Association of Air Pollution with the Number of Common Respiratory Visits in Children in a Heavily Polluted Central City, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Source of Data
2.2. Methods
2.2.1. Processing of Data
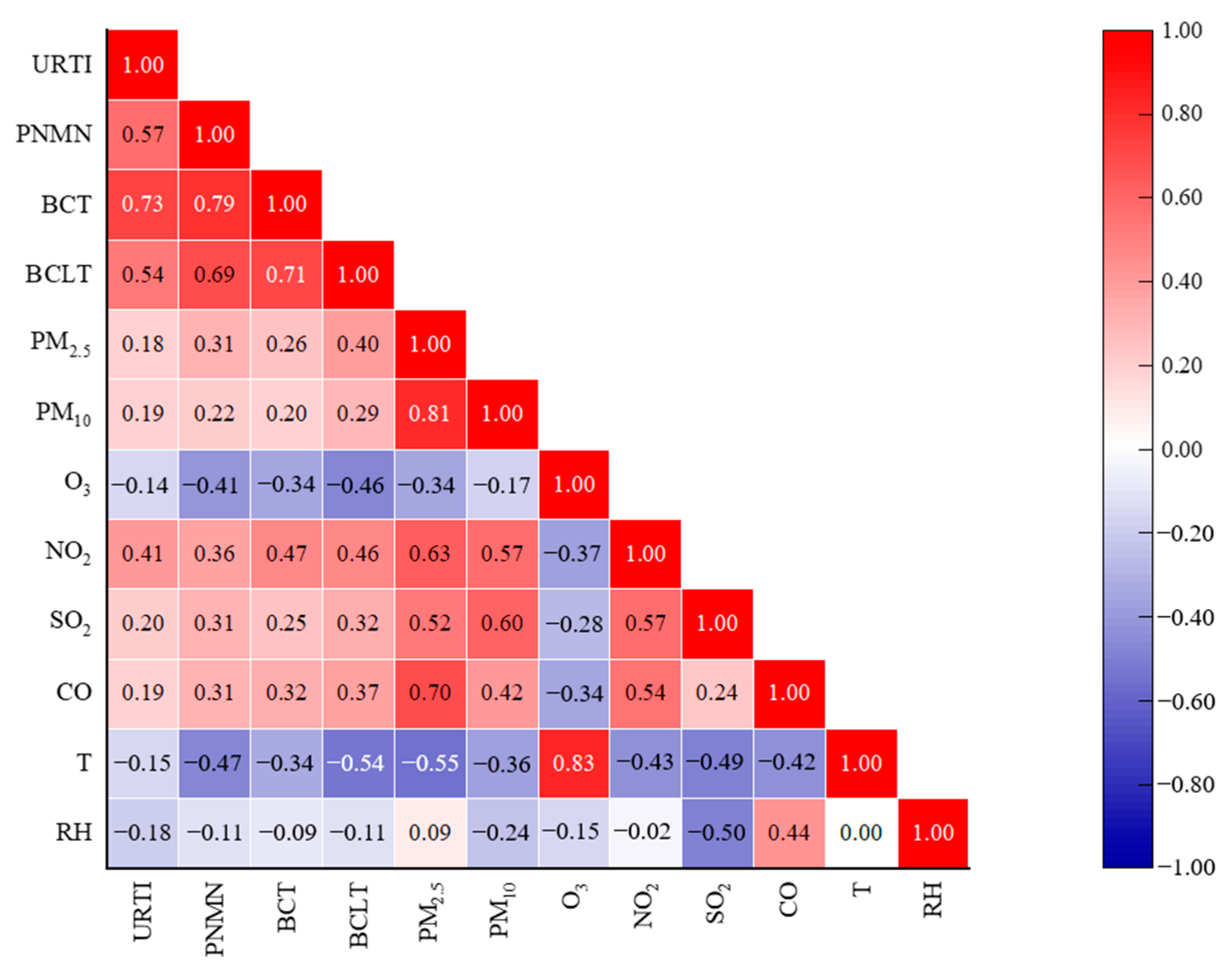
2.2.2. Spearman Correlation Analysis
2.2.3. Generalized Additive Model (GAM)
3. Results and Discussion
3.1. Spearman Correlation Analysis
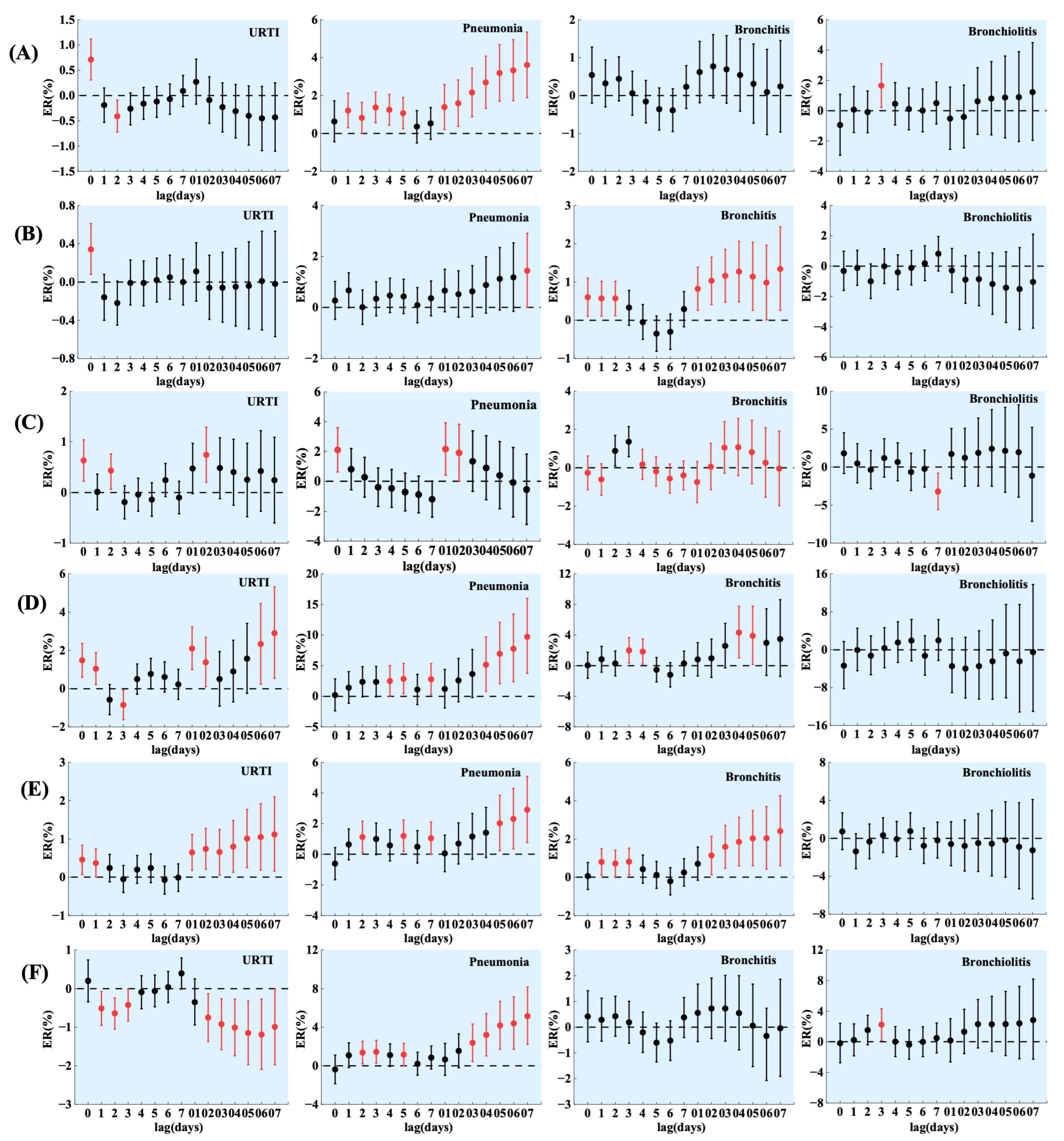
3.2. GAM of Single Pollutants
3.3. Stratified Analysis
3.3.1. Sex-Stratified Analysis
3.3.2. Age-Stratified Analysis
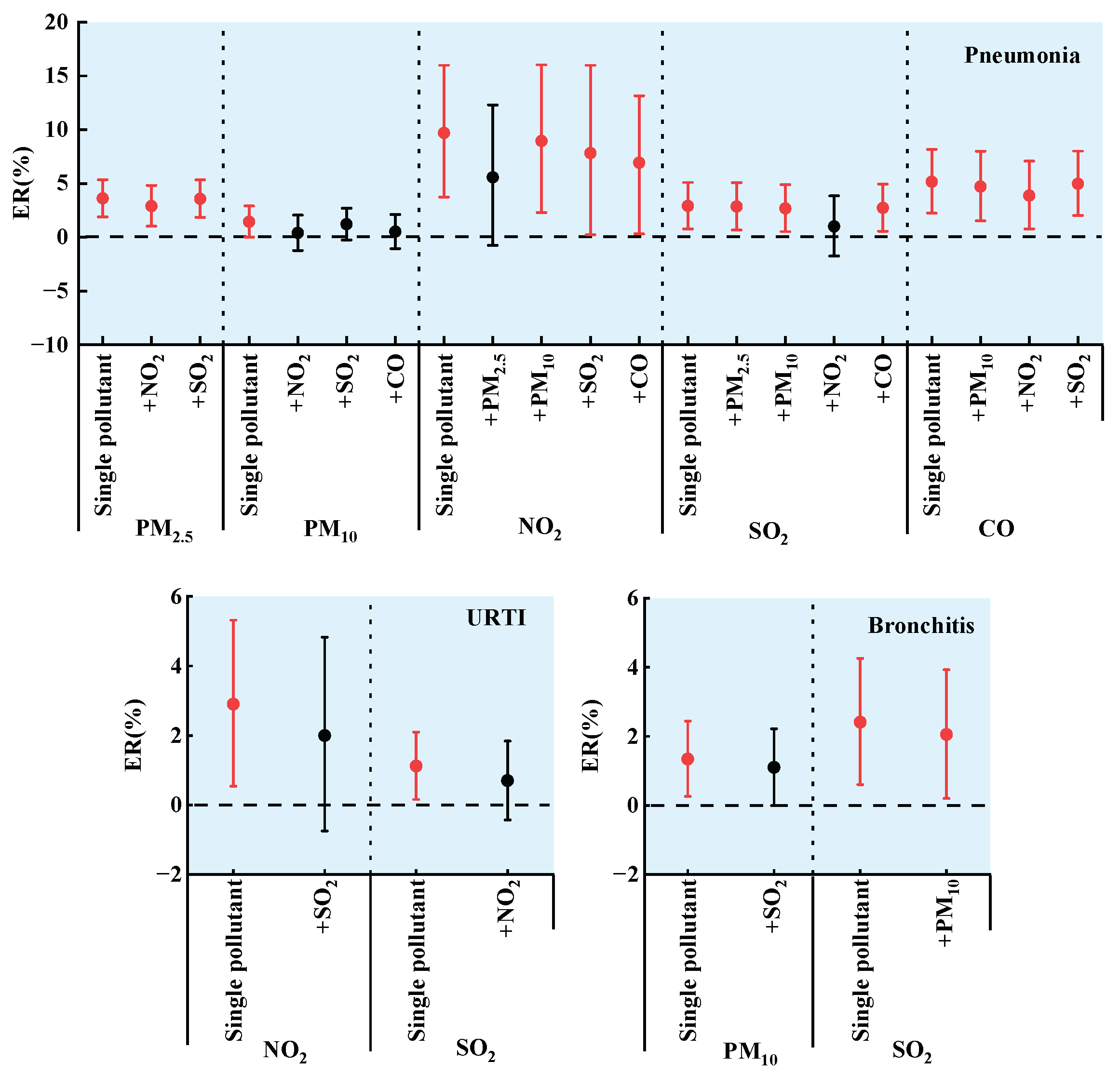
3.4. GAM of Two Pollutants
4. Conclusions
- (1)
- The number of visits for URTI, PNMN, BCT, and BCLT in children was positively correlated with PM2.5, PM10, NO2, SO2, and CO. Conversely, it was negatively correlated with temperature and relative humidity.
- (2)
- The number of URTI, PNMN, BCT, and BCLT visits in children was significantly affected by a variety of air pollutants, with a lag effect. On the day of the strongest effect, NO2 and SO2 had a greater effect on the number of URTI and BCT visits in children; NO2, SO2, and CO had a more pronounced effect on the number of PNMN visits in children; and CO had a greater effect on the number of BCLT visits in children.
- (3)
- The number of URTI, PNMN, BCT, and BCLT visits in children of different ages was affected differently by air pollutants. There were no significant sex differences in the number of URTI and PNMN visits in children affected by air pollutants. However, the number of BCT and BCLT visits in boys was more likely to be affected by air pollutants compared to girls.
- (4)
- The effects of pollutants on the number of common respiratory visits in children differed between the two-pollutant GAM and a single pollutant. Additionally, there may be complex interactions between different air pollutants.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- An, R.P.; Ji, M.M.; Yan, H.; Guan, C.H. Impact of ambient air pollution on obesity: A systematic review. Int. J. Obes. 2018, 42, 1112–1126. [Google Scholar] [CrossRef]
- Ambient (Outdoor) Air Pollution. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 1 August 2023).
- Chang, J.; Liu, W.; Huang, C. Residential ambient traffic in relation to childhood pneumonia among urban children in Shandong, China: A cross-sectional study. Int. J. Environ. Res. Public Health 2018, 15, 1076. [Google Scholar] [CrossRef] [PubMed]
- Almetwally, A.A.; Bin-Jumah, M.; Allam, A.A. Ambient air pollution and its influence on human health and welfare: An overview. Environ. Sci. Pollut. Res. 2020, 27, 24815–24830. [Google Scholar] [CrossRef] [PubMed]
- Li, D.Y. Research on the mechanisms underlying the effects of atmospheric environmental pollution on sports people. Fresenius Environ. Bull. 2021, 30, 1732–1739. [Google Scholar]
- Chang, Q.; Liu, S.; Chen, Z.; Chen, Z.J.; Zu, B.; Zhang, H.H. Association between air pollutants and outpatient and emergency hospital visits for childhood asthma in Shenyang city of China. Int. J. Biometeorol. 2020, 64, 1539–1548. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Kang, S.L.; Lin, X.; Zhang, X.Y. Impact of air pollutants on hospital visits for pediatric asthma in Fuzhou city, southeast China. Environ. Sci. Pollut. Res. 2020, 29, 58664–58674. [Google Scholar] [CrossRef]
- Hu, F.P.; Guo, Y.M. Health impacts of air pollution in China. Front. Environ. Sci. Eng. 2021, 15, 74. [Google Scholar] [CrossRef]
- Gheissari, R.; Liao, J.W.; Garcia, E.; Pavlovic, N.; Gilliland, F.D.; Xiang, A.H.; Chen, Z.H. Health outcomes in children associated with prenatal and early-life exposures to air pollution: A narrative review. Toxics 2022, 10, 458. [Google Scholar] [CrossRef]
- Armas, F.V.; D’Angiulli, A. Neuroinflammation and neurodegeneration of the central nervous system from air pollutants: A scoping review. Toxics 2022, 10, 666. [Google Scholar] [CrossRef]
- Wang, Q.N.; Chen, Z.; Huang, W.; Kou, B.; Li, J.W. Short-term effect of moderate level air pollution on outpatient visits for multiple clinic departments: A time-series analysis in Xi’an China. Toxics 2023, 11, 166. [Google Scholar] [CrossRef]
- Jarernwong, K.; Gheewala, S.H.; Sampattagul, S. Health impact related to ambient particulate matter exposure as a spatial health risk map case study in Chiang Mai, Thailand. Atmosphere 2023, 14, 261. [Google Scholar] [CrossRef]
- Pyo, J.S.; Kim, N.Y.; Kang, D.W. Impacts of outdoor particulate matter exposure on the incidence of lung cancer and mortality. Medicina 2022, 58, 1159. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Pizzol, M.; Jacobsen, J.B.; Xu, L.Y. Contingent valuation of health and mood impacts of PM2.5 in Beijing, China. Sci. Total Environ. 2018, 630, 1269–1282. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.W.; Kang, S.C.; Kim, S.Y.; Cho, Y.J.; Hwang, S. Long-term exposure to PM10 increases lung cancer risks: A cohort analysis. Cancer Res. Treat. 2022, 54, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Dedele, A.; Miskinyte, A.; Grazuleviciene, R. The impact of particulate matter on allergy risk among adults: Integrated exposure assessment. Environ. Sci. Pollut. Res. 2019, 26, 10070–10082. [Google Scholar] [CrossRef]
- Samoli, E.; Aga, E.; Touloumi, G.; Nislotis, K.; Forsberg, B.; Lefranc, A.; Pekkanen, J.; Wojtyniak, B.; Schindler, C.; Niciu, E.; et al. Short-term effects of nitrogen dioxide on mortality: An analysis within the APHEA project. Eur. Respir. J. 2006, 27, 1129–1137. [Google Scholar] [CrossRef]
- Li, Y.L.; Chuang, T.W.; Chang, P.Y.; Lin, L.Y.; Su, C.T.; Chien, L.N.; Chiou, H.Y. Long-term exposure to ozone and sulfur dioxide increases the incidence of type 2 diabetes mellitus among aged 30 to 50 adult population. Environ. Res. 2021, 194, 110624. [Google Scholar] [CrossRef]
- Abulude, F.; Abulude, I.; Oluwagbayide, S.; Afolayan, S.; Ishaku, D. Air Quality Index: A case of 1-day monitoring in 253 Nigerian urban and suburban towns. J. Geovis. Spat. Anal. 2022, 6, 5. [Google Scholar] [CrossRef]
- Gryech, I.; Ghogho, M.; Mahraoui, C.; Kobbane, A. An exploration of features impacting respiratory diseases in urban areas. Int. J. Environ. Res. Public Health 2022, 19, 3095. [Google Scholar] [CrossRef]
- Chen, Z.; Salam, M.T.; Eckel, S.P.; Breton, C.V.; Gilliland, F.D. Chronic effects of air pollution on respiratory health in southern California children: Findings from the southern California children’s health study. J. Thorac. Dis. 2015, 7, 46–58. [Google Scholar]
- Mo, Z.; Fu, Q.L.; Zhang, L.F.; Lyu, D.N.; Mao, G.M.; Wu, L.Z.; Xu, P.W.; Wang, Z.F.; Pan, X.J.; Chen, Z.J.; et al. Acute effects of air pollution on respiratory disease mortalities and outpatients in southeastern China. Sci. Rep. 2018, 8, 3461. [Google Scholar] [CrossRef] [PubMed]
- Dondi, A.; Carbone, C.; Manieri, E.; Zama, D.; Del Bono, C.; Betti, L.; Biagi, C.; Lanari, M. Outdoor air pollution and childhood respiratory disease: The role of oxidative stress. Int. J. Mol. Sci. 2023, 24, 4345. [Google Scholar] [CrossRef] [PubMed]
- Feng, G.S.; Zeng, Y.P.; Tian, J.; Wang, X.Y.; Tai, J.; Song, F.; Zhang, X.; Xu, X.; Chen, J.; Shi, T.L.; et al. Disease spectrum analysis of hospitalized children in China: A study of 18 tertiary children’s hospitals. Pediat. Investig. 2019, 3, 159–164. [Google Scholar] [CrossRef]
- Xiao, Q.Y.; Liu, Y.; Mulholland, J.A.; Russell, A.G.; Darrow, L.A.; Tolbert, P.E.; Strickland, M.J. Pediatric emergency department visits and ambient air pollution in the US state of Georgia: A case-crossover study. Environ. Health 2016, 15, 115. [Google Scholar] [CrossRef]
- Zar, H.J.; Ferkol, T.W. The global burden of respiratory disease-impact on child health. Pediatr. Pulmonol. 2014, 49, 430–434. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Yan, C.; Li, M.; Zhao, L.; Long, Z.; Fan, Y.; Zhang, Z.; Chen, R.; Huang, Y.; Lu, C.; et al. Short term effects of air pollutants on hospital admissions for respiratory diseases among children: A multi-city time-series study in China. Int. J. Hyg. Environ. Health 2021, 231, 113638. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.Y.; You, C.M.; Zhang, X.; Wang, X.J.; Xiao, D.X.; He, S.; Wu, F.; Meng, Q. Three exposure metrics of size-specific particulate matter associated with acute lower respiratory infection hospitalization in children: A multi-city time-series analysis in China. Sci. Total Environ. 2022, 816, 151636. [Google Scholar] [CrossRef]
- Luong, L.M.T.; Phung, D.; Dang, T.N.; Sly, P.D.; Morawska, L.; Thai, P.K. Seasonal association between ambient ozone and hospital admission for respiratory diseases in Hanoi, Vietnam. PLoS ONE 2018, 13, e0203751. [Google Scholar] [CrossRef]
- Janke, K. Air pollution, avoidance behaviour and children’s respiratory health: Evidence from England. J. Health Econ. 2014, 38, 23–42. [Google Scholar] [CrossRef]
- Cheng, C.Y.; Tseng, Y.L.; Huang, K.C.; Chiu, I.M.; Pan, H.Y.; Cheng, F.J. Association between ambient air pollution and emergency room visits for pediatric respiratory diseases: The impact of COVID-19 pandemic. Toxics 2022, 10, 247. [Google Scholar] [CrossRef]
- Chen, S.J.; Wu, S.Z. Deep learning for identifying environmental risk factors of acute respiratory diseases in Beijing, China: Implications for population with different age and gender. Int. J. Environ. Health Res. 2020, 30, 435–446. [Google Scholar] [CrossRef] [PubMed]
- Vanos, J.K.; Hebbern, C.; Cakmak, S. Risk assessment for cardiovascular and respiratory mortality due to air pollution and synoptic meteorology in 10 Canadian cities. Environ. Pollut. 2014, 185, 322–332. [Google Scholar] [CrossRef]
- Liu, W.Y.; Yi, J.P.; Shi, L.Y.; Tung, T.H. Association between air pollutants and pediatric respiratory outpatient visits in Zhoushan, China. Front. Public Health 2022, 10, 865798. [Google Scholar] [CrossRef]
- Ma, Y.L.; Yue, L.; Liu, J.T.; He, X.T.; Li, L.Y.; Niu, J.P.; Luo, B. Association of air pollution with outpatient visits for respiratory diseases of children in an ex-heavily polluted northwestern city, China. BMC Public Health 2020, 20, 816. [Google Scholar] [CrossRef]
- Song, J.; Lu, M.X.; Zheng, L.H.; Liu, Y.; Xu, P.W.; Li, Y.C.; Xu, D.Q.; Wu, W.D. Acute effects of ambient air pollution on outpatient children with respiratory diseases in Shijiazhuang, China. BMC Pulm. Med. 2018, 18, 150. [Google Scholar] [CrossRef] [PubMed]
- Filonchyk, M.; Peterson, M. Air quality changes in Shanghai, China, and the surrounding urban agglomeration during the COVID-19 lockdown. J. Geovis. Spat. Anal. 2020, 4, 22. [Google Scholar] [CrossRef]
- Xu, H.; Wang, X.Y.; Tian, Y.H.; Tian, J.; Zeng, Y.P.; Guo, Y.L.; Song, F.; Xu, X.; Ni, X.; Feng, G.S. Short-term exposure to gaseous air pollutants and daily hospitalizations for acute upper and lower respiratory infections among children from 25 cities in China. Environ. Res. 2022, 212, 113493. [Google Scholar] [CrossRef]
- Niu, Y.; Chen, R.; Wang, C.; Wang, W.; Jiang, J.; Wu, W.; Cai, J.; Zhao, Z.; Xu, X.; Kan, H. Ozone exposure leads to changes in airway permeability, microbiota and metabolome: A randomised, double-blind, crossover trial. Eur. Respir. J. 2020, 56, 2000165. [Google Scholar] [CrossRef]
- Hu, F.; Jing, L.M.; Shi, R. Analysis of related factors and disease costs of respiratory infection and environmental pollution in children. Technol. Health Care 2020, 28, S355–S360. [Google Scholar] [CrossRef]
- Li, Y.W.; Li, C.C.; Liu, J.Y.; Meng, C.S.; Xu, C.Y.; Liu, Z.; Wang, Q.; Liu, Y.; Han, J.X.; Xu, D.Q. An association between PM2.5 and pediatric respiratory outpatient visits in four Chinese cities. Chemosphere 2021, 280, 130843. [Google Scholar] [CrossRef]
- He, M.; Zhong, Y.P.; Chen, Y.A.; Zhong, N.S.; Lai, K.F. Association of short-term exposure to air pollution with emergency visits for respiratory diseases in children. iScience 2022, 25, 104879. [Google Scholar] [CrossRef]
- Ma, Y.X.; Yang, S.X.; Zhou, J.D.; Yu, Z.A.; Zhou, J. Effect of ambient air pollution on emergency room admissions for respiratory diseases in Beijing, China. Atmos. Environ. 2018, 191, 320–327. [Google Scholar] [CrossRef]
- Granados-Canal, D.J.; Chardon, B.; Lefranc, A.; Gremy, I. Air pollution and respiratory hospital admissions in greater Paris: Exploring sex differences. Arch. Environ. Occup. Health 2005, 60, 307–313. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Jiang, W.Y.H.; Gao, X.; Lin, C.W.; Li, J.; Yang, L. Short-term effects and economic burden of air pollutants on acute lower respiratory tract infections in children in southwest China: A time-series study. Environ. Health 2023, 22, 6. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.W.; Wang, J.B.; Zhang, Z.Y.; Shen, P.; Chai, P.F.; Li, D.; Jin, M.J.; Tang, M.L.; Lu, H.C.; Lin, H.B.; et al. Air pollution and hospital visits for acute upper and lower respiratory infections among children in Ningbo, China: A time-series analysis. Environ. Sci. Pollut. Res. 2017, 24, 18860–18869. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wang, B.Y.; Qian, N.N.; Wei, H.Y.; Yang, G.M.; Wan, L.P.; He, Y. Association between ambient PM2.5 and outpatient visits of children’s respiratory diseases in a megacity in central China. Front. Public Health 2022, 10, 952662. [Google Scholar] [CrossRef]
| ER (%) and 95% CI | |||||||
|---|---|---|---|---|---|---|---|
| PM2.5 | PM10 | O3 | NO2 | SO2 | CO | ||
| URTI | Boy | 0.69 (0.15, 1.22) | 0.32 (−0.03, 0.67) | 0.84 (0.13, 1.554) | 0.42 (−2.59, 3.53) | 0.99 (−0.28, 2.27) | — |
| Girl | 0.73 (0.12, 1.34) | 0.35 (−0.05, 0.76) | 0.67 (−0.15, 1.50) | 6.24 (2.59, 10.01) | 1.37 (−0.05, 2.82) | — | |
| PNMN | Boy | 3.42 (1.18, 5.71) | 1.30 (−0.58, 3.21) | 1.78 (−0.43, 4.03) | 7.67 (0.16, 15.74) | 3.93 (1.11, 6.83) | 4.23 (0.46, 8.15) |
| Girl | 3.92 (1.32, 6.58) | 1.33 (−0.82, 3.52) | 2.89 (0.12, 5.74) | 13.29 (4.53, 22.78) | 3.28 (0.15, 6.51) | 6.58 (2.10, 11.26) | |
| BCT | Boy | — | 2.23 (0.86, 3.63) | 1.44 (0.48, 2.41) | 5.50 (1.35, 9.81) | 3.89 (1.66, 6.17) | — |
| Girl | — | 0.33 (−1.35, 2.03) | 1.26 (−0.06, 2.60) | 3.03 (−2.01, 8.34) | 0.98 (−1.77, 3.81) | — | |
| BCLT | Boy | 2.13 (0.37, 3.93) | — | — | — | — | 2.68 (0.11, 5.31) |
| Girl | 0.81 (−1.50, 3.17) | — | — | — | — | 1.39 (−1.91, 4.81) | |
| ER (%) and 95% CI | |||||||
|---|---|---|---|---|---|---|---|
| PM2.5 | PM10 | O3 | NO2 | SO2 | CO | ||
| URTI | <1 | 0.75 (−0.12, 1.63) | 0.57 (0.01, 1.13) | −0.14 (−1.21, 0.93) | 1.95 (−2.48, 6.58) | 0.76 (−1.15, 2.70) | — |
| 1–3 | 0.76 (0.17, 1.35) | 0.32 (−0.06, 0.71) | 0.46 (−0.32, 1.26) | 1.70 (−1.63, 5.15) | 0.99 (−0.43, 2.42) | — | |
| 4–6 | 0.33 (−0.54, 1.21) | −0.09 (−0.69, 0.51) | 2.65 (1.35, 3.97) | 4.13 (−1.44, 10.01) | 0.43 (−1.63, 2.54) | — | |
| 7–13 | 1.59 (0.20, 3.00) | 0.80 (−0.08, 1.69) | 2.76 (0.87, 4.69) | 10.60 (2.43, 19.42) | 4.05 (0.79, 7.42) | — | |
| 14–16 | 3.36 (−1.42, 8.37) | 3.55 (0.50, 6.68) | −3.34 (−10.07, 3.90) | −14.60 (−34.19, 10.82) | −6.18 (−16.05, 4.84) | — | |
| PNMN | <1 | 3.61 (0.86, 6.44) | 1.91 (−0.38, 4.25) | 1.02 (−1.61, 3.72) | 8.28 (−1.00, 18.42) | 3.15 (−0.33, 6.76) | 7.15 (2.52, 11.99) |
| 1–3 | 3.67 (1.16, 6.24) | 1.79 (−0.34, 3.96) | 3.50 (0.77, 6.30) | 10.93 (2.14, 20.49) | 3.50 (0.29, 6.82) | 3.81 (−0.47, 8.26) | |
| 4–6 | 4.14 (−0.60, 9.10) | −0.44 (−4.28, 3.55) | 2.13 (−2.78, 7.27) | 3.23 (−10.87, 19.54) | 5.69 (−0.03, 11.74) | 5.85 (−2.48, 14.88) | |
| 7–13 | 2.71 (−6.48, 12.80) | −3.82 (−10.18, 2.98) | 6.34 (−0.29, 13.42) | 31.34 (1.88, 69.32) | 7.78 (−2.20, 18.78) | 3.36 (−10.55, 19.43) | |
| 14–16 | 2.13 (−28.86, 46.61) | −9.12 (−35.29, 27.65) | 0.32 (−32.90, 49.98) | −17.23 (−75.27, 177.10) | −20.05 (−50.90, 30.19) | 1.94 (−44.20, 86.24) | |
| BCT | <1 | — | 2.11 (−0.08, 4.36) | 0.74 (−0.96,2.47) | 8.45 (1.59,15.77) | 0.95 (−2.52,4.54) | — |
| 1–3 | — | 1.23 (−0.17, 2.65) | 1.42 (0.41, 2.44) | 1.90 (−2.23, 6.19) | 2.62 (0.29, 5.00) | — | |
| 4–6 | — | 1.37 (−1.08, 3.88) | 1.69 (−0.22, 3.63) | 10.95 (3.81, 18.58) | 7.40 (4.11, 10.79) | — | |
| 7–13 | — | 7.42 (0.02, 15.37) | 1.82 (−2.10, 5.89) | 11.02 (−9.06, 35.54) | 16.81 (4.35, 30.77) | — | |
| 14–16 | — | The confidence interval is wide. | −10.90 (−46.57, 48.60) | ||||
| BCLT | <1 | 1.89 (0.27, 3.54) | — | — | — | — | 2.15 (−0.12, 4.48) |
| 1–3 | 0.71 (−1.71, 3.20) | — | — | — | — | 1.24 (−2.25, 4.85) | |
| 4–6 | 2.21 (−24.96, 39.23) | — | — | — | — | −2.75 (−36.59, 49.17) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, D.; Wang, Y.; Liu, Q.; Sun, W.; Wei, L.; Ye, C.; Zhu, R. Association of Air Pollution with the Number of Common Respiratory Visits in Children in a Heavily Polluted Central City, China. Toxics 2023, 11, 815. https://doi.org/10.3390/toxics11100815
Wang D, Wang Y, Liu Q, Sun W, Wei L, Ye C, Zhu R. Association of Air Pollution with the Number of Common Respiratory Visits in Children in a Heavily Polluted Central City, China. Toxics. 2023; 11(10):815. https://doi.org/10.3390/toxics11100815
Chicago/Turabian StyleWang, Dan, Yanan Wang, Qianqian Liu, Wenxin Sun, Liangkui Wei, Chengxin Ye, and Rencheng Zhu. 2023. "Association of Air Pollution with the Number of Common Respiratory Visits in Children in a Heavily Polluted Central City, China" Toxics 11, no. 10: 815. https://doi.org/10.3390/toxics11100815
APA StyleWang, D., Wang, Y., Liu, Q., Sun, W., Wei, L., Ye, C., & Zhu, R. (2023). Association of Air Pollution with the Number of Common Respiratory Visits in Children in a Heavily Polluted Central City, China. Toxics, 11(10), 815. https://doi.org/10.3390/toxics11100815








