Crown–Root Ratio as a Predictive Morphometric Indicator in Mandibular First Molars with Occlusal Trauma and Periodontitis: A Radiographic and Clinical Modeling Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population and Sampling
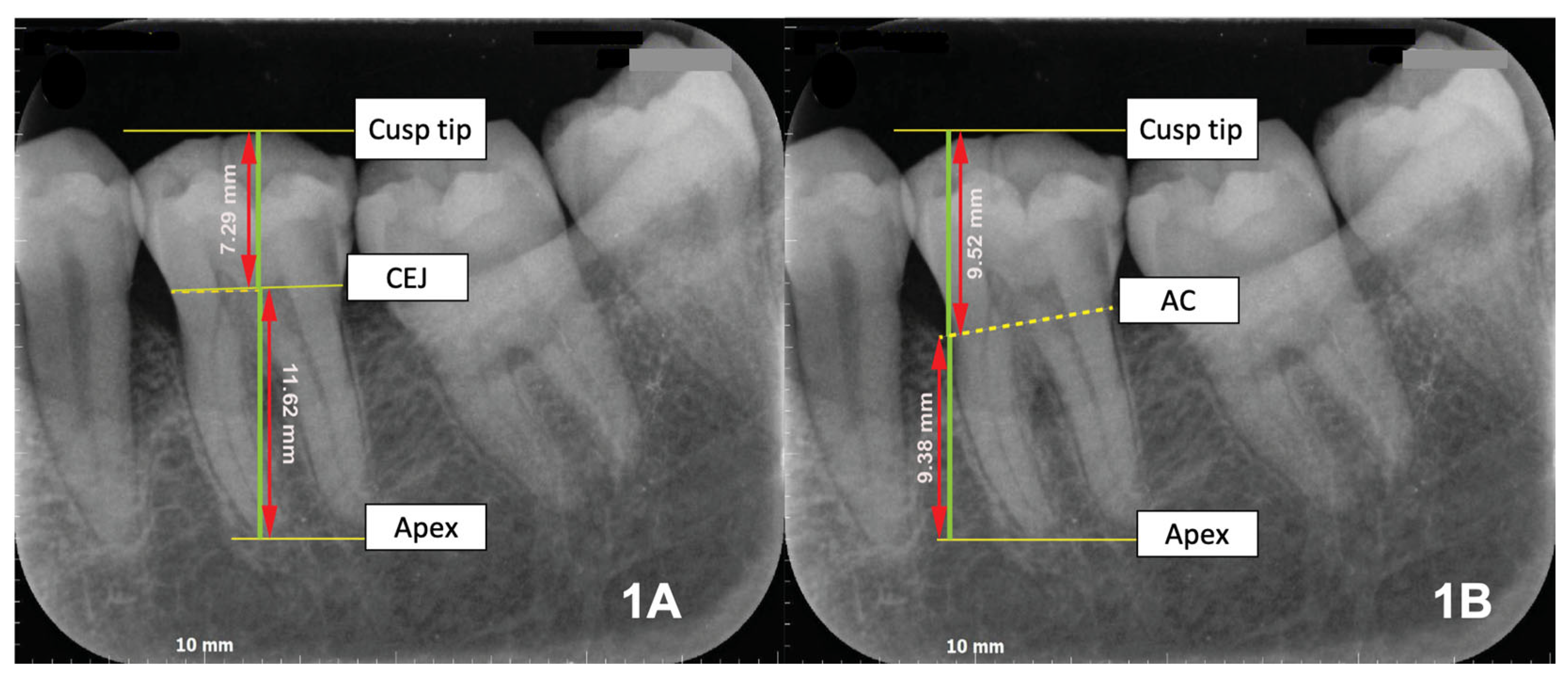
2.3. Operational Definitions and Measurements
2.4. Data Collection and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harrel, S.K.; Nunn, M.E. The effect of occlusal discrepancies on periodontitis. II. Relationship of occlusal treatment to the progression of periodontal disease. J. Periodontol. 2001, 72, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, R.A.; Killeen, A.C. Do mobility and occlusal trauma impact periodontal longevity? Dent. Clin. N. Am. 2015, 59, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Caton, J.G. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J. Clin. Periodontol. 2018, 45, S199–S206. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.H.; Liu, H.L.; Hong, A.; Chao, P. Inconsistency in the crown-to-root ratios of single-rooted premolars measured by 2D and 3D examinations. Sci. Rep. 2017, 7, 16484. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, Y.; Sadan, A. The prosthodontic concept of crown-to-root ratio: A review of the literature. J. Prosthet. Dent. 2005, 93, 559–562. [Google Scholar] [CrossRef] [PubMed]
- Penny, R.E.; Kraal, J.H. Crown-to-root ratio: Its significance in restorative dentistry. J. Prosthet. Dent. 1979, 42, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Liu, Y.; Yang, Y.; Ren, M.; Luo, L.; Zheng, L.; Liu, Y. Effect of short implant crown-to-implant ratio on stress distribution in anisotropic bone with different osseointegration rates. BMC Oral Health 2023, 23, 683. [Google Scholar] [CrossRef] [PubMed]
- Bruhnke, M.; Voß, I.; Sterzenbach, G.; Beuer, F.; Naumann, M. Evaluating the prospective crown-root ratio after extrusion and crown lengthening procedures in vitro. Sci. Rep. 2023, 13, 18899. [Google Scholar] [CrossRef] [PubMed]
- Mowry, J.K.; Ching, M.G.; Orjansen, M.D.; Cobb, C.M.; Friesen, L.R.; MacNeill, S.R.; Rapley, J.W. Root surface area of the mandibular cuspid and bicuspids. J. Periodontol. 2002, 73, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.W.; Meng, Y.; Jiao, J.; Shi, D.; Feng, X.H.; Meng, H.X. Association of crown-root ratio and tooth survival in Chinese patients with advanced periodontitis: An 11-year retrospective cohort study. J. Dent. 2024, 150, 105360. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89, S159–S172. [Google Scholar] [CrossRef] [PubMed]
- Lind, V. Short root anomaly. Scand. J. Dent. Res. 1972, 80, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.J.; Jeong, J.S.; Pang, N.S.; Kwon, I.K.; Jung, B.Y. Radiographic assessment of clinical root-crown ratios of permanent teeth in a healthy Korean population. J. Adv. Prosthodont. 2014, 6, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Han, S.; Wang, S.; Wei, X.; Zhang, H. Evaluation of anterior teeth crown-root morphology and alveolar bone structure in patients with closed deep overbite using cone beam computed tomography. Sci. Rep. 2024, 14, 24670. [Google Scholar] [CrossRef] [PubMed]
- Anggraini, W.; Masulili, S.L.C.; Lessang, R. The relationship between root-crown ratio of first molar’s teeth with trauma from occlusion. J. Int. Dent. Med. Res. 2017, 10, 265–269. [Google Scholar]
- Nissan, J.; Ghelfan, O.; Gross, O.; Priel, I.; Gross, M.; Chaushu, G. The effect of crown/implant ratio and crown height space on stress distribution in unsplinted implant supporting restorations. J. Oral Maxillofac. Surg. 2011, 69, 1934–1939. [Google Scholar] [CrossRef] [PubMed]
- Tajik, M.; Movahhedian, N. Canine sexual dimorphism in crown and root dimensions: A cone-beam computed tomographic study. J. Forensic. Odontostomatol. 2024, 42, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Escudero, T.M.; Toro, D.A.; Parada-Sanchez, M.T. How teeth can be used to estimate sexual dimorphism? A scoping review. Forensic. Sci. Int. 2024, 360, 112061. [Google Scholar] [CrossRef] [PubMed]
- Alsofi, L.; Al-Habib, M.; Zahran, S.; Alsulaiman, M.; Barayan, M.; Khawaji, S.; Sanari, M.; Altorkestani, M.; Alshehri, L.; Zarei, L.; et al. Three-dimensional evaluation of root canal morphology in mandibular premolars of Saudi individuals: A CBCT study. Libyan J. Med. 2025, 20, 2464292. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Wang, Q.; Li, J.; Zhou, M.; Tang, K.; Chen, J.; Wang, F. Construction of a novel digital method for quantitative analysis of occlusal contact and force. BMC Oral Health 2023, 23, 190. [Google Scholar] [CrossRef] [PubMed]

| Variables | Sex | p-Value | |
|---|---|---|---|
| Female | Male | ||
| Age (years) * | 46 (20–70) | 42 (30–77) | Not significant (independent samples median test) |
| Clinical Examination | |||
| Tooth mobility 0: No | 50 (50.5%) | 23 (23.2%) | Not significant (Pearson chi-square) |
| 1: Yes | 18 (18.2%) | 8 (8.1%) | |
| Presence of premature contact 0: No | 40 (40.4%) | 19 (19.2%) | Not significant (Pearson chi-square) |
| 1: Yes | 28 (28.3%) | 12 (12.1%) | |
| Probing pocket depth (PPD) 0: Suprabony pocket | 7 (7.1%) | 6 (6.1%) | Not significant (Pearson chi-square) |
| 1: Infrabony pocket | 61 (61.6%) | 25 (25.3%) | |
| Dental radiology examination | |||
| Periodontal space widening and lamina dura thinning (unilateral) 0: No | 3 (3%) | 0 (0%) | Not significant (Fisher’s exact test) |
| 1: Yes | 65 (65.7%) | 31 (31.3%) | |
| Pattern of alveolar bone loss 0: Horizontal loss on both mesial and distal surfaces | 7 (7.1%) | 6 (6.1%) | Not significant (Pearson chi-square) |
| 1: Vertical loss on either mesial or distal surface | 28 (28.3%) | 16 (16.2%) | |
| 2: Vertical loss on both mesial and distal surfaces | 33 (33.3%) | 9 (9.1%) | |
| Occlusal arch alignment 0: Parallel occlusal arch | 15 (15.2%) | 9 (9.1%) | Not significant (Pearson chi-square) |
| 1: Non-parallel occlusal arch | 53 (53.5%) | 22 (22.2%) | |
| Root morphology 0: normal root shape on both mesial and distal roots | 0 (0%) | 0 (0%) | Not significant (Fisher’s exact test) |
| 1: Blunt/curved root on either mesial or distal root | 13 (13.1%) | 7 (7.1%) | |
| 2: Blunt/curved root on both mesial and distal roots | 55 (55.6%) | 24 (24.2%) | |
| Crown length (mm) * | 7.2 (5.4–11.5) | 7.6 (6.3–9.2) | p = 0.025 (independent samples median test) |
| Root length (mm) * | 12.3 (9–20.4) | 13.3 (11.5–16.6) | p = 0.008 (independent samples median test) |
| Clinical crown-root ratio (CRR) ** | 0.59 (0.11) | 0.57 (0.08) | Not significant (independent samples t-test) |
| Crown width (mm) * | 12.3 (2.3–14.2) | 12.6 (10.4–14.6) | Not significant (independent samples median test) |
| Root width (mm) ** | 8.6 (1.4) | 8.8 (1.1) | Not significant (independent samples t-test) |
| Tooth axis inclination to the occlusal arch (°) * | 76.2 (55.8–86.8) | 75.7 (48–86.4) | Not significant (independent samples median test) |
| Interproximal bone loss (mm) * | 2.3 (0.5–9) | 2.9 (0.5–7.8) | Not significant (Independent samples median test) |
| Radiographic crown-root ratio * | 1 (0.8–1.9) | 1.2 (0.8–1.6) | p = 0.008 (Independent samples median test) |
| Variables | Crown Length | Root Length | ||
|---|---|---|---|---|
| Correlation Coefficient (r) | p-Value | Correlation Coefficient (r) | p-Value | |
| Age (years) | −0.171 | 0.09 | 0.035 | 0.729 |
| Sex 1: Female | 0.237 * | 0.018 | 0.312 ** | 0.002 |
| 2: Male | ||||
| Clinical examination | ||||
| Tooth mobility 0: No | 0.027 | 0.791 | −0.068 | 0.502 |
| 1: Yes | ||||
| Presence of premature contact 0: No | 0.053 | 0.605 | 0.003 | 0.980 |
| 1: Yes | ||||
| Probing pocket depth (PPD) 0: Suprabony pocket | 0.035 | 0.730 | −0.136 | 0.179 |
| 1: Infrabony pocket | ||||
| Dental radiology examination | ||||
| Periodontal space widening and lamina dura thinning (unilateral) 0: No | −0.134 | 0.186 | 0.056 | 0.584 |
| 1: Yes | ||||
| Pattern of alveolar bone loss 0: Horizontal loss on both mesial and distal surfaces | −0.099 | 0.331 | −0.228 * | 0.023 |
| 1: Vertical loss on either mesial or distal surface | ||||
| 2: Vertical loss on both mesial and distal surfaces | ||||
| Occlusal arch alignment 0: Parallel occlusal arch | 0.036 | 0.721 | −0.134 | 0.187 |
| 1: Non-parallel occlusal arch | ||||
| Root morphology 0: normal root shape on both mesial and distal roots | −0.019 | 0.852 | −0.129 | 0.203 |
| 1: Blunt/curved root on either mesial or distal root | ||||
| 2: Blunt/curved root on both mesial and distal roots | ||||
| Crown length (mm) | 0.142 | 0.16 | ||
| Root length (mm) | 0.142 | 0.16 | ||
| Clinical crown-root ratio (CRR) | 0.526 ** | 0.000 | −0.735 ** | 0.000 |
| Crown width (mm) | 0.291 ** | 0.003 | 0.027 | 0.791 |
| Root width (mm) | 0.063 | 0.538 | 0.308 ** | 0.002 |
| Tooth axis inclination (°) | 0.148 | 0.144 | 0.126 | 0.213 |
| Interproximal bone loss (mm) | −0.134 | 0.186 | −0.053 | 0.605 |
| Radiographic crown-root ratio | 0.236 * | 0.019 | 0.366 ** | 0.000 |
| Model | Coefficients (B) | Standard Error (SE) | Standardized Coefficients (β) | p-Value | Collinearity VIF | |
|---|---|---|---|---|---|---|
| 1 | (Constant) | 4.201 | 0.412 | 0.000 | ||
| Clinical crown–root ratio (CRR) | 5.547 | 0.690 | 0.632 | 0.000 | 1.000 | |
| R2 | 0.400 | |||||
| 2 | (Constant) | −6.199 | 0.358 | 0.000 | ||
| Clinical crown–root ratio (CRR) | 11.959 | 0.295 | 1.363 | 0.000 | 1.978 | |
| Root length (mm) | 0.513 | 0.017 | 1.039 | 0.000 | 1.978 | |
| R2 | 0.945 | |||||
| 3 | (Constant) | −6.179 | 0.346 | 0.000 | ||
| Clinical crown–root ratio (CRR) | 11.868 | 0.286 | 1.352 | 0.000 | 2.003 | |
| Root length (mm) | 0.502 | 0.016 | 1.017 | 0.000 | 2.093 | |
| Sex (1 = Female; 2 = Male) | 0.134 | 0.047 | 0.068 | 0.005 | 1.065 | |
| R2 | 0.950 | |||||
| 4 | (Constant) | −5.950 | 0.348 | 0.000 | ||
| Clinical crown–root ratio (CRR) | 11.899 | 0.278 | 1.356 | 0.000 | 2.007 | |
| Root length (mm) | 0.501 | 0.016 | 1.015 | 0.000 | 2.094 | |
| Sex (1 = Female, 2 = Male) | 0.131 | 0.046 | 0.066 | 0.005 | 1.066 | |
| Root morphology 1 | −0.130 | 0.051 | −0.057 | 0.013 | 1.009 | |
| R2 | 0.953 | |||||
| 5 | (Constant) | −5.726 | 0.358 | 0.000 | ||
| Clinical crown–root ratio (CRR) | 11.850 | 0.274 | 1.350 | 0.000 | 2.021 | |
| Root length (mm) | 0.500 | 0.016 | 1.013 | 0.000 | 2.096 | |
| Sex (1 = Female, 2 = Male) | 0.132 | 0.045 | 0.067 | 0.004 | 1.066 | |
| Root morphology 1 | −0.132 | 0.050 | −0.058 | 0.010 | 1.009 | |
| Age (years) | −0.004 | 0.002 | −0.046 | 0.038 | 1.010 | |
| R2 | 0.955 | |||||
| Model | Coefficients (B) | Standard Error (SE) | Standardized Coefficients (β) | p-Value | Collinearity VIF | |
|---|---|---|---|---|---|---|
| 1 | (Constant) | 20.272 | 0.766 | 0.000 | ||
| Clinical crown–root ratio (CRR) | −12.499 | 1.283 | 0.703 | 0.000 | 1.000 | |
| R2 | 0.494 | |||||
| 2 | (Constant) | 12.829 | 0.334 | 0.000 | ||
| Clinical crown–root ratio (CRR) | −22.327 | 0.502 | −1.256 | 0.000 | 1.665 | |
| Crown length (mm) | 1.772 | 0.057 | 0.875 | 0.000 | 1.665 | |
| R2 | 0.954 | |||||
| 3 | (Constant) | 12.401 | 0.375 | 0.000 | ||
| Clinical crown–root ratio (CRR) | −22.474 | 0.495 | −1.264 | 0.000 | 1.693 | |
| Crown length (mm) | 1.785 | 0.056 | 0.881 | 0.000 | 1.682 | |
| Root morphology 1 | 0.231 | 0.100 | 0.050 | 0.022 | 1.017 | |
| R2 | 0.956 | |||||
| 4 | (Constant) | 12.525 | 0.374 | 0.000 | ||
| Clinical crown–root ratio (CRR) | −22.736 | 0.504 | −1.279 | 0.000 | 1.812 | |
| Crown length (mm) | 1.821 | 0.058 | 0.899 | 0.000 | 1.854 | |
| Root morphology 1 | 0.231 | 0.098 | 0.050 | 0.021 | 1.017 | |
| Sex (1 = Female; 2 = Male) | −0.180 | 0.089 | −0.045 | 0.045 | 1.110 | |
| R2 | 0.958 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nainggolan, L.I.; Kiswanjaya, B.; Priaminiarti, M.; Masulili, S.L.C.; Bachtiar-Iskandar, H.H.; Soeroso, Y.; Wulandari, P.; Astuti, E.R.; Yoshihara, A. Crown–Root Ratio as a Predictive Morphometric Indicator in Mandibular First Molars with Occlusal Trauma and Periodontitis: A Radiographic and Clinical Modeling Study. Dent. J. 2025, 13, 419. https://doi.org/10.3390/dj13090419
Nainggolan LI, Kiswanjaya B, Priaminiarti M, Masulili SLC, Bachtiar-Iskandar HH, Soeroso Y, Wulandari P, Astuti ER, Yoshihara A. Crown–Root Ratio as a Predictive Morphometric Indicator in Mandibular First Molars with Occlusal Trauma and Periodontitis: A Radiographic and Clinical Modeling Study. Dentistry Journal. 2025; 13(9):419. https://doi.org/10.3390/dj13090419
Chicago/Turabian StyleNainggolan, Lidya Irani, Bramma Kiswanjaya, Menik Priaminiarti, Sri Lelyati Chaidar Masulili, Hanna H. Bachtiar-Iskandar, Yuniarti Soeroso, Pitu Wulandari, Eha Renwi Astuti, and Akihiro Yoshihara. 2025. "Crown–Root Ratio as a Predictive Morphometric Indicator in Mandibular First Molars with Occlusal Trauma and Periodontitis: A Radiographic and Clinical Modeling Study" Dentistry Journal 13, no. 9: 419. https://doi.org/10.3390/dj13090419
APA StyleNainggolan, L. I., Kiswanjaya, B., Priaminiarti, M., Masulili, S. L. C., Bachtiar-Iskandar, H. H., Soeroso, Y., Wulandari, P., Astuti, E. R., & Yoshihara, A. (2025). Crown–Root Ratio as a Predictive Morphometric Indicator in Mandibular First Molars with Occlusal Trauma and Periodontitis: A Radiographic and Clinical Modeling Study. Dentistry Journal, 13(9), 419. https://doi.org/10.3390/dj13090419







