Mitigation of Benzene-Induced Haematotoxicity in Sprague Dawley Rats through Plant-Extract-Loaded Silica Nanobeads
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection and Preparation of Plant Material
2.2. Synthesis of Silica Nanobeads
2.3. Characterization
2.4. Drug Loading on SNBs
2.5. CMC Coating on Plant-Extract-Loaded SNBs
2.6. In Vivo Studies
2.7. Animal Study
2.8. Induction of Benzene Haematotoxicity in Sprague Dawley Rats
2.9. Drug Administration
2.10. Blood Profiling of Rats
2.11. Bone Marrow Staining
3. Results
3.1. UV–Vis Spectroscopy of Plant-Extract-Loaded SNBs and UV/LC-MS of Plant Extracts
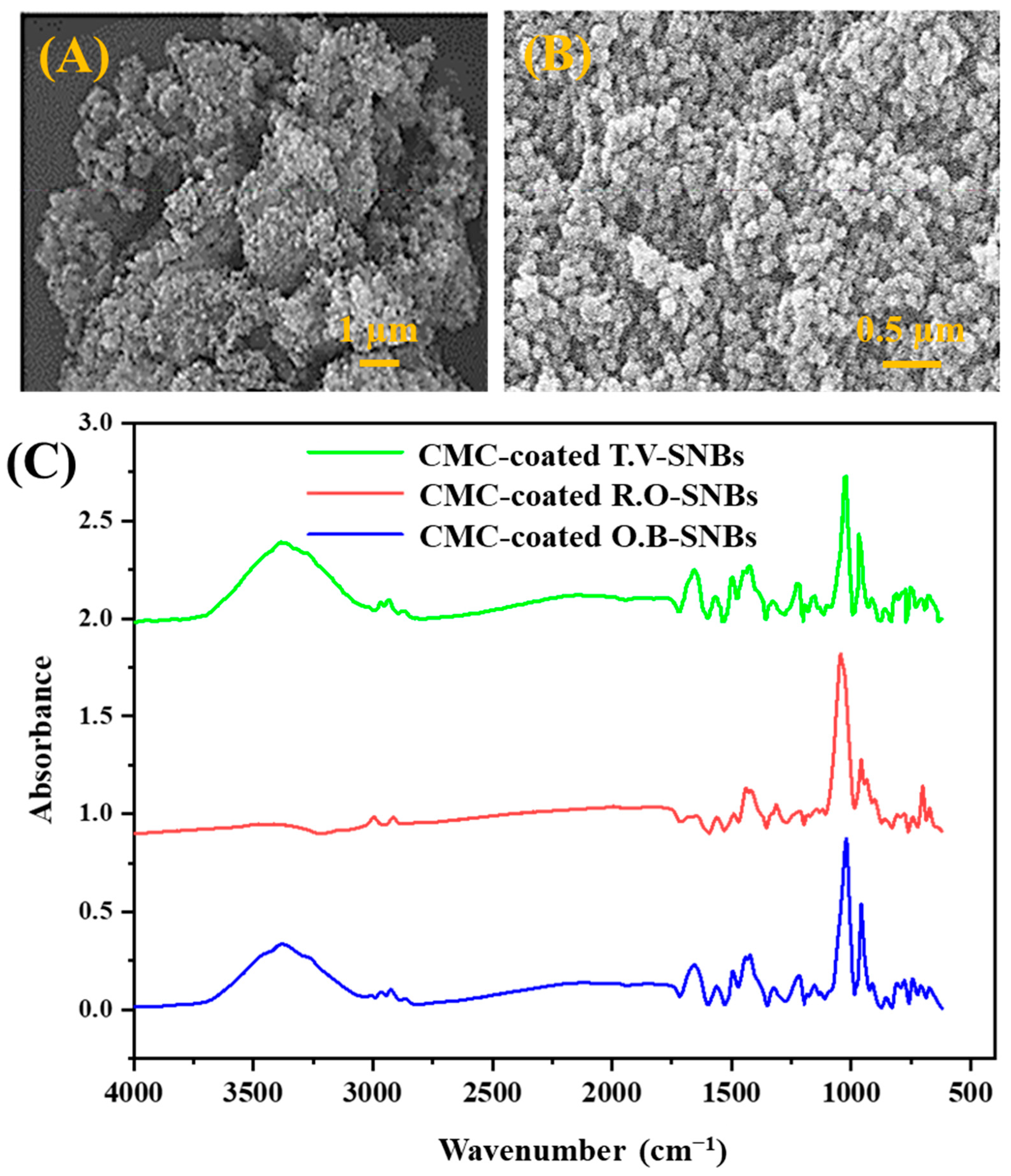
3.2. Structural Morphology of SNBs
3.3. Chemical Structure Analysis of SNBs
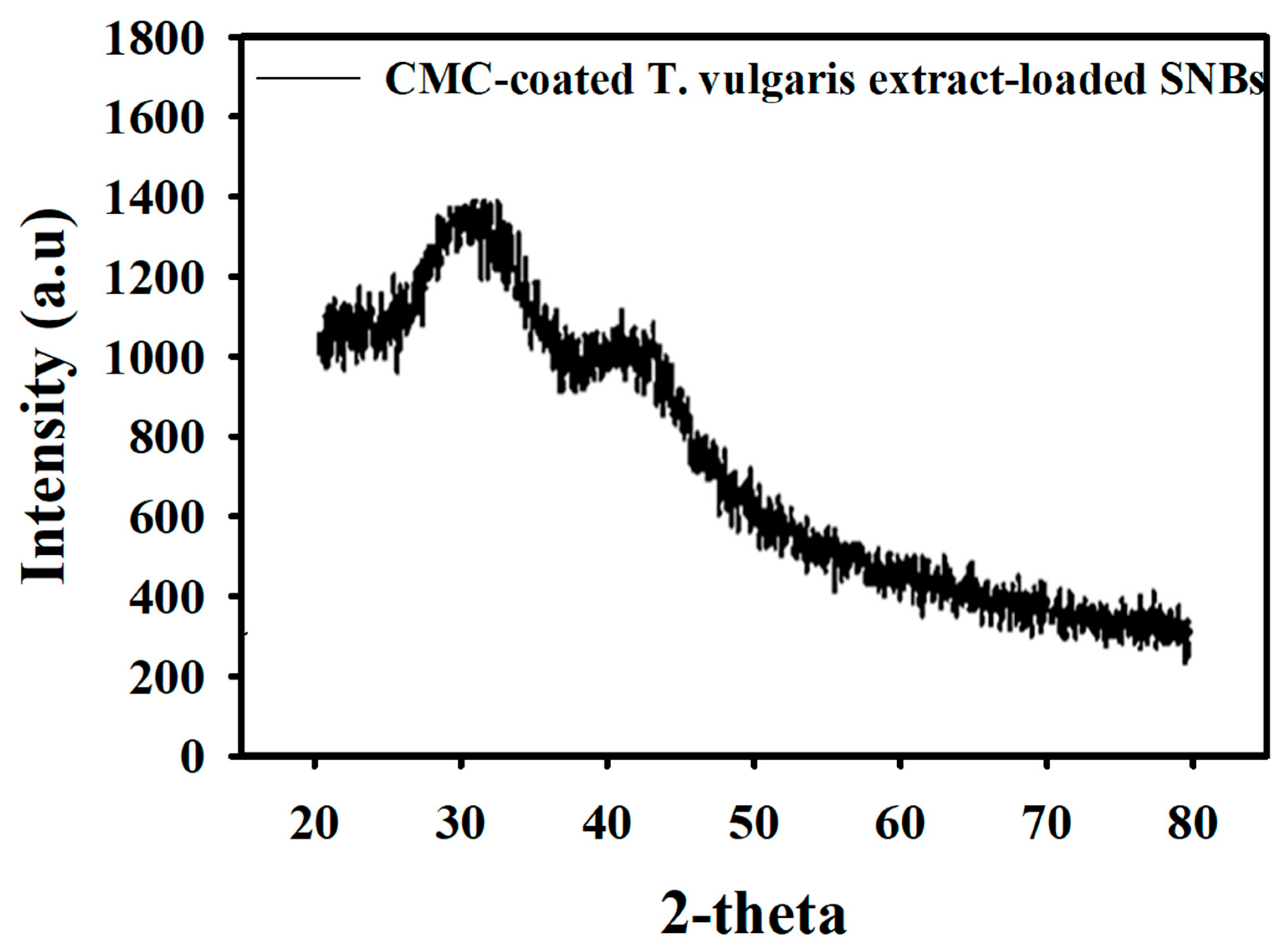
3.4. XRD Analysis of Particle Size of SNBs
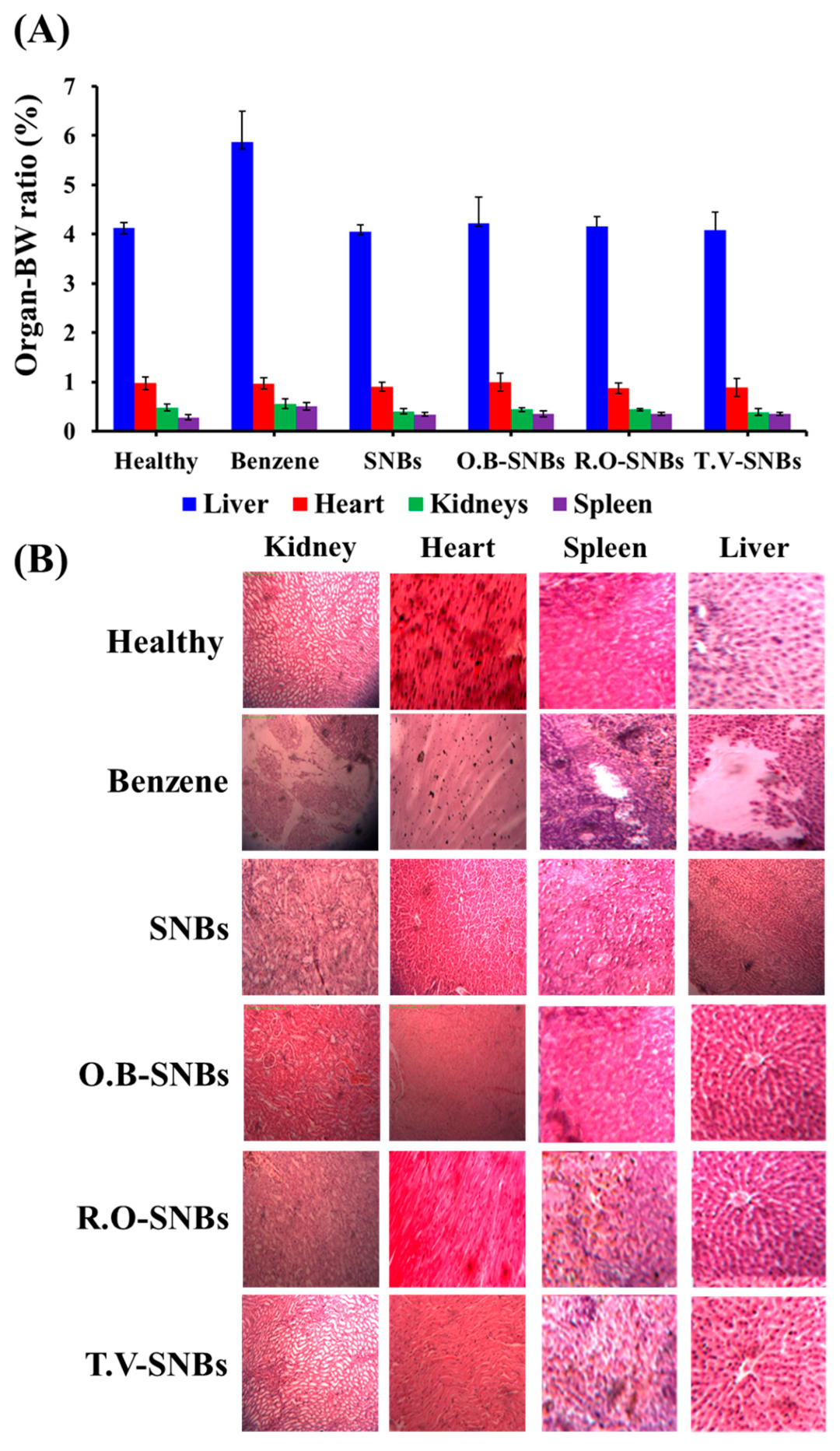
3.5. Relative Organ Weight Measurement
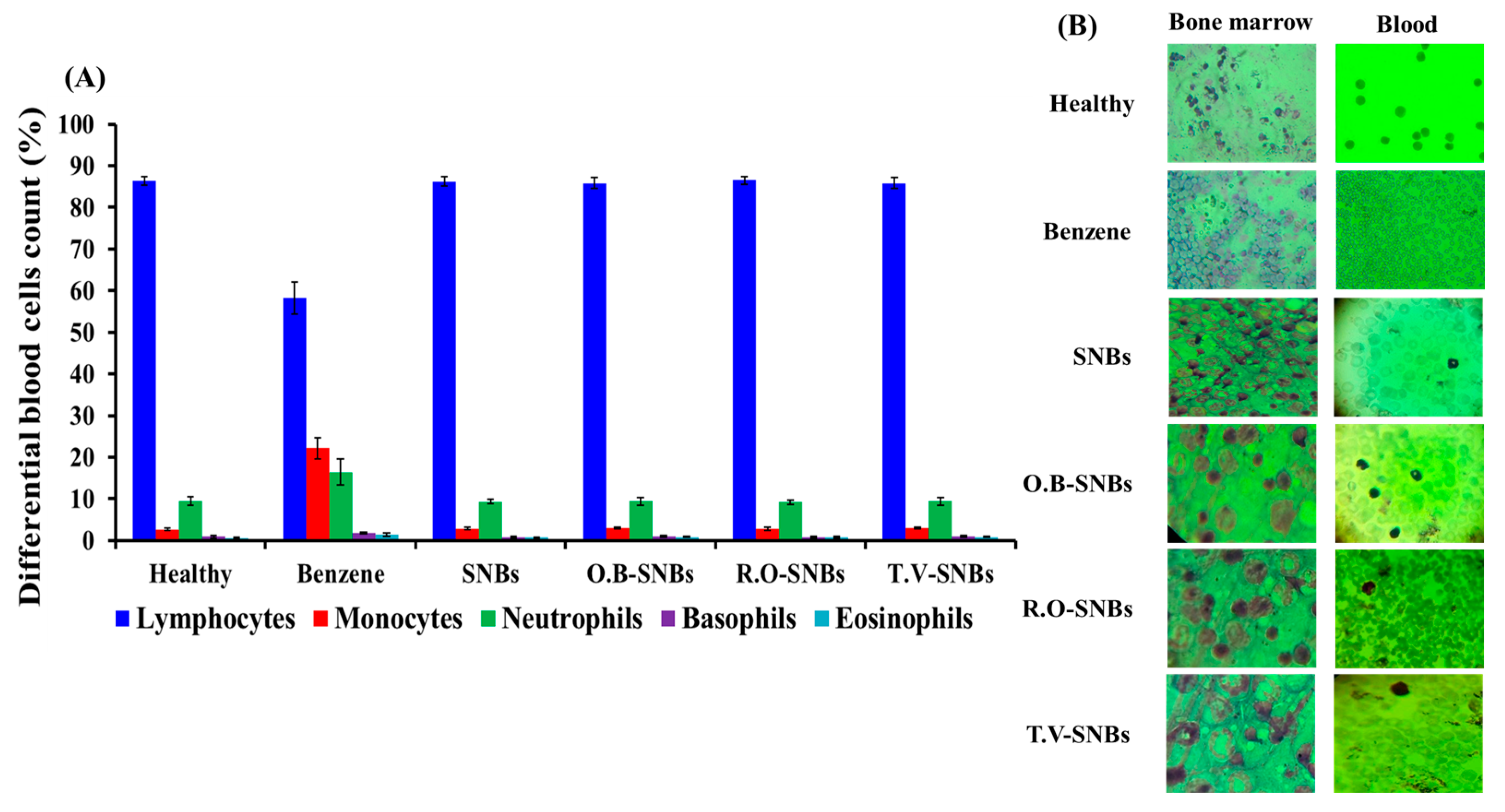
3.6. Differential Counting of Blood Cells
3.7. Microscopic Examination of Blood and Bone Marrow Cells
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yang, X.; Li, C.; Yu, G.; Sun, L.; Guo, S.; Sai, L.; Bo, C.; Xing, C.; Shao, H.; Peng, C.; et al. Ligand-independent activation of AhR by hydroquinone mediates benzene-induced hematopoietic toxicity. Chem. Biol. Interact. 2022, 355, 109845. [Google Scholar] [CrossRef]
- Newell, L.F.; Cook, R.J. Advances in acute myeloid leukemia. BMJ 2021, 375, n2026. [Google Scholar] [CrossRef]
- Bailly, C. Ready for a comeback of natural products in oncology. Biochem. Pharmacol. 2009, 77, 1447–1457. [Google Scholar] [CrossRef]
- Pan, M.-H.; Ho, C.-T. Chemopreventive effects of natural dietary compounds on cancer development. Chem. Soc. Rev. 2008, 37, 2558–2574. [Google Scholar] [CrossRef]
- Gutierrez, J.; Barry-Ryan, C.; Bourke, P. The antimicrobial efficacy of plant essential oil combinations and interactions with food ingredients. Int. J. Food Microbiol. 2008, 124, 91–97. [Google Scholar] [CrossRef]
- Dianová, L.; Tirpák, F.; Halo, M.; Slanina, T.; Massányi, M.; Stawarz, R.; Formicki, G.; Madeddu, R.; Massányi, P. Effects of Selected Metal Nanoparticles (Ag, ZnO, TiO2) on the Structure and Function of Reproductive Organs. Toxics 2022, 10, 459. [Google Scholar] [CrossRef]
- Shahcheraghi, N.; Golchin, H.; Sadri, Z.; Tabari, Y.; Borhanifar, F.; Makani, S. Nano-Biotechnology, an Applicable Approach for Sustainable Future. 3 Biotech 2022, 12, 65. [Google Scholar] [CrossRef]
- Mao, L.; Zheng, L.; You, H.; Ullah, M.W.; Cheng, H.; Guo, Q.; Zhu, Z.; Xi, Z.; Li, R. A Comparison of Hepatotoxicity Induced by Different Lengths of Tungsten Trioxide Nanorods and the Protective Effects of Melatonin in BALB/c Mice. Environ. Sci. Pollut. Res. 2021, 28, 40793–40807. [Google Scholar] [CrossRef]
- Allen, T.M.; Cullis, P.R. Drug Delivery Systems: Entering the Mainstream. Science 2004, 303, 1818–1822. [Google Scholar] [CrossRef]
- Li, S.; Jasim, A.; Zhao, W.; Fu, L.; Ullah, M.W.; Shi, Z.; Yang, G. Fabrication of pH-Electroactive Bacterial Cellulose/Polyaniline Hydrogel for the Development of a Controlled Drug Release System. ES Mater. Manuf. 2018, 1, 41–49. [Google Scholar] [CrossRef]
- Cho, K.; Wang, X.U.; Nie, S.; Chen, Z.; Shin, D.M. Therapeutic Nanoparticles for Drug Delivery in Cancer. Clin. Cancer Res. 2008, 14, 1310–1316. [Google Scholar] [CrossRef]
- Cho, M.; Cho, W.-S.; Choi, M.; Kim, S.J.; Han, B.S.; Kim, S.H.; Kim, H.O.; Sheen, Y.Y.; Jeong, J. The impact of size on tissue distribution and elimination by single intravenous injection of silica nanoparticles. Toxicol. Lett. 2009, 189, 177–183. [Google Scholar] [CrossRef]
- Ashley, C.E.; Carnes, E.C.; Phillips, G.K.; Padilla, D.; Durfee, P.N.; Brown, P.A.; Hanna, T.N.; Liu, J.; Phillips, B.; Carter, M.B.; et al. The targeted delivery of multicomponent cargos to cancer cells by nanoporous particle-supported lipid bilayers. Nat. Mater. 2011, 10, 389–397. [Google Scholar] [CrossRef]
- Manzano, M.; Vallet-Regí, M. Mesoporous silica nanoparticles for drug delivery. Adv. Funct. Mater. 2020, 30, 1902634. [Google Scholar] [CrossRef]
- Watermann, A.; Brieger, J. Mesoporous Silica Nanoparticles as Drug Delivery Vehicles in Cancer. Nanomaterials 2017, 7, 189. [Google Scholar] [CrossRef]
- Li, L.; Tang, F.; Liu, H.; Liu, T.; Hao, N.; Chen, D.; Teng, X.; He, J. In Vivo Delivery of Silica Nanorattle Encapsulated Docetaxel for Liver Cancer Therapy with Low Toxicity and High Efficacy. ACS Nano 2010, 4, 6874–6882. [Google Scholar] [CrossRef]
- Sang, H.; Mao, C.; Wu, Y.; Wei, Y. Study on the Effect of Gamma-Ray Irradiation on the Adsorption of 99Tc and Re by a Silica-Based Pyridine Resin. Toxics 2022, 10, 638. [Google Scholar] [CrossRef]
- Siddiqui, B.; Rehman, A.; Haq, I.-U.; Al-Dossary, A.A.; Elaissari, A.; Ahmed, N. Exploiting recent trends for the synthesis and surface functionalization of mesoporous silica nanoparticles towards biomedical applications. Int. J. Pharm. X 2022, 4, 100116. [Google Scholar] [CrossRef]
- Morimoto, K.; Wolff, S. Increase of sister chromatid exchanges and perturbations of cell division kinetics in human lymphocytes by benzene metabolites. Cancer Res. 1980, 40, 1189–1193. [Google Scholar]
- Asami, D.K.; Hong, Y.-J.; Barrett, D.M.; Mitchell, A.E. Comparison of the Total Phenolic and Ascorbic Acid Content of Freeze-Dried and Air-Dried Marionberry, Strawberry, and Corn Grown Using Conventional, Organic, and Sustainable Agricultural Practices. J. Agric. Food Chem. 2003, 51, 1237–1241. [Google Scholar] [CrossRef]
- Laurindo, L.F.; de Maio, M.C.; Minniti, G.; de Góes Corrêa, N.; Barbalho, S.M.; Quesada, K.; Guiguer, E.L.; Sloan, K.P.; Detregiachi, C.R.P.; Araújo, A.C.; et al. Effects of Medicinal Plants and Phytochemicals in Nrf2 Pathways during Inflammatory Bowel Diseases and Related Colorectal Cancer: A Comprehensive Review. Metabolites 2023, 13, 243. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, A.M.E.; Xiao, L.; Ullah, M.W.; Yu, M.; Ouyang, C.; Yang, G. Current Challenges of Cancer Anti-angiogenic Therapy and the Promise of Nanotherapeutics. Theranostics 2018, 8, 533–548. [Google Scholar] [CrossRef] [PubMed]
- Chiang, L.-C.; Ng, L.-T.; Cheng, P.-W.; Chiang, W.; Lin, C.-C. Antiviral Activities of Extracts and Selected Pure Constituents of Ocimum basilicum. Clin. Exp. Pharmacol. Physiol. 2005, 32, 811–816. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.I.; Anwar, F.; Sherazi, S.T.H.; Przybylski, R. Chemical Composition, Antioxidant and Antimicrobial Activities of Basil (Ocimum basilicum) Essential Oils Depends on Seasonal Variations. Food Chem. 2008, 108, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Mukhopadhyay, M.K.; Ghosh, P.D.; Nath, D. Effect of Methanolic Leaf Extract of Ocimum basilicum L. on Benzene-Induced Hematotoxicity in Mice. Evid.-Based Complement. Altern. Med. 2012, 2012, 176385. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, X.; Li, P.-Z.; Nguyen, K.T.; Wang, X.-J.; Luo, Z.; Zhang, H.; Tan, N.S.; Zhao, Y. Biocompatible, Uniform, and Redispersible Mesoporous Silica Nanoparticles for Cancer-Targeted Drug Delivery In Vivo. Adv. Funct. Mater. 2014, 24, 2450–2461. [Google Scholar] [CrossRef]
- Nieto, G. Biological Activities of Three Essential Oils of the Lamiaceae Family. Medicines 2017, 4, 63. [Google Scholar] [CrossRef]
- Slowing, I.I.; Vivero-Escoto, J.L.; Trewyn, B.G.; Lin, V.S.-Y. Mesoporous silica Nanoparticles: Structural Design and Applications. J. Mater. Chem. 2010, 20, 7924–7937. [Google Scholar] [CrossRef]
- Singletary, K.; MacDonald, C.; Wallig, M. Inhibition by Rosemary and Carnosol of 7,12-Dimethylbenz [a] Anthracene (DMBA)-Induced Rat Mammary Tumorigenesis and in Vivo DMBA-DNA Adduct Formation. Cancer Lett. 1996, 104, 43–48. [Google Scholar] [CrossRef]
- Rustaiyan, A.; Masoudi, S.; Monfared, A.; Kamalinejad, M.; Lajevardi, T.; Sedaghat, S.; Yari, M. Volatile Constituents of Three Thymus Species Grown Wild in Iran. Planta Medica 2000, 66, 197–198. [Google Scholar] [CrossRef]
- Lee, S.J.; Umano, K.; Shibamoto, T.; Lee, K.G. Identification of volatile components in basil (Ocimum basilicum L.) and thyme leaves (Thymus vulgaris L.) and their antioxidant properties. Food Chem. 2005, 91, 131–137. [Google Scholar] [CrossRef]
- El-Nekeety, A.A.; Mohamed, S.R.; Hathout, A.S.; Hassan, N.S.; Aly, S.E.; Abdel-Wahhab, M.A. Antioxidant properties of Thymus vulgaris oil against aflatoxin-induce oxidative stress in male rats. Toxicon 2011, 57, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Horvathova, E.; Turcaniova, V.; Slamenova, D. Comparative study of DNA-damaging and DNA-protective effects of selected components of essential plant oils in human leukemic cells K562. Neoplasma 2007, 54, 478. [Google Scholar]
- Smith, M.T.; Zhang, L.; Jeng, M.; Wang, Y.; Guo, W.; Duramad, P.; Hubbard, A.E.; Hofstadler, G.; Holland, N.T. Hydroquinone, a Benzene Metabolite, Increases the Level of Aneusomy of Chromosomes 7 and 8 in Human CD34-Positive Blood Progenitor Cells. Carcinogenesis 2000, 21, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, A.T.; Betti, C.J.; Villalobos, M.J.; Premkumar, K.; Cline, E.; Jiang, Q.; Diaz, M.O. Surviving apoptosis: A possible mechanism of benzene-induced leukemia. Chem. Biol. Interact. 2005, 153, 179–185. [Google Scholar] [CrossRef]
- Panday, R.; Poudel, A.J.; Li, X.; Adhikari, M.; Ullah, M.W.; Yang, G. Amphiphilic core-shell nanoparticles: Synthesis, biophysical properties, and applications. Colloids Surf. B Biointerfaces 2018, 172, 68–81. [Google Scholar] [CrossRef]
- Li, X.; Ji, X.; Chen, K.; Ullah, M.W.; Yuan, X.; Lei, Z.; Cao, J.; Xiao, J.; Yang, G. Development of finasteride/PHBV@polyvinyl alcohol/chitosan reservoir-type microspheres as a potential embolic agent: From in vitro evaluation to animal study. Biomater. Sci. 2020, 8, 2797–2813. [Google Scholar] [CrossRef]
- Li, X.; Li, B.; Ullah, M.W.; Panday, R.; Cao, J.; Li, Q.; Zhang, Y.; Wang, L.; Yang, G. Water-Stable and Finasteride-Loaded Polyvinyl Alcohol Nanofibrous Particles with Sustained Drug Release for Improved Prostatic Artery Embolization—In vitro and in vivo evaluation. Mater. Sci. Eng. C 2020, 115, 111107. [Google Scholar] [CrossRef]
- Li, X.; Ji, X.; Chen, K.; Ullah, M.W.; Li, B.; Cao, J.; Xiao, L.; Xiao, J.; Yang, G. Immobilized Thrombin on X-ray Radiopaque Polyvinyl Alcohol/Chitosan Embolic Microspheres for Precise Localization and Topical Blood Coagulation. Bioact. Mater. 2021, 6, 2105–2119. [Google Scholar] [CrossRef]
- Ullah, M.W.; Manan, S.; Khattak, W.A.; Shahzad, A.; Ul-Islam, M.; Yang, G. Biotemplate-Mediated Green Synthesis and Applications of Nanomaterials. Curr. Pharm. Des. 2020, 26, 5819–5836. [Google Scholar] [CrossRef]
- Mondal, A.; Mishra, S. Silica Nanoparticles: Synthesis and Functionalization for Drug Delivery Application. Ph.D. Thesis, National Institute of Technology, Rourkela, India, 2014. [Google Scholar]
- Kim, J.W.; Kim, L.U.; Kim, C.K. Size Control of Silica Nanoparticles and Their Surface Treatment for Fabrication of Dental Nanocomposites. Biomacromolecules 2007, 8, 215–222. [Google Scholar] [CrossRef]
- Kim, T.G.; An, G.S.; Han, J.S.; Hur, J.U.; Park, B.G.; Choi, S.-C.; Kim, T.G.; An, G.S.; Han, J.S.; Hur, J.U. Synthesis of Size Controlled Spherical Silica Nanoparticles via Sol-Gel Process within Hydrophilic Solvent. J. Korean Ceram. Soc. 2017, 54, 49–54. [Google Scholar] [CrossRef]
- Lu, J.; Liong, M.; Li, Z.; Zink, J.I.; Tamanoi, F. Biocompatibility, Biodistribution, and Drug-Delivery Efficiency of Mesoporous Silica Nanoparticles for Cancer Therapy in Animals. Small 2010, 6, 1794–1805. [Google Scholar] [CrossRef] [PubMed]
- Mabasa, X.E.; Mathomu, L.M.; Madala, N.E.; Musie, E.M.; Sigidi, M.T. Molecular Spectroscopic (FTIR and UV-Vis) and Hyphenated Chromatographic (UHPLC-qTOF-MS) Analysis and in Vitro Bioactivities of the Momordica Balsamina Leaf Extract. Biochem. Res. Int. 2021, 2021, 2854217. [Google Scholar] [CrossRef] [PubMed]
- Alara, O.R.; Abdurahman, N.H.; Mudalip, S.K.A.; Olalere, O.A. Characterization and Effect of Extraction Solvents on the Yield and Total Phenolic Content from Vernonia amygdalina Leaves. J. Food Meas. Charact. 2018, 12, 311–316. [Google Scholar] [CrossRef]
- Slowing, I.I.; Vivero-Escoto, J.L.; Wu, C.-W.; Lin, V.S.-Y. Mesoporous Silica Nanoparticles as Controlled Release Drug Delivery and Gene Transfection Carriers. Adv. Drug Deliv. Rev. 2008, 60, 1278–1288. [Google Scholar] [CrossRef] [PubMed]
- Božanić, D.K.; Djoković, V.; Blanuša, J.; Nair, P.S.; Georges, M.K.; Radhakrishnan, T. Preparation and Properties of Nano-Sized Ag and Ag2S Particles in Biopolymer Matrix. Eur. Phys. J. E 2007, 22, 51–59. [Google Scholar] [CrossRef]
- Mussai, F.; De Santo, C.; Abu-Dayyeh, I.; Booth, S.; Quek, L.; McEwen-Smith, R.M.; Qureshi, A.; Dazzi, F.; Vyas, P.; Cerundolo, V. Acute myeloid leukemia creates an arginase-dependent immunosuppressive microenvironment. Blood J. Am. Soc. Hematol. 2013, 122, 749–758. [Google Scholar] [CrossRef]
- Snyder, R. Leukemia and Benzene. Int. J. Environ. Res. Public Health 2012, 9, 2875–2893. [Google Scholar] [CrossRef]
- Rehan, T.; MacEwan, D.; Shah, N.; Rehan, T.; Tahira, R.; Murad, S.; Anees, M.; Murtaza, I.; Farman, M.; Abid, O.-U.; et al. Apoptosis of Leukemia Cells by Ocimum basilicum Fractions Following TNF alpha Induced Activation of JNK and Caspase 3. Curr. Pharm. Des. 2019, 25, 3681–3691. [Google Scholar] [CrossRef]
- Shay, J.; Elbaz, H.A.; Lee, I.; Zielske, S.P.; Malek, M.H.; Hüttemann, M. Molecular Mechanisms and Therapeutic Effects of (-)-Epicatechin and Other Polyphenols in Cancer, Inflammation, Diabetes, and Neurodegeneration. Oxidative Med. Cell. Longev. 2015, 2015, 181260. [Google Scholar] [CrossRef] [PubMed]
- Tousian, B.; Ghasemi, M.H.; Khosravi, A.R. Targeted Chitosan Nanoparticles Embedded into Graphene Oxide Functionalized with Caffeic Acid as a Potential Drug Delivery System: New Insight into Cancer Therapy. Int. J. Biol. Macromol. 2022, 222, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ullah, M.W.; Siddique, R.; Liu, Y.; Ullah, I.; Xue, M.; Yang, G.; Hou, H. Catechins-Modified Selenium-Doped Hydroxyapatite Nanomaterials for Improved Osteosarcoma Therapy Through Generation of Reactive Oxygen Species. Front. Oncol. 2019, 9, 499. [Google Scholar] [CrossRef] [PubMed]
- Golmohammadi, M.; Elmaghraby, D.A.; Ramírez-Coronel, A.A.; Rakhimov, N.; Mohammed, S.S.; Romero-Parra, R.M.; Jawad, M.A.; Zamanian, M.Y.; Soltani, A.; Taheri, N.; et al. A Comprehensive View on the Quercetin Impact on Bladder Cancer: Focusing on Oxidative Stress, Cellular, and Molecular Mechanisms. Fundam. Clin. Pharmacol. 2023, 37, 900–909. [Google Scholar] [CrossRef]
- Feng, L.; Cheng, J.; Su, W.; Li, H.; Xiao, T.; Chen, D.; Zhang, Z. Cinnamic Acid Hybrids as Anticancer Agents: A Mini-review. Arch. Pharm. 2022, 355, e2200052. [Google Scholar] [CrossRef] [PubMed]

| Fraction | Compounds | MS (m/z) | Other Fragment Ions | UV Maxima (nm) |
|---|---|---|---|---|
| RF1 | (-) Epicatechin derivative | 922.1 | 707.3, 365.6, 187.6, 129.1 | 240, 320 |
| Caffeic acid-3-glucoside (Dimer) | 683.1 | 341.5 | 242, 330 | |
| RF2 | D-Alanine, N-(2,5-ditrifluoromethylbenzoyl), nonadecyl ester | 545.0 | 507.2, 425.9 | 280, 330 |
| Rosemarinic acid | 553.2 | 187.8 | 265, 330 | |
| TF2 | Trans-3-trifluoromethyl cinamic acid, 3-4-dichlorophenyl ester (Dimer) | 719.4 | 360 | 230, 322 |
| Thymol | 756.7 | 361.4, 856.7 | 280, 322 | |
| TF7 | Kaempferol-3-o-alpha-l-rhamopyranosyl-(1-6)-beta-d-galactopyranosyl]7-o-alpha-l-rhamanopyranoside (flavonoid) | 945.1 | 470.5, 407.5 | 262 |
| Carvecrol | 956.0 | 391.1, 203.8 | 260, 290, 330 | |
| Succinic acid, 3,5-dichlorophenyl hexadecyl ester | 956.2 | 486.5, 263.0 | 230, 280 | |
| TF8 | Trans-3-trifluoromethyl cinamic acid, 3-4-dichlorophenyl ester (Dimer) | 719.4 | 360 | 220, 320 |
| Trans-3-trifluoromethyl cinamic acid, 3-4-dichlorophenyl ester derivative | 756.7 | 361.4, 856.7 | 270, 325 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rehan, T.; Tahir, A.; Sultan, A.; Alabbosh, K.F.; Waseem, S.; Ul-Islam, M.; Khan, K.A.; Ibrahim, E.H.; Ullah, M.W.; Shah, N. Mitigation of Benzene-Induced Haematotoxicity in Sprague Dawley Rats through Plant-Extract-Loaded Silica Nanobeads. Toxics 2023, 11, 865. https://doi.org/10.3390/toxics11100865
Rehan T, Tahir A, Sultan A, Alabbosh KF, Waseem S, Ul-Islam M, Khan KA, Ibrahim EH, Ullah MW, Shah N. Mitigation of Benzene-Induced Haematotoxicity in Sprague Dawley Rats through Plant-Extract-Loaded Silica Nanobeads. Toxics. 2023; 11(10):865. https://doi.org/10.3390/toxics11100865
Chicago/Turabian StyleRehan, Touseef, Anum Tahir, Aneesa Sultan, Khulood Fahad Alabbosh, Shahid Waseem, Mazhar Ul-Islam, Khalid Ali Khan, Essam H. Ibrahim, Muhammad Wajid Ullah, and Nasrullah Shah. 2023. "Mitigation of Benzene-Induced Haematotoxicity in Sprague Dawley Rats through Plant-Extract-Loaded Silica Nanobeads" Toxics 11, no. 10: 865. https://doi.org/10.3390/toxics11100865
APA StyleRehan, T., Tahir, A., Sultan, A., Alabbosh, K. F., Waseem, S., Ul-Islam, M., Khan, K. A., Ibrahim, E. H., Ullah, M. W., & Shah, N. (2023). Mitigation of Benzene-Induced Haematotoxicity in Sprague Dawley Rats through Plant-Extract-Loaded Silica Nanobeads. Toxics, 11(10), 865. https://doi.org/10.3390/toxics11100865









