Risk Factors and Predictive Model for Mortality of Hospitalized COVID-19 Elderly Patients from a Tertiary Care Hospital in Thailand
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Outcomes
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Treatment and Complication
3.3. Risk Factors for Mortality
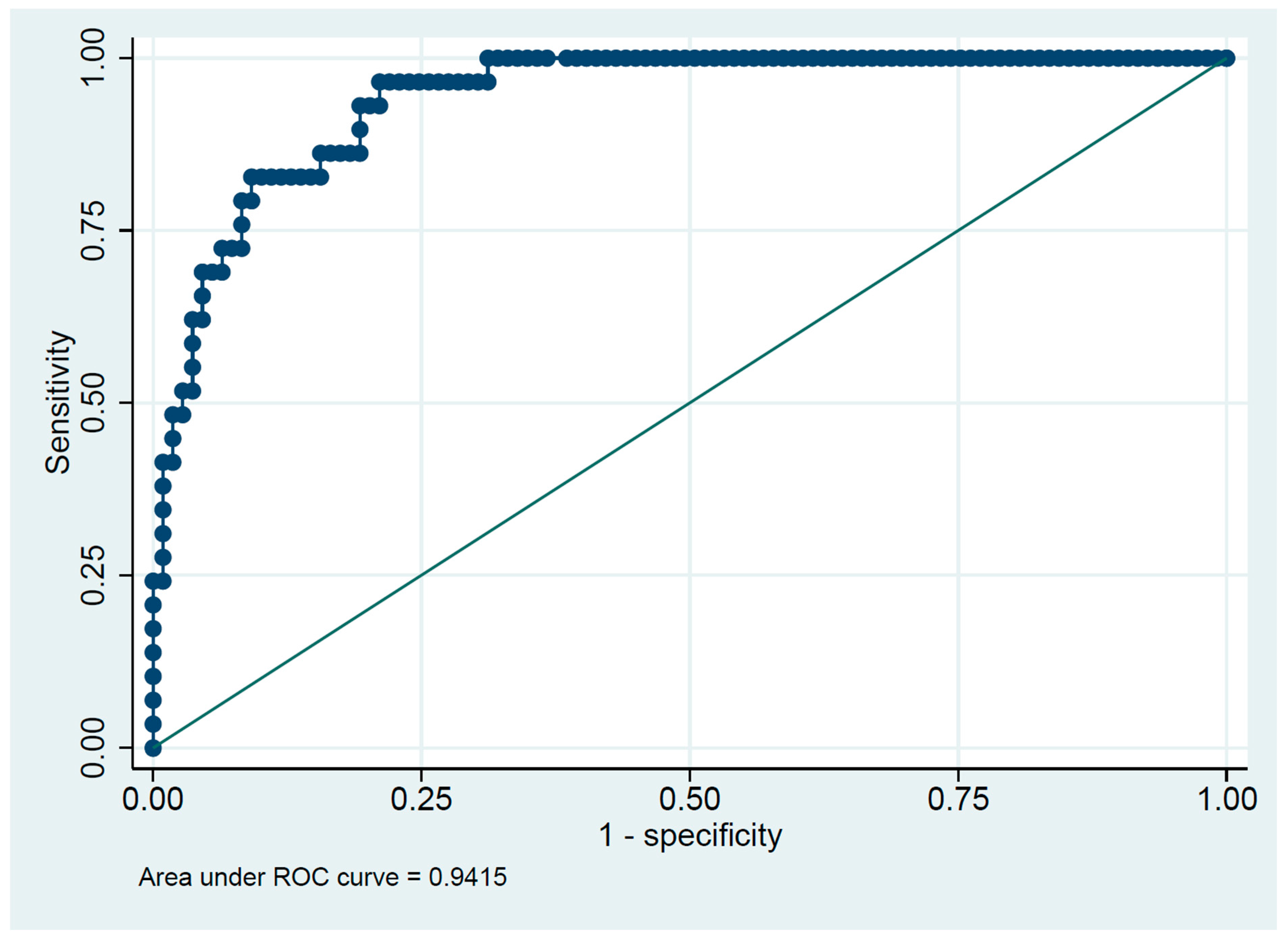
3.4. Predicting Risk Score for Assessing Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Chief Declares End to COVID-19 as a Global Health Emergency. Available online: https://news.un.org/en/story/2023/05/1136367/ (accessed on 7 September 2023).
- Parasher, A. COVID-19: Current understanding of its Pathophysiology, Clinical presentation and Treatment. Postgrad. Med. J. 2020, 97, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Bansod, S.; Ahirwar, A.K.; Sakarde, A.; Asia, P.; Gopal, N.; Alam, S.; Kaim, K.; Ahirwar, P.; Sorte, S.R. COVID-19 and geriatric population: From pathophysiology to clinical perspectives. Horm. Mol. Biol. Clin. Investig. 2021, 42, 87–98. [Google Scholar] [CrossRef] [PubMed]
- COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/index.html (accessed on 18 February 2023).
- Tizazu, A.M.; Mengist, H.M.; Demeke, G. Aging, inflammaging and immunosenescence as risk factors of severe COVID-19. Immun. Ageing 2022, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Sherwani, S.; Khan, M.W.A. Cytokine Response in SARS-CoV-2 Infection in the Elderly. J. Inflamm. Res. 2020, 13, 737–747. [Google Scholar] [CrossRef] [PubMed]
- Becerra-Muñoz, V.M.; Núñez-Gil, I.J.; Eid, C.M.; Aguado, M.G.; Romero, R.; Huang, J.; Mulet, A.; Ugo, F.; Rametta, F.; Liebetrau, C.; et al. Clinical profile and predictors of in-hospital mortality among older patients hospitalised for COVID-19. Age Ageing 2021, 50, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Knopp, P.; Miles, A.; Webb, T.E.; Mcloughlin, B.C.; Mannan, I.; Raja, N.; Wan, B.; Davis, D. Presenting features of COVID-19 in older people: Relationships with frailty, inflammation and mortality. Eur. Geriatr. Med. 2020, 11, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Rincon, J.-M.; Buonaiuto, V.; Ricci, M.; Martín-Carmona, J.; Paredes-Ruíz, D.; Calderón-Moreno, M.; Rubio-Rivas, M.; Beato-Pérez, J.-L.; Arnalich-Fernández, F.; Monge-Monge, D.; et al. Clinical Characteristics and Risk Factors for Mortality in Very Old Patients Hospitalized With COVID-19 in Spain. J. Gerontol. Ser. A 2021, 76, e28–e37. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Ning, R.; Tao, Y.; Yu, C.; Deng, X.; Zhao, C.; Meng, S.; Tang, F.; Xu, D. Risk Factors for Mortality in 244 Older Adults With COVID-19 in Wuhan, China: A Retrospective Study. J. Am. Geriatr. Soc. 2020, 68, e19–e23. [Google Scholar] [CrossRef] [PubMed]
- Gálvez-Barrón, C.; Arroyo-Huidobro, M.; Miňarro, A.; Añaños, G.; Chamero, A.; Martín, M.; Gris, C.; Avalos, J.L.; Capielo, A.M.; Ventosa, E.; et al. COVID-19: Clinical Presentation and Prognostic Factors of Severe Disease and Mortality in the Oldest-Old Population: A Cohort Study. Gerontology 2022, 68, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Garcia, P.; Garmendia-Prieto, B.; Cristofori, G.; Montoya, I.L.; Hidalgo, J.J.; Feijoo, M.Q.; Cortés, J.J.B.; Gómez-Pavón, J. Health status in survivors older than 70 years after hospitalization with COVID-19: Observational follow-up study at 3 months. Eur. Geriatr. Med. 2021, 12, 1091–1094. [Google Scholar] [CrossRef] [PubMed]
- Zerah, L.; Baudouin, É.; Pépin, M.; Mary, M.; Krypciak, S.; Bianco, C.; Roux, S.; Gross, A.; Toméo, C.; Lemarié, N.; et al. Clinical Characteristics and Outcomes of 821 Older Patients With SARS-CoV-2 Infection Admitted to Acute Care Geriatric Wards. J. Gerontol. Ser. A 2021, 76, e4–e12. [Google Scholar] [CrossRef] [PubMed]
- Morandi, A.; Rebora, P.; Isaia, G.; Grossi, E.; Faraci, B.; Gentile, S.; Bo, M.; Valsecchi, M.G.; Deiana, V.; Ghezzi, N.; et al. Delirium symptoms duration and mortality in SARS-CoV2 elderly: Results of a multicenter retrospective cohort study. Aging Clin. Exp. Res. 2021, 33, 2327–2333. [Google Scholar] [CrossRef] [PubMed]
- Trecarichi, E.M.; Mazzitelli, M.; Serapide, F.; Pelle, M.C.; Tassone, B.; Arrighi, E.; Perri, G.; Fusco, P.; Scaglione, V.; Davoli, C.; et al. Clinical characteristics and predictors of mortality associated with COVID-19 in elderly patients from a long-term care facility. Sci. Rep. 2020, 10, 20834. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Montoya, I.; Quezada-Feijoo, M.; Jaramillo-Hidalgo, J.; Garmendia-Prieto, B.; Lisette-Carrillo, P.; Gómez-Pavón, F.J. Mortality risk factors in a Spanish cohort of oldest-old patients hospitalized with COVID-19 in an acute geriatric unit: The OCTA-COVID study. Eur. Geriatr. Med. 2021, 12, 1169–1180. [Google Scholar] [CrossRef] [PubMed]
- Covino, M.; De Matteis, G.; Santoro, M.; Sabia, L.; Simeoni, B.; Candelli, M.; Ojetti, V.; Franceschi, F. Clinical characteristics and prognostic factors in COVID-19 patients aged ≥80 years. Geriatr. Gerontol. Int. 2020, 20, 704–708. [Google Scholar] [CrossRef] [PubMed]
- Srisompong, J. Predictive factors associated with mortality outcomes of severe COVID-19 pneumonia in elderly patients, Suratthani Hospital, Thailand. Reg. 11 Med. J. 2023, 37, 1–19. [Google Scholar]
- Na, Y.S.; Kim, J.H.; Baek, M.S.; Kim, W.-Y.; Baek, A.-R.; Lee, B.Y.; Seong, G.M.; Lee, S.-I. In-hospital mortality prediction using frailty scale and severity score in elderly patients with severe COVID-19. Acute Crit. Care 2022, 37, 303–311. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 138) | Survive (n = 109) | Death (n = 29) | p-Value |
|---|---|---|---|---|
| Age (years), mean ± SD | 72.8 ± 8.4 | 71.6 ± 7.6 | 77.6 ± 9.7 | 0.003 |
| Male, n (%) | 66 (48%) | 50 (46%) | 16 (55%) | 0.41 |
| Comorbidity, n (%) | ||||
| Diabetes mellitus | 60 (43%) | 44 (40%) | 16 (55%) | 0.21 |
| Hypertension | 93 (67%) | 69 (63%) | 24 (83%) | 0.073 |
| Dyslipidemia | 71 (51%) | 53 (49%) | 18 (62%) | 0.22 |
| Coronary artery disease | 17 (16%) | 12 (11%) | 5 (17%) | 0.35 |
| Congestive heart failure | 2 (1%) | 1 (1%) | 1 (3%) | 0.38 |
| Ischemic stroke | 11 (8%) | 5 (5%) | 6 (21%) | 0.01 |
| Hemorrhagic stroke | 2 (1%) | 0 | 2 (7%) | 0.04 |
| Connective tissue disease | 1 (1%) | 1 (1%) | 0 | 1 |
| Chronic kidney disease | 11 (8%) | 5 (5%) | 6 (21%) | 0.01 |
| Cirrhosis | 2 (1%) | 1 (1%) | 1 (3%) | 0.38 |
| Chronic lung disease | 8 (6%) | 7 (6%) | 1 (3%) | 1 |
| Dementia | 6 (4%) | 3 (3%) | 3 (10%) | 0.11 |
| Depression | 1 (1%) | 1 (1%) | 0 | 1 |
| Hearing problem | 2 (1%) | 1 (1%) | 1 (3%) | 0.38 |
| Adjusted Charlson comorbidity index, mean ± SD | 3.9 ± 1.8 | 3.6 ± 1.7 | 4.8 ± 2.1 | 0.001 |
| Medication, n (%) | ||||
| Aspirin | 36 (27%) | 26 (25%) | 10 (36%) | 0.24 |
| ACE inhibitors | 22 (16%) | 18 (17%) | 4 (14%) | 1 |
| ARBs | 23 (17%) | 17 (16%) | 6 (21%) | 0.58 |
| Corticosteroid | 10 (7%) | 7 (7%) | 3 (11%) | 0.43 |
| Statin | 67 (50%) | 49 (46%) | 18 (64%) | 0.09 |
| Metformin | 35 (26%) | 24 (22%) | 11 (41%) | 0.08 |
| COVID Vaccine, n (%) | ||||
| None | 39 (28%) | 32 (29%) | 7 (24%) | 0.255 |
| 1 dose | 90 (65%) | 68 (62%) | 22 (76%) | |
| 2 doses | 9 (7%) | 9 (8%) | 0 | |
| COVID vaccine type, n (%) | ||||
| 1st dose | ||||
| CoronaVac | 7 (7%) | 7 (9%) | 0 | |
| BBIBP-CorV | 2 (2%) | 1 (1%) | 1 (5%) | 0.132 |
| ChAdOx1-S/AZD1222 | 34 (34%) | 29 (38%) | 5 (23%) | |
| 2nd dose | ||||
| CoronaVac | 1 (1%) | 1 (1%) | 0 | |
| BBIBP-CorV | 1 (1%) | 1 (1%) | 0 | 1.00 |
| ChAdOx1-S/AZD1222 | 6 (4%) | 6 (6%) | 0 | |
| BNT162b2 | 1 (1%) | 1 (1%) | 0 |
| Total (n = 138) | Survive (n = 109) | Death (n = 29) | p-Value | |
|---|---|---|---|---|
| Clinical presentation, n (%) | ||||
| Fever | 101 (73%) | 79 (72) | 22 (76) | 0.82 |
| Cough | 121 (88%) | 94 (86) | 27 (93) | 0.53 |
| Dyspnea | 79 (57%) | 54 (50) | 25 (86) | <0.001 |
| Fatigue | 87 (63%) | 62 (57) | 25 (86) | 0.004 |
| Anorexia | 34 (25%) | 26 (24) | 8 (28) | 0.81 |
| Anosmia | 16 (12%) | 15 (14) | 1 (3) | 0.19 |
| Ageusia | 18 (13%) | 15 (14) | 3 (10) | 0.76 |
| Diarrhea | 19 (14%) | 15 (14) | 4 (14) | 1 |
| Confusion | 6 (4%) | 1 (1) | 5 (17) | 0.002 |
| Physical examination, mean ± SD | ||||
| Body weight (kg) | 63.1 ± 14 | 62.9 ± 15 | 64.2 ± 13 | 0.36 |
| BMI (kg/m2) | 24.7 ± 5.1 | 24.8 ± 5.3 | 24.1 ± 4.3 | 0.73 |
| Body temperature (°C) | 37.2 ± 0.9 | 37.1 ± 0.7 | 37.5 ± 1.2 | 0.34 |
| MAP (mmHg) | 96 ± 15 | 98 ± 12.8 | 90 ± 69 | 0.02 |
| Pulse rate (/min) | 88 ± 17 | 86 ± 16 | 94 ± 18 | 0.02 |
| Respiratory rate (/min) | 22 ± 5 | 20 ± 3 | 27 ± 7 | <0.001 |
| Oxygen saturation (%) | 94 ± 9 | 96 ± 3 | 86 ± 16 | <0.001 |
| Laboratory, mean ± SD | ||||
| Hemoglobin (g/dL) | 12 ± 2 | 12 ± 2 | 11 ± 2 | 0.003 |
| Hematocrit (%) | 37 ± 5 | 38 ± 5 | 34 ± 7 | <0.001 |
| WBC (/µL) | 6302 ± 2929 | 5885 ± 2432 | 7869 ± 3994 | 0.004 |
| TLC (/µL) | 1494 ± 843 | 1629 ± 853 | 988 ± 578 | <0.001 |
| TNC (/µL) | 4105 ± 2824 | 3530 ± 2175 | 6265 ± 3829 | <0.001 |
| Total protein (g/dL) | 7.3 ± 0.7 | 7.4 ± 0.7 | 7.1 ± 0.7 | 0.045 |
| Albumin (g/dL) | 3.6 ± 0.4 | 3.7 ± 0.4 | 3.3 ± 0.4 | <0.001 |
| AST (U/L) | 71 ± 201 | 48 ± 92 | 159 ± 393 | <0.001 |
| ALT (U/L) | 44 ± 120 | 31 ± 35 | 91 ± 251 | 0.02 |
| ALP (U/L) | 83 ± 56 | 81 ± 57 | 91 ± 50 | 0.2 |
| CRP (mg/dL) | 54 ± 58 | 40 ± 47 | 106 ± 69 | <0.001 |
| BUN (mg/dL) | 19 ± 12 | 16 ± 7 | 31 ± 19 | <0.001 |
| Creatinine (mg/dL) | 1.2 ± 1.1 | 1.0 ± 0.7 | 2.1 ± 1.8 | <0.001 |
| eGFR (mL/min/1.73 m2) | 65 ± 24 | 71 ± 21 | 43 ± 24 | <0.001 |
| Sodium (mEq/L) | 136 ± 5 | 137 ± 5 | 133 ± 5 | <0.001 |
| Potassium (mEq/L) | 3.8 ± 0.6 | 3.7 ± 0.5 | 4.2 ± 0.9 | 0.003 |
| Chloride (mEq/L) | 101 ± 5 | 101 ± 5 | 100 ± 6 | 0.17 |
| Bicarbonate (mEq/L) | 25 ± 3 | 26 ± 3 | 22 ± 4 | <0.001 |
| Total (n = 138) | Survive (n = 109) | Death (n = 29) | |
|---|---|---|---|
| Treatment, n (%) | |||
| Anti-coagulant | 70 (50%) | 48 (44%) | 22 (75%) |
| Antibiotic | 44 (32%) | 17 (16%) | 27 (93%) |
| Steroid | 113 (81%) | 85 (78%) | 28 (97%) |
| Inotropic drug | 15 (11%) | 1 (1%) | 14 (48%) |
| Invasive mechanical ventilator | 12 (9%) | 0 | 12 (41%) |
| Non-invasive mechanical ventilator | 38 (27%) | 14 (13%) | 24 (83%) |
| Intensive care unit | 20 (14%) | 5 (5%) | 15 (52%) |
| Complication, n (%) | |||
| Sepsis | 23 (16%) | 4 (4%) | 19 (66%) |
| Respiratory failure | 38 (28%) | 9 (8%) | 29 (100%) |
| Hospital-acquired pneumonia | 27 (20%) | 7 (6%) | 20 (69%) |
| Renal failure | 25 (18%) | 8 (7%) | 17 (59%) |
| Arrhythmia | 9 (7%) | 1 (1%) | 8 (28%) |
| Pulmonary embolism | 3 (2%) | 0 | 3 (10%) |
| Delirium | 16 (12%) | 6 (6%) | 10 (34%) |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Variable | Odds Ratio | 95% CI | p-Value | Odds Ratio | 95% CI | p-Value |
| Age | 1.09 | 1.04–1.15 | 0.001 | 1.27 | 1.06–1.51 | 0.009 |
| Female | 0.69 | 0.30–1.57 | 0.374 | |||
| Under-weight 1 | 1.78 | 0.40–7.84 | 0.446 | 24.45 | 0.14–4312 | 0.226 |
| Obesity 2 | 1.13 | 0.48–2.66 | 0.789 | 14.75 | 0.61–345 | 0.097 |
| Diabetes mellitus | 1.82 | 0.80–4.15 | 0.156 | 1.95 | 0.15–26.12 | 0.613 |
| Charlson comorbidities index | 1.38 | 1.11–1.71 | 0.004 | 0.41 | 0.16–1.09 | 0.074 |
| Body temperature | 1.53 | 0.98–2.39 | 0.063 | |||
| Pulse rate | 1.03 | 1.01–1.06 | 0.019 | 1.06 | 0.98–1.15 | 0.136 |
| Mean arterial pressure | 0.96 | 0.93–0.99 | 0.012 | 0.99 | 0.89–1.10 | 0.902 |
| Respiratory rate | 1.37 | 1.20–1.55 | <0.001 | 1.40 | 1.11–1.76 | 0.005 |
| Hemoglobin | 0.67 | 0.53–0.85 | 0.001 | 0.66 | 0.36–1.20 | 0.168 |
| Total lymphocyte count | 1.00 | 0.997–0.999 | <0.001 | 1.00 | 0.99–1.00 | 0.125 |
| Total Neutrophil count | 1.00 | 1.0002–1.0005 | <0.001 | 1.00 | 1.00–1.00 | 0.624 |
| Albumin | 0.13 | 0.05–0.37 | <0.001 | 0.07 | 0.00–3.29 | 0.177 |
| CRP | 1.02 | 1.01–1.03 | <0.001 | 1.01 | 0.99–1.03 | 0.532 |
| Sodium | 0.89 | 0.81–0.97 | 0.007 | 0.90 | 0.76–1.07 | 0.231 |
| GFR | 0.95 | 0.93–0.97 | <0.001 | 0.93 | 0.88–0.98 | 0.01 |
| Congestive heart failure | 3.86 | 0.23–63.61 | 0.345 | |||
| Stroke | 5.43 | 1.52–19.32 | 0.009 | 89.20 | 1.83–4339 | 0.023 |
| Hypertension | 2.78 | 0.98–7.87 | 0.054 | |||
| Chronic lung disease | 0.52 | 0.06–4.41 | 0.549 | 0.05 | 0.00–98.67 | 0.442 |
| ACE-inhibitor | 1.32 | 0.76–2.29 | 0.325 | 1.83 | 0.11–29.53 | 0.672 |
| Anti-coagulant | 0.80 | 0.25–2.58 | 0.704 | 4.17 | 0.13–137 | 0.423 |
| Statin | 2.13 | 0.90–5.04 | 0.085 | |||
| Metformin | 2.38 | 0.97–5.80 | 0.057 | |||
| Any COVID vaccine | 1.31 | 0.51–3.36 | 0.580 | |||
| Variable | Coefficient | 95% CI | p-Value |
|---|---|---|---|
| Age | 0.10 | 0.02–0.17 | 0.01 |
| Respiratory rate | 0.32 | 0.16–0.49 | <0.001 |
| GFR | −0.05 | −0.09 to −0.02 | 0.001 |
| Stroke | 0.93 | −0.775 to 2.634 | 0.285 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuansangeam, M.; Srithan, B.; Pattharanitima, P.; Phadungsaksawasdi, P. Risk Factors and Predictive Model for Mortality of Hospitalized COVID-19 Elderly Patients from a Tertiary Care Hospital in Thailand. Medicines 2023, 10, 59. https://doi.org/10.3390/medicines10110059
Chuansangeam M, Srithan B, Pattharanitima P, Phadungsaksawasdi P. Risk Factors and Predictive Model for Mortality of Hospitalized COVID-19 Elderly Patients from a Tertiary Care Hospital in Thailand. Medicines. 2023; 10(11):59. https://doi.org/10.3390/medicines10110059
Chicago/Turabian StyleChuansangeam, Mallika, Bunyarat Srithan, Pattharawin Pattharanitima, and Pawit Phadungsaksawasdi. 2023. "Risk Factors and Predictive Model for Mortality of Hospitalized COVID-19 Elderly Patients from a Tertiary Care Hospital in Thailand" Medicines 10, no. 11: 59. https://doi.org/10.3390/medicines10110059
APA StyleChuansangeam, M., Srithan, B., Pattharanitima, P., & Phadungsaksawasdi, P. (2023). Risk Factors and Predictive Model for Mortality of Hospitalized COVID-19 Elderly Patients from a Tertiary Care Hospital in Thailand. Medicines, 10(11), 59. https://doi.org/10.3390/medicines10110059






