Comparison in Four Different Implant Systems of Mechanical Resistance to Maximal Stress in Prosthetic Screws—An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Characterization
2.2. Sample Characteristics
2.3. Inclusion and Exclusion Criteria
2.4. Data Collection
- (1)
- All prosthetic screws from the manufacturers were labeled with serial number and control date: 10 Megagen® prosthetic screws; 10 Dentium® prosthetic screws; 10 BIOMET 3i® prosthetic screws and 10 BTI® prosthetic screws.
- (2)
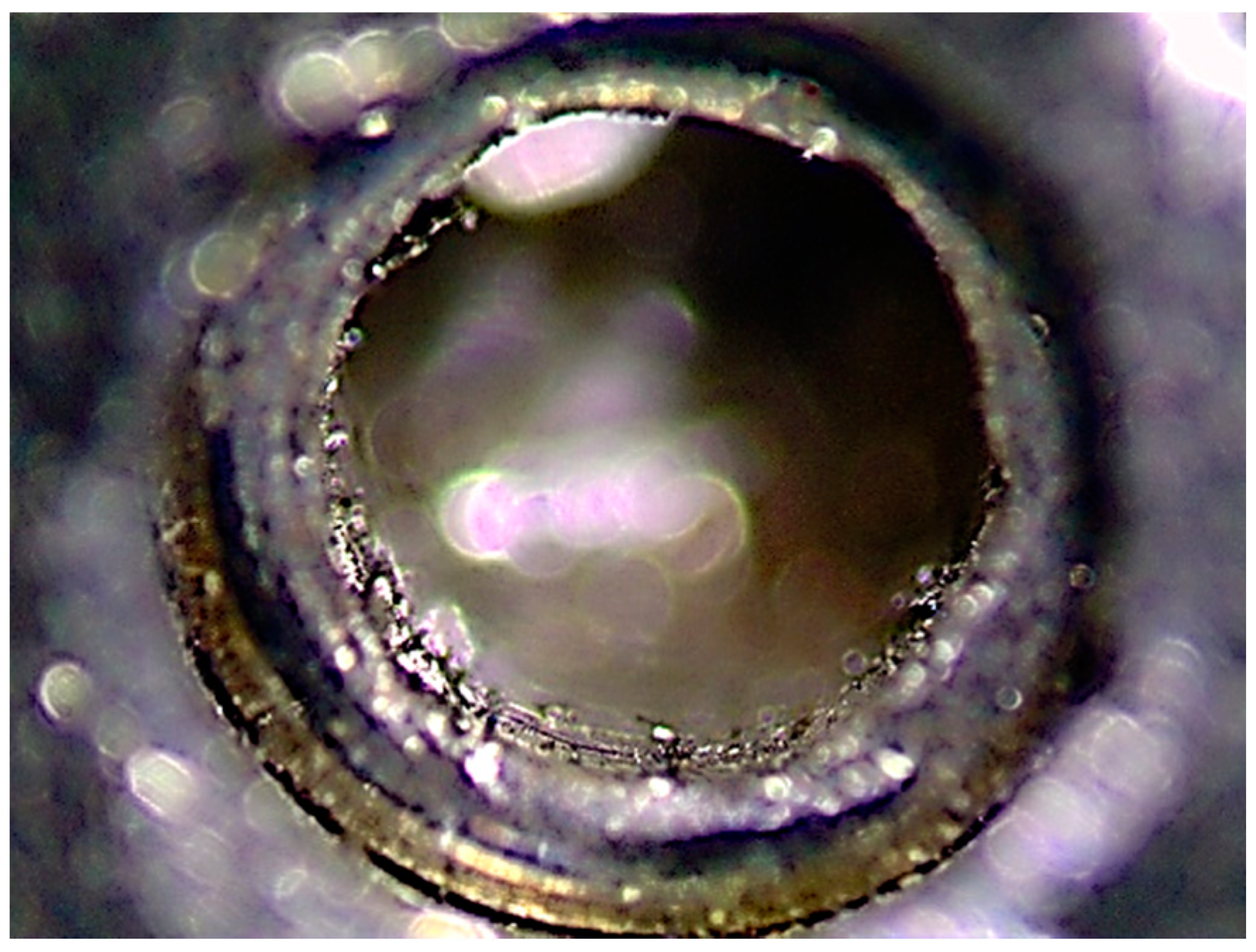
- The presence of anomalies and defects was assessed with a stereoscope (Olympus® SZ61—Tokyo, Japan), and a 90× magnifier was used to evaluate any changes in the surfaces.
- (3)
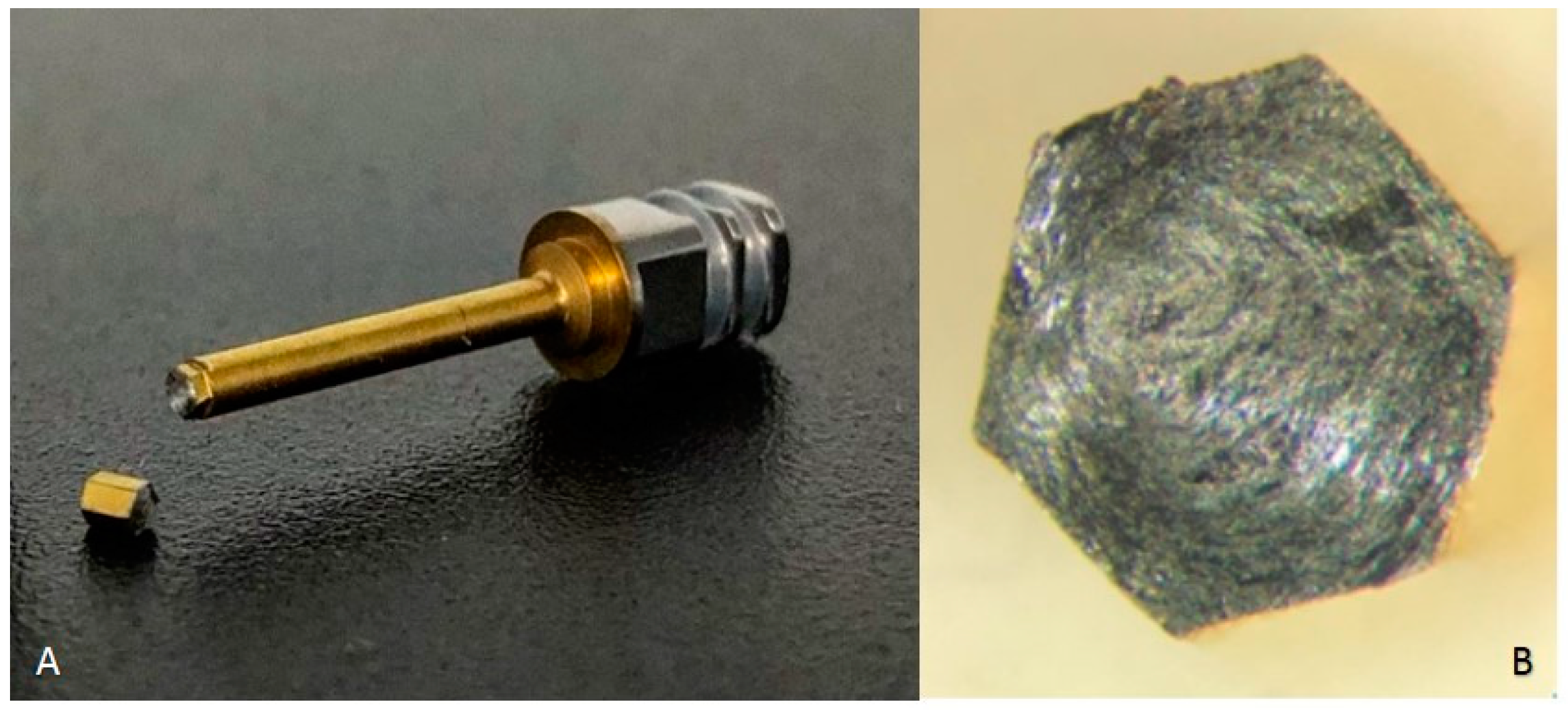
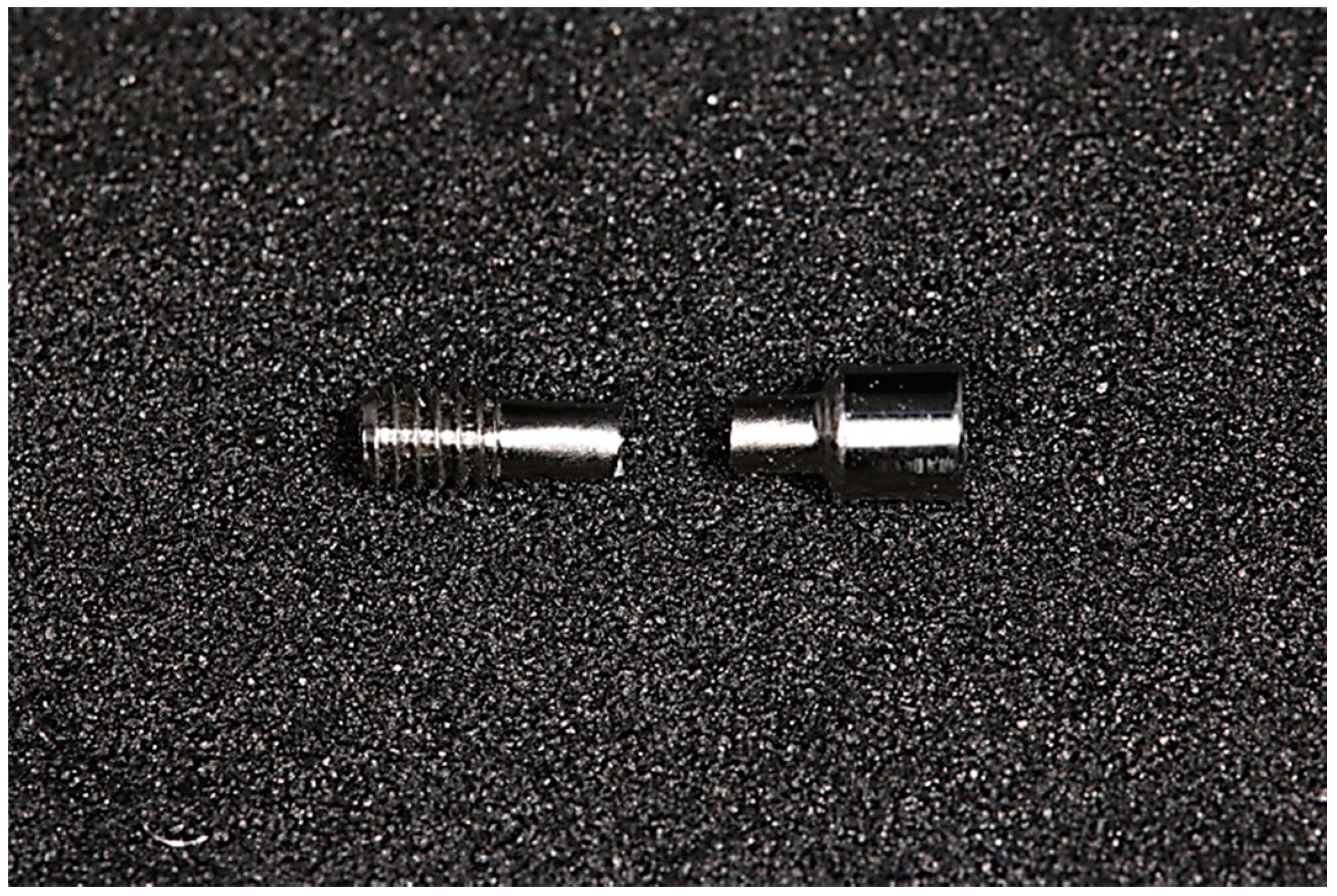
- The prosthetic abutment was coupled to the implant analog (of the corresponding brands) with the prosthetic screw (Figure 2) with the respective manual key. The prosthetic screw was tightened by hand until there were no gaps between the two parts.A brand-new manual screwdriver was used every time a prosthetic screw was tested.
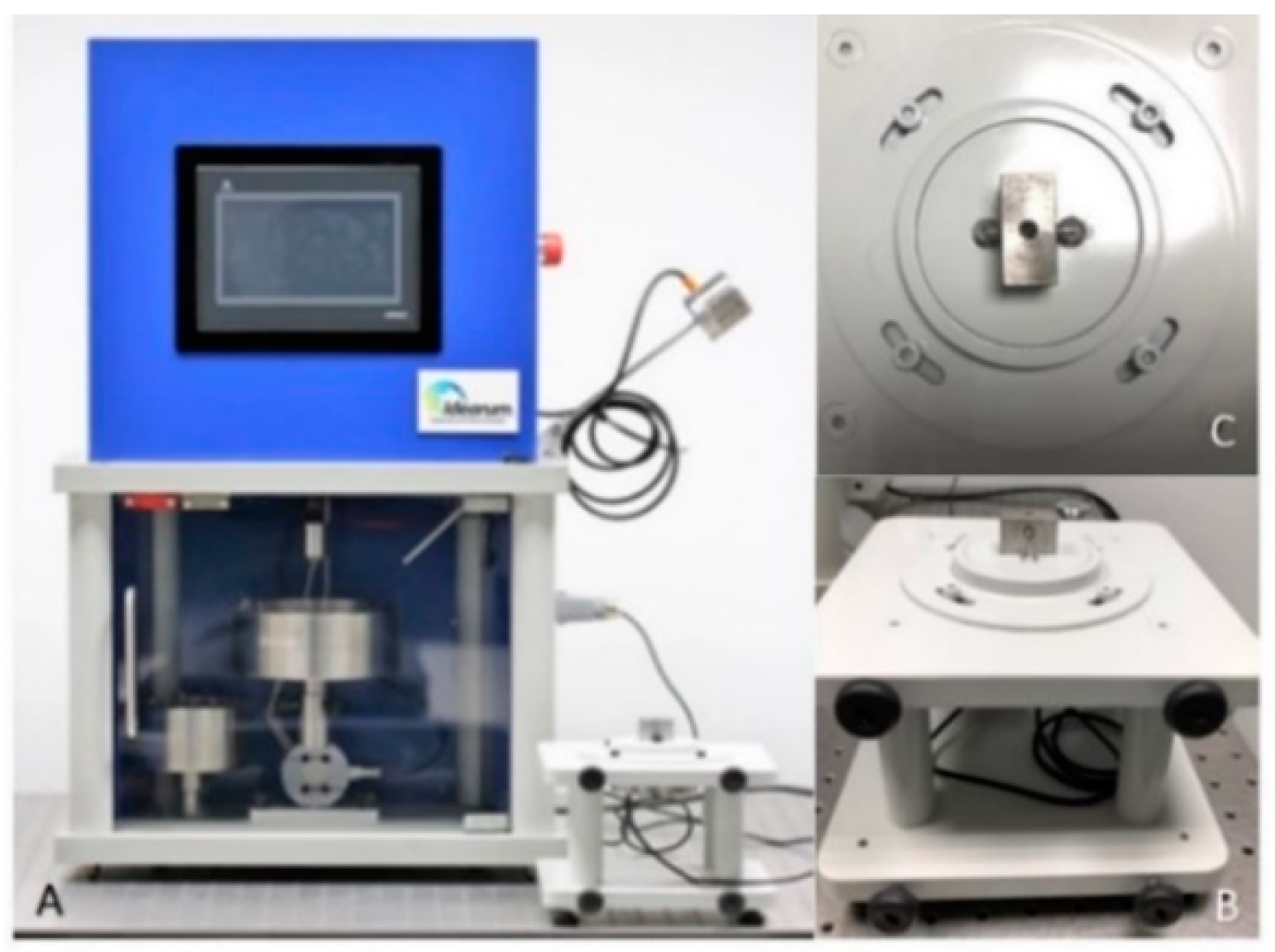
- (4)
- The two parts were placed in a load cell (Figure 3B,C), connected to the CS-Dental Testing Machine® (Figure 3A), and stabilized. CS® Dental Testing Machine is a fatigue test device built in agreement with 2006/42/CE safety of machines and the norms EN 12100-1/2, EN 954-1, EN 1037, EN 61310-1/2, EN 60204-1, EN ISSO 14121-1, and EN ISSO 13850.The screws to be tested were subjected to a torsional force with a torque wrench until fracture occurred. A brand-new torque wrench was also used every time a prosthetic screw was tested.
- (5)
- The fracture points were automatically recorded in the machine and compared between all samples.
- (6)
- The CS-Dental Testing Machine® (Barcelona, Spain) Excel file was stored on a computer for further graphical and value analyses.
- (7)
- The fractured parts were analyzed under an optical microscope to observe microscopic fracture characteristics.
2.5. Statistical Analysis
3. Results
4. Discussion
- i.
- ii.
- Increasing the screw torque above 30 Ncm could be beneficial for implant–abutment stability and reducing screw loosening [23].
5. Conclusions
- (1)
- The greatest resistance, evidenced by the highest load torque before screw fracture, was achieved by BTI®;
- (2)
- The maximal average fatigue loads were within the parameters defined by the manufacturers. However, there were prosthetic screws that did not reflect this reference value; and
- (3)
- There seemed to be a correlation between better results for screws and surface treatment.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ring, M.E. A thousand years of dental implants: A definitive history—Part 1. Compend. Contin. Educ. Dent. 1995, 16, 1060–1062. [Google Scholar] [PubMed]
- Bornstein, M.M.; Halbritter, S.; Harnisch, H.; Weber, H.P.; Buser, D. A retrospective analysis of patients referred for implant placement to a specialty clinic: Indications, surgical procedures, and early failures. Int. J. Oral Maxillofac. Implant. 2008, 23, 1109–1116. [Google Scholar]
- Klokkevold, P.R.; Han, T.J. How do smoking, diabetes, and periodontitis affect outcomes of implant treatment? Int. J. Oral Maxillofac. Implant. 2007, 22, 173–202. [Google Scholar]
- Freese, H.L.; Volas, M.G.; Wood, J.R. Metallurgy and Technological Properties of Titanium and Titanium Alloys. In Titanium in Medicine; Freese, H.L., Volas, M.G., Wood, J.R., Eds.; Engineering Materials; Springer: Berlin/Heidelberg, Germany, 2001; pp. 25–51. [Google Scholar]
- Patterson, E.A.; Johns, R.B. Theoretical analysis of the fatigue life of fixture screws in osseointegrated dental implants. Int. J. Oral Maxillofac. Implant. 1992, 7, 26–33. [Google Scholar]
- Pjetursson, B.E.; Bragger, U.; Lang, N.P.; Zwahlen, M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin. Oral Implant. Res. 2007, 18, 97–113. [Google Scholar] [CrossRef]
- Andersson, B.; Odman, P.; Carlsson, L.; Branemark, P.I. A new Branemark single tooth abutment: Handling and early clinical experiences. Int. J. Oral Maxillofac. Implant. 1992, 7, 105–111. [Google Scholar]
- Cibirka, R.M.; Nelson, S.K.; Lang, B.R.; Rueggeberg, F.A. Examination of the implant-abutment interface after fatigue testing. J. Prosthet. Dent. 2001, 85, 268–275. [Google Scholar] [CrossRef]
- Gratton, D.G.; Aquilino, S.A.; Stanford, C.M. Micromotion and dynamic fatigue properties of the dental implant-abutment interface. J. Prosthet. Dent. 2001, 85, 47–52. [Google Scholar] [CrossRef]
- Jemt, T. Modified single and short-span restorations supported by osseointegrated fixtures in the partially edentulous jaw. J. Prosthet. Dent. 1986, 55, 243–247. [Google Scholar] [CrossRef]
- Jorneus, L.; Jemt, T.; Carlsson, L. Loads and designs of screw joints for single crowns supported by osseointegrated implants. Int. J. Oral Maxillofac. Implant. 1992, 7, 353–359. [Google Scholar]
- Lang, L.A.; Kang, B.; Wang, R.F.; Lang, B.R. Finite element analysis to determine implant preload. J. Prosthet. Dent. 2003, 90, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Binon, P.P. The external hexagonal interface and screw-joint stability: A primer on threaded fasteners in implant dentistry. J. Prosthet. Dent. 2000, 23, 91–105. [Google Scholar]
- Burguete, R.L.; Johns, R.B.; King, T.; Patterson, E.A. Tightening characteristics for screwed joints in osseointegrated dental implants. J. Prosthet. Dent. 1994, 71, 592–599. [Google Scholar] [CrossRef]
- Haack, J.E.; Sakaguchi, R.L.; Sun, T.; Coffey, J.P. Elongation and preload stress in dental implant abutment screws. Int. J. Oral Maxillofac. Implant. 1995, 10, 529–536. [Google Scholar]
- Khraisat, A.; Abu-Hammad, O.; Al-Kayed, A.M.; Dar-Odeh, N. Stability of the implant/abutment joint in a single-tooth external-hexagon implant system: Clinical and mechanical review. Clin. Implant. Dent. Relat. Res. 2004, 6, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.B.; Nicholls, J.I. The effect of 3 torque delivery systems on gold screw preload at the gold cylinder-abutment screw joint. Int. J. Oral Maxillofac. Implant. 2002, 17, 175–183. [Google Scholar]
- Yokoyama, K.; Ichikawa, T.; Murakami, H.; Miyamoto, Y.; Asaoka, K. Fracture mechanisms of retrieved titanium screw thread in dental implant. Biomaterials 2002, 23, 2459–2465. [Google Scholar] [CrossRef]
- Guda, T.; Ross, T.A.; Lang, L.A.; Millwater, H.R. Probabilistic analysis of preload in the abutment screw of a dental implant complex. J. Prosthet. Dent. 2008, 100, 183–193. [Google Scholar] [CrossRef]
- Ricciardi Coppedê, A.; de Mattos, M.d.G.C.; Rodrigues, R.C.S.; Ribeiro, R.F. Effect of repeated torque/mechanical loading cycles on two different abutment types in implants with internal tapered connections: Anin vitrostudy. Clin. Oral Implant. Res. 2009, 20, 624–632. [Google Scholar] [CrossRef]
- Tsuge, T.; Hagiwara, Y. Influence of lateral–oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent. Mater. J. 2009, 28, 373–381. [Google Scholar] [CrossRef]
- Dailey, B.; Jordan, L.; Blind, O.; Tavernier, B. Axial displacement of abutments into implants and implant replicas, with the tapered cone-screw internal connection, as a function of tightening torque. Int. J. Oral Maxillofac. Implant. 2009, 24, 251–256. [Google Scholar]
- Manda, M.G.; Psyllaki, P.P.; Tsipas, D.N.; Koidis, P.T. Observations on an in-vivo failure of a titanium dental implant/abutment screw system: A case report. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 89, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Winkler, S.; Ring, K.; Ring, J.D.; Boberick, K.G. Implant screw mechanics and the settling effect: An overview. J. Oral Implantol. 2003, 29, 242–245. [Google Scholar] [CrossRef]
- Gil, F.J.; Herrero-Climent, M.; Lázaro, P.; Rios, J.V. Implant–abutment connections: Influence of the design on the microgap and their fatigue and fracture behavior of dental implants. J. Mater. Sci. Mater. Med. 2014, 25, 1825–1830. [Google Scholar] [CrossRef]
- Theoharidou, A.; Petridis, H.P.; Tzannas, K.; Garefis, P. Abutment screw loosening in single-implant restorations: A systematic review. Int. J. Oral Maxillofac. Implant. 2008, 23, 681–690. [Google Scholar]
- Siamos, G.; Winkler, S.; Boberick, K.G. The relationship between implant preload and screw loosening on implant-supported prostheses. J. Oral Implantol. 2002, 28, 67–73. [Google Scholar] [CrossRef]
- Cho, S.-C.; Small, P.-N.; Elian, N.; Tarnow, D. Screw loosening for standard and wide diameter implants in partially edentulous cases: 3- to 7-year longitudinal data. Implant. Dent. 2004, 13, 245–250. [Google Scholar] [CrossRef]
- Standlee, J.P.; Caputo, A.A.; Chwu, M.Y.; Sun, T.T. Accuracy of mechanical torque-limiting devices for implants. Int. J. Oral Maxillofac. Implant. 2002, 17, 220–224. [Google Scholar]
- Khraisat, A.; Baqain, Z.H.; Smadi, L.; Nomura, S.; Miyakawa, O.; Elnasser, Z. Abutment rotational displacement of external hexagon implant system under lateral cyclic loading. Clin. Implant. Dent. Relat. Res. 2006, 8, 95–99. [Google Scholar] [CrossRef]
- Zinsli, B.; Sägesser, T.; Mericske, E.; Mericske-Stern, R. Clinical evaluation of small-diameter ITI implants: A prospective study. Int. J. Oral Maxillofac. Implant. 2004, 19, 92–99. [Google Scholar]
- Barbosa, G.A.S.; Bernardes, S.R.; Neves, F.D.D.; Fernandes Neto, A.J.; Mattos, M.D.G.C.D.; Ribeiro, R.F. Relation between implant/abutment vertical misfit and torque loss of abutment screws. Braz. Dent. J. 2008, 19, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Figueira, D.C.; Rios, P.R. Influence of the coating material on the loosing of dental implant abutment screw joints. Mater. Sci. Eng. C 2006, 26, 1361–1366. [Google Scholar] [CrossRef]
- Tzenakis, G.K.; Nagy, W.W.; Fournelle, R.A.; Dhuru, V.B. The effect of repeated torque and salivary contamination on the preload of slotted gold implant prosthetic screws. J. Prosthet. Dent. 2002, 88, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Ballini, A.; Capodiferro, S.; Toia, M.; Cantore, S.; Favia, G.; de Frenza, G.; Grassi, F.R. Evidence-Based Dentistry: What’s New? Int. J. Med. Sci. 2007, 4, 174–178. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kofro, M.D.; Carstens, M.; Fu, C.; Wen, H.B. In vitro assessment of connection strength and stability of internal implant-abutment connections. Clin. Biomech. 2019, 65, 92–99. [Google Scholar] [CrossRef]


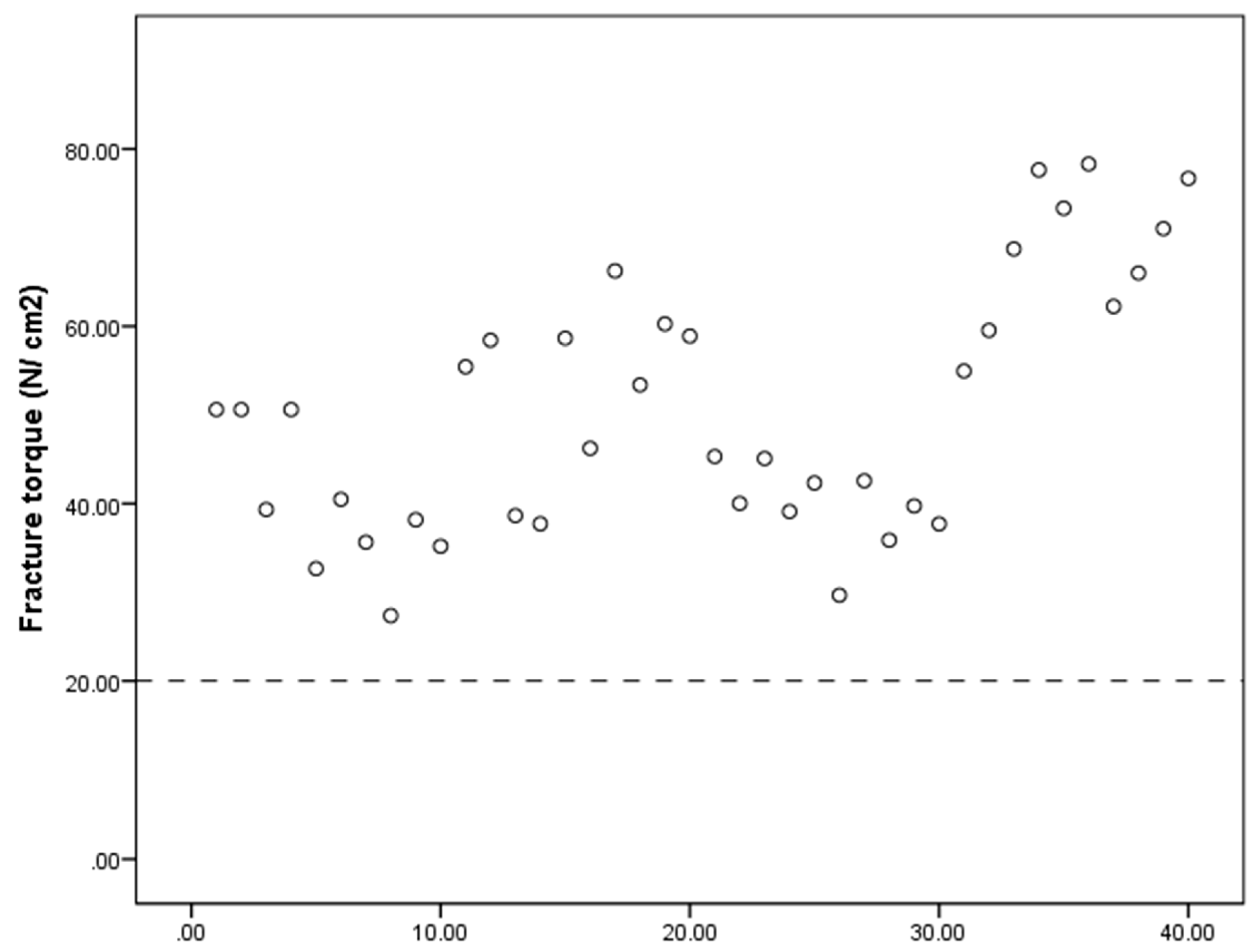
| Sample | Fracture Point (Ncm) | |||
|---|---|---|---|---|
| Megagen® | Dentium® | BIOMET 3i® | BTI® | |
| 1 | 50.60 | 55.43 | 45.31 | 54.95 |
| 2 | 50.60 | 58.42 | 40.02 | 59.54 |
| 3 | 39.33 | 38.64 | 45.08 | 68.72 |
| 4 | 50.60 | 37.72 | 39.10 | 77.63 |
| 5 | 32.66 | 58.65 | 42.32 | 73.31 |
| 6 | 40.48 | 46.23 | 29.67 | 78.30 |
| 7 | 35.65 | 66.24 | 42.57 | 62.24 |
| 8 | 27.36 | 13.18 | 35.88 | 66.01 |
| 9 | 38.18 | 60.26 | 22.54 | 71.01 |
| 10 | 35.19 | 58.89 | 37.71 | 76.68 |
| Megagen® | Dentium® | BIOMET 3i® | BTI® | |
|---|---|---|---|---|
| Mean (Ncm) | 40.07 | 53.39 | 39.74 | 68.84 |
| Brand | M | DP | Reference Value | t-Test (p-Value) |
|---|---|---|---|---|
| Megagen® (n = 10) | 40.07 | 8.14 | 35 N/cm2 | t(9) = 1.97 (p = 0.081) |
| Dentium® (n = 10) | 53.39 | 9.51 | 30 N/cm2 | t(9) = 7.78 (p < 0.001) |
| BIOMET 3i® (n = 10) | 39.74 | 4.66 | 20 N/cm2 | t(9) = 9.58 (p < 0.001) |
| BTI® (n =10) | 68.84 | 8.05 | 35 N/cm2 | t(9) = 19.17 (p < 0.001) |
| Brand | n | % |
|---|---|---|
| Megagen® (n = 10) | 2 | 20.0% |
| Dentium® (n = 10) | 0 | 0% |
| BIOMET 3i® (n = 10) | 0 | 0% |
| BTI® (n = 10) | 0 | 0% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barreiros, P.; Neves, L.; Aroso, C.; Mendes, J.M.; Silva, A.S. Comparison in Four Different Implant Systems of Mechanical Resistance to Maximal Stress in Prosthetic Screws—An In Vitro Study. Dent. J. 2020, 8, 116. https://doi.org/10.3390/dj8040116
Barreiros P, Neves L, Aroso C, Mendes JM, Silva AS. Comparison in Four Different Implant Systems of Mechanical Resistance to Maximal Stress in Prosthetic Screws—An In Vitro Study. Dentistry Journal. 2020; 8(4):116. https://doi.org/10.3390/dj8040116
Chicago/Turabian StyleBarreiros, Pedro, Luís Neves, Carlos Aroso, José M. Mendes, and António Sérgio Silva. 2020. "Comparison in Four Different Implant Systems of Mechanical Resistance to Maximal Stress in Prosthetic Screws—An In Vitro Study" Dentistry Journal 8, no. 4: 116. https://doi.org/10.3390/dj8040116
APA StyleBarreiros, P., Neves, L., Aroso, C., Mendes, J. M., & Silva, A. S. (2020). Comparison in Four Different Implant Systems of Mechanical Resistance to Maximal Stress in Prosthetic Screws—An In Vitro Study. Dentistry Journal, 8(4), 116. https://doi.org/10.3390/dj8040116








