‘Message to Dentist’: Facilitating Communication with Dentally Anxious Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
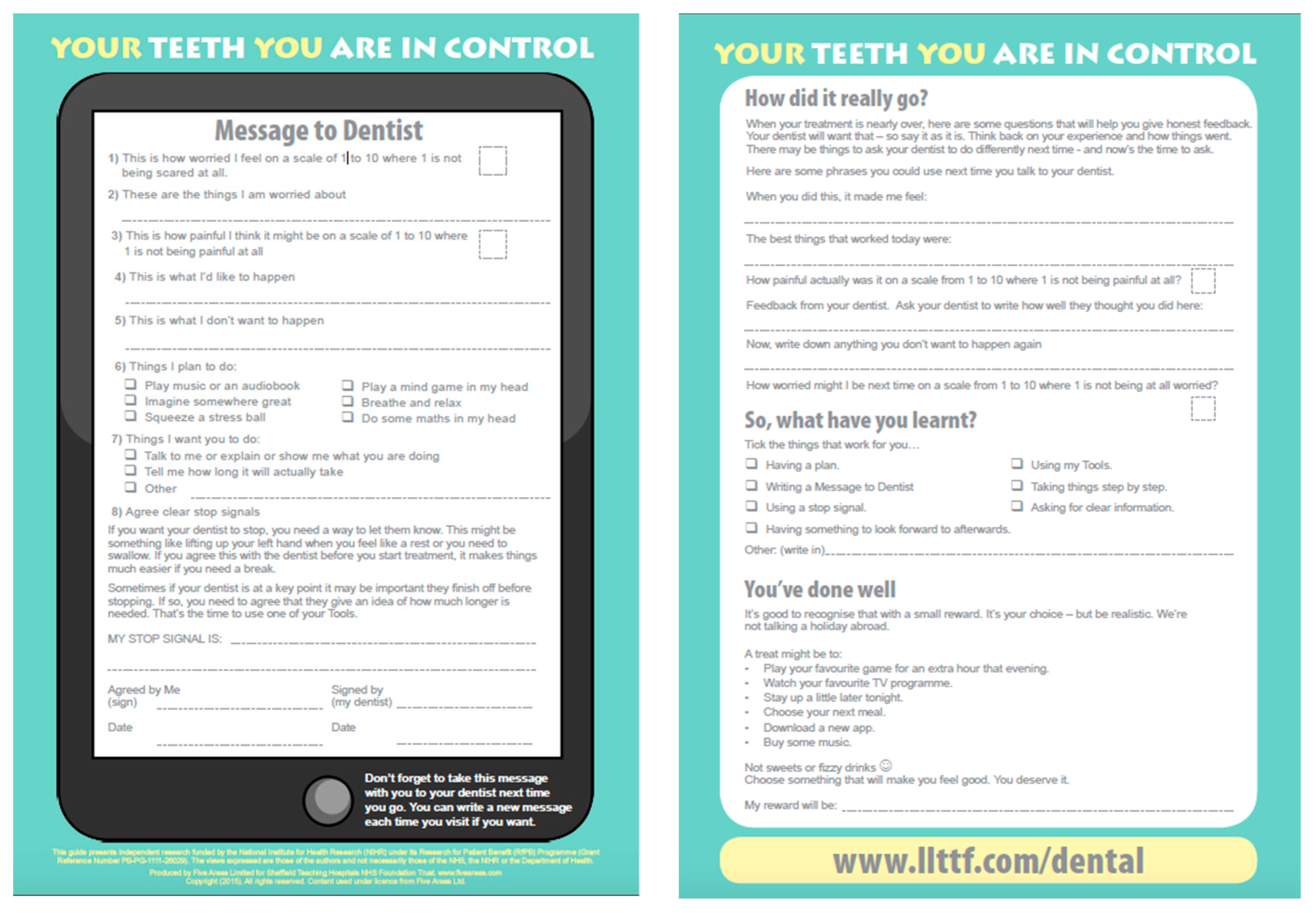
- Self-report worry score from 1–10 (10 = most worried);
- Things which they are worried about;
- Self-report anticipated pain score from 1–10 (10 = worst pain);
- Items of care that they are willing to accept;
- Things that they do not want to happen;
- Things they plan to do, to help them cope (from a list of suggested options);
- An agreed stop signal (signed by patient and clinician);
- Things that worked well;
- Self-report worry score from 0–10 (10 = most worried);
- Self-report anticipated pain score from 0–10 (10 = worst pain);
- ‘Reward’ for progress made.
2.2. Data Processing and Analysis
3. Results
3.1. Participants
3.2. Worry and Pain Scores
3.2.1. Pre- and post-treatment
3.2.2. Hospital and practice patients
3.2.3. Gender
3.3. What Children Said They Were Worried About
3.4. What Children Said They Would Like to Happen
3.4.1. Coping plans
3.4.2. Stop signals
3.4.3. Self-reflection
3.4.4. Rewards
4. Discussion
5. Patents
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S.; Salvato, R. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar] [PubMed]
- Merdad, L.; El-Housseiny, A.A. Do children’s previous dental experience and fear affect their perceived oral health-related quality of life (OHRQoL)? BMC Oral Health 2017, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Goettems, M.L.; Shqair, A.Q.; Bergmann, V.F.; Cadermatori, M.G.; Correa, M.B.; Demarco, F.F. Oral health self-perception, dental caries, and pain: The role of dental fear underlying this association. Int. J. Paediatr. Dent. 2018, 28, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Porritt, J.; Marshman, Z.; Rodd, H.D. Understanding children’s dental anxiety and psychological approaches to its reduction. Int. J. Paediatr. Dent. 2012, 22, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Prado, I.M.; Carcavalli, L.; Abreu, L.G.; Serra-Negra, J.M.; Paiva, S.M.; Martins, C.C. Use of distraction techniques for the management of anxiety and fear in pediatric dental practice: A systematic review of randomized controlled trials. Int. J. Paediatr. Dent. 2019. [Google Scholar] [CrossRef] [PubMed]
- Gomes, H.S.; Viana, K.A.; Batista, A.C.; Costa, L.R.; Hosey, M.T.; Newton, T. Cognitive behaviour therapy for anxious paediatric dental patients: A systematic review. Int. J. Paediatr. Dent. 2018, 28, 422–431. [Google Scholar] [CrossRef]
- James, A.C.; James, G.; Cowdrey, F.A.; Soler, A.; Choke, A. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst. Rev. 2015, 18, CD004690. [Google Scholar] [CrossRef]
- Mahdi, M.; Jhawar, S.; Bennett, S.D.; Shafran, R. Cognitive behavioral therapy for childhood anxiety disorders: What happens to comorbid mood and behavioral disorders? A systematic review. J. Affect. Disord. 2019, 251, 141–148. [Google Scholar] [CrossRef]
- Porritt, J.; Rodd, H.; Morgan, A.; Williams, C.; Gupta, E.; Kirby, J.; Creswell, C.; Newton, T.; Stevens, K.; Baker, S.; et al. Development and Testing of a Cognitive Behavioral Therapy Resource for Children’s Dental Anxiety. JDR Clin. Trans. Res. 2017, 2, 23–37. [Google Scholar] [CrossRef]
- Williams, C.; Garland, A. A cognitive-behavioural therapy assessment model for use in everyday clinical practice. Adv. Psychiatr. Treat. 2002, 8, 172–179. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Porritt, J.; Buchanan, H.; Hall, M.; Gilchrist, F.; Marshman, Z. Assessing children’s dental anxiety: A systematic review of current measures. Community Dent. Oral Epidemiol. 2013, 41, 130–142. [Google Scholar] [CrossRef]
- Dailey, Y.M.; Humphris, G.M.; Lennon, M.A. Reducing patients’ state anxiety in general dental practice: A randomized controlled trial. J. Dent. Res. 2002, 81, 319–322. [Google Scholar] [CrossRef]
- Jones, L.M.; Huggins, T.J. The rationale and pilot study of a new paediatric dental patient request form to improve communication and outcomes of dental appointments. Child Care Health Dev. 2013, 39, 869–872. [Google Scholar] [CrossRef]
- Yee, R.; Jones, L.M.; Hosey, M.T. What the child “SAID” to the dentist: A UK randomized controlled trial. Child Care Health Dev. 2017, 43, 926–932. [Google Scholar] [CrossRef]
- Morgan, A.G.; Rodd, H.D.; Porritt, J.M.; Baker, S.R.; Creswell, C.; Newton, T.; Williams, C.; Marshman, Z. Children’s experiences of dental anxiety. Int. J. Paediatr. Dent. 2017, 27, 87–97. [Google Scholar] [CrossRef]
- Shahnavaz, S.; Rutley, S.; Larsson, K.; Dahllöf, G. Children and parents’ experiences of cognitive behavioral therapy for dental anxiety—A qualitative study. Int. J. Paediatr Dent. 2015, 25, 317–326. [Google Scholar] [CrossRef]
- Ainscough, S.L.; Windsor, L.; Tahmassebi, J.F. A review of the effect of music on dental anxiety in children. Eur. Arch. Paediatr. Dent. 2019, 20, 23–26. [Google Scholar] [CrossRef]
- Marker, C.D.; Comer, J.S.; Abramova, V.; Kendall, P.C. The reciprocal relationship between alliance and symptom improvement across treatment of childhood anxiety. J. Clin. Child Adolesc. Psychol. 2013, 42, 22–33. [Google Scholar] [CrossRef]
- Tomlinson, R.M.; Cousins, L.A.; McMurtry, C.M.; Cohen, L.L. The power of pain self-efficacy: Applying a positive psychology framework to pediatric pain. Pediatr. Pain Lett. 2017, 19, 9–13. [Google Scholar]
- Lucas, P.J.; Patsios, D.; Walls, K.; Neville, P.; Harwood, P.; Williams, J.G.; Sandy, J. Neighbourhood incidence rate of paediatric dental extractions under general anaesthetic in South West England. Br. Dent. J. 2018, 9, 169–176. [Google Scholar] [CrossRef]
- Bux, S.; Porritt, J.; Marshman, Z. Evaluation of Self-Help Cognitive Behavioural Therapy for Children’s Dental Anxiety in General Dental Practice. Dent. J. 2019, 7, 36. [Google Scholar] [CrossRef]
| Patient Setting | Initial Worry Score | Post-Treat Worry Score | Initial Pain Score | Post-Treat Pain Score |
|---|---|---|---|---|
| Practice (n = 52) | ||||
| Mean (SD) | 3.71 (2.15) | 1.84 (1.55) | 3.99 (2.37) | 1.96 (1.97) |
| Range | 1–10 | 0–6 | 1–10 | 0–8 |
| Hospital (n = 53) | ||||
| Mean (SD) | 5.98 (1.95) | 4.00 (1.67) | 6.21 (1.87) | 1.75 (1.50) |
| Range | 2–10 | 0–3 | 2–10 | 0–3 |
| Total Group (105) | ||||
| Mean (SD) | 4.85 (2.34) | 2.06 (1.69) | 5.12 (2.40) | 1.95 (1.93) |
| Range | 1–10 | 0–8 | 1–10 | 0–6 |
| Pain | Catastrophising | Uncertainty | Procedures |
|---|---|---|---|
| For it to be painful | Something will go wrong | Not knowing what is happening | Metal stuff in mouth |
| For it to hurt | I am worried something bad will happen | I don’t really know what they are going to do | Water in mouth |
| Me screaming and getting hurt | The wrong tooth to be taken out | It might make me frustrated | Seat going back and having things in my mouth |
| I think the injection is going to hurt | Something might get stuck | It may take a long time | Drill |
| Pain and unable to eat | If the dentist makes a mistake | - | Just injections |
| - | - | - | Needles |
| Absence of Pain | Good Communication | Speed | Good Clinical Outcome |
|---|---|---|---|
| Not to hurt | The dentist to listen to me | It to go smoothly and quickly | For it to get sorted |
| So I could not feel the pain | Dentist to tell me what is going to happen | To be quick | For my teeth to be clean |
| Numbing gel | When I put my hand up they stop | To be as quick and painless as possible | Get tooth out so no more pain |
| I can’t feel much | To be treated kindly | All to go quick and fine | For them to take away the decay |
| - | - | Smooth and calm | Leave smiling |
| Clinician Competence | Good Communication | Use of Coping Strategies |
|---|---|---|
| The actual process, because it wasn’t painful | Showing me everything and what it did | Listening to music |
| It was faster than expected | Plan-knowing what will happen next | Hand signals |
| Nothing nasty went in my mouth | Not thinking about it and understanding what was going on | Mind games |
| Everything went well | The explanation so I knew what was happening | Music and stress ball |
| It was quick | Not too much information given | - |
| The injection | - | - |
| Topical numbing gel | - | - |
| Digital Technology | Social Activities | Food-Related Treats |
| Play PS4 | Friend coming to house | Popcorn |
| More screen time | Fun with cousins | Have ice cream |
| Playing on the computer | Play on trampoline | Chicken |
| Go on my phone | Football | Favourite food |
| To go on my iPod | - | Baking |
| Play station | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodd, H.; Timms, L.; Noble, F.; Bux, S.; Porritt, J.; Marshman, Z. ‘Message to Dentist’: Facilitating Communication with Dentally Anxious Children. Dent. J. 2019, 7, 69. https://doi.org/10.3390/dj7030069
Rodd H, Timms L, Noble F, Bux S, Porritt J, Marshman Z. ‘Message to Dentist’: Facilitating Communication with Dentally Anxious Children. Dentistry Journal. 2019; 7(3):69. https://doi.org/10.3390/dj7030069
Chicago/Turabian StyleRodd, Helen, Laura Timms, Fiona Noble, Sarah Bux, Jenny Porritt, and Zoe Marshman. 2019. "‘Message to Dentist’: Facilitating Communication with Dentally Anxious Children" Dentistry Journal 7, no. 3: 69. https://doi.org/10.3390/dj7030069
APA StyleRodd, H., Timms, L., Noble, F., Bux, S., Porritt, J., & Marshman, Z. (2019). ‘Message to Dentist’: Facilitating Communication with Dentally Anxious Children. Dentistry Journal, 7(3), 69. https://doi.org/10.3390/dj7030069







