Consequences of Untreated Dental Caries on Schoolchildren in Mexico State’s Rural and Urban Areas
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Variables
2.3. Data Collection
2.3.1. Questionnaires
2.3.2. Oral Health Assessment
2.3.3. Nutritional Assessment
2.4. Data Analysis
3. Results
3.1. Population Characteristics by Geographical Area
3.2. Consequences of Untreated Dental Caries
3.3. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CUDC | Consequences of untreated dental caries |
| PUFA | Pulp involvement, ulcerations, fistula, and abscess |
| OR | Odds ratio |
| CI | Confidence interval |
| DMFT | Number of decayed, missing, and filled teeth |
| ICDAS | International caries detection and assessment system |
| OHI-S | Simplified Oral Hygiene Index |
| BMI | Body mass index |
References
- Machiulskiene, V.; Campus, G.; Carvalho, J.C.; Dige, I.; Ekstrand, K.R.; Jablonski-Momeni, A.; Maltz, M.; Manton, D.J.; Martignon, S.; Martinez-Mier, E.; et al. Terminology of Dental Caries and Dental Caries Management: Consensus Report of a Workshop Organized by ORCA and Cariology Research Group of IADR. Caries Res. 2020, 54, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Marcenes, W.; Kassebaum, N.J.; Bernabé, E.; Flaxman, A.; Naghavi, M.; Lopez, A.; Murray, C.J. Global burden of oral conditions in 1990–2010: A systematic analysis. J. Dent. Res. 2013, 92, 592–597. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Highlights Oral Health Neglect Affecting Nearly Half of the World’s Population. 2022. Available online: https://www.who.int/news/item/18-11-2022-who-highlights-oral-health-neglect-affecting-nearly-half-of-the-world-s-population (accessed on 7 May 2025).
- World Health Organization. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Petersen, P.E. Sociobehavioural risk factors in dental caries—International perspectives. Community Dent. Oral Epidemiol. 2005, 33, 274–279. [Google Scholar] [CrossRef]
- Tinanoff, N.; Baez, R.J.; Diaz Guillory, C.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: Global perspective. Int. J. Paediatr. Dent. 2019, 29, 238–248. [Google Scholar] [CrossRef]
- Afaneh, H.; Kc, M.; Lieberman, A.; Fenton, A.; Santa Ana, S.; Staples, L.; Conner, J.; Peters, E. Rural-urban disparities in the distribution of dental caries among children in south-eastern Louisiana: A cross-sectional study. Rural Remote Health 2020, 20, 5954. [Google Scholar] [CrossRef]
- Lynch, R.J. The primary and mixed dentition, post-eruptive enamel maturation and dental caries: A review. Int. Dent. J. 2013, 63 (Suppl. 2), 3–13. [Google Scholar] [CrossRef]
- Pakkhesal, M.; Riyahi, E.; Naghavi Alhosseini, A.; Amdjadi, P.; Behnampour, N. Impact of dental caries on oral health related quality of life among preschool children: Perceptions of parents. BMC Oral Health 2021, 21, 68. [Google Scholar] [CrossRef]
- Capurro, D.A.; Iafolla, T.; Kingman, A.; Chattopadhyay, A.; Garcia, I. Trends in income-related inequality in untreated caries among children in the United States: Findings from NHANES I, NHANES III, and NHANES 1999–2004. Community Dent. Oral Epidemiol. 2015, 43, 500–510. [Google Scholar] [CrossRef]
- Kandelman, D.; Arpin, S.; Baez, R.J.; Baehni, P.C.; Petersen, P.E. Oral health care systems in developing and developed countries. Periodontol. 2000 2012, 60, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Gomes, P.R.; Costa, S.C.; Cypriano, S.; Sousa, M.d.L.R.d. Paulínia, São Paulo, Brasil: Situação da cárie dentária com relação às metas OMS 2000 e 2010. Cad. Saúde Pública 2004, 20, 866–870. [Google Scholar] [CrossRef] [PubMed]
- Pitts, N. “ICDAS”—An international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent. Health 2004, 21, 193–198. [Google Scholar]
- Monse, B.; Heinrich-Weltzien, R.; Benzian, H.; Holmgren, C.; van Palenstein Helderman, W. PUFA—An index of clinical consequences of untreated dental caries. Community Dent. Oral Epidemiol. 2010, 38, 77–82. [Google Scholar] [CrossRef]
- Giacaman, R.A.; Bustos, I.P.; Bazán, P.; Mariño, R.J. Oral health disparities among adolescents from urban and rural communities of central Chile. Rural Remote Health 2018, 18, 4312. [Google Scholar] [CrossRef]
- Vélez-León, E.M.; Albaladejo-Martínez, A.; Cuenca-León, K.; Encalada-Verdugo, L.; Armas-Vega, A.; Melo, M. Caries Experience and Treatment Needs in Urban and Rural Environments in School-Age Children from Three Provinces of Ecuador: A Cross-Sectional Study. Dent. J. 2022, 10, 185. [Google Scholar] [CrossRef]
- Al-Rafee, M.A.; AlShammery, A.R.; AlRumikan, A.S.; Pani, S.C. A Comparison of Dental Caries in Urban and Rural Children of the Riyadh Region of Saudi Arabia. Front. Public Health 2019, 7, 195. [Google Scholar] [CrossRef] [PubMed]
- Doley, S.; Srivastava, M.; Piplani, A.; Gupta, R.; Gautam, Y.; Singh, C. Status of Dental Caries and Its Association with Oral Hygiene Practices among School-going Children of Rural and Urban Areas in Kamrup District of Assam. Int. J. Clin. Pediatr. Dent. 2022, 15, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.; Brandt, K.; Wienke, A.; Schaller, H.G. Regional Disparities in Caries Experience and Associating Factors of Ghanaian Children Aged 3 to 13 Years in Urban Accra and Rural Kpando. Int. J. Environ. Res. Public Health 2022, 19, 5771. [Google Scholar] [CrossRef]
- Dalla Nora, Â.; Dalmolin, A.; Gindri, L.D.; Moreira, C.H.C.; Alves, L.S.; Zenkner, J. Oral health status of schoolchildren living in rural and urban areas in southern Brazil. Braz. Oral Res. 2020, 34, e060. [Google Scholar] [CrossRef] [PubMed]
- Beaglehole, R. The Oral Health Atlas: Mapping a Neglected Global Health Issue; FDI World Dental Federation: Geneva, Switzerland, 2009. [Google Scholar]
- Masanja, I.M.; Mumghamba, E.G. Knowledge on gingivitis and oral hygiene practices among secondary school adolescents in rural and urban Morogoro, Tanzania. Int. J. Dent. Hyg. 2004, 2, 172–178. [Google Scholar] [CrossRef]
- Varenne, B.; Petersen, P.E.; Ouattara, S. Oral health behaviour of children and adults in urban and rural areas of Burkina Faso, Africa. Int. Dent. J. 2006, 56, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Vasavan, S.K.; Retnakumari, N. Assessing consequences of untreated dental caries using pufa/PUFA index among 6–12 years old schoolchildren in a rural population of Kerala. J. Indian Soc. Pedod. Prev. Dent. 2022, 40, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Bagińska, J.; Rodakowska, E.; Wilczyńska-Borawska, M.; Jamiołkowski, J. Index of clinical consequences of untreated dental caries (pufa) in primary dentition of children from north-east Poland. Adv. Med. Sci. 2013, 58, 442–447. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Benzian, H.; Monse, B.; Heinrich-Weltzien, R.; Hobdell, M.; Mulder, J.; van Palenstein Helderman, W. Untreated severe dental decay: A neglected determinant of low Body Mass Index in 12-year-old Filipino children. BMC Public Health 2011, 11, 558. [Google Scholar] [CrossRef] [PubMed]
- Karki, S.; Laitala, M.L.; Humagain, M.; Seppänen, M.; Päkkila, J.; Anttonen, V. Oral health status associated with sociodemographic factors of Nepalese schoolchildren: A population-based study. Int. Dent. J. 2018, 68, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional Estadística y Geografía (INEGI). 2020. Available online: https://www.inegi.org.mx/default.html (accessed on 7 May 2025).
- Consejo Nacional de Población (CONAPO). Indices de Marginación por Entidad Federativa y Municipio. 2021. Available online: https://www.gob.mx/conapo/documentos/indices-de-marginacion-2020-284372 (accessed on 7 May 2025).
- Rodrigues, C.R.; Ando, T.; Guimarães, L.O. Simplified oral hygiene index for ages 4 to 6 and 7 to 10 (deciduous and mixed dentition). Rev. Odontol. Univ. Sao Paulo 1990, 4, 20–24. [Google Scholar]
- González-Aragón Pineda, A.E.; García-Pérez, A.; Gómez-Clavel, J.F. Caries experience in adolescents 13–14 years with and without erosive tooth wear: A case-control study. J. Clin. Pediatr. Dent. 2022, 46, 31–37. [Google Scholar] [CrossRef]
- Sánchez-Guerrero, J.; Aguirre-García, E.; Pérez-Dosal, M.R.; Kraus, A.; Cardiel, M.H.; Soto-Rojas, A.E. The wafer test: A semi-quantitative test to screen for xerostomia. Rheumatology 2002, 41, 381–389. [Google Scholar] [CrossRef]
- Sullivan, K.M.; Gorstein, J. ANTHRO: Software for Calculating Pediatric Anthropometry; WHO: Geneva, Switzerland, 1999. [Google Scholar]
- Singhal, D.K.; Singla, N. Severity and Clinical Consequences of Untreated Dental Caries Using PUFA Index Among Schoolchildren in Udupi Taluk, India. J. Orofac. Sci. 2018, 10, 19–23. [Google Scholar] [CrossRef]
- Gören, B.D.; Derelioğlu, S.Ş.; Yılmaz, S. Assessing the Clinical Consequences of Untreated Caries in 8- to 10-Year-Old Children with Pufa Index. J. Adv. Oral Res. 2022, 13, 105–112. [Google Scholar] [CrossRef]
- Romo-Sáenz, C.I.; Chavez-Reyes, E.M.; Gomez-Flores, R.; González-Flores, M.N.; Sosa-Martínez, R.; Cruz-Fierro, N.; Elizondo–Elizondo, J.; De La Garza-Ramos, M.A. Food Insecurity and Dental Caries in Rural Mexican Populations. Int. J. Dent. 2023, 2023, 6694259. [Google Scholar] [CrossRef]
- Jiménez-Gayosso, S.I.; Medina-Solís, C.E.; Lara-Carrillo, E.; Scougal-Vilchis, R.J.; de la Rosa-Santillana, R.; Márquez-Rodríguez, S.; Mendoza-Rodríguez, M.; de Jesús Navarrete-Hernández, J. Socioeconomic inequalities in oral health service utilization any time in their lives for Mexican schoolchildren from 6 to 12 years old. Gac. Med. Mex. 2015, 151, 27–33. [Google Scholar]
- Hernández Vázquez, J.M. Benefits of Health and Wellness Education in the Adult Population in México, 2006. Rev. Electrónica Investig. Educ. 2013, 15, 69–81. [Google Scholar]
- Sekhri, P.; Sandhu, M.; Sachdev, V.; Chopra, R. Estimation of Trace Elements in Mixed Saliva of Caries Free and Caries Active Children. J. Clin. Pediatr. Dent. 2018, 42, 135–139. [Google Scholar] [CrossRef] [PubMed]
- González-Aragón Pineda, A.E.; García Pérez, A.; García-Godoy, F. Salivary parameters and oral health status amongst adolescents in Mexico. BMC Oral Health 2020, 20, 190. [Google Scholar] [CrossRef] [PubMed]
- Spatafora, G.; Li, Y.; He, X.; Cowan, A.; Tanner, A.C.R. The Evolving Microbiome of Dental Caries. Microorganisms 2024, 12, 121. [Google Scholar] [CrossRef]
- Sánchez-Péreza, L.; Alanís-Tavirab, J.; Vera-Hermosilloc, H.; Rodríguez-Gurzad, M.; Arjona-Serranob, J.; Sáenz-Martíneza, L. Ciencias Clínicas. Cienc. Clínicas 2013, 14, 3–11. [Google Scholar]
- Buzalaf, M.A.R.; Pessan, J.P.; Honório, H.M.; Ten Cate, J.M. Mechanisms of action of fluoride for caries control. Monogr. Oral Sci. 2011, 22, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Pontigo-Loyola, A.P.; Mendoza-Rodriguez, M.; de la Rosa-Santillana, R.; Rivera-Pacheco, M.G.; Islas-Granillo, H.; Casanova-Rosado, J.F.; Márquez-Corona, M.L.; Navarrete-Hernández, J.J.; Medina-Solís, C.E.; Manton, D.J. Control of Dental Caries in Children and Adolescents Using Fluoride: An Overview of Community-Level Fluoridation Methods. Pediatr. Rep. 2024, 16, 243–253. [Google Scholar] [CrossRef]
- Simmer, J.P.; Hardy, N.C.; Chinoy, A.F.; Bartlett, J.D.; Hu, J.C. How Fluoride Protects Dental Enamel from Demineralization. J. Int. Soc. Prev. Community Dent. 2020, 10, 134–141. [Google Scholar] [CrossRef]
| Total (%) n = 408 (100.0) | Rural (%) n = 203 (100.0) | Urban (%) n = 205 (100.0) | p | ||
|---|---|---|---|---|---|
| Age | Mean ± S.D. | 10.0 ± 0.9 | 9.9 ± 0.8 | 10.0 ± 0.9 | 0.052 * |
| Sex | Male | 193 (47.3) | 103 (50.7) | 90 (43.9) | 0.167 ** |
| Female | 215 (52.7) | 100 (49.3) | 115 (56.1) | ||
| Artificial juice intake | No | 300 (73.5) | 155 (76.3) | 145 (70.7) | 0.198 ** |
| Yes | 108 (26.5) | 48 (23.7) | 60 (29.3) | ||
| Soft drink consumption | No | 277 (67.8) | 150 (73.8) | 127 (61.9) | 0.010 ** |
| Yes | 131 (32.2) | 53 (26.2) | 78 (38.1) | ||
| Consuming sugary drinks before bed | No | 369 (90.5) | 179 (88.2) | 190 (92.6) | 0.012 ** |
| Yes | 39 (9.5) | 24 (11.8) | 15 (7.4) | ||
| Intake of candy | No | 268 (65.6) | 130 (64.1) | 138 (67.4) | 0.468 ** |
| Yes | 140 (34.4) | 73 (35.9) | 67 (32.6) | ||
| Chewing gum consumption | No | 327 (80.2) | 158 (77.8) | 169 (82.4) | 0.243 ** |
| Yes | 81 (19.8) | 45 (22.2) | 36 (17.6) | ||
| Brushing frequency | Once a day | 82 (20.1) | 57 (28.0) | 25 (12.2) | 0.001 ** |
| At least twice a day | 326 (79.9) | 146 (72.0) | 180 (87.8) | ||
| Use of toothpaste | No | 5 (1.3) | 5 (2.4) | 0 (0.0) | 0.024 *** |
| Yes | 403 (98.7) | 198 (97.6) | 205 (100.0) | ||
| OHI-S | Mean ± S.D. | 1.4 ± 0.6 | 1.7 ± 0.6 | 1.1 ± 0.5 | 0.001 * |
| DMFT | Mean ± S.D. | 5.2 ± 3.1 | 5.9 ± 3.0 | 4.6 ± 3.0 | <0.001 * |
| Total (%) n = 408 (100.0) | Rural (%) n = 203 (100.0) | Urban (%) n = 205 (100.0) | p | ||
|---|---|---|---|---|---|
| Pulp involvement (P) | No | 272 (66.6) | 126 (62.0) | 146 (71.2) | 0.050 * |
| Yes | 136 (33.4) | 77 (38.0) | 59 (28.8) | ||
| Ulceration (U) | No | 405 (99.2) | 200 (98.5) | 205 (100.0) | 0.071 ** |
| Yes | 3 (0.8) | 3 (1.5) | 0 (0.0) | ||
| Fistula (F) | No | 318 (77.9) | 142 (69.9) | 176 (85.8) | <0.001 * |
| Yes | 90 (22.1) | 61 (30.1) | 29 (14.2) | ||
| Abscess (A) | No | 312 (76.4) | 141 (69.5) | 171 (83.4) | 0.001 * |
| Yes | 96 (23.6) | 62 (30.5) | 34 (16.5) | ||
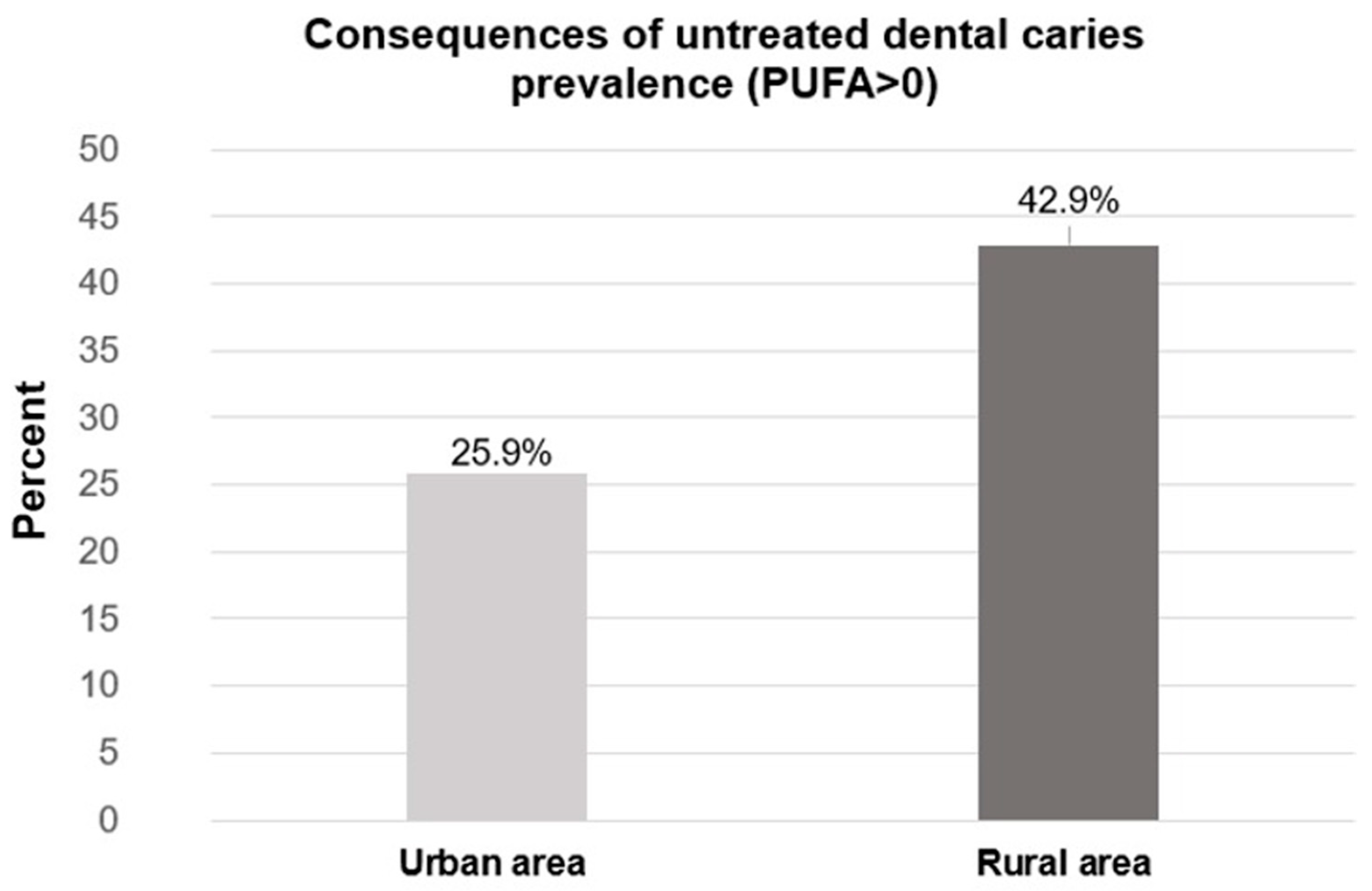
| CUDC (PUFA) | No | 268 (65.7) | 116 (57.1) | 152 (74.1) | 0.007 * |
| Yes | 140 (34.3) | 87 (42.9) | 53 (25.9) |
| Total (%) n = 408 | CUDC = 0 (%) n = 268 | CUDC > 0 n = 140 | p | ||
|---|---|---|---|---|---|
| Nutritional status | Underweight | 8 (100.0) | 5 (62.5) | 3 (37.5) | 0.212 * |
| Normal weight | 209 (100.0) | 134 (64.1) | 75 (35.9) | ||
| Overweight | 97 (100.0) | 59 (60.8) | 38 (39.2) | ||
| Obesity | 94 (100.0) | 70 (74.4) | 24 (25.6) | ||
| Hyposalivation | No | 385 (100.0) | 257 (66.8) | 128 (33.2) | 0.063 ** |
| Yes | 23 (100.0) | 11 (47.8) | 12 (52.2) | ||
| Own toothbrush | No | 34 (100.0) | 21 (61.7) | 13 (38.3) | 0.615 ** |
| Yes | 374 (100.0) | 247 (66.0) | 127 (34.0) | ||
| Topical fluoride application | No | 324 (100.0) | 193 (59.6) | 131 (40.4) | <0.001 ** |
| Yes | 84 (100.0) | 75 (89.2) | 9 (10.8) |
| Variables | Crude OR (CI 95%) | Adjusted OR * (CI 95%) | Age and Sex Adjusted OR (CI 95%) |
|---|---|---|---|
| Geographic area (reference = urban) | 2.19 (1.42–3.56) | 2.16 (1.39–3.42) | 2.15 (1.38–3.34) |
| Hyposalivation (reference = no) | 2.06 (1.24–4.23) | 2.01 (1.19–3.51) | 1.93 (1.11–3.37) |
| Application of topical fluoride (reference = no) | 0.18 (0.12–0.52) | 0.16 (0.09–0.46) | 0.15 (0.07–0.32) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-Núñez, J.C.; González-Aragón Pineda, Á.E.; Vázquez-Ortíz, M.F.; Flores-Preciado, J.C.; Jiménez-Corona, M.E.; Borges-Yáñez, S.A. Consequences of Untreated Dental Caries on Schoolchildren in Mexico State’s Rural and Urban Areas. Dent. J. 2025, 13, 359. https://doi.org/10.3390/dj13080359
Jiménez-Núñez JC, González-Aragón Pineda ÁE, Vázquez-Ortíz MF, Flores-Preciado JC, Jiménez-Corona ME, Borges-Yáñez SA. Consequences of Untreated Dental Caries on Schoolchildren in Mexico State’s Rural and Urban Areas. Dentistry Journal. 2025; 13(8):359. https://doi.org/10.3390/dj13080359
Chicago/Turabian StyleJiménez-Núñez, José Cuauhtémoc, Álvaro Edgar González-Aragón Pineda, María Fernanda Vázquez-Ortíz, Julio César Flores-Preciado, María Eugenia Jiménez-Corona, and Socorro Aída Borges-Yáñez. 2025. "Consequences of Untreated Dental Caries on Schoolchildren in Mexico State’s Rural and Urban Areas" Dentistry Journal 13, no. 8: 359. https://doi.org/10.3390/dj13080359
APA StyleJiménez-Núñez, J. C., González-Aragón Pineda, Á. E., Vázquez-Ortíz, M. F., Flores-Preciado, J. C., Jiménez-Corona, M. E., & Borges-Yáñez, S. A. (2025). Consequences of Untreated Dental Caries on Schoolchildren in Mexico State’s Rural and Urban Areas. Dentistry Journal, 13(8), 359. https://doi.org/10.3390/dj13080359








