Abstract
Background: Preclinical dental training requires simulation-based tools to develop fine motor skills, but traditional models like plastic teeth often lack realistic tactile feedback, and systematic evaluations of multi-layered drilling plates are scarce. This study aimed to evaluate the educational utility and perceived realism of a novel multi-layered drilling plate designed to simulate enamel, dentin, and pulp, with null hypotheses that it would not differ in realism from natural dental tissues or in educational utility from existing tools. Methods: Seventy dental educators (mean preclinical teaching experience: 112.9 ± 116.7 months) from 14 institutions across four continents assessed the plates using standardized protocols. Statistical analysis (Mann–Whitney U Test) was performed to analyze the results. Results: Quantitative ratings (1–10 scale) showed high mean scores for drilling quality (enamel: 7.80 ± 1.55, dentin: 7.27 ± 1.94, pulp: 7.48 ± 2.33), surface smoothness (enamel: 8.17 ± 1.55, dentin: 8.17 ± 1.57), and ergonomic visibility (8.56 ± 1.58), with 90% passing grades, rejecting the null hypothesis of no difference in educational utility. Tissue transition scores (enamel/dentin: 7.09 ± 2.56; dentin/pulp: 6.86 ± 2.46) showed significant differences (p < 0.05) in realism from natural tissues, rejecting the null hypothesis of no difference. Inter-rater reliability was poor (Krippendorff’s alpha: 0.449 for failing scores, 0.211 for passing scores). Qualitative feedback praised ease of use but noted limitations in dentin haptic simulation. Conclusions: The drilling plate shows promise for skill development, though without controlled comparisons to existing tools, its relative efficacy remains preliminary. Further research on student outcomes and tool refinement is needed to validate its use in dental education.
1. Introduction
The development of fine motor skills is a cornerstone of dental education, enabling students to perform precise clinical procedures that require discerning the positions, sizes, shapes, and tactile properties of dental tissues [1,2]. Traditional preclinical training relies on phantom head simulators and plastic teeth, which often fail to replicate the tactile feedback of natural dental tissues, particularly the distinct hardness of enamel, dentin, and pulp [3,4]. Advances in dental technology have introduced virtual reality simulators with haptic interfaces (VR-haptics), which enhance skill acquisition but cannot fully replace physical simulation [5,6]. These limitations can impede students’ ability to develop the tactile sensitivity needed for procedures like caries removal, which demand differentiation between healthy and carious tissues [7,8,9].
To address these challenges, multi-layered drilling plates have been developed to mimic the mechanical properties of dental hard tissues, incorporating distinct layers for enamel, dentin, and pulp, though replicating soft tissues remains a challenge [10,11]. Early in dental education, students practice preparing geometric shapes in drilling plates inserted into phantom heads, allowing handpiece-naïve learners to hone skills in a controlled environment [12,13]. Early during practical education, the students also practice the preparation of geometric shapes in drilling plates on a bench and not only inserted into phantom heads [13]. These drilling plates, designed with varying hardness levels to simulate clinical conditions, provide a foundational step for preclinical training, bridging the gap between theoretical knowledge and clinical application, yet systematic evaluations of their efficacy and realism are limited [14,15].
The evolving landscape of dental education emphasizes the integration of traditional hands-on methods with innovative technologies, including virtual reality (VR), haptic simulators, and AI-powered platforms [16]. For example, AI-designed dental crowns and the resulting virtual patient models may enhance dental training by providing realistic, patient-specific scenarios that can improve both clinical precision and decision-making skills [17]. This blended approach not only enhances technical proficiency, but also supports student well-being by incorporating stress-reduction strategies, such as background music and mindfulness techniques, which have been shown to accelerate skill acquisition and reduce anxiety [18]. While digital tools offer individualized feedback and low-risk practice environments, traditional mentorship remains essential for fostering clinical judgment and professional values [19,20]. This synergy creates a comprehensive educational framework that prepares students for clinical practice.
To date, there is a lack of nationally or internationally available data specifically evaluating the use of drilling plates in preclinical training. While various preclinical training tools are used nationally and internationally, systematic studies comparing their efficacy, cost, durability, or simulation realism are scarce. This gap highlights the need for further research to establish standardized metrics and comparative analyses, as addressed in the present study. This study evaluated the educational utility and perceived realism of a novel multi-layered drilling plate designed to simulate the tactile and structural properties of human dental hard tissues. Unlike conventional plastic teeth, which lacked adequate differentiation between enamel, dentin, and pulp, this drilling plate incorporated three distinct layers to enhance preclinical training. The null hypotheses of this study were that the novel multi-layered drilling plate would not differ in perceived realism from natural dental tissues and that it would not differ in educational utility from existing preclinical training tools, as assessed by dental educators. Through a multi-institutional investigation involving dental educators from diverse pedagogical and cultural backgrounds, this study assessed the generalizability, realism, and efficacy of the drilling plate as a training tool, aiming to advance the integration of innovative and traditional methods in dental education.
2. Methods
2.1. Study Design and Ethical Considerations
This multi-institutional study was designed based on established guidelines for educational research, ensuring methodological rigor, reproducibility, and ethical compliance. All procedures adhered to the principles outlined in the Declaration of Helsinki [21]. Informed consent was obtained from all participants, and the study protocol was approved by the Institutional Review Board of the University of Eastern Finland (Reference Number: 40/2023).
2.2. Participant Recruitment
All 30 dental institutions of the Digital, VR, and Haptic Thinkers Global Network were invited to participate in this study. The inclusion criteria for individual participants were as follows [22]:
- Those who hold a primary dental degree;
- Those who are involved in preclinical teaching.
The exclusion criteria were as follows:
- Those who have not received a recognized primary dental qualification;
- Those who have no experience in preclinical teaching.
From those expressing interest, 15 dental institutions were randomly selected using a randomization table [23], from four different continents and representing a broad range of pedagogical perspectives.
2.3. Standardization and Pre-Study Calibration
To ensure uniform execution, a preparatory video meeting was conducted via Microsoft Teams, where procedural steps were thoroughly reviewed and calibrated. A detailed written guideline, including standard operating procedures and the assessor form (Figure A1), was distributed to all participants. The guideline specified that five independent testers (T1–T5) at each institution would evaluate five distinct drilling samples (S1–S5), each marked with a different color for identification (Figure A2). All participants were instructed to complete each sampling procedure within 2 minutes. This calibration process minimized inter-operator variability and ensured adherence to EU standards for testing dental materials.
2.4. Materials and Equipment
The test material consisted of multi-layered drilling plates manufactured by Nissin Dental Products, Inc. (Kyoto, Japan), designed for compatibility with dental phantom heads to simulate clinical scenarios (Figure 1) [3]. Each plate featured three distinct layers mimicking enamel (in white), dentin (in yellow), and pulp (in red), with varying hardness levels to replicate natural dental tissues. Drilling was performed using a dental handpiece (model identical across sites) and uniform burs (fissure), with rotational speeds (RPM) controlled as follows: enamel (150,000–200,000 RPM), dentin (100,000–150,000 RPM), and pulp (80,000–100,000 RPM). Procedures were conducted in an ergonomic body posture, without the use of magnifying loupes, to reflect typical preclinical training conditions and ensure consistent visual assessment [24].
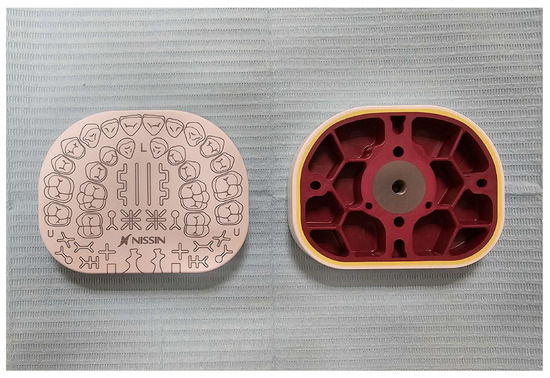
Figure 1.
Front and rear views of the drilling plates assessed in the study. Dimensions: 16 mm (H) × 80 mm (W) × 62 mm (L). Thickness of layers: white (enamel) = 1.5 mm, yellow (dentin) = 1.0 mm, and red (pulp) = 2.0 mm.
2.5. Experimental Procedure
At each institution, five participants (T1–T5) independently performed predefined drilling exercises on five samples (S1–S5) [25]: (1) enamel only, (2) enamel and dentin, (3) enamel only (tooth-shaped areas), (4) enamel and dentin (tooth-shaped areas), and (5) all layers (enamel, dentin, and pulp). All participants were instructed to follow the standardized RPM when performing the tasks. Each sample was drilled once per tester, and the test date was recorded for each sample. Exercises were designed to assess the material’s performance across clinically relevant scenarios, with color-coded samples ensuring accurate identification and traceability, made in a randomized order for the different participants.
2.6. Evaluation and Data Collection
Each participant independently assessed their subjective drilling experience using a standardized assessment form (Figure A3) provided in the assessor guidelines. The form included quantitative ratings (1–10 scale, where 1 = poor and 10 = excellent) for the following parameters [26,27,28,29]:
- Drilling quality of enamel;
- Drilling quality of dentin;
- Drilling quality of pulp;
- Hardness differences between enamel and dentin;
- Hardness differences between dentin and pulp;
- Smoothness of prepared dentin surface;
- Visibility of drilling patterns from an ergonomic viewpoint (without magnification).
Qualitative feedback was collected via a free-text section for additional observations or recommendations [30,31]. Each plate received a binary pass/fail grade based on overall performance, with testers providing a rationale for their assessment [32]. The form also recorded testers’ months of preclinical experience and the RPM settings used.
2.7. Data Management and Statistical Analysis
Data were collected anonymously to ensure integrity and minimize bias. Quantitative ratings were analyzed using IBM SPSS Statistics (version 29.0.0 or higher, IBM Deutschland GmbH, Böblingen, Germany). Mean scores and standard deviations were calculated for each parameter, and inter-rater reliability was assessed using Krippendorff’s alpha [33]. Linear regression was used to test for potential associations between ratings and educator experience, and the Mann–Whitney U test was used to find potential similarities between the pass and fail groups. Qualitative feedback was thematically analyzed to identify common observations and recommendations. All data were stored securely in compliance with the GDPR [34].
3. Results
3.1. Quantitative Evaluation
Of the 15 dental institutions invited, 14 participated, yielding 70 evaluators with a mean preclinical teaching experience of 112.9 months (approximately 9.4 years; SD = 116.7 months). Table 1 summarizes the quantitative evaluation of the multi-layered drilling plates across all assessed parameters. Mean scores (± standard deviation) for drilling quality were as follows: enamel, 7.80 ± 1.55 (95% CI [7.46, 8.20]); dentin, 7.27 ± 1.94 (95% CI [6.81, 7.73]); and pulp, 7.48 ± 2.33 (95% CI [6.92, 8.04]). The perceived hardness difference between enamel and dentin scored 7.09 ± 2.56 (95% CI [6.47, 7.70]), while the transition between dentin and pulp scored slightly lower at 6.86 ± 2.46 (95% CI [6.26, 7.45]). Surface smoothness post drilling received high mean scores for both enamel (8.17 ± 1.55, 95% CI [7.80, 8.54]) and dentin (8.17 ± 1.57, 95% CI [7.80, 8.55]). The visibility of drilling patterns from an ergonomic perspective (without magnifying loupes) was rated highly at 8.56 ± 1.58 (95% CI [8.17, 8.92]).

Table 1.
Dental plate quantitative assessment results. Mean scores with standard deviations (SDs) and 95% confidence intervals (CIs) are shown.
Inter-rater reliability was poor, with Krippendorff’s alpha values of 0.449 for evaluators assigning failing scores and 0.211 for those assigning passing scores, indicating variability in assessments likely due to diverse evaluator backgrounds. Figure 2 illustrates the distribution of ratings for pass and fail groups, showing greater variability in passing scores, particularly for dentin and pulp drilling quality.
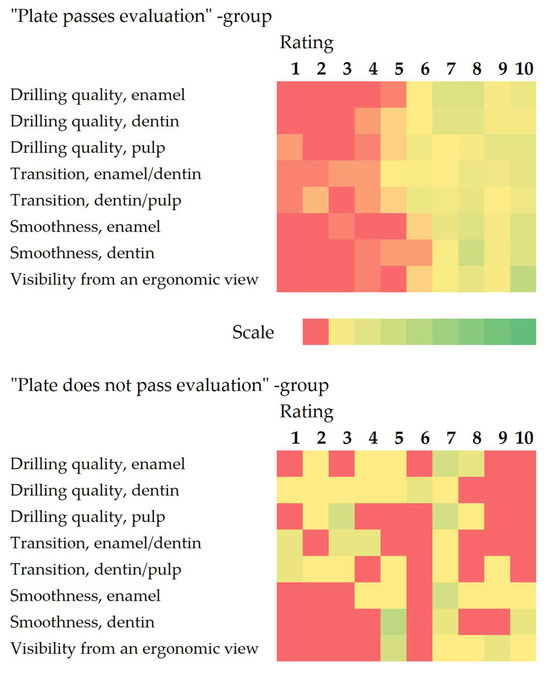
Figure 2.
Distribution of ratings. Results shown as heatmaps with the color scales set between zero and the maximum number of replies for the group (“pass” group n = 62; “fail” group n = 8).
Linear regression analysis revealed a significant relationship between teaching experience and assessment ratings (F(8, 57) = 2.412, p = 0.026, R2 = 0.253, and adjusted R2 = 0.148). Specifically, the drilling quality of enamel (p = 0.002) and the visibility of drilling patterns (p = 0.019) were significantly influenced by evaluators’ experience, suggesting that more experienced educators rated these parameters more favorably.
3.2. Qualitative Feedback
Of the 70 participants, 63 (90%) assigned a passing grade to the drilling plates. Statistical analysis showed significant differences in rating distributions between pass and fail groups for all parameters except enamel smoothness (p = 0.080). Qualitative feedback highlighted the plates’ strengths, including ease of integration into standard phantom heads, clear visualization of simulated anatomical structures, and straightforward setup. However, 22 participants (31%) noted that the haptic feedback for dentin hardness did not fully replicate natural dental tissue, suggesting an area for refinement to enhance simulation realism. Several evaluators recommended incorporating AI-generated virtual patient models to contextualize drilling exercises, emphasizing the plates’ potential to support preclinical training when paired with advanced digital tools.
4. Discussion
The integration of innovative tools, such as multi-layered drilling plates, into dental education might enhance the development of clinical skills in a safe environment [1], particularly for students new to handpiece use. However, challenges such as high initial costs and resistance to change among educators might impede widespread adoption [35,36]. The results from this multi-institutional study, which was one of the first, according to the authors’ best knowledge, involving dental educators with diverse backgrounds, demonstrated the plates’ potential. Ongoing refinement and international collaboration might help to further standardize training tools in dental education. Although VR-haptic simulators are becoming increasingly popular in dental education, physical models remain irreplaceable for preclinical training, as they provide a more direct and tangible experience of resistance and vibration feedback, which are essential to tactile learning and confidence-building in the early training phases [12,37].
The drilling plates received high ratings for surface smoothness and ergonomic visibility, reflecting their suitability for early psychomotor skill development [9]. However, lower scores for tissue transitions indicated challenges in replicating tactile differentiation, a critical skill for restorative dentistry [10,38]. This aligns with findings on 3D-printed models, where intermediate tissues, such as dentin, remained difficult to simulate haptically [7,9,10,11]. The plates’ layered structure and color coding supported tissue identification, but further improvements in haptic realism might be needed.
The high pass rate and positive feedback on ease of use underscored the plates’ value as a training and assessment tool, aligning with competency-based education principles. The wide SDs suggested that participant perceptions varied, potentially influenced by cultural or experiential differences in preclinical training [39]. The relatively high SDs observed in scores, particularly for pulp drilling quality and tissue transitions, likely reflect inter-rater variability. This variability may stem from participants’ diverse teaching experiences and differing institutional practices, which could influence expectations and perceptions of the drilling plates’ haptic and tactile qualities [40]. Such discrepancies highlight the challenge of achieving consistent evaluations across varied expertise levels and suggest a need for standardized rater training or calibration in future studies to enhance inter-rater reliability [41,42]. Nonetheless, the drilling plates might provide additional teaching opportunities, as they could offer a means for structured, objective assessments that are predefined, validated, and reproducible—a growing requirement for dental educators to meet the modern principles of competency-based education [11,43].
However, this study had limitations. The results relied on expert evaluations without student outcome data, limiting insights into long-term learning effects. Given the diverse backgrounds of participants, there might be additional factors that impacted the results, such as variations in familiarity with specific techniques (e.g., orthodontists potentially being less familiar with conservative/endodontic procedures) [44,45], lighting, drill models, handpiece conditions, and ambient noise [46], alongside the likely scenario that each institution might deploy phantom head systems and mounting fixtures from different brands, introducing extra variables. Additionally, the relatively low inter-rater reliability, possibly caused by the wide age range of the participants and differences in their training and professional experience, indicated some level of disagreement among the participants regarding the quality of the drilling plates. This disagreement might have impacted the internal validity of the study by introducing measurement error, despite pre-study calibration efforts, including a video meeting and standardized guidelines. However, as a pilot study, the multi-institutional design and standardized protocols provided preliminary insights into the performance of the novel multi-layered drilling plates.
Still, the drilling plates offered a promising tool for preclinical training, with strengths in usability and assessment potential. Future research should compare the plates with existing models nationally and internationally, especially in terms of cost, durability, and simulation realism [47,48]. Efforts should also be made to include student performance metrics under a more standardized setting to address these gaps. Efforts might also be made to address haptic limitations, standardize equipment compatibility, and explore AI integration [49], which could further enhance their educational impact [50,51], supported by continued multi-institutional collaboration. To address the identified limitations, subsequent studies should incorporate stronger standardization settings, inter-rater reliability training, and statistical adjustments to account for evaluator variability. Future evaluations should include qualitative student feedback on satisfaction and quantitative metrics, such as practice scores and stress levels, to validate the educational impact [52,53]. It would also be important to assess whether there is any variation between different dental specialties. As the global dental community switches its focus from treatment to holistic oral health promotion [54,55], efforts would also be needed from dental educators to integrate approaches with new digital tools such as AI and mHealth into dental curricula [56,57], so that future dentists are equipped with preventive, interdisciplinary, and evidence-based approaches to promote community oral healthcare [58,59].
5. Conclusions
The multi-layered drilling plate demonstrated potential as a tool for preclinical dental training, with high educator ratings for drilling quality, smoothness, and visibility, supporting its use for skill development and assessment. However, without direct comparisons to existing training tools, its relative efficacy and realism remain preliminary. Limitations, including reliance on expert evaluations without student outcome data and poor inter-rater reliability due to diverse evaluator backgrounds, suggest the need for cautious interpretation of its effectiveness. Refinements to improve tactile differentiation, particularly for dentin, are needed. Future multi-institutional research should include controlled comparisons with standard tools and student performance metrics to validate the plate’s educational utility and inform its potential integration into dental curricula.
Author Contributions
Conceptualization, S.F., U.T.Ö. and P.L.; methodology, S.F., U.T.Ö. and P.L.; validation, S.F., M.L., U.T.Ö. and P.L.; formal analysis, M.L.; investigation, R.C.W.C., S.F., M.F.S.-P., S.A.-H., S.B., M.M. (Margrit Maggio), M.M. (Murat Mutluay), D.P.R., W.Y.H.L., S.N.U., B.F.Q., J.T., M.N., M.P., M.I., A.M.C.T., A.R., A.T.-M., S.K., K.L., M.L., O.S.H., U.T.Ö. and P.L.; resources, S.F.; data curation, S.F. and M.L.; writing—original draft preparation, R.C.W.C.; writing—review and editing, R.C.W.C., S.F., M.F.S.-P., S.A.-H., S.B., M.M. (Margrit Maggio), M.M. (Murat Mutluay), D.P.R., W.Y.H.L., S.N.U., B.F.Q., J.T., M.N., M.P., M.I., A.M.C.T., A.R., A.T.-M., S.K., K.L., M.L., O.S.H., U.T.Ö. and P.L.; visualization, R.C.W.C., S.F. and M.L.; supervision, S.F., U.T.Ö. and P.L.; project administration, S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the University of Eastern Finland (protocol code 40/2023, approved on 13 October 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be made available upon reasonable request to the corresponding author.
Acknowledgments
The authors would like to thank all participating dental institutions and educators for their contributions and valuable feedback during the testing phase.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AI | Artificial intelligence |
| CI | Confidence interval |
| EU | European Union |
| RPM | Revolutions per minute |
| SD | Standard deviation |
| VR | Virtual reality |
Appendix A
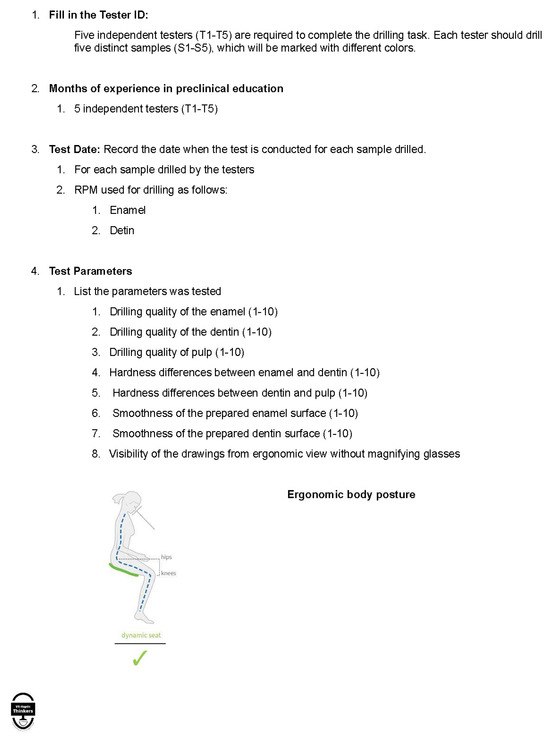
Figure A1.
The written guideline with standard operating procedures used in the study.
Appendix B
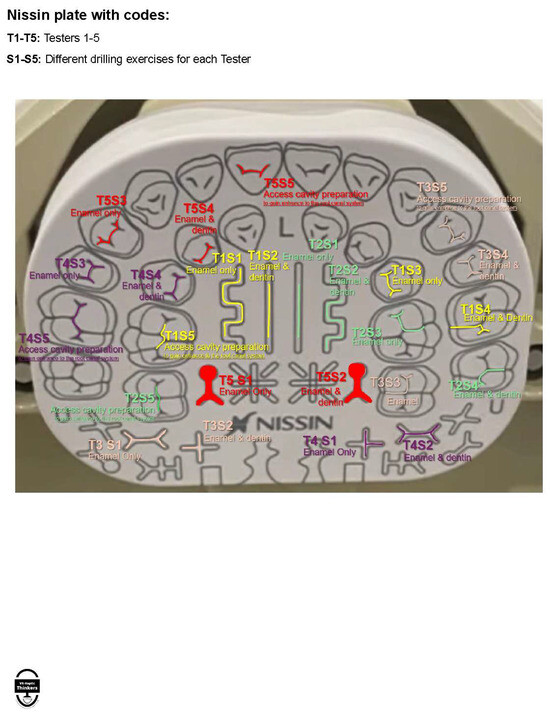
Figure A2.
The colored drilling guideline used in the study.
Appendix C
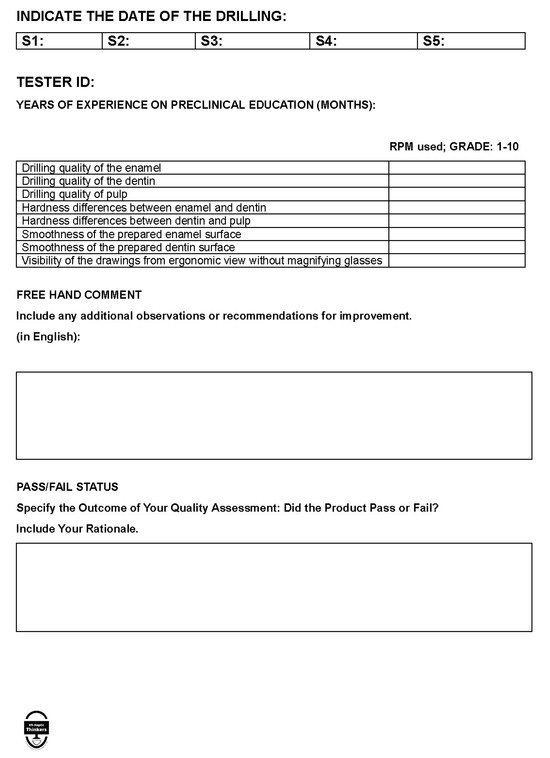
Figure A3.
The standardized assessor form used in the study.
References
- Ben-Gal, G.; Katorza, L.; Weiss, E.I.; Ziv, A. Testing motor learning curves among dental students. J. Dent. Educ. 2017, 81, 1171–1178. [Google Scholar] [CrossRef]
- Dimitrijevic, T.; Kahler, B.; Evans, G.; Collins, M.; Moule, A. Depth and distance perception of dentists and dental students. Oper. Dent. 2011, 36, 467–477. [Google Scholar] [CrossRef]
- Fugill, M. Defining the purpose of phantom head. Eur. J. Dent. Educ. 2013, 17, e1–e4. [Google Scholar] [CrossRef]
- Plessas, A. Computerized Virtual Reality Simulation in Preclinical Dentistry: Can a Computerized Simulator Replace the Conventional Phantom Heads and Human Instruction? Simul. Healthc. 2017, 12, 332–338. [Google Scholar] [CrossRef]
- Al-Saud, L.M.; Mushtaq, F.; Mann, R.P.; Mirghani, I.; Balkhoyor, A.; Harris, R.; Osnes, C.; Keeling, A.; A Mon-Williams, M.; Manogue, M. Early assessment with a virtual reality haptic simulator predicts performance in clinical practice. BMJ Simul. Technol. Enhanc. Learn. 2020, 6, 274. [Google Scholar] [CrossRef] [PubMed]
- Saghiri, M.A.; Vakhnovetsky, J.; Nadershahi, N. Scoping review of artificial intelligence and immersive digital tools in dental education. J. Dent. Educ. 2022, 86, 736–750. [Google Scholar] [CrossRef]
- Höhne, C.; Schwarzbauer, R.; Schmitter, M. 3D printed teeth with enamel and dentin layer for educating dental students in crown preparation. J. Dent. Educ. 2019, 83, 1457–1463. [Google Scholar] [CrossRef]
- Sonkaya, E.; Kürklü, Z.G.B. Comparisons of student comprehension of 3D-printed, standard model, and extracted teeth in hands-on sessions. Eur. J. Dent. Educ. 2024, 28, 452–460. [Google Scholar] [CrossRef]
- Höhne, C.; Schmitter, M. 3D printed teeth for the preclinical education of dental students. J. Dent. Educ. 2019, 83, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Dobroś, K.; Hajto-Bryk, J.; Zarzecka, J. Application of 3D-printed teeth models in teaching dentistry students: A scoping review. Eur. J. Dent. Educ. 2023, 27, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Kröger, E.; Dekiff, M.; Dirksen, D. 3D printed simulation models based on real patient situations for hands-on practice. Eur. J. Dent. Educ. 2017, 21, e119–e125. [Google Scholar] [CrossRef]
- Boushell, L.W.; Walter, R.; Phillips, C. Learn-A-Prep II as a predictor of psychomotor performance in a restorative dentistry course. J. Dent. Educ. 2011, 75, 1362–1369. [Google Scholar] [CrossRef]
- Perry, S.; Bridges, S.M.; Burrow, M.F. A review of the use of simulation in dental education. Simul. Healthc. 2015, 10, 31–37. [Google Scholar] [CrossRef]
- Field, J. Pre-Clinical Dental Skills at a Glance; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Zitzmann, N.U.; Matthisson, L.; Ohla, H.; Joda, T. Digital undergraduate education in dentistry: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 3269. [Google Scholar] [CrossRef]
- Lin, P.Y.; Chen, T.C.; Lin, C.J.; Huang, C.C.; Tsai, Y.H.; Wang, C.Y. The use of augmented reality (AR) and virtual reality (VR) in dental surgery education and practice: A narrative review. J. Dent. Sci. 2024, 19, S91–S101. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Rahimi, H.M.; Tichy, A. Artificial intelligence in prosthodontics. Dent. Clin. 2025, 69, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Brelet, L.; Gaffary, Y. Stress reduction interventions: A scoping review to explore progress toward use of haptic feedback in virtual reality. Front. Virtual Real. 2022, 3, 900970. [Google Scholar] [CrossRef]
- Bandiaky, O.N.; Lopez, S.; Hamon, L.; Clouet, R.; Soueidan, A.; Le Guehennec, L. Impact of haptic simulators in preclinical dental education: A systematic review. J. Dent. Educ. 2024, 88, 366–379. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.S.S.; Tan, W.W.; Tan, H.J.; Khoo, C.W.; Afrashtehfar, K.I. Innovative pedagogical strategies in health professions education: Active learning in dental materials science. Int. J. Environ. Res. Public Health 2023, 20, 2041. [Google Scholar] [CrossRef]
- Williams, J.R. The Declaration of Helsinki and public health. Bull. World Health Organ. 2008, 86, 650–652. [Google Scholar] [CrossRef]
- Frese, C.; Wolff, D.; Saure, D.; Staehle, H.; Schulte, A. Psychosocial impact, perceived stress and learning effect in undergraduate dental students during transition from pre-clinical to clinical education. Eur. J. Dent. Educ. 2018, 22, e555–e563. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.; Lennon, M.A.; Brook, A.H.; Robinson, P.G. A randomized controlled trial of outreach placement’s effect on dental students’ clinical confidence. J. Dent. Educ. 2006, 70, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Tedone, M.; Adorno, C.G.; Ortiz-Hugues, J.C.; Jesús Conde Villar, A.; Pérez Alfayate, R.; Loroño, G.; Estévez, R.; Díaz-Flores, V.; Meza, M.S. Musculoskeletal risk of first-year postgraduate endodontic students using dental microscope, ergonomic loupes or no magnification. Int. Endod. J. 2025, 6, 274–278. [Google Scholar] [CrossRef]
- Banerjee, A.; Watson, T.; Kidd, E. Dentine caries excavation: A review of current clinical techniques. Br. Dent. J. 2000, 188, 476–482. [Google Scholar] [CrossRef]
- Wang, D.; Zhao, S.; Li, T.; Zhang, Y.; Wang, X. Preliminary evaluation of a virtual reality dental simulation system on drilling operation. Bio Med. Mater. Eng. 2015, 26 (Suppl. S1), S747–S756. [Google Scholar] [CrossRef]
- Zamani, N.; Culbertson, H. Effects of physical hardness on the perception of rendered stiffness in an encountered-type haptic display. IEEE Trans. Haptics 2022, 16, 46–56. [Google Scholar] [CrossRef]
- Agra, C.M.; Vieira, G.F. Quantitative analysis of dental porcelain surfaces following different treatments: Correlation between parameters obtained by a surface profiling instrument. Dent. Mater. J. 2002, 21, 44–52. [Google Scholar] [CrossRef][Green Version]
- Kihara, T.; Keller, A.; Ogawa, T.; Armand, M.; Martin-Gomez, A. Evaluating the feasibility of using augmented reality for tooth preparation. J. Dent. 2024, 148, 105217. [Google Scholar] [CrossRef]
- Ricci-Cabello, I.; Saletti-Cuesta, L.; Slight, S.P.; Valderas, J.M. Identifying patient-centred recommendations for improving patient safety in general practices in England: A qualitative content analysis of free-text responses using the patient reported experiences and outcomes of safety in primary care (PREOS-PC) questionnaire. Health Expect. 2017, 20, 961–972. [Google Scholar]
- Maramba, I.D.; Davey, A.; Elliott, M.N.; Roberts, M.; Roland, M.; Brown, F.; Burt, J.; Boiko, O.; Campbell, J. Web-based textual analysis of free-text patient experience comments from a survey in primary care. JMIR Public Health Surveill. 2015, 3, e3783. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, T. Designing an Assessment Program for the Competency-Based Era; University of Toronto: Toronto, ON, Canada, 2016. [Google Scholar]
- Hayes, A.F.; Krippendorff, K. Answering the call for a standard reliability measure for coding data. Commun. Methods Meas. 2007, 1, 77–89. [Google Scholar] [CrossRef]
- Voigt, P.; Von dem Bussche, A. The Eu General Data Protection Regulation (gdpr): A Practical Guide, 1st ed.; Springer International Publishing: Cham, Switzerland, 2017; pp. 10–5555. [Google Scholar]
- Felszeghy, S.; Mutluay, M.; Liukkonen, M.; Flacco, N.; Bakr, M.M.; Rampf, S.; Schick, S.; Mushtaq, F.; Sittoni-Pino, M.F.; Ackerman, K.; et al. Benefits and challenges of the integration of haptics-enhanced virtual reality training within dental curricula. J. Dent. Educ. 2024, 89, 1070–1083. [Google Scholar] [CrossRef]
- Bencharit, S.; Quinn, B.; Sittoni-Pino, M.F.; Arias-Herrera, S.; Schick, S.G.; Rampf, S.; Byrne, S.; Shazib, M.A.; Örtengren, U.; Lam, W.Y.H.; et al. Insights from the global education survey on the use of VR-haptics in dental education. Front. Dent. Med. 2025, 6, 1576646. [Google Scholar] [CrossRef]
- Khalaf, M.E.; Alkhubaizi, Q.; Alomari, Q.D. Layered Base Plate Blocks and Operative Dentistry Skills. J. Contemp. Dent. Pr. 2018, 19, 554–559. [Google Scholar] [CrossRef]
- Roberson, T.; Heymann, H.O.; Swift, E.J., Jr. Sturdevant’s Art and Science of Operative Dentistry; Elsevier Health Sciences: Amsterdam, Netherlands, 2006. [Google Scholar]
- Di Carvalho Melo, L.; Bastos Silveira, B.; Amorim dos Santos, J.; Cena JAd Damé-Teixeira, N.; Martins, M.D.; De Luca Canto, G.; Neves Silva Guerra, E. Dental education profile in COVID-19 pandemic: A scoping review. Eur. J. Dent. Educ. 2023, 27, 252–261. [Google Scholar] [CrossRef]
- Oleson, A.; Hora, M.T. Teaching the way they were taught? Revisiting the sources of teaching knowledge and the role of prior experience in shaping faculty teaching practices. High. Educ. 2014, 68, 29–45. [Google Scholar] [CrossRef]
- Scott, J. Dental education in Europe: The challenges of variety. J. Dent. Educ. 2003, 67, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Bader, J.D. Challenges in quality assessment of dental care. J. Am. Dent. Assoc. 2009, 140, 1456. [Google Scholar] [CrossRef]
- Reymus, M.; Liebermann, A.; Diegritz, C.; Keßler, A. Development and evaluation of an interdisciplinary teaching model via 3D printing. Clin. Exp. Dent. Res. 2021, 7, 3–10. [Google Scholar] [CrossRef]
- Bader, J.D.; Shugars, D.A. Variation in dentists’clinical decisions. J. Public Health Dent. 1995, 55, 181–188. [Google Scholar] [CrossRef]
- Listl, S.; Faggion Jr, C.; Staehle, H. Professional variability in decision making in modern dentistry: A pilot study. Oper. Dent. 2016, 41, S79–S87. [Google Scholar] [CrossRef] [PubMed]
- Torresin, S.; Pernigotto, G.; Cappelletti, F.; Gasparella, A. Combined effects of environmental factors on human perception and objective performance: A review of experimental laboratory works. Indoor Air. 2018, 28, 525–538. [Google Scholar] [CrossRef]
- Herzog, J.; Karacic, J.; Svellenti, L.; Sahrmann, P. In-vitro simulation methods for mechanical plaque removal: A systematic scoping review of current techniques and future directions. BMC Oral Health 2025, 25, 178. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.P.; Duley, S.I.; Beach, M.M.; Deem, L.; Pileggi, R.; Samet, N.; Segura, A.; Williams, J.N. Dental education economics: Challenges and innovative strategies. J. Dent. Educ. 2008, 72, 1440–1449. [Google Scholar] [CrossRef] [PubMed]
- Chau, R.C.W.; Thu, K.M.; Yu, O.Y.; Hsung, R.T.-C.; Wang, D.C.P.; Man, M.W.H.; Wang, J.J.; Lam, W.Y.H. Evaluation of Chatbot Responses to Text-Based Multiple-Choice Questions in Prosthodontic and Restorative Dentistry. Dent. J. 2025, 13, 279. [Google Scholar] [CrossRef] [PubMed]
- Thurzo, A.; Strunga, M.; Urban, R.; Surovková, J.; Afrashtehfar, K.I. Impact of artificial intelligence on dental education: A review and guide for curriculum update. Educ. Sci. 2023, 13, 150. [Google Scholar] [CrossRef]
- Kuhail, M.A.; Berengueres, J.; Taher, F.; Al Kuwaiti, M. Advances, Applications and the Future of Haptic Technology; Springer: Berlin/Heidelberg, Germany, 2024. [Google Scholar]
- Rung, A.; George, R. A systematic literature review of assessment feedback in preclinical dental education. Eur. J. Dent. Educ. 2021, 25, 135–150. [Google Scholar] [CrossRef]
- Albino, J.E.; Young, S.K.; Neumann, L.M.; Kramer, G.A.; Andrieu, S.C.; Henson, L.; Horn, B.; Hendricson, W.D. Assessing dental students’ competence: Best practice recommendations in the performance assessment literature and investigation of current practices in predoctoral dental education. J. Dent. Educ. 2008, 72, 1405–1435. [Google Scholar] [CrossRef]
- Petersen, P.E. Challenges to improvement of oral health in the 21st century—The approach of the WHO Global Oral Health Programme. Int. Dent. J. 2004, 54, 329–343. [Google Scholar] [CrossRef]
- Petersen, P.E. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent. Oral Epidemiol. 2003, 31, 3–24. [Google Scholar] [CrossRef]
- Chau, R.C.W.; Cheng, A.C.C.; Mao, K.; Thu, K.M.; Ling, Z.; Tew, I.M.; Chang, T.H.; Tan, H.J.; McGrath, C.; Lo, W.L.; et al. External Validation of an AI mHealth Tool for Gingivitis Detection among Older Adults at Daycare Centers: A Pilot Study. Int. Dent. J. 2025, 75, 1970–1978. [Google Scholar] [CrossRef] [PubMed]
- Chau, R.C.-W.; Thu, K.M.; Hsung, R.T.-C.; McGrath, C.; Lam, W.Y.-H. Self-monitoring of Oral Health Using Smartphone Selfie Powered by Artificial Intelligence: Implications for Preventive Dentistry. Oral Health Prev. Dent. 2024, 22, 5758200. [Google Scholar]
- Slavkin, H.C. The impact of research on the future of dental education: How research and innovation shape dental education and the dental profession. J. Dent. Educ. 2017, 81, eS108–eS127. [Google Scholar] [CrossRef] [PubMed]
- Inglehart, M.; Albino, J.; Feine, J.; Okunseri, C. Sociodemographic changes and oral health inequities: Dental workforce considerations. JDR Clin. Transl. Res. 2022, 7, 5S–15S. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).