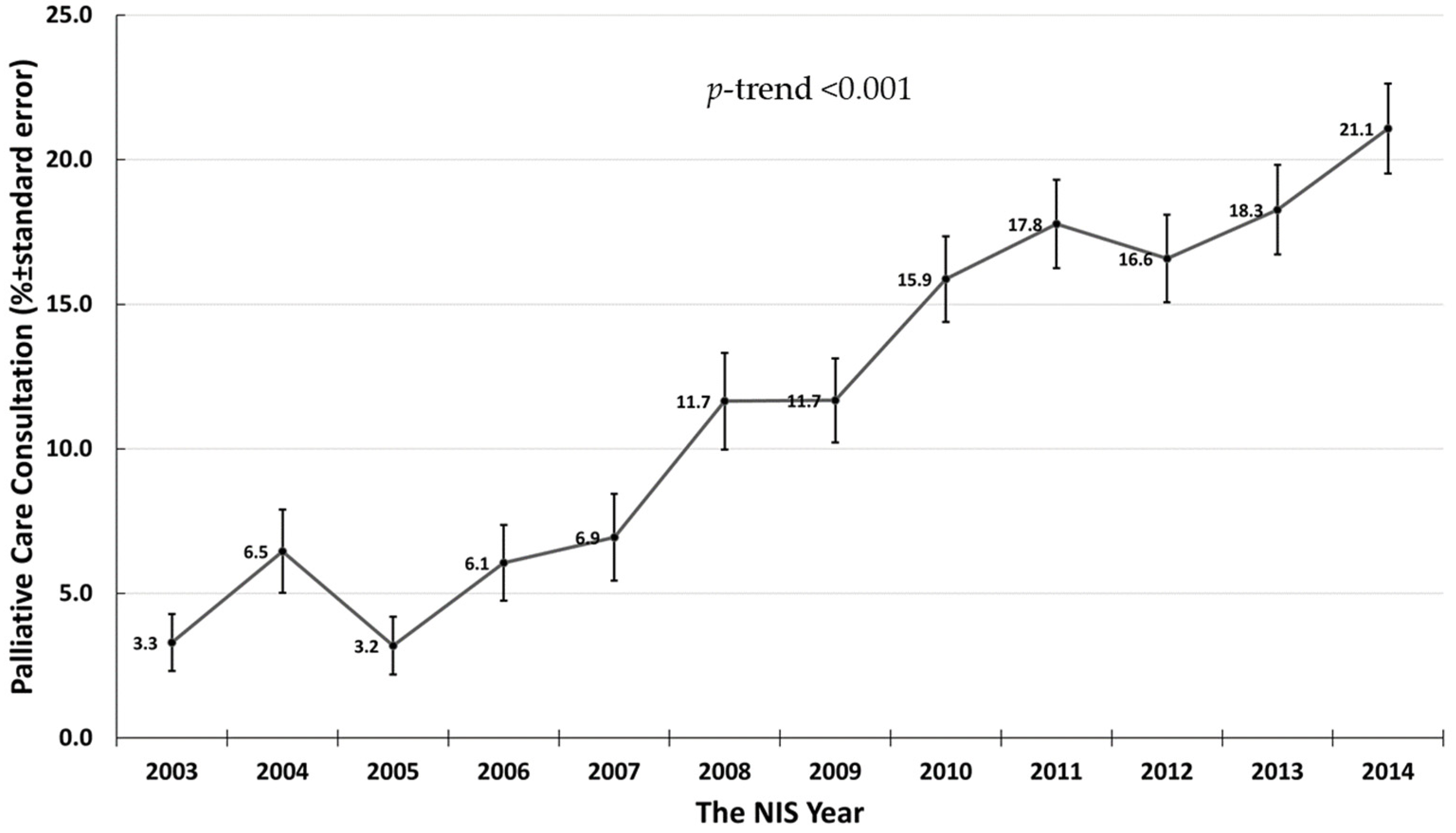
3.1. The Rate of and Trend in Palliative Care Service Use in Hospital Admissions for Hepatorenal Syndrome
3.2. The Predictors of Inpatient Palliative Care Service Use in Hospital Admissions for Hepatorenal Syndrome
3.3. The Impact of Inpatient Palliative Care Service Use on Treatments and Resource Use in Hospital Admissions for Hepatorenal Syndrome
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Low, G.; Alexander, G.J.; Lomas, D.J. Hepatorenal syndrome: Aetiology, diagnosis, and treatment. Gastroenterol. Res. Pract. 2015, 2015, 207012. [Google Scholar] [CrossRef] [PubMed]
- Salerno, F.; Cazzaniga, M.; Merli, M.; Spinzi, G.; Saibeni, S.; Salmi, A.; Fagiuoli, S.; Spadaccini, A.; Trotta, E.; Laffi, G.; et al. Diagnosis, treatment and survival of patients with hepatorenal syndrome: A survey on daily medical practice. J. Hepatol. 2011, 55, 1241–1248. [Google Scholar] [CrossRef] [PubMed]
- Martin-Llahi, M.; Guevara, M.; Torre, A.; Fagundes, C.; Restuccia, T.; Gilabert, R.; Sola, E.; Pereira, G.; Marinelli, M.; Pavesi, M.; et al. Prognostic importance of the cause of renal failure in patients with cirrhosis. Gastroenterology 2011, 140, 488–496.e4. [Google Scholar] [CrossRef] [PubMed]
- Rey, R.M.; Delgado, A.F.; De Zubiria, A.; Pinto, R.; De la Hoz-Valle, J.A.; Perez-Riveros, E.D.; Ardila, G.; Sierra-Arango, F. Prevalence and short-term outcome of hepatorenal syndrome: A 9-year experience in a high-complexity hospital in Colombia. PLoS ONE 2020, 15, e0239834. [Google Scholar] [CrossRef] [PubMed]
- Utako, P.; Emyoo, T.; Anothaisintawee, T.; Yamashiki, N.; Thakkinstian, A.; Sobhonslidsuk, A. Clinical Outcomes after Liver Transplantation for Hepatorenal Syndrome: A Systematic Review and Meta-Analysis. BioMed Res. Int. 2018, 2018, 5362810. [Google Scholar] [CrossRef] [PubMed]
- Gines, A.; Escorsell, A.; Gines, P.; Salo, J.; Jimenez, W.; Inglada, L.; Navasa, M.; Claria, J.; Rimola, A.; Arroyo, V.; et al. Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites. Gastroenterology 1993, 105, 229–236. [Google Scholar] [CrossRef]
- Bianchi, G.; Marchesini, G.; Nicolino, F.; Graziani, R.; Sgarbi, D.; Loguercio, C.; Abbiati, R.; Zoli, M. Psychological status and depression in patients with liver cirrhosis. Dig. Liver Dis. 2005, 37, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Verma, M.; Tapper, E.B.; Singal, A.G.; Navarro, V. Nonhospice Palliative Care Within the Treatment of End-Stage Liver Disease. Hepatology 2020, 71, 2149–2159. [Google Scholar] [CrossRef] [PubMed]
- Barnes, A.; Woodman, R.J.; Kleinig, P.; Briffa, M.; To, T.; Wigg, A.J. Early palliative care referral in patients with end stage liver disease is associated with reduced resource utilisation. J. Gastroenterol. Hepatol. 2019. [Google Scholar] [CrossRef]
- Patel, A.A.; Walling, A.M.; Ricks-Oddie, J.; May, F.P.; Saab, S.; Wenger, N. Palliative Care and Health Care Utilization for Patients With End-Stage Liver Disease at the End of Life. Clin. Gastroenterol Hepatol 2017, 15, 1612–1619.e4. [Google Scholar] [CrossRef] [PubMed]
- Holden, J.H.; Shamseddeen, H.; Johnson, A.W.; Byriel, B.; Subramoney, K.; Cheng, Y.W.; Saito, A.; Ghabril, M.; Chalasani, N.; Sachs, G.A.; et al. Palliative Care and Hospice Referrals in Patients with Decompensated Cirrhosis: What Factors Are Important? J. Palliat. Med. 2020, 23, 1066–1075. [Google Scholar] [CrossRef] [PubMed]
- Feder, S.L.; Redeker, N.S.; Jeon, S.; Schulman-Green, D.; Womack, J.A.; Tate, J.P.; Bedimo, R.J.; Budoff, M.J.; Butt, A.A.; Crothers, K.; et al. Validation of the ICD-9 Diagnostic Code for Palliative Care in Patients Hospitalized With Heart Failure Within the Veterans Health Administration. Am. J. Hosp. Palliat. Care 2018, 35, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Hua, M.; Li, G.; Clancy, C.; Morrison, R.S.; Wunsch, H. Validation of the V66.7 Code for Palliative Care Consultation in a Single Academic Medical Center. J. Palliat. Med. 2017, 20, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Mulvey, C.L.; Smith, T.J.; Gourin, C.G. Use of inpatient palliative care services in patients with metastatic incurable head and neck cancer. Head Neck 2016, 38, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Martin, P.; DiMartini, A.; Feng, S.; Brown, R., Jr.; Fallon, M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology 2014, 59, 1144–1165. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.; Jalan, R.; Gines, P.; Pavesi, M.; Angeli, P.; Cordoba, J.; Durand, F.; Gustot, T.; Saliba, F.; Domenicali, M.; et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013, 144, 1426–1437. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.; Phillips, J. End of life care-the importance of culture and ethnicity. Aust. Fam. Phys. 2010, 39, 210–213. [Google Scholar]
- Ekser, B.; Contreras, A.G.; Andraus, W.; Taner, T. Current status of combined liver-kidney transplantation. Int. J. Surg. 2020, 82S, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Rush, B.; Fruhstofer, C.; Walley, K.R.; Celi, L.A.; Brahmania, M. Palliative medicine and hospital readmissions in end-stage liver disease. BMJ Support. Palliat. Care 2019. [Google Scholar] [CrossRef] [PubMed]
- Kimbell, B.; Murray, S.A.; Byrne, H.; Baird, A.; Hayes, P.C.; MacGilchrist, A.; Finucane, A.; Brookes Young, P.; O’Carroll, R.E.; Weir, C.J.; et al. Palliative care for people with advanced liver disease: A feasibility trial of a supportive care liver nurse specialist. Palliat. Med. 2018, 32, 919–929. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristics | Total | Palliative Care | No Palliative Care | p-Value |
|---|---|---|---|---|
| N | 5571 | 748 | 4823 | |
| Age (years), mean ± SD | 58.8 ± 12.6 | 60.4 ± 12.4 | 58.5 ± 12.6 | <0.001 |
| <50 | 1216 (21.8%) | 129 (17.2%) | 1087 (22.5%) | 0.002 |
| 50–59 | 1852 (33.2%) | 241 (32.2%) | 1611 (33.4%) | |
| 60–69 | 1403 (25.2%) | 208 (27.8%) | 1195 (24.8%) | |
| ≥70 | 1100 (19.7%) | 170 (22.7%) | 930 (19.3%) | |
| Male | 3537 (63.5%) | 493 (65.9%) | 3044 (63.1%) | 0.14 |
| Race | ||||
| Caucasian | 3422 (61.4%) | 504 (67.4%) | 2918 (60.5%) | 0.001 |
| African American | 473 (8.5%) | 59 (7.9%) | 414 (8.6%) | |
| Hispanic | 584 (10.5%) | 77 (10.3%) | 507 (10.5%) | |
| Other | 1092 (19.6%) | 108 (14.4%) | 984 (20.4%) | |
| Year of hospitalization | ||||
| 2003–2006 | 1270 (22.8%) | 60 (8.0%) | 1210 (25.1%) | <0.001 |
| 2007–2010 | 1756 (31.5%) | 217 (29.0%) | 1539 (31.9%) | |
| 2011–2014 | 2545 (45.7%) | 471 (63.0%) | 2074 (43.0%) | |
| Smoking | 446 (8.0%) | 65 (8.7%) | 381 (7.9%) | 0.46 |
| Alcohol drinking | 1796 (32.2%) | 263 (35.2%) | 1533 (31.8%) | 0.07 |
| Obesity | 340 (6.1%) | 46 (6.1%) | 294 (6.1%) | 0.95 |
| Diabetes mellitus | 1184 (21.3%) | 155 (20.7%) | 1029 (21.3%) | 0.70 |
| Hypertension | 1739 (31.2%) | 217 (29.0%) | 1522 (31.6%) | 0.16 |
| Hyperlipidemia | 352 (6.3%) | 43 (5.7%) | 309 (6.4%) | 0.49 |
| Coronary artery disease | 467 (8.4%) | 56 (7.5%) | 411 (8.5%) | 0.34 |
| Atrial flutter/fibrillation | 400 (7.2%) | 47 (6.3%) | 353 (7.3%) | 0.31 |
| Congestive heart failure | 680 (12.2%) | 73 (9.8%) | 607 (12.6%) | 0.03 |
| Chronic kidney disease | 1620 (29.1%) | 192 (25.7%) | 1428 (29.6%) | 0.03 |
| Acute liver failure | 2247 (40.3%) | 345 (46.1%) | 1902 (39.4%) | 0.001 |
| Hepatitis B infection | 149 (2.7%) | 13 (1.7%) | 136 (2.8%) | 0.09 |
| Hepatitis C infection | 1208 (21.7%) | 148 (19.8%) | 1060 (22.0%) | 0.18 |
| Alcoholic cirrhosis | 2081 (37.4%) | 312 (41.7%) | 1769 (36.7%) | 0.008 |
| Non-alcoholic steatohepatitis | 1069 (19.2%) | 133 (17.8%) | 936 (19.4%) | 0.29 |
| Hepatocellular carcinoma | 343 (6.2%) | 78 (10.4%) | 265 (5.5%) | <0.001 |
| Hospital events | ||||
| Gastrointestinal bleeding | 689 (12.4%) | 83 (11.1%) | 606 (12.6%) | 0.26 |
| Septic shock | 198 (3.6%) | 31 (4.1%) | 167 (3.5%) | 0.35 |
| Bloodstream infections | 641 (11.5%) | 70 (9.4%) | 571 (11.8%) | 0.04 |
| Cardiac arrest | 187 (3.4%) | 22 (2.9%) | 165 (3.4%) | 0.50 |
| In hospital mortality | 1857 (33.3%) | 405 (54.1%) | 1452 (30.1%) | <0.001 |
| Organ dysfunction | ||||
| Respiratory failure | 920 (16.5%) | 119 (15.9%) | 801 (16.6%) | 0.63 |
| Circulatory failure | 1070 (19.2%) | 157 (21.0%) | 913 (18.9%) | 0.18 |
| Metabolic failure | 1371 (24.6%) | 190 (25.4%) | 1181 (24.5%) | 0.59 |
| Neurological failure | 447 (8.0%) | 70 (9.4%) | 377 (7.8%) | 0.15 |
| Hematological failure | 1987 (35.7%) | 262 (35.0%) | 1725 (35.8%) | 0.69 |
| Variables | Univariable Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |
| Clinical characteristics | ||||
| Age (years) | ||||
| <50 | 1 (reference) | 1 (reference) | ||
| 50–59 | 1.26 (1.01–1.58) | 0.04 | 1.22 (0.97–1.54) | 0.10 |
| 60–69 | 1.47 (1.16–1.85) | 0.001 | 1.47 (1.15–1.88) | 0.002 |
| ≥70 | 1.54 (1.21–1.97) | 0.001 | 1.88 (1.44–2.44) | <0.001 |
| Male | 1.13 (0.96–1.33) | 0.14 | ||
| Race | ||||
| Caucasian | 1 (reference) | 1 (reference) | ||
| African American | 0.83 (0.62–1.10) | 0.19 | 0.89 (0.66–1.19) | 0.43 |
| Hispanic | 0.88 (0.68–1.14) | 0.33 | 0.92 (0.70–1.19) | 0.52 |
| Other | 0.64 (0.51–0.79) | <0.001 | 0.80 (0.63–0.99) | 0.04 |
| Year | ||||
| 2003–2006 | 1 (reference) | 1 (reference) | ||
| 2007–2010 | 2.84 (2.12–3.82) | <0.001 | 2.95 (2.19–3.98) | <0.001 |
| 2011–2014 | 4.58 (3.47–6.05) | <0.001 | 4.59 (3.45–6.10) | <0.001 |
| Smoking | 1.11 (0.84–1.46) | 0.46 | ||
| Alcohol drinking | 1.16 (0.99–1.37) | 0.07 | ||
| Obesity | 1.01 (0.73–1.39) | 0.95 | ||
| Diabetes mellitus | 0.96 (0.80–1.17) | 0.70 | ||
| Hypertension | 0.88 (0.75–1.05) | 0.16 | ||
| Dyslipidemia | 0.89 (0.64–1.24) | 0.49 | ||
| Coronary artery disease | 0.87 (0.65–1.16) | 0.34 | ||
| Atrial flutter/fibrillation | 0.85 (0.62–1.16) | 0.31 | ||
| Congestive heart failure | 0.75 (0.58–0.97) | 0.03 | ||
| Chronic kidney disease | 0.82 (0.69–0.98) | 0.03 | 0.65 (0.54–0.78) | <0.001 |
| Acute liver failure | 1.32 (1.13–1.54) | 0.001 | 1.24 (1.05–1.46) | 0.01 |
| Hepatitis B infection | 0.61 (0.34–1.08) | 0.09 | ||
| Hepatitis C infection | 0.88 (0.72–1.06) | 0.18 | ||
| Alcoholic cirrhosis | 1.24 (1.06–1.45) | 0.008 | 1.26 (1.07–1.49) | 0.007 |
| Non-alcoholic steatohepatitis | 0.90 (0.74–1.10) | 0.29 | ||
| Hepatocellular carcinoma | 2.00 (1.54–2.61) | <0.001 | 1.73 (1.31–2.28) | <0.001 |
| Hospital events and organ dysfunction | ||||
| Gastrointestinal bleeding | 0.87 (0.68–1.11) | 0.26 | ||
| Septic shock | 1.21 (0.82–1.78) | 0.35 | ||
| Bloodstream infections | 0.77 (0.59–0.99) | 0.04 | ||
| Cardiac arrest | 0.86 (0.55–1.34) | 0.50 | ||
| Respiratory failure | 0.95 (0.77–1.17) | 0.63 | ||
| Circulatory failure | 1.14 (0.94–1.38) | 0.18 | ||
| Metabolic failure | 1.05 (0.88–1.25) | 0.59 | ||
| Neurological failure | 1.22 (0.93–1.59) | 0.15 | ||
| Hematological failure | 0.97 (0.82–1.14) | 0.69 | ||
| Treatments | Total | Palliative Care | No Palliative Care | p-Value |
|---|---|---|---|---|
| Invasive mechanical ventilation | 575 (10.3) | 59 (7.9) | 516 (10.7) | 0.02 |
| Non-invasive ventilation | 94 (1.7) | 13 (1.7) | 81 (1.7) | 0.91 |
| Blood product transfusion | 1765 (31.7) | 175 (23.4) | 1590 (33.0) | <0.001 |
| Enteral nutrition | 97 (1.7) | 11 (1.5) | 86 (1.8) | 0.54 |
| Paracentesis | 2423 (43.5) | 245 (32.8) | 2178 (45.2) | <0.001 |
| Renal replacement therapy | 1122 (20.1) | 93 (12.4) | 1029 (21.3) | <0.001 |
| Vasopressor | 2491 (44.7) | 257 (34.4) | 2234 (46.3) | <0.001 |
| Do-not-resuscitate status | 379 (6.8) | 183 (24.5) | 196 (4.1) | <0.001 |
| Resource utilization | ||||
| Length of hospital stay (days), mean ± SD | 8.7 ± 10.7 | 6.9 ± 8.4 | 9.0 ± 11.0 | <0.001 |
| Hospital cost ($), mean ± SD | 69,765 ± 130,188 | 52,929 ± 82,404 | 72,340 ± 135,848 | <0.001 |
| Treatments | Adjusted Odds Ratio * (95% CI) | p-Value |
|---|---|---|
| Invasive mechanical ventilation | 0.72 (0.54–0.96) | 0.02 |
| Non-invasive ventilation | 0.97 (0.53–1.77) | 0.91 |
| Blood product transfusion | 0.59 (0.49–0.71) | <0.001 |
| Enteral nutrition | 0.73 (0.38–1.38) | 0.33 |
| Paracentesis | 0.50 (0.42–0.59) | <0.001 |
| Renal replacement therapy | 0.52 (0.41–0.66) | <0.001 |
| Vasopressor | 0.51 (0.43–0.60) | <0.001 |
| Do-not-resuscitate status | 5.95 (4.68–7.56) | <0.001 |
| Resource use | Adjusted coefficient * (95% CI) | |
| Length of stay (days) | −2.1 (−2.9 to −1.3) | <0.001 |
| Hospital cost ($) | −26,268 (−36,429 to −16,107) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thongprayoon, C.; Kaewput, W.; Petnak, T.; O’Corragain, O.A.; Boonpheng, B.; Bathini, T.; Vallabhajosyula, S.; Pattharanitima, P.; Lertjitbanjong, P.; Qureshi, F.; et al. Impact of Palliative Care Services on Treatment and Resource Utilization for Hepatorenal Syndrome in the United States. Medicines 2021, 8, 21. https://doi.org/10.3390/medicines8050021
Thongprayoon C, Kaewput W, Petnak T, O’Corragain OA, Boonpheng B, Bathini T, Vallabhajosyula S, Pattharanitima P, Lertjitbanjong P, Qureshi F, et al. Impact of Palliative Care Services on Treatment and Resource Utilization for Hepatorenal Syndrome in the United States. Medicines. 2021; 8(5):21. https://doi.org/10.3390/medicines8050021
Chicago/Turabian StyleThongprayoon, Charat, Wisit Kaewput, Tananchai Petnak, Oisin A. O’Corragain, Boonphiphop Boonpheng, Tarun Bathini, Saraschandra Vallabhajosyula, Pattharawin Pattharanitima, Ploypin Lertjitbanjong, Fawad Qureshi, and et al. 2021. "Impact of Palliative Care Services on Treatment and Resource Utilization for Hepatorenal Syndrome in the United States" Medicines 8, no. 5: 21. https://doi.org/10.3390/medicines8050021
APA StyleThongprayoon, C., Kaewput, W., Petnak, T., O’Corragain, O. A., Boonpheng, B., Bathini, T., Vallabhajosyula, S., Pattharanitima, P., Lertjitbanjong, P., Qureshi, F., & Cheungpasitporn, W. (2021). Impact of Palliative Care Services on Treatment and Resource Utilization for Hepatorenal Syndrome in the United States. Medicines, 8(5), 21. https://doi.org/10.3390/medicines8050021









