Suicidal Behavior and Its Relationship with Postmortem Forensic Toxicological Findings
Abstract
1. Introduction
2. Materials and Methods
2.1. Suicide Enrolment, Data Acquisition, and Mechanisms of Suicide
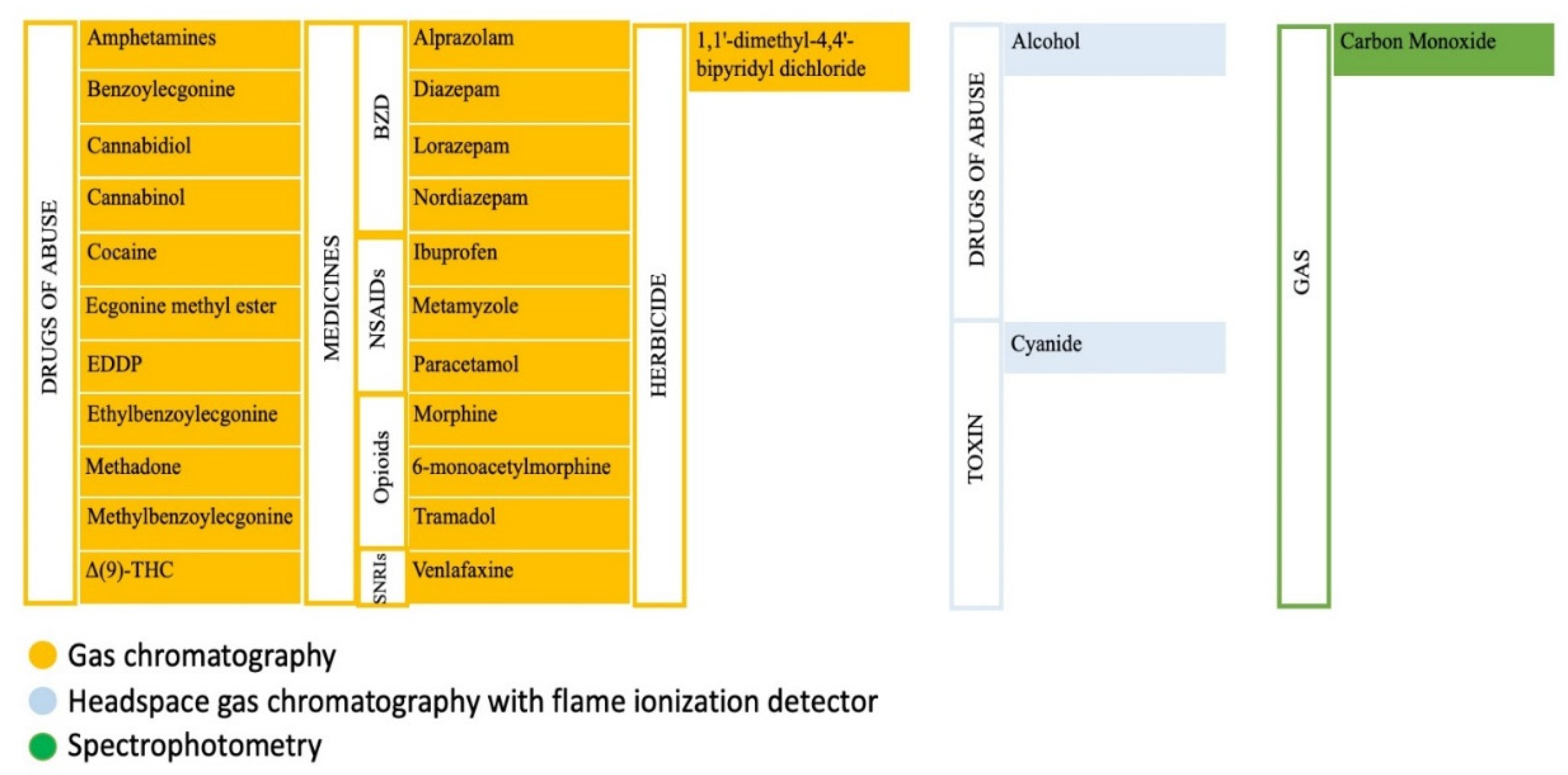
2.2. Chemical–Toxicological Analytical Techniques
2.3. Statistical Analysis
3. Results
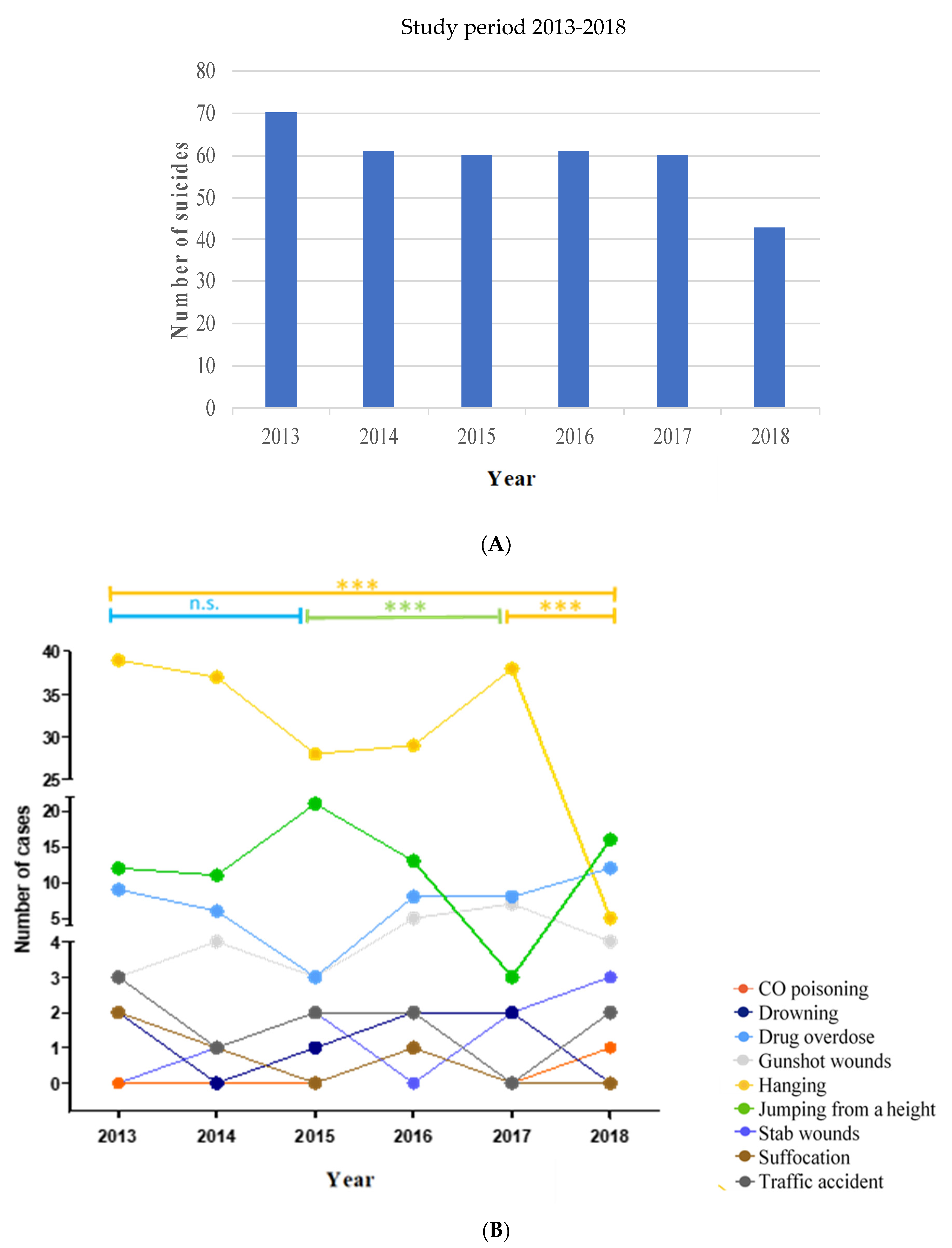
3.1. Suicides in the Study Period Analyzed
3.2. Analysis of Suicide Mechanism, Toxicological Findings, and Sex
3.3. Analysis of Suicide Mechanisms and the Number of Toxics Found
3.4. Analysis of the Types of Toxics Found According to the Sex of the Suicide Victims
3.5. Toxic Combinations Found in Suicides
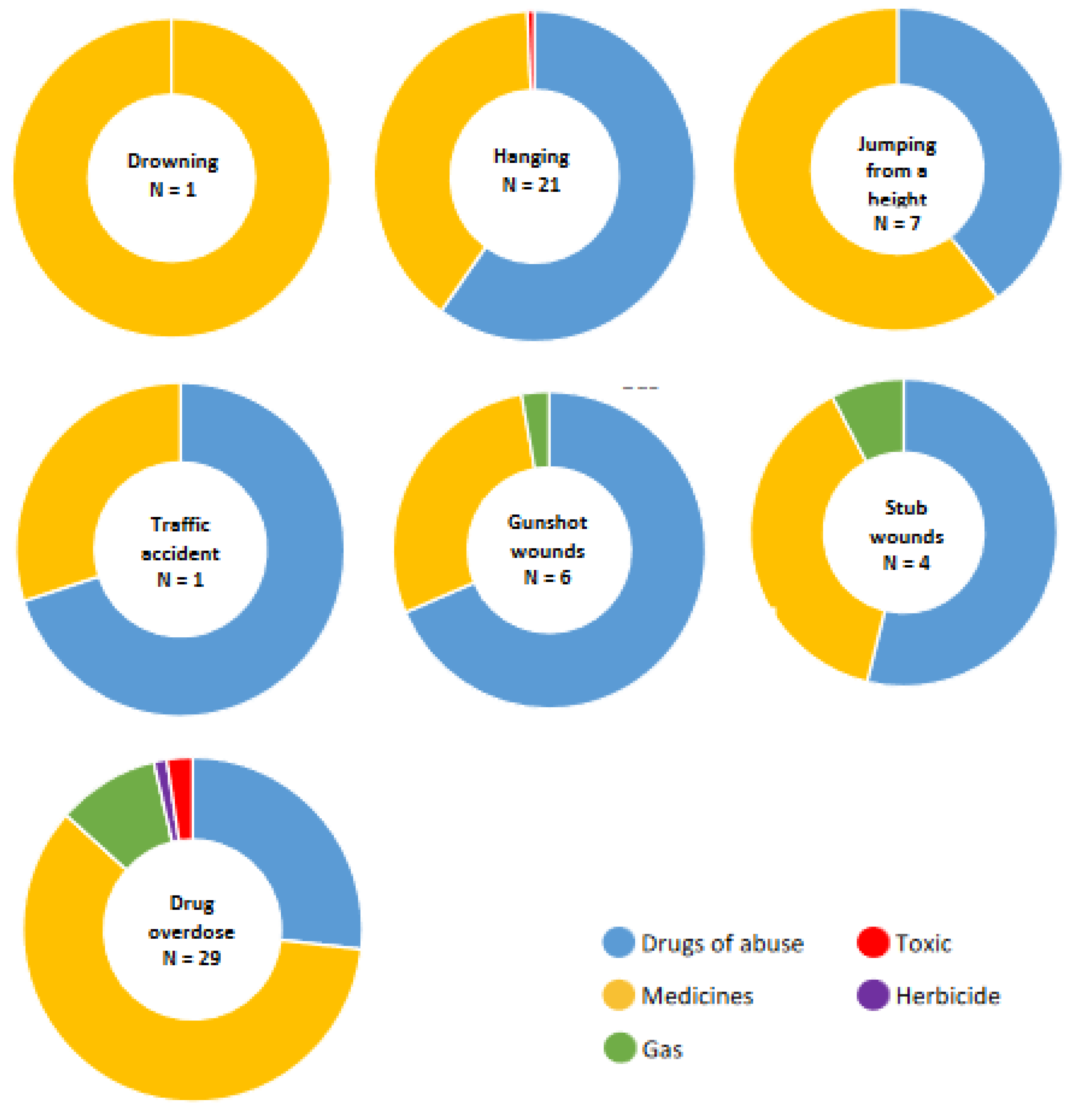
3.6. Types of Toxics Found in the Different Mechanisms of Suicide
3.7. Analysis of Concentrations of the Different Toxics in Drug Overdose Suicides
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- WHO. National Suicide Prevention Strategies; 2018; Volume 30, ISBN 9789241515016.World Health Organization. Preventing Suicide: A Global Imperative. 2014. Available online: https://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ (accessed on 26 April 2022).
- Blosnich, J.R.; Montgomery, A.E.; Dichter, M.E.; Gordon, A.J.; Kavalieratos, D.; Taylor, L.; Ketterer, B.; Bossarte, R.M. Social Determinants and Military Veterans’ Suicide Ideation and Attempt: A Cross-sectional Analysis of Electronic Health Record Data. J. Gen. Intern. Med. 2020, 35, 1759–1767. [Google Scholar] [CrossRef] [PubMed]
- Amudhan, S.; Gururaj, G.; Varghese, M.; Benegal, V.; Rao, G.N.; Sheehan, D.V.; Kokane, A.M.; Chavan, B.S.; Dalal, P.K.; Ram, D.; et al. A population-based analysis of suicidality and its correlates: Findings from the National Mental Health Survey of India, 2015–2016. Lancet Psychiatry 2020, 7, 41–51. [Google Scholar] [CrossRef]
- Näher, A.F.; Rummel-Kluge, C.; Hegerl, U. Associations of Suicide Rates With Socioeconomic Status and Social Isolation: Findings From Longitudinal Register and Census Data. Front. Psychiatry 2020, 10, 898. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.T. The psychological scars of suicide: Accounting for how risk for suicidal behavior is heightened by its past occurrence. Neurosci. Biobehav. Rev. 2019, 99, 42–48. [Google Scholar] [CrossRef]
- Macalli, M.; Tournier, M.; Galéra, C.; Montagni, I.; Soumare, A.; Côté, S.M.; Tzourio, C. Perceived parental support in childhood and adolescence and suicidal ideation in young adults: A cross-sectional analysis of the i-Share study. BMC Psychiatry 2018, 18, 373. [Google Scholar] [CrossRef]
- Suicidio. Available online: https://www.who.int/es/news-room/fact-sheets/detail/suicide (accessed on 24 October 2019).
- Huertas, P.; Moreno-Küstner, B.; Gutiérrez, B.; Cervilla, J.A. Prevalence and correlates of suicidality in Andalusia (Spain): Results of the epidemiological study PISMA-ep. J. Affect. Disord. 2020, 266, 503–511. [Google Scholar] [CrossRef]
- Pearson, J.L.; Conwell, Y. Suicide and Aging: International Perspectives; Springer Publishing Co.: New York, NY, USA, 1996; ISBN 0-8261-9370-6. [Google Scholar]
- Harris, E.C.; Barraclough, B. Suicide as an outcome for mental disorders. A meta-analysis. Br. J. Psychiatry 1997, 170, 205–228. [Google Scholar] [CrossRef]
- Reger, M.A.; Stanley, I.H.; Joiner, T.E. Suicide Mortality and Coronavirus Disease 2019—A Perfect Storm? JAMA Psychiatry 2020, 77, 1093–1094. [Google Scholar] [CrossRef]
- Millner, A.J.; Lee, M.D.; Hoyt, K.; Buckholtz, J.W.; Auerbach, R.P.; Nock, M.K. Are suicide attempters more impulsive than suicide ideators? Gen. Hosp. Psychiatry 2020, 63, 103–110. [Google Scholar] [CrossRef]
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J.; Caine, E.D.; et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef]
- Conner, K.R.; Lathrop, S.; Caetano, R.; Wiegand, T.; Kaukeinen, K.; Nolte, K.B. Presence of Alcohol, Cocaine, and Other Drugs in Suicide and Motor Vehicle Crash Decedents Ages 18 to 54. Alcohol. Clin. Exp. Res. 2017, 41, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, J.M.; Witte, T.K.; Correia, C.J. Suicide Ideation, Alcohol Consumption, Motives, and Related Problems: Exploring the Association in College Students. Suicide Life-Threatening Behav. 2017, 47, 142–154. [Google Scholar] [CrossRef] [PubMed]
- Kopacz, M.S.; Bryan, C.J.; Bishop, T.M.; Ashrafioun, L. Alcohol and Suicide Risk: Examining the Role of Meaning-Making. J. Dual Diagn. 2018, 14, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Conway, C.C.; Keenan-Miller, D.; Hammen, C.; Lind, P.A.; Najman, J.M.; Brennan, P.A. Coaction of stress and serotonin transporter genotype in predicting aggression at the transition to adulthood. J. Clin. Child Adolesc. Psychol. 2012, 41, 53–63. [Google Scholar] [CrossRef][Green Version]
- Dome, P.; Rihmer, Z.; Gonda, X. Suicide risk in bipolar disorder: A brief review. Medicina 2019, 55, 8–10. [Google Scholar] [CrossRef]
- Gabriel, F.C.; de Melo, D.O.; Fráguas, R.; Leite-Santos, N.C.; da Silva, R.A.M.; Ribeiro, E. Pharmacological treatment of depression: A systematic review comparing clinical practice guideline recommendations. PLoS ONE 2020, 15, e0231700. [Google Scholar] [CrossRef]
- Barbui, C.; Esposito, E.; Cipriani, A. Selective serotonin reuptake inhibitors and risk of suicide: A systematic review of observational studies. Can. Med. Assoc. J. 2009, 180, 291–297. [Google Scholar] [CrossRef]
- Forsman, J.; Taipale, H.; Masterman, T.; Tiihonen, J.; Tanskanen, A. Adherence to psychotropic medication in completed suicide in Sweden 2006–2013: A forensic-toxicological matched case-control study. Eur. J. Clin. Pharmacol. 2019, 75, 1421–1430. [Google Scholar] [CrossRef]
- Pompili, M.; Serafini, G.; Innamorati, M.; Dominici, G.; Ferracuti, S.; Kotzalidis, G.D.; Serra, G.; Girardi, P.; Janiri, L.; Tatarelli, R.; et al. Suicidal behavior and alcohol abuse. Int. J. Environ. Res. Public Health 2010, 7, 1392–1431. [Google Scholar] [CrossRef]
- Schneeweiss, S.; Patrick, A.R.; Solomon, D.H.; Mehta, J.; Dormuth, C.; Ma, S.; Miller, M.; Lee, J.C.; Wang, P.S. Variation in the Risk of Suicide Attempts and Completed Suicides by Antidepressant Agent in Adults A Propensity Score-Adjusted Analysis of 9 Years’ Data. Arch. Gen. Psychiatry 2010, 67, 497–506. [Google Scholar] [CrossRef]
- Borges, G.; Cherpitel, C.J.; MacDonald, S.; Giesbrecht, N.; Stockwell, T.; Wilcox, H.C. A case-crossover study of acute alcohol use and suicide attempt. J. Stud. Alcohol 2004, 65, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Miller, T.R.; Swedler, D.I.; Lawrence, B.A.; Ali, B.; Rockett, I.R.H.; Carlson, N.N.; Leonardo, J. Incidence and Lethality of Suicidal Overdoses by Drug Class. JAMA Netw. Open 2020, 3, e200607. [Google Scholar] [CrossRef] [PubMed]
- Dean, B.; Duncan, C.; Gibbons, A. Changes in levels of cortical metabotropic glutamate 2 receptors with gender and suicide but not psychiatric diagnoses. J. Affect. Disord. 2019, 244, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Lutz, P.E.; Wang, Y.C.; Ragoussis, J.; Turecki, G. Global long non-coding RNA expression in the rostral anterior cingulate cortex of depressed suicides. Transl. Psychiatry 2018, 8, 224. [Google Scholar] [CrossRef]
- Wei, S.; Womer, F.Y.; Edmiston, E.K.; Zhang, R.; Jiang, X.; Wu, F.; Kong, L.; Zhou, Y.; Tang, Y.; Wang, F. Structural alterations associated with suicide attempts in major depressive disorder and bipolar disorder: A diffusion tensor imaging study. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2020, 98, 109827. [Google Scholar] [CrossRef]
- Manji, H.K.; Drevets, W.C.; Charney, D.S. The cellular neurobiology of depression. Nat. Med. 2001, 7, 541–547. [Google Scholar] [CrossRef]
- Kinkead, B.; Nemeroff, C.B. Neurotensin: An endogenous antipsychotic? Curr. Opin. Pharmacol. 2002, 2, 99–103. [Google Scholar] [CrossRef]
- Cabrera-Mendoza, B.; Fresno, C.; Monroy-Jaramillo, N.; Fries, G.R.; Walss-Bass, C.; Glahn, D.C.; Ostrosky-Wegman, P.; Mendoza-Morales, R.C.; García-Dolores, F.; Díaz-Otañez, C.E.; et al. Sex differences in brain gene expression among suicide completers. J. Affect. Disord. 2020, 267, 67–77. [Google Scholar] [CrossRef]
- Sequeira, A.; Morgan, L.; Walsh, D.M.; Cartagena, P.M.; Choudary, P.; Li, J.; Schatzberg, A.F.; Watson, S.J.; Akil, H.; Myers, R.M.; et al. Gene expression changes in the prefrontal cortex, anterior cingulate cortex and nucleus accumbens of mood disorders subjects that committed suicide. PLoS ONE 2012, 7, e35367. [Google Scholar] [CrossRef]
- Raust, A.; Slama, F.; Mathieu, F.; Roy, I.; Chenu, A.; Koncke, D.; Fouques, D.; Jollant, F.; Jouvent, E.; Courtet, P.; et al. Prefrontal cortex dysfunction in patients with suicidal behavior. Psychol. Med. 2007, 37, 411–419. [Google Scholar] [CrossRef]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Nagamatsu, K.; Kudo, K.; Usumoto, Y.; Tsuji, A.; Nishi, H.; Ikeda, N. Rapid screening of 18 nonsteroidal anti-inflammatory drugs (NSAIDs) using novel NAGINATATM gas chromatography-mass spectrometry software. Forensic Toxicol. 2012, 30, 11–18. [Google Scholar] [CrossRef]
- Al-Asmari, A.I.; Anderson, R.A. Method for Quantification of Opioids and their Metabolites in Autopsy Blood by Liquid Chromatography-Tandem Mass Spectrometry. J. Anal. Toxicol. 2007, 31, 394–408. [Google Scholar] [CrossRef] [PubMed]
- Rasanen, I.; Neuvonen, M.; Ojanperä, I.; Vuori, E. Benzodiazepine findings in blood and urine by gas chromatography and immunoassay. Forensic Sci. Int. 2000, 112, 191–200. [Google Scholar] [CrossRef]
- Jantos, R.; Skopp, G. Postmortem blood and tissue concentrations of R- and S-enantiomers of methadone and its metabolite EDDP. Forensic Sci. Int. 2013, 226, 254–260. [Google Scholar] [CrossRef]
- Andrews, R.; Paterson, S. A validated method for the analysis of cannabinoids in postmortem blood using liquid–liquid extraction and two-dimensional gas chromatography–mass spectrometry. Forensic Sci. Int. 2012, 222, 111–117. [Google Scholar] [CrossRef]
- Shimomura, E.T.; Hodge, G.D.; Paul, B.D. Examination of Postmortem Fluids and Tissues for the Presence of Methylecgonidine, Ecgonidine, Cocaine, and Benzoylecgonine Using Solid-Phase Extraction and Gas Chromatography–Mass Spectrometry. Clin. Chem. 2001, 47, 1040–1047. [Google Scholar] [CrossRef]
- Hasegawa, C.; Kumazawa, T.; Lee, X.P.; Marumo, A.; Shinmen, N.; Seno, H.; Sato, K. Pipette tip solid-phase extraction and gas chromatography—Mass spectrometry for the determination of methamphetamine and amphetamine in human whole blood. Anal. Bioanal. Chem. 2007, 389, 563–570. [Google Scholar] [CrossRef]
- Paterson, S.; Cordero, R.; Burlinson, S. Screening and semi-quantitative analysis of post mortem blood for basic drugs using gas chromatography/ion trap mass spectrometry. J. Chromatogr. B 2004, 813, 323–330. [Google Scholar] [CrossRef]
- Xiao, H.T.; He, L.; Tong, R.S.; Yu, J.Y.; Chen, L.; Zou, J.; Li, J.Q.; Bian, Y.; Zhang, Y. Rapid and sensitive headspace gas chromatography-mass spectrometry method for the analysis of ethanol in the whole blood. J. Clin. Lab. Anal. 2014, 28, 386–390. [Google Scholar] [CrossRef]
- Destanoğlu, O.; Ateş, İ. Headspace gas chromatography–mass spectrometry method for the determination of total cyanide concentration in water and postmortem blood samples. J. Serb. Chem. Soc. 2021, 86, 77–90. [Google Scholar] [CrossRef]
- Widdop, B. Analysis of carbon monoxide. Ann. Clin. Biochem. 2002, 39, 378–391. [Google Scholar] [CrossRef] [PubMed]
- Molina, D.K. Handbook of Forensic Toxicology for Medical Examiners; CRC Press: Boca Raton, FL, USA, 2009. [Google Scholar]
- Repetto, M.R.; Repetto, M. Tabla de Concentraciones de Xenobióticos en Fluidos Biológicos Humanos Como Referencia Para el Diagnóstico Toxicológico; Area de Toxicología de la Universidad de Sevilla: Sevilla, Spain, 2015; Volume 151, ISBN 9781450349185. [Google Scholar]
- Turecki, G.; Brent, D.A.; Gunnell, D.; O’Connor, R.C.; Oquendo, M.A.; Pirkis, J.; Stanley, B.H. Suicide and suicide risk. Nat. Rev. Dis. Prim. 2019, 5, 74. [Google Scholar] [CrossRef] [PubMed]
- Yip, P.S.F.; Caine, E.; Yousuf, S.; Chang, S.S.; Wu, K.C.C.; Chen, Y.Y. Means restriction for suicide prevention. Lancet 2012, 379, 2393–2399. [Google Scholar] [CrossRef]
- Mann, J.J.; Apter, A.; Bertolote, J.; Beautrais, A.; Currier, D.; Haas, A.; Hegerl, U.; Lonnqvist, J.; Malone, K.; Marusic, A.; et al. Suicide Prevention Strategies: A Systematic Review. JAMA 2005, 294, 2064–2074. [Google Scholar] [CrossRef]
- Kim, H.; Kwon, S.W.; Ahn, Y.M.; Jeon, H.J.; Park, S.; Hong, J.P. Implementation and outcomes of suicide-prevention strategies by restricting access to lethal suicide methods in Korea. J. Public Heal. Policy 2018, 40, 91–102. [Google Scholar] [CrossRef]
- Yuodelis-Flores, C.; Ries, R.K. Addiction and suicide: A review. Am. J. Addict. 2015, 24, 98–104. [Google Scholar] [CrossRef]
- Wong, J.C. Predicting Suicide and its Prevention. Ann. Acad. Med. Singap. 2018, 47, 357–359. [Google Scholar]
- Van Heeringen, K.; Mann, J.J. The neurobiology of suicide. Lancet Psychiatry 2014, 1, 63–72. [Google Scholar] [CrossRef]
- Turecki, G.; Brent, D.A. Suicide and suicidal behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef]
- Anzillotti, L.; Marezza, F.; Calò, L.; Cucurachi, N.; Veronesi, L.; Cecchi, R. Toxicological findings: A retrospective overview of medico-legal investigations in Parma (Italy). J. Forensic Leg. Med. 2019, 62, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Behzadifar, M.; Spencer, L.J.; Chris, D.C.; Zachary, V.D.; Jack, T.F. Global injury morbidity and mortality from 1990 to 2017: Results from the Global Burden of Disease Study 2017. Inj. Prev. 2020, injuryprev-2019-043494. [Google Scholar]
- Nikitopoulou, T.; Moraitis, K.; Tsellou, M.; Stefanidou-Loutsidou, M.; Spiliopoulou, C.; Papadodima, S. Violent deaths among elderly in Attica, Greece: A 5-year survey (2011–2015). J. Forensic Leg. Med. 2019, 65, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Mereish, E.H.; Peters, J.R.; Yen, S. Minority Stress and Relational Mechanisms of Suicide among Sexual Minorities: Subgroup Differences in the Associations between Heterosexist Victimization, Shame, Rejection Sensitivity, and Suicide Risk. Suicide Life-Threatening Behav. 2019, 49, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Ivey-Stephenson, A.Z.; Crosby, A.E.; Jack, S.P.D.; Haileyesus, T.; Kresnow-Sedacca, M.J. Suicide Trends Among and Within Urbanization Levels by Sex, Race/Ethnicity, Age Group, and Mechanism of Death—United States, 2001–2015. MMWR Surveill. Summ. 2017, 66, 1–16. [Google Scholar] [CrossRef]
- Biddle, L.; Brock, A.; Brookes, S.T.; Gunnell, D. Suicide rates in young men in England and Wales in the 21st century: Time trend study. BMJ 2008, 336, 539–542. [Google Scholar] [CrossRef]
- Gunnell, D.; Wehner, H.; Frankel, S. Research Letters. Lancet 1999, 9152, 556–557. [Google Scholar] [CrossRef]
- Santurtún, M.; Santurtún, A.; Agudo, G.; Zarrabeitia, M.T. Método empleado en las muertes por suicidio en España: Envenenamiento y agentes violentos no tóxicos. Cuad. Med. Forense 2016, 22, 73–80. [Google Scholar]
- Parra Uribe, I.; Blasco-Fontecilla, H.; García-Parés, G.; Giró Batalla, M.; Llorens Capdevila, M.; Cebrià Meca, A.; De Leon-Martinez, V.; Pérez-Solà, V.; Palao Vidal, D.J. Attempted and completed suicide: Not what we expected? J. Affect. Disord. 2013, 150, 840–846. [Google Scholar] [CrossRef]
- Mejías-Martín, Y.; Luna del Castillo, J.D.D.; Rodríguez-Mejías, C.; Martí-García, C.; Valencia-Quintero, J.P.; García-Caro, M.P. Factors associated with suicide attempts and suicides in the general population of andalusia (Spain). Int. J. Environ. Res. Public Health 2019, 16, 4496. [Google Scholar] [CrossRef]
- Cano-Montalbán, I.; Quevedo-Blasco, R. Sociodemographic variables most associated with suicidal behaviour and suicide methods in Europe and America. A systematic review. Eur. J. Psychol. Appl. Leg. Context 2018, 10, 15–25. [Google Scholar] [CrossRef]
- Mergl, R.; Koburger, N.; Heinrichs, K.; Székely, A.; Tóth, M.D.; Coyne, J.; Quintão, S.; Arensman, E.; Coffey, C.; Maxwell, M.; et al. What Are Reasons for the Large Gender Differences in the Lethality of Suicidal Acts? An Epidemiological Analysis in Four European Countries. PLoS ONE 2015, 10, e0129062. [Google Scholar] [CrossRef] [PubMed]
- Hingson, R.W.; Zha, W.; White, A.M. Drinking Beyond the Binge Threshold: Predictors, Consequences, and Changes in the U.S. Am. J. Prev. Med. 2017, 52, 717–727. [Google Scholar] [CrossRef] [PubMed]
- NIH. Entender Los Riesgos de Sobredosis de Alcohol; National Institute on Alcohol Abuse and Alcoholism: Bethesda, MD, USA, 2020. [Google Scholar]
- Tesfazion, A.A. Emergency Department Visits for Drug-Related Suicide Attempts among Middle-Aged Adults Aged 45 to 64; The CBHSQ Report; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2013. [Google Scholar]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N.; Choi, B.Y. Relationship between marijuana and other illicit drug use and depression/suicidal thoughts among late middle-aged and older adults. Int. Psychogeriatr. 2016, 28, 577–589. [Google Scholar] [CrossRef]
- Britton, P.; Bohnert, A.; Wines, J.; Conner, K. A procedure that differentiates unintentional from intentional overdose in opioid abusers. Addict. Behav. 2012, 37, 127–130. [Google Scholar] [CrossRef][Green Version]
- Richer, I.; Bertrand, K.; Vandermeershen, J.; Roy, E. A prospective cohort study of non-fatal accidental overdose among street youth: The link with suicidal ideation. Drug Alcohol Rev. 2013, 32, 398–404. [Google Scholar] [CrossRef]
- Allan, N.P.; Ashrafioun, L.; Kolnogorova, K.; Raines, A.M.; Hoge, C.W.; Stecker, T. Interactive effects of PTSD and substance use on suicidal ideation and behavior in military personnel: Increased risk from marijuana use. Depress. Anxiety 2019, 36, 1072–1079. [Google Scholar] [CrossRef]
- Fernandez, A.; Miguel, A.; Pereiro, C. Relación entre sobredosis y suicidio en las muertes asociadas al consumo de drogas. Rev. Toxicol. 2018, 35, 37–44. [Google Scholar]
- Simonovska, N.K.; Stefanovska, V.V.; Babulovska, A. Non-Opioid Substances Acute Poisonings with Suicidal Intent in Patients with Opioid Use Disorder. Folia Med. 2020, 62, 117–123. [Google Scholar] [CrossRef]
- Brent, D.A.; Baugher, M.; Bridge, J.; Chen, T.; Chiappetta, L. Age- and Sex-Related Risk Factors for Adolescent Suicide. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 1497–1505. [Google Scholar] [CrossRef]
- Choi, N.G.; DiNitto, D.M.; Sagna, A.O.; Marti, C.N. Older women who died by suicide: Suicide means, sociodemographic and psychiatric risk factors, and other precipitating circumstances. Int. Psychogeriatr. 2018, 30, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, G.A.; Olfson, M.; Martins, S.S. Sex differences in US emergency department non-fatal visits for benzodiazepine poisonings in adolescents and young adults. Drug Alcohol Depend. 2021, 221, 108609. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Case, B.; Spirito, A. Injection drug use is associated with suicide attempts but not ideation or plans in a sample of adolescents with depressive symptoms. J. Psychiatr. Res. 2014, 56, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Mitra, G.; Wood, E.; Nguyen, P.; Kerr, T.; DeBeck, K. Drug use patterns predict risk of non-fatal overdose among street-involved youth in a Canadian setting. Drug Alcohol Depend. 2015, 153, 135–139. [Google Scholar] [CrossRef]
- O’Halloran, C.; Cullen, K.; Njoroge, J.; Jessop, L.; Smith, J.; Hope, V.; Ncube, F. The extent of and factors associated with self-reported overdose and self-reported receipt of naloxone among people who inject drugs (PWID) in England, Wales and Northern Ireland. Int. J. Drug Policy 2017, 46, 34–40. [Google Scholar] [CrossRef]
- Park, S.; Song, H. Factors That Affect Adolescent Drug Users’ Suicide Attempts. Psychiatry Investig. 2016, 13, 360–363. [Google Scholar] [CrossRef]
- Davidson, K.M. Diagnosis of Depression in Alcohol Dependence: Changes in Prevalence with Drinking Status. Br. J. Psychiatry 1995, 166, 199–204. [Google Scholar] [CrossRef]
- Hardt, J.; Bernert, S.; Matschinger, H.; Angermeier, M.C.; Vilagut, G.; Bruffaerts, R.; De Girolamo, G.; De Graaf, R.; Haro, J.M.; Kovess, V.; et al. Suicidality and its relationship with depression, alcohol disorders and childhood experiences of violence: Results from the ESEMeD study. J. Affect. Disord. 2015, 175, 168–174. [Google Scholar] [CrossRef]
- Perez, J.; Beale, E.; Overholser, J.; Athey, A.; Stockmeier, C. Depression and alcohol use disorders as precursors to death by suicide. Death Stud. 2020, 46, 619–627. [Google Scholar] [CrossRef]
- Schuckit, M.A.; Smith, T.L.; Danko, G.P.; Pierson, J.; Trim, R.; Nurnberger, J.I.; Kramer, J.; Kuperman, S.; Bierut, L.J.; Hesselbrock, V. A Comparison of Factors Associated With Substance-Induced Versus Independent Depressions. J. Stud. Alcohol Drugs 2007, 68, 805–812. [Google Scholar] [CrossRef][Green Version]
- Campagne, D.M.; García-Campayo, J. El inadecuado uso de las benzodiacepinas. Semergen 2005, 31, 319–324. [Google Scholar] [CrossRef]
- Sher, L. Alcohol and suicide: Neurobiological and clinical aspects. Sci. World J. 2006, 6, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Ortega Pérez, A. Estaba intoxicado por cocaína este individuo? (y II): Estimaciones basadas en los efectos de la droga y en las concentraciones de benzoilecgonina. Cuad. Med. Forense 2003, 13–24. [Google Scholar] [CrossRef][Green Version]
- Lizasoain, I.; Moro, M.A.; Lorenzo, P. Cocaína: Aspectos farmacológicos. Adicciones 2002, 14, 57–64. [Google Scholar] [CrossRef]


| Suicide Mechanisms | Total Suicide Cases | Positive Toxicology | Negative Toxicology | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total N = 355, n (%) (Mean ± SD) * | Male | Female | P1 | Total | Male | Female | P2 | Total | Male | Female | P3 | |
| TOTAL | 355 (100) 52.09 ± 17.47 | 273 (76.9) 53.02 ± 17.85 | 82 (23.1) 49.00 ± 15.84 | 0.067 | 202 (56.9) 50.60 ± 15.33 | 155 (76.7) 50.83 ± 15.13 | 47 (23.2) 49.85 ± 16.13 | <0.001 a 0.702 | 153 (43.1) 54.07 ± 19.82 | 118 (77.1) 55.91 ± 20.611 | 35 (22.8) 47.86 ± 15.60 | 0.034 d |
| CO poisoning | 2 (0.6) 57.00 ± 2.82 | 2 (100) 57.00 ± 2.82 | - - | - - | 1 (0.5) 55.00 ± 0.00 | 1 (0.6) 59.78 ± 12.82 | - - | - - | 1 (0.6) 59.00 ± 0.00 | 1 (0.8) 59.00 ± 0.00 | - - | - - |
| Drowning | 7 (2.0) 66.43 ± 16.64 | 5 (71.4) 72.20 ± 16.42 | 2 (28.5) 52.00 ± 0.00 | - 0.161 | 1 (0.5) 52.00 ± 0.00 | - - | 1 (2.1) 52.00 ±0.00 | - - | 6 (3.9) 68.83 ± 16.84 | 5 (4.2) 72.20 ±16.42 | 1 (2.8) 52.00 ± 0.00 | 1.000 |
| Drug overdose | 46 (13.0) 51.11 ± 16.16 | 32 (69.6) 53.78 ± 15.13 | 14 (30.4) 45.00 ± 17.33 | 0.090 | 46 (22.7) 51.11 ± 16.16 | 32 (20.6) 53.78 ± 15.13 | 14 (29.0) 45.00 ± 17.33 | 0.233 0.090 | - - | - - | - - | - - |
| Gunshot wounds | 26 (7.3) 55.15 ± 17.65 | 25 (96.2) 55.64 ± 17.84 | 1 (3.8) 43.00 ± 0.01 | - - | 12 (5.9) 51.58 ± 18.84 | 12 (7.7) 51.58 ±18.84 | - - | - - | 14 (9.1) 58.21 ± 16.65 | 13 (11.0) 59.38 ± 16.72 | 1 (2.8) 43.00 ±0.00 | 0.192 |
| Hanging | 176 (49.6) 53.11 ± 17.60 | 150 (85.2) 53.30 ± 17.52 | 26 (14.7) 52.04 ± 18.35 | 0.737 | 92 (45.5) 51.15 ±14.95 | 78 (50.3) 51.01 ± 14.47 | 14 (29.7) 51.93 ± 18.00 | 0.019 b 0.834 | 84 (54.9) 55.26 ± 19.98 | 72 (61.0) 55.78 ± 20.10 | 12 (34.2) 52.17 ± 19.55 | 0.007 d 0.564 |
| Jumping from a height | 76 (21.4) 47.39 ± 17.69 | 43 (56.6) 46.88 ± 20.18 | 33 (43.4) 48.06 ± 14.09 | 0.775 | 36 (17.8) 48.36 ± 15.04 | 22 (14.2) 45.91 ±15.81 | 14 (29.7) 52.21± 3.40 | 0.028 c 0.152 | 40 (26.1) 46.53 ± 19.93 | 21 (17.8) 47.90 ± 24.30 | 19 (54.2) 45.00 ±14.14 | <0.001 e 0.651 |
| Stab wounds | 8 (2.2) 56.38 ± 15.96 | 6 (75.0) 57.83 ± 18.57 | 2 (25.0) 52.00 ± 2.82 | 0.688 | 6 (2.9) 51.33 ±10.59 | 5 (3.2) 51.60 ±11.82 | 1 (2.1) 50.00 ± 0.00 | - - | 2 (1.3) 71.50 ± 24.74 | 1 (0.8) 89.00 ±0.00 | 1 (2.8) 54.00 ± 0.00 | 0.406- |
| Suffocation | 4 (1.10) 54.25 ± 15.69 | 2 (50.0) 49.50 ± 0.7 | 2 (50.0) 59.00 ± 25.45 | 0.650 | 2 (0.9) 59.00 ± 25.45 | - - | 2 (4.2) 59.00 ± 25.45 | - - | 2 (1.3) 49.50 ± 0.70 | 2 (1.6) 49.50 ± 0.70 | - - | - - |
| Traffic accident | 10 (2.8) 51.10 ± 17.51 | 8 (80.0) 53.88 ± 18.52 | 2 (20.0) 40.00 ± 7.07 | 0.345 | 6 (2.9) 45.17 ±17.52 | 5 (3.2) 47.20 ± 18.78 | 1 (2.1) 35.00 ± 0.00 | 1.000- | 4 (2.6) 60.00 ± 15.25 | 3 (2.5) 65.00 ±14.10 | 1 (2.8) 45.00 ± 0.00 | 1.000 - |
| Positive Toxicology, n = 202 | |||
|---|---|---|---|
| Suicide mechanisms | 1 toxic n = 133, (65.8%) | ≥2 toxics n = 69, (34.2%) | p |
| CO poisoning (n = 1) | 1 (0.7) | 0 (0.0) | - |
| Drowning (n = 1) | 0 (0.0) | 1 (1.5) | 0.342 |
| Drug overdose (n = 46) | 17 (12.8) | 29 (42.0) | <0.001 a |
| Gunshot wounds (n = 12) | 6 (4.51) | 6 (8.70) | 0.346 |
| Hanging (n = 92) | 71 (53.4) | 21 (30.4) | 0.003 b |
| Jumping from a height (n = 36) | 29 (21.8) | 7 (10.1) | 0.052 |
| Stab wounds (n = 6) | 2 (1.5) | 4 (5.8) | 0.183 |
| Suffocation (n = 2) | 2 (1.5) | 0 (0) | 0.548 |
| Traffic accident (n = 6) | 5 (3.8) | 1 (1.5) | 0.666 |
| Types of Toxics | Total N = 202, (%) | Male n = 273, (%) | Female n = 82 (%) | p | |
|---|---|---|---|---|---|
| Medicines | Total | 158 (46.9) | 106 (40.3) | 52 (70.3) | <0.001 a |
| Benzodiazepines | 104 (30.9) | 72 (27.4)c | 32 (43.2) | 0.011 b | |
| Alprazolam | 17 (5.0) | 11 (4.2) | 6 (8.1) | 0.224 | |
| Diazepam | 10 (3.0) | 8 (3.0) | 2 (2.7) | 1.000 | |
| Lorazepam | 27 (8.0) | 16 (6.1) | 11 (14.9) | 0.026 c | |
| Nordiazepam | 50 (14.8) | 37 (14.1) | 13 (17.6) | 0.462 | |
| SNRIs Venlafaxine | 31 (9.2) | 20 (7.6) | 11 (14.9) | 0.068 | |
| NSAIDs | 13 (3.9) | 9 (3.4) | 4 (5.4) | 0.493 | |
| Ibuprofen | 3 (0.9) | 2 (0.8) | 1 (1.4) | 0.526 | |
| Metamizole | 1 (0.3) | 1 (0.4) | 0 (0.0) | - | |
| Paracetamol | 9 (2.7) | 6 (2.3) | 3 (4.0) | 0.418 | |
| Opioids | 10 (2.9) | 5 (1.9) | 5 (6.8) | 0.045 d | |
| Morphine | 5 (1.5) | 3 (1.1) | 2 (2.7) | 0.303 | |
| 6-monoacetylmorphine | 3 (0.9) | 2 (0.8) | 1 (1.4) | 0.526 | |
| Tramadol | 2 (0.6) | 0 (0.0) | 2 (2.7) | - | |
| Drugs of abuse | Total | 164 (48.7) | 146 (55.5) a | 18 (24.3) | <0.001 e |
| Alcohol | 73 (21.7) | 63 (24.0)b | 10 (13.5) | 0.057 | |
| Amphetamines | 2 (0.6) | 1 (0.4) | 1 (1.4) | 0.391 | |
| Cocaine and metabolites | 55 (16.3) | 53 (20.2) | 2 (2.7) | 0.000 f | |
| Cocaine | 13 (3.9) | 13 (5.0) | 0 (0.0) | - | |
| Benzoylecgonine | 21 (6.2) | 20 (7.6) | 1 (1.4) | 0.056 | |
| Ecgonine methyl ester | 18 (5.3) | 17 (6.5) | 1 (1.4) | 0.138 | |
| Ethylbenzoylecgonine | 2 (0.6) | 2 (0.8) | 0 (0.0) | - | |
| Methylbenzoylecgonine | 1 (0.3) | 1 (0.4) | 0 (0.0) | - | |
| Cannabinoids | 28 (8.3) | 23 (8.7) | 5 (6.8) | 0.642 | |
| Δ(9)-THC | 2 (0.6) | 2 (0.8) | 0 (0.0) | - | |
| Cannabidiol | 9 (2.7) | 7 (2.7) | 2 (2.7) | 1.000 | |
| Cannabinol | 17 (5.0) | 14 (5.3) | 3 (4.0) | 1.000 | |
| Methadone and metabolites | 6 (1.8) | 6 (2.3) | 0 (0.0) | 0.343 | |
| Methadone | 3 (0.9) | 3 (1.1) | 0 (0.0) | - | |
| EDDP | 3 (0.9) | 3 (1.1) | 0 (0.0) | - | |
| Gas | Carbon monoxide | 11 (3.3) | 8 (3.0) | 3 (4.0) | 0.712 |
| Toxin | Cyanide | 3 (0.9) | 2 (0.8) | 1 (1.4) | 0.526 |
| Herbicide | 1,1′-dimethyl-4,4′-bipyridyl dichloride | 1 (0.3) | 1 (0.4) | 0 (0.0) | - |
| Combinations of Toxics, n (%) | Suicides, n = 63 | ||||
|---|---|---|---|---|---|
| Alcohol+ | Alprazolam | 1 | |||
| +Cocaine | 1 | ||||
| +Nordiazepam | 1 | ||||
| +Nordiazepam + Diazepam + Cannabis | 1 | ||||
| Cannabis | 1 | ||||
| Cocaine | 5 | ||||
| +Cannabis | 3 | ||||
| +Amphetamines + Paracetamol | 1 | ||||
| Diazepam | +Nordiazepam | 3 | |||
| Paracetamol + Venlafaxine | 1 | ||||
| Carbon monoxide | 3 | ||||
| +Cannabis | 1 | ||||
| +Paracetamol | 1 | ||||
| Lorazepam | 3 | ||||
| Morphine | +Cannabis | 1 | |||
| Nordiazepam | 3 | ||||
| Paracetamol | 1 | ||||
| Venlafaxine | 1 | ||||
| Cannabis+ | Nordiazepam | 1 | |||
| Cocaine+ | Alprazolam + Cannabis | 4 | |||
| Nordiazepam | +Lorazepam | 1 | |||
| +Morphine | 1 | ||||
| +Methadone | 1 | ||||
| Ibuprofen + Paracetamol | 1 | ||||
| Cyanide+ | Lorazepam | 1 | |||
| Methadone+ | Cannabis | 1 | |||
| Carbon monoxide + | Alprazolam | 1 | |||
| Nordiazepam + Cannabis | 1 | ||||
| Morphine+ | Amphetamines + Cannabis | 1 | |||
| Nordiazepam+ | Diazepam | 4 | |||
| +Paracetamol + Tramadol | 1 | ||||
| Lorazepam | 2 | ||||
| +Paracetamol + Tramadol | 1 | ||||
| Venlafaxine+ | Alprazolam | 1 | |||
| Cannabis | 1 | ||||
| Lorazepam | 2 | ||||
| Nordiazepam | 4 | ||||
| + Lorazepam | 1 | ||||
| Types of Toxics | Concentration Postmortem (Mean ± SD) | Concentration Range (Min-Max) | Lethal Reference Dose * | Number of Cases with Lethal Doses (n = 28) | |
|---|---|---|---|---|---|
| Medicines, n | Benzodiazepines, n | ||||
| Alprazolam, 6 | 0.270 ± 0.333 | 0.04–1.00 | 0.13–2.1 | 3 | |
| Diazepam, 7 | 2.433 ± 2.087 | 0.31–6.85 | 5–30 | 1 | |
| Lorazepam, 8 | 0.531 ± 0.283 | 0.03–1.00 | 0.04–0.8 | 7 | |
| Nordiazepam, 11 | 1.885 ± 1.289 | 0.19–4.48 | 5–30 | - | |
| SNRIs, n | |||||
| Venlafaxine, 6 | 1.260 ± 1.368 | 0.05–4.12 | 1.3–20 | 2 | |
| NSAIDs, n | |||||
| Paracetamol, 4 | 15.150 ± 20.345 | 0.85–50.15 | 81–1050 | - | |
| Opioids, n | |||||
| Morphine, 4 | 0.468 ± 0.333 | 0.10–1.00 | 0.2–7.2 | 3 | |
| 6-monoacetylmorphine, 2 | 0.380 ± 0.080 | 0.30–0.46 | - | - | |
| Tramadol, 1 | 1.250 ± 0.000 | - | 1.3–20 | - | |
| Drugs of abuse, n | Alcohol, 11 | 1.269 ± 0.698 | 0.19–2.32 | >3.2 | - |
| Amphetamines, 1 | <0.01 | 0.5–41 | - | ||
| Cocaine and metabolites, n | |||||
| Cocaine, 1 | 1.08 ± 0.000 | - | 0.1–330 | 1 | |
| Benzoylecgonine, 2 | 1.105 ± 0.275 | 0.83–1.38 | 0.05–26 | 2 | |
| Ecgonine methyl ester, 1 | 0.12 ± 0.000 | - | - | - | |
| Cannabinoids | |||||
| Cannabidiol, 4 | 0.485 ± 0.425 | 0.05–1.00 | - | - | |
| Cannabinol, 2 | 1.000 ± 0.000 | 1.00–1.00 | - | - | |
| Gas, n | Carbon monoxide, 8 | 53.125 ± 18.864 | 5.00–70.00 | 33–72 | 7 |
| Toxic, n | Cyanide, 2 | 31.575 ± 6.575 | 4.15–38.15 | 1–100 | 2 |
| Herbicide, n | 1,1′-dimethyl-4,4′-bipyridyl dichloride, 1 | 3.400 ± 0.000 | 3.40–3.40 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Collados-Ros, A.; Torres-Sánchez, C.; Pérez-Cárceles, M.D.; Luna, A.; Legaz, I. Suicidal Behavior and Its Relationship with Postmortem Forensic Toxicological Findings. Toxics 2022, 10, 319. https://doi.org/10.3390/toxics10060319
Collados-Ros A, Torres-Sánchez C, Pérez-Cárceles MD, Luna A, Legaz I. Suicidal Behavior and Its Relationship with Postmortem Forensic Toxicological Findings. Toxics. 2022; 10(6):319. https://doi.org/10.3390/toxics10060319
Chicago/Turabian StyleCollados-Ros, Aurelia, Carmen Torres-Sánchez, María Dolores Pérez-Cárceles, Aurelio Luna, and Isabel Legaz. 2022. "Suicidal Behavior and Its Relationship with Postmortem Forensic Toxicological Findings" Toxics 10, no. 6: 319. https://doi.org/10.3390/toxics10060319
APA StyleCollados-Ros, A., Torres-Sánchez, C., Pérez-Cárceles, M. D., Luna, A., & Legaz, I. (2022). Suicidal Behavior and Its Relationship with Postmortem Forensic Toxicological Findings. Toxics, 10(6), 319. https://doi.org/10.3390/toxics10060319









