A Goal Intervention Improves Language Fluency: Evidence from Parkinson’s Disease and Healthy Aging
Abstract
1. Introduction
1.1. Language Generation
1.2. Apathy
1.3. Goal-Directed Behavior
1.4. Current Study
2. Materials and Methods
2.1. Participants
2.2. Cognitive Tests and Self-Report Questionnaires
2.3. Language Generation Tasks and Goal Intervention
2.3.1. Complex Scene Description
2.3.2. Word Fluency
2.4. Statistical Analyses
2.4.1. Apathy and Language Generation
2.4.2. Goal Intervention
3. Results
3.1. Cognitive Tests and Self-Report Questionnaires
3.2. Spoken Language Tasks and Goal Intervention
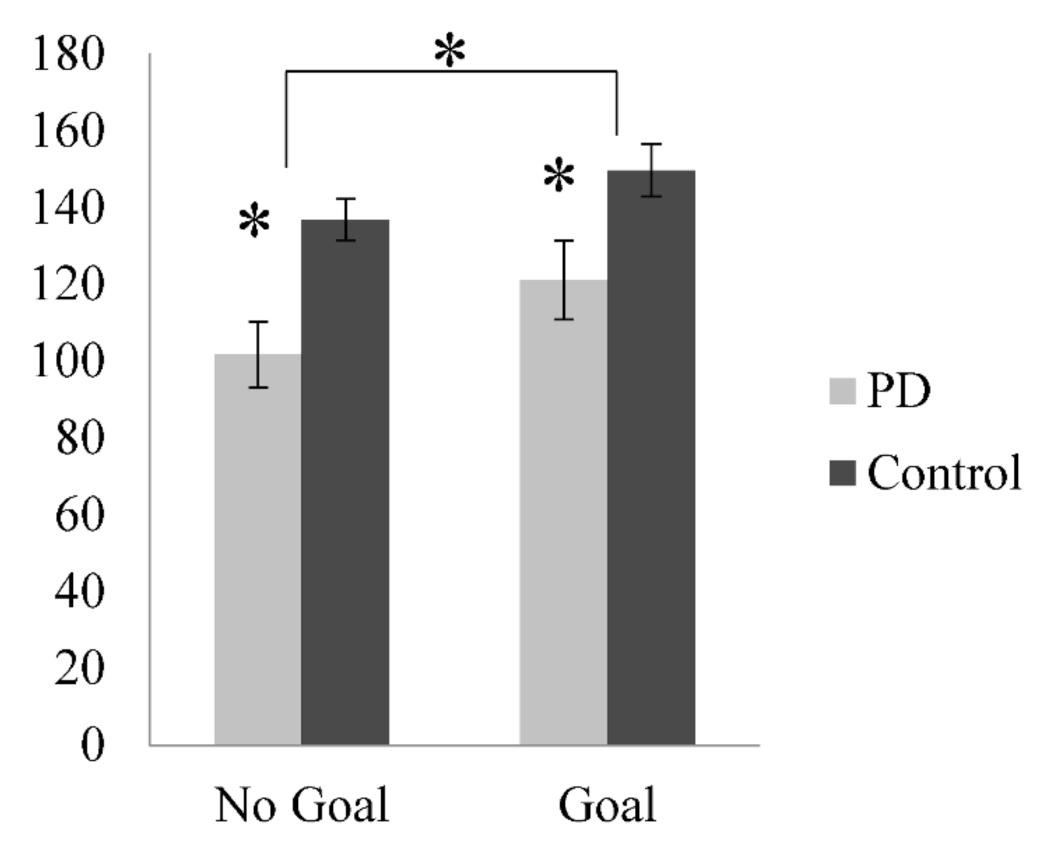
3.2.1. Complex Scene Description
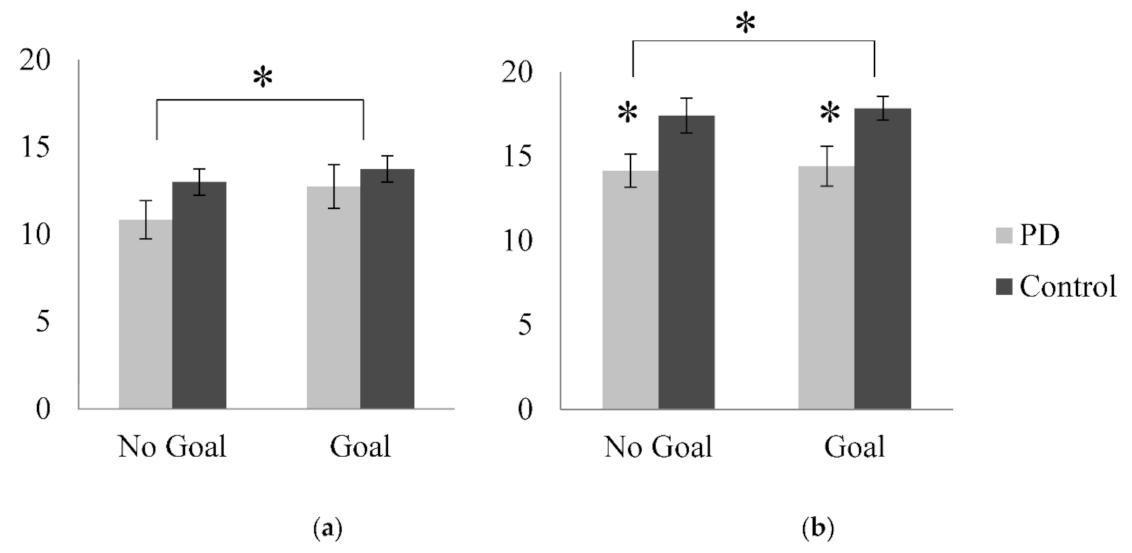
3.2.2. Word Fluency
3.3. Apathy Dimensions and Language Generation
3.4. Apathy Dimension and Goal Intervention
4. Discussion
4.1. Language Generation
4.2. Goal Intervention and Language Generation
4.3. Apathy Dimensions and Language Generation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
Appendix A
| Apathy Evaluation Scale Item | Marin et al. | Levy & Dubois | Current |
|---|---|---|---|
| 1. I am interested in things | Cognitive | Emotional-Affective | Emotion |
| 2. I get things done during the day | Behavioral | Auto-Activation | Initiation |
| 3. Getting things started on my own is important to me | Cognitive | Auto-Activation | Initiation |
| 4. I am interested in having new experiences | Cognitive | Emotional-Affective | Emotion |
| 5. I am interested in learning new things | Cognitive | Emotional-Affective | Emotion |
| 6. I put little effort into anything * | Behavioral | Auto-Activation | Initiation |
| 7. I approach life with intensity | Emotional | Emotional-Affective | Emotion |
| 8. Seeing a job through is important to me | Cognitive | Auto-Activation | Initiation |
| 9. I spend time doing things that interest me | Behavioral | Emotional-Affective | Emotion |
| 10. Someone has to tell me what to do each day * | Behavioral | Auto-Activation | Initiation |
| 11. I am less concerned about my problems than I should be * | Cognitive | Emotional-Affective | Emotion |
| 12. I have friends | Behavioral | Emotional-Affective | Emotion |
| 13. Getting together with friends is important to me | Cognitive | Emotional-Affective | Emotion |
| 14. When something good happens, I get excited | Emotional | Emotional-Affective | Emotion |
| 15. I have an accurate understanding of my problems | Other | Emotional-Affective | Emotion |
| 16. Getting things done during the day is important to me | Cognitive | Auto-Activation | Initiation |
| 17. I have initiative | Other | Auto-Activation | Initiation |
| 18. I have motivation | Other | Emotional-Affective | Emotion |
Appendix B
| Lesion or Dysfunction | Clinical Signs | Measures |
|---|---|---|
| EXECUTIVE APATHY | ||
| Dorsolateral Prefrontal Cortex Basal ganglia (cognitive) Anterior Thalamic Nuclei | ↓ planning & organizing goals: (Poor s elf-generation, switching, spontaneous retrieval, working memory, set maintaining) | ↓ performance on cognitive tests (Tower, Word Fluency, Trail Making B, Brixton, Logical Memory II Digit Span Backwards, Card Shifting) |
| INITIATION APATHY | ||
| Medial Prefrontal Cortex (Superior Frontal Gyrus and Anterior Cingulate Cortex) Basal ganglia (cognitive/limbic) | Short-lived emotional responses ↓ spontaneous activation of mental set/emotional response ↓ self-generation of thoughts ↑ behaviors in response to external solicitation | → AES3, AES6 → AES8, AES16, AES17, AES2 → ↑ performance with external cues → AES10 |
| EMOTION APATHY | ||
| Orbitomedial Prefrontal Cortex Basal ganglia (limbic) | Emotional blunting Loss of interest in activities Decreased reward sensitivity Decreased social involvement | → AES7, AES14, AES11, AES15 → AES1, AES4, AES5, AES9, AES18 → BAS Reward Responsiveness Scale → Gambling and reversal tasks → AES12, AES13 |
References
- Barone, P.; Antonini, A.; Colosimo, C.; Marconi, R.; Morgante, L.; Avarello, T.P.; Bottacchi, E.; Cannas, A.; Ceravolo, G.; Ceravolo, R.; et al. The priamo study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in parkinson’s disease. Mov. Disord. 2009, 24, 1641–1649. [Google Scholar] [CrossRef]
- Brooks, D.J. Diagnosis and management of atypical Parkinsonian syndromes. J. Neurol. Neurosurg. Psychiatry 2002, 72 (Suppl. 1), i10–i16. [Google Scholar]
- Birba, A.; García-Cordero, I.; Kozono, G.; Legaz, A.; Ibáñez, A.; Sedeño, L.; García, A.M. Losing ground: Frontostriatal atrophy disrupts language embodiment in Parkinson’s and Huntington’s disease. Neurosci. Biobehav. Rev. 2017, 80, 673–687. [Google Scholar] [CrossRef]
- Maiti, P.; Manna, J.; Dunbar, G.L. Current understanding of the molecular mechanisms in Parkinson’s disease: Target for potential treatments. Transl. Neurodegener. 2017, 6, 28. [Google Scholar] [CrossRef]
- Owen, A.M.; James, M.; Leigh, P.N.; Summers, B.A.; Marsden, C.D.; Quinn, N.P.; Lange, K.W.; Robbins, T.W.; Robbins, T.W. Fronto-striatal cognitive deficits at different stages of Parkinson’s disease. Brain 1992, 115, 1727–1751. [Google Scholar] [CrossRef]
- Barker, M.S.; Nelson, N.L.; O’Sullivan, J.D.; Adam, R.; Robinson, G.A. Energization and spoken language production: Evidence from progressive supranuclear palsy. Neuropsychologia 2018, 119, 349–362. [Google Scholar] [CrossRef]
- Ellis, C.; Crosson, B.; Gonzalez Rothi, L.J.; Okun, M.S.; Rosenbek, J.C. Narrative discourse cohesion in early stage Parkinson’s disease. J. Parkinson’s Dis. 2015, 5, 403–411. [Google Scholar] [CrossRef]
- Owen, A.M. Cognitive dysfunction in Parkinson’s disease: The role of frontostriatal circuitry. Neuroscientist 2004, 10, 525–537. [Google Scholar] [CrossRef]
- Tjokrowijoto, P.; Ceslis, A.; Sullivan, J.D.; Adam, R.; Mellick, G.; Silburn, P.; Robinson, G.A. Differential patterns of internally generated responses in parkinsonian disorders. Neuropsychologia 2020, 146, 107569. [Google Scholar] [CrossRef]
- Levy, R.; Dubois, B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb. Cortex 2006, 16, 916–928. [Google Scholar] [CrossRef]
- Marin, R.S.; Biedrzycki, R.C.; Firinciogullari, S. Reliability and validity of the apathy evaluation scale. Psychiatry Res. 1991, 38, 143–162. [Google Scholar] [CrossRef]
- Stuss, D.T.; Van Reekum, R.; Murphy, K.J. Differentiation of states and causes of apathy. In The Neuropsychology of Emotion; Borod, J.C., Ed.; Oxford University Press: Oxford, UK, 2000; pp. 340–363. [Google Scholar]
- Barker, M.S.; Nelson, N.L.; Robinson, G.A. Idea Formulation for Spoken Language Production: The Interface of Cognition and Language. J. Int. Neuropsychol. Soc. 2019, 26, 226–240. [Google Scholar] [CrossRef] [PubMed]
- Dell, G.S. A spreading activation theory of retrieval in sentence production. Psychol. Rev. 1986, 93, 283–321. [Google Scholar] [CrossRef]
- Dell, G.S.; Chang, F.; Griffin, Z.M. Connectionist models of language production: Lexical access and grammatical encoding. Cogn. Sci. 1999, 23, 517–542. [Google Scholar] [CrossRef]
- Frederiksen, C.H.; Bracewell, R.J.; Breuleux, A.; Renaud, A. The cognitive representation and processing of discourse: Function and dysfunction. In Discourse Ability and Brain Damage: Theoretical and Empirical Perspectives; Joanette, Y., Brownell, H., Eds.; Springer: New York, NT, USA, 1990; pp. 69–110. [Google Scholar]
- Levelt, W.J.M. Speaking: From Intention to Articulation; MIT Press: Cambridge, MA, USA, 1989. [Google Scholar]
- Levelt, W.J.M.; Roelofs, A.; Meyer, A.S. A theory of lexical access in speech production. Behav. Brain Sci. 1999, 22, 1–75. [Google Scholar] [CrossRef]
- Sherratt, S. Multi-level discourse analysis: A feasible approach. Aphasiology 2007, 21, 375–393. [Google Scholar] [CrossRef]
- Levelt, W.J.M. A blueprint of the speaker. In The Neurocognition of Language; Brown, C., Hagoort, P., Eds.; Oxford Press: Oxford, UK, 1999; pp. 83–122. [Google Scholar]
- Robinson, G.; Shallice, T.; Cipolotti, L. Dynamic aphasia in progressive supranuclear palsy: A deficit in generating a fluent sequence of novel thought. Neuropsychologia 2006, 44, 1344–1360. [Google Scholar] [CrossRef] [PubMed]
- Murray, L.L. Language and parkinson’s disease. Annu. Rev. Appl. Linguist. 2008, 28, 113–127. [Google Scholar] [CrossRef]
- Altmann, L.J.P.; Troche, M.S. High-level language production in parkinson’s disease: A review. Parkinson’s Dis. 2011, 2011, 238956. [Google Scholar] [CrossRef]
- Luria, A.R. Traumatic Aphasia; Mouton: The Hague, The Netherlands, 1970. [Google Scholar]
- Robinson, G.A. Primary progressive dynamic aphasia and Parkinsonism: Generation, selection and sequencing deficits. Neuropsychologia 2013, 51, 2534–2547. [Google Scholar] [CrossRef]
- Esmonde, T.; Giles, E.; Xuereb, J.; Hodges, J. Progressive supranuclear palsy presenting with dynamic aphasia. J. Neurol. Neurosurg. Psychiatry 1996, 60, 403–410. [Google Scholar] [CrossRef]
- Robinson, G.A.; Spooner, D.; Harrison, W.J. Frontal dynamic aphasia in progressive supranuclear palsy: Distinguishing between generation and fluent sequencing of novel thoughts. Neuropsychologia 2015, 77, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Crescentini, C.; Lunardelli, A.; Mussoni, A.; Zadini, A.; Shallice, T. A left basal ganglia case of dynamic aphasia or impairment of extra-language cognitive processes? Neurocase 2008, 14, 184–203. [Google Scholar] [CrossRef] [PubMed]
- Gold, M.; Nadeau, S.E.; Jacobs, D.H.; Adair, J.C.; Rothi, L.J.; Heilman, K.M. Adynamic aphasia: A transcortical motor aphasia with defective semantic strategy formation. Brain Lang. 1997, 57, 374–393. [Google Scholar] [CrossRef] [PubMed]
- Robinson, G.; Shallice, T.; Bozzali, M.; Cipolotti, L. The differing roles of the frontal cortex in fluency tests. Brain 2012, 135, 2202–2214. [Google Scholar] [CrossRef] [PubMed]
- Dirnberger, G.; Jahanshahi, M. Executive dysfunction in parkinson’s disease: A review. J. Neuropsychol. 2013, 7, 193–224. [Google Scholar] [CrossRef]
- Lanctôt, K.L.; Agüera-Ortiz, L.; Brodaty, H.; Francis, P.T.; Geda, Y.E.; Ismail, Z.; Marshall, G.A.; Mortby, M.E.; Onyike, C.U.; Padala, P.R.; et al. Apathy associated with neurocognitive disorders: Recent progress and future directions. Alzheimer’s Dement. 2017, 13, 84–100. [Google Scholar] [CrossRef]
- Nobis, L.; Husain, M. Apathy in Alzheimer’s disease. Curr. Opin. Behav. Sci. 2018, 22, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Robert, P.; Lanctôt, K.L.; Agüera-Ortiz, L.; Aalten, P.; Bremond, F.; Defrancesco, M.; Hanon, C.; David, R.; Dubois, B.; Dujardin, K.; et al. Is it time to revise the diagnostic criteria for apathy in brain disorders? The 2018 international consensus group. Eur. Psychiatry 2018, 54, 71–76. [Google Scholar] [CrossRef]
- Aarsland, D.; Brønnick, K.; Larsen, J.P.; Tysnes, O.B.; Alves, G. Cognitive impairment in incident, untreated Parkinson disease: The Norwegian ParkWest study. Neurology 2009, 72, 1121–1126. [Google Scholar] [CrossRef]
- Pedersen, K.F.; Larsen, J.P.; Aarsland, D. Validation of the unified parkinson’s disease rating scale (updrs) section i as a screening and diagnostic instrument for apathy in patients with parkinson’s disease. Parkinsonism Relat. Disord. 2008, 14, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Radakovic, R.; Abrahams, S. Developing a new apathy measurement scale: Dimensional Apathy Scale. Psychiatry Res. 2014, 219, 658–663. [Google Scholar] [CrossRef] [PubMed]
- Stuss, D.T. Functions of the frontal lobes: Relation to executive functions. J. Int. Neuropsychol. Soc. 2011, 17, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Radakovic, R.; Davenport, R.; Starr, J.M.; Abrahams, S. Apathy dimensions in Parkinsson’s disease. Int. J. Geriatr. Psychiatry 2018, 33, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.E.; Heilman, K.M. Dynamic-intentional thalamic aphasia: A failure of lexical-semantic self-activation. Neurocase 2011, 17, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Luria, A.R.; Tsvetkova, L.S. The Mechanism of Dynamic Aphasia. Found. Lang. 1968, 4, 296–307. [Google Scholar]
- Schultz, W. The primate basal ganglia and the voluntary control of behaviour. J. Conscious. Stud. 1999, 6, 31–45. [Google Scholar]
- Brown, R.; Pluck, G. Negative symptoms: The ‘pathology’ of motivation and goal-directed behaviour. Trends Neurosci. 2000, 23, 412–417. [Google Scholar] [CrossRef]
- Searle, J.R. Intentionality: An Essay in the Philosophy of Mind; Cambridge University Press: Cambridge, UK, 1983. [Google Scholar]
- Locke, E.A.; Latham, G.P. Building a practically useful theory of goal setting and task motivation. Am. Psychol. 2002, 57, 705–717. [Google Scholar] [CrossRef]
- Gauggel, S.; Fischer, S. The effect of goal setting on motor performance and motor learning in brain-damaged patients. Neuropsychol. Rehabil. 2001, 11, 33–44. [Google Scholar] [CrossRef]
- Gauggel, S.; Leinberger, R.; Richardt, M. Goal setting and reaction time performance in brain-damaged patients. J. Clin. Exp. Neuropsychol. 2001, 23, 351–361. [Google Scholar] [CrossRef]
- Schut, H.A.; Stam, H.J. Goals in rehabilitation teamwork. Disabil. Rehabil. 1994, 16, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.L.; Darkins, A.; Mendez, M.; Hill, A.; Benson, D.F. Alzheimer’s disease and parkinson’s disease: Comparison of speech and language alterations. Neurology 1988, 38, 680. [Google Scholar] [CrossRef]
- Radakovic, R.; Abrahams, S. Multidimensional apathy: Evidence from neurodegenerative disease. Curr. Opin. Behav. Sci. 2018, 22, 42–49. [Google Scholar] [CrossRef]
- Hughes, A.J.; Daniel, S.E.; Kilford, L.; Lees, A.J. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. J. Neurol. Neurosurg. Psychiatry 1992, 55, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Oldfield, R.C. The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia 1971, 9, 97–113. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bedirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The montreal cognitive assessment: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Hoops, S.; Nazem, S.; Siderowf, A.D.; Duda, J.E.; Xie, S.X.; Stern, M.B.; Weintraub, D. Validity of the moca and mmse in the detection of mci and dementia in parkinson disease. Neurology 2009, 73, 1738–1745. [Google Scholar] [CrossRef]
- Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease. The Unified Parkinson’s Disease Rating Scale (UPDRS): Status and recommendations. Mov. Disord. 2003, 18, 738–750. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.E.; Willison, J. National Adult Reading Test (NART); Nfer-Nelson: Windsor, UK, 1991. [Google Scholar]
- Raven, J.C. Advanced Progressive Matrices, Set 1; Psychologists Press: Oxford, UK, 1976. [Google Scholar]
- Warrington, E.K.; James, M. The Visual Object and Space Perception Battery; Thames Valley Test Company: Bury St Edmunds, UK, 1991. [Google Scholar]
- Robertson, I.H.; Ward, T.; Ridgeway, V.; Nimmo-Smith, I. The Test of Everyday Attention; Thames Valley Test Company: Bury St Edmunds, UK, 1994. [Google Scholar]
- Wechsler, D. WAIS-III: Wechsler Adult Intelligence Scale, 3rd ed.; Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- Wechsler, D. Wechsler Memory Scale, 3rd ed.; Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- McCarthy, R.; Warrington, E.K. A two-route model of speech production: Evidence from aphasia. Brain 1994, 107, 463–485. [Google Scholar] [CrossRef]
- Druks, J.; Masterson, J. An Object and Action Naming Test: Hove; Psychology Press: London, UK, 2000. [Google Scholar]
- Kay, J.; Lesser, R.; Coltheart, M. Palpa: Psycholinguistic Assessments of Language Processing in Aphasia; Lawrence Erlbaum: Hove, UK, 1992. [Google Scholar]
- Reitan, R.M.; Wolfson, D. The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation; Neuropsychology Press: Tucson, AZ, USA, 1984. [Google Scholar]
- Delis, D.C.; Kaplan, E.; Kramer, J.H. Delis Kaplan Executive Function System: Technical Manual; Psychological Corporation: San Antonio, TX, USA, 2001. [Google Scholar]
- Wilson, B.A.; Alderman, N.; Burgess, P.W.; Emslie, H.; Evans, J.J. Behavioural Assessment of the Dysexecutive Syndrome; Thames Valley Test Company: Bury St Edmunds, UK, 1996. [Google Scholar]
- Burgess, P.W.; Shallice, T. The Hayling and Brixton Tests; Thames Valley Test Company: Bury St Edmunds, UK, 1997. [Google Scholar]
- Lejuez, C.W.; Read, J.P.; Kahler, C.W.; Richards, J.B.; Ramsey, S.E.; Stuart, G.L.; Strong, D.R.; Brown, R.A. Evaluation of a behavioral measure of risk-taking: The balloon analogue risk task (bart). J. Exp. Psychol. 2002, 6, 75–84. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; White, T.L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The bis/bas scales. J. Personal. Soc. Psychol. 1994, 67, 319–333. [Google Scholar] [CrossRef]
- Aarts, E.; Helmich, R.C.; Janssen, M.J.R.; Oyen, W.J.G.; Bloem, B.R.; Cools, R. Aberrant reward processing in parkinson’s disease is associated with dopamine cell loss. NeuroImage 2012, 59, 3339–3346. [Google Scholar] [CrossRef]
- Jordon, L.L.; Zahodne, L.B.; Okun, M.S.; Bowers, D. Hedonic and behavioral deficits associated with apathy in parkinson’s disease: Potential treatment implications. Mov. Disord. 2013, 28, 1301–1304. [Google Scholar] [CrossRef]
- Goodglass, H.; Kaplan, E.; Barresi, B. Boston Diagnostic Aphasia Examination, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Warrington, E.K. The Queen Square Screening Test for Cognitive Deficits; Institute of Neurology: London, UK, 1989. [Google Scholar]
- Benton, A.L. Differential behavioural effects in frontal lobe disease. Neuropsychologia 1968, 6, 53–60. [Google Scholar] [CrossRef]
- Milner, B. Some effects of frontal lobectomy in man. In The Frontal Granular Cortex and Behavior; Warren, J.M., Akert, K., Eds.; McGraw-Hill: New York, NY, USA, 1964; pp. 313–334. [Google Scholar]
- Strauss, E.; Sherman, E.M.S.; Spreen, O. A Compendium of Neuropsychological Tests: Administration, Norms and Commentary; Oxford University Press: New York, NY, USA, 2006. [Google Scholar]
- Borkowski, J.G.; Benton, A.L.; Spreen, O. Word fluency and brain damage. Neuropsychologia 1967, 5, 135–140. [Google Scholar] [CrossRef]
- Fu, C.H.Y.; Morgan, K.; Suckling, J.; Williams, S.C.R.; Andrew, C.; Vythelingum, G.N.; McGuire, P.K. A functional magnetic resonance imaging study of overt letter verbal fluency using a clustered acquisition sequence: Greater anterior cingulate activation with increased task demand. NeuroImage 2002, 17, 871–879. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Satterthwaite, F.E. An approximate distribution of estimates of variance components. Biom. Bull. 1946, 2, 110–114. [Google Scholar] [CrossRef]
- Crawford, J.R.; Garthwaite, P.H. Investigation of the single case in neuropsychology: Confidence limits on the abnormality of test scores and test score differences. Neuropsychologia 2002, 40, 1196–1208. [Google Scholar] [CrossRef]
- Crawford, J.R.; Howell, D.C. Comparing an individual’s test score against norms derived from small samples. Clin. Neuropsychol. 1998, 12, 482–486. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using Spss, 3rd ed.; Sage Publications: London, UK, 2009. [Google Scholar]
- Fisher, R.A. On the interpretation of chi-square from contingency tables, and the calculation of p. J. R. Stat. Soc. 1922, 85, 87–94. [Google Scholar] [CrossRef]
- Pereira, J.B.; Junqué, C.; Martí, M.J.; Ramirez-Ruiz, B.; Bartrés-Faz, D.; Tolosa, E. Structural brain correlates of verbal fluency in Parkinson’s disease. Neuroreport 2009, 20, 741–744. [Google Scholar] [CrossRef]
- Henry, J.D.; Crawford, J.R. Verbal fluency deficits in Parkinson’s disease: A meta-analysis. J. Int. Neuropsychol. Soc. 2004, 10, 608–622. [Google Scholar] [CrossRef] [PubMed]
- Barker, M.S.; Knight, J.L.; Dean, R.J.; Mandelstam, S.; Richards, L.J.; Robinson, G.A. Spoken language production in corpus callosum dysgenesis and partial rhombencephalosynapsis: Verbal adynamia and conceptualisation. Cogn. Behav. Neurol. 2021, 34, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Ceslis, A.; Argall, R.; Henderson, R.D.; McCombe, P.A.; Robinson, G.A. The spectrum of language impairments in amyotrophic lateral sclerosis. Cortex 2020, 132, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Litvan, I.; Goldman, J.G.; Tröster, A.I.; Schmand, B.A.; Weintraub, D.; Petersen, R.C.; Mollenhauer, B.; Adler, C.H.; Marder, K.; Williams-Gray, C.H.; et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov. Disord. 2012, 27, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Lupton, M.K.; Robinson, G.A.; Adam, R.J.; Rose, S.; Byrne, G.J.; Salvado, O.; Pachana, N.A.; Almeida, O.P.; McAloney, K.; Gordan, S.D.; et al. A prospective cohort study of prodromal Alzheimer’s disease: Prospective Imaging Study of Ageing: Genes, Brain and Behaviour (PISA). Neuroimage Clin. 2021, 29, 102527. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M.P. Impairments of procedures for implementing complex language are due to disruption of frontal attention processes. J. Int. Neuropsychol. Soc. 2006, 12, 236–247. [Google Scholar] [CrossRef]
- Gibson, E.C.; Barker, M.S.; Martin, A.K.; Robinson, G.A. Initiation, inhibition and strategy generation across the healthy adult lifespan. Arch. Clin. Neuropsychol. 2018, 34, 511–523. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.K.; Barker, M.S.; Gibson, E.C.; Robinson, G.A. Response initiation and inhibition and the relationship with fluid intelligence across the adult lifespan. Arch. Clin. Neuropsychol. 2021, 36, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Madden, D.L.; Sale, M.V.; Robinson, G.A. Age-related differences in idea generation and selection for propositional language. Aging Neuropsychol. Cogn. 2019, 26, 486–506. [Google Scholar] [CrossRef] [PubMed]
- Salthouse, T.A.; Atkinson, T.M.; Berish, D.E. Executive functioning as a potential mediator of age-related cognitive decline in normal adults. J. Exp. Psychol. Gen. 2003, 132, 566–594. [Google Scholar] [CrossRef]
- Kievit, R.A.; Davis, S.W.; Mitchell, D.J.; Taylor, J.R.; Duncan, J.; Henson, R.N.A. Distinct aspects of frontal lobe structure mediate age-related differences in fluid intelligence and multi-tasking. Nat. Commun. 2014, 5, 5658. [Google Scholar] [CrossRef]
- Barker, M.S.; Young, B.; Robinson, G.A. Cohesive and coherent connected speech deficits in mild stroke. Brain Lang. 2017, 168, 23–36. [Google Scholar] [CrossRef] [PubMed]
- Den Brok, M.G.H.E.; Van Dalen, J.W.; Van Gool, W.A.; Moll van Charante, E.P.; De Bie, R.M.A.; Richard, E. Apathy in Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2015, 30, 759–769. [Google Scholar] [CrossRef] [PubMed]
| PD Patients n = 21 | Healthy Controls n = 22 | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Sex (Male:Female) | 14:7 | - | 10:12 | - |
| Age (Years) | 70.24 | 5.98 | 66.81 | 8.68 |
| Education (Years) | 13.36 | 3.29 | 13.84 | 3.53 |
| MoCA (/30) | 25.43 | 3.82 | 27.87 | 2.10 |
| Disease Severity | ||||
| Years since Diagnosis | 8.38 | 5.26 | - | - |
| UPDRS | 64.56 | 18.54 | - | - |
| Hoehn & Yahr | 2.69 | 0.87 | - | - |
| Executive Apathy (Cognitive) | Initiation Apathy (Auto-Activation) | Emotion Apathy (Emotional-Affective) |
|---|---|---|
| Significantly impaired on ≥2/5 executive function tests (Trail Making B Test, Digit Span Backwards, Brixton, Tower, Card Shift 2) | Significantly elevated above controls on AES Initiation Apathy subscale (see Appendix A) | Significantly elevated above controls on AES Emotion Apathy subscale (see Appendix A) BART BIS/BAS Reward Responsiveness |
| PD Patients n = 21 | Healthy Controls n = 22 | ||||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| Intellectual Functioning | |||||
| NART Estimated FSIQ | 111.15 | 10.52 | 113.00 | 9.62 | |
| Raven’s APM (/12) | 6.05 * | 3.53 | 8.65 | 2.37 | |
| Visual Perception | |||||
| Incomplete Letters (/20) | 19.14 * | 1.20 | 19.95 | 0.22 | |
| Working Memory | |||||
| Digit Span Total (/30) | 17.85 | 4.28 | 18.95 | 4.83 | |
| Digit Span Forward (/16) | 10.70 | 2.62 | 11.45 | 2.80 | |
| Digit Span Backward (/14) | 7.15 | 2.32 | 7.50 | 2.26 | |
| Speed and Attention | |||||
| Trail Making Test Motor Speed (s) | 34.05 | 13.08 | 28.30 | 10.22 | |
| Trail Making Test A (s) | 50.44 | 46.07 | 34.41 | 17.67 | |
| Elevator Counting (/7) | 6.87 | 0.52 | 7.00 | 0.00 | |
| Elevator Count + Distraction (/10) | 7.56 | 3.18 | 7.73 | 2.55 | |
| Memory | |||||
| Verbal Immediate (/75) | 35.79 * | 8.52 | 44.23 | 12.98 | |
| Verbal Delayed (/50) | 20.21 * | 6.84 | 27.82 | 10.02 | |
| Verbal Recognition (/30) | 24.31 | 3.61 | 25.35 | 3.54 | |
| Language | |||||
| Sentence Repetition (/10) | 9.67 | 0.66 | 9.91 | 0.29 | |
| Object Naming (/79) | 77.950 | 2.12 | 78.65 | 0.59 | |
| Synonyms Total (/60) | 57.17 | 2.68 | 58.75 | 1.73 | |
| Executive Functioning | |||||
| Trail Making Test B (s) | 119.45 * | 84.91 | 72.11 | 30.13 | |
| BART (average adjusted pumps) | 21.55 | 9.20 | 24.62 | 8.36 | |
| Tower Total Achievement Score (/30) | 16.60 | 6.52 | 17.59 | 3.18 | |
| Card Shift Rule 1 (/20) | 19.81 | 0.87 | 20.00 | 0.00 | |
| Card Shift Rule 2 (/20) | 17.90 * | 2.15 | 19.32 | 1.11 | |
| Brixton SS (/10) | 4.00 | 2.66 | 5.44 | 1.86 | |
| Brixton Errors (total) | 23.61 * | 10.11 | 17.50 | 5.65 | |
| Hayling SS (/10) | 4.50 | 1.99 | 5.35 | 1.37 | |
| PD Patients n = 21 | Healthy Controls n = 22 | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Apathy Evaluation Scale (/72) | 31.70 * | 8.14 | 25.94 | 7.52 |
| HADS Anxiety (/21) | 5.05 | 2.91 | 3.65 | 2.91 |
| HADS Depression (/21) | 4.63 ** | 2.90 | 1.75 | 1.71 |
| Behavioral Inhibition Scale (/28) | 18.25 | 2.32 | 20.31 | 3.89 |
| BAS: Drive (/16) | 10.75 | 2.59 | 9.25 | 2.18 |
| BAS: Fun Seeking (/16) | 11.16 | 2.03 | 10.38 | 2.22 |
| BAS: Reward Response (/20) | 15.50 | 2.92 | 16.12 | 2.52 |
| PD Patients n = 21 | Healthy Controls n = 22 | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Picture Elicited Narrative Task | ||||
| Baseline (Cookie) | 104.58 | 40.75 | 136.83 | 24.81 |
| Goal (Beach) | 122.95 | 43.18 | 149.67 | 29.35 |
| Phonemic Fluency | ||||
| Baseline (FAS) | 10.93 | 4.72 | 12.98 | 3.43 |
| Goal (BMW) | 12.92 | 5.38 | 13.75 | 3.26 |
| Semantic Fluency | ||||
| Baseline (F&V, Animals) | 14.05 | 4.21 | 17.42 | 4.50 |
| Goal (Food, Clothing) | 14.39 | 4.87 | 17.84 | 3.08 |
| No Apathy | Executive Apathy | Initiation Apathy | Emotion Apathy | |
|---|---|---|---|---|
| Complex Scene Description | ||||
| Deficit: No Deficit | 3:10 | 4:0 | 3:1 | 1:2 |
| % with Deficit | 23% | 100% * | 75% | 50% |
| Phonemic Fluency | ||||
| Deficit: No Deficit | 0:13 | 0:4 | 0:4 | 0:4 |
| % with Deficit | 0% | 0% | 0% | 0% |
| Semantic Fluency | ||||
| Deficit: No Deficit | 2:11 | 4:0 | 3:1 | 1:6 |
| % with Deficit | 15% | 100% * | 75% | 14% |
| Controls | PD No Apathy | PD Executive Apathy | PD Initiation Apathy | PD Emotion Apathy | |
|---|---|---|---|---|---|
| Complex Scene Description | |||||
| Goal Benefit: No Goal Benefit | 12:6 | 9:2 | 2:1 | 1:2 | 1:1 |
| % with Benefit | 67% | 82% | 67% | 33% | 50% |
| Phonemic Fluency | |||||
| Goal Benefit: No Goal Benefit | 11:8 | 10:2 | 3:1 | 2:1 | 2:0 |
| % with Benefit | 58% | 83% | 75% | 67% | 100% |
| Semantic Fluency | |||||
| Goal Benefit: No Goal Benefit | 12:7 | 5:6 | 2:2 | 1:2 | 2:0 |
| % with Benefit | 63% | 45% | 50% | 33% | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson, G.A.; Campbell, L.; Ceslis, A. A Goal Intervention Improves Language Fluency: Evidence from Parkinson’s Disease and Healthy Aging. Medicines 2021, 8, 15. https://doi.org/10.3390/medicines8030015
Robinson GA, Campbell L, Ceslis A. A Goal Intervention Improves Language Fluency: Evidence from Parkinson’s Disease and Healthy Aging. Medicines. 2021; 8(3):15. https://doi.org/10.3390/medicines8030015
Chicago/Turabian StyleRobinson, Gail A., Lara Campbell, and Amelia Ceslis. 2021. "A Goal Intervention Improves Language Fluency: Evidence from Parkinson’s Disease and Healthy Aging" Medicines 8, no. 3: 15. https://doi.org/10.3390/medicines8030015
APA StyleRobinson, G. A., Campbell, L., & Ceslis, A. (2021). A Goal Intervention Improves Language Fluency: Evidence from Parkinson’s Disease and Healthy Aging. Medicines, 8(3), 15. https://doi.org/10.3390/medicines8030015





