1. Introduction
Distalization is a key orthodontic strategy for correcting Class II and Class III malocclusions and can serve as a camouflage approach in cases involving mild to moderate skeletal discrepancies [
1,
2]. This movement involves the posterior displacement of teeth to create anterior space, often avoiding the need for extractions [
3]. Maxillary molar distalization is particularly effective for Class II correction, while mandibular distalization, although less frequently indicated, can contribute to the management of mild Class III cases [
1,
4]. While methods such as mandibular advancement are also employed in the correction of Class II malocclusions, as evidenced by the literature [
5,
6], distalization is particularly indicated in cases where specific dental or skeletal conditions favor its application.
The growing demand for discreet and comfortable orthodontic solutions has contributed to the widespread adoption of clear aligners [
7,
8]. Initially developed for minor tooth movements, systems like Invisalign
® have evolved through technological innovations, such as attachments, precision cuts, and CAD-CAM digital planning tools like ClinCheck
® to enable the execution of more complex movements, including distalization [
9,
10].
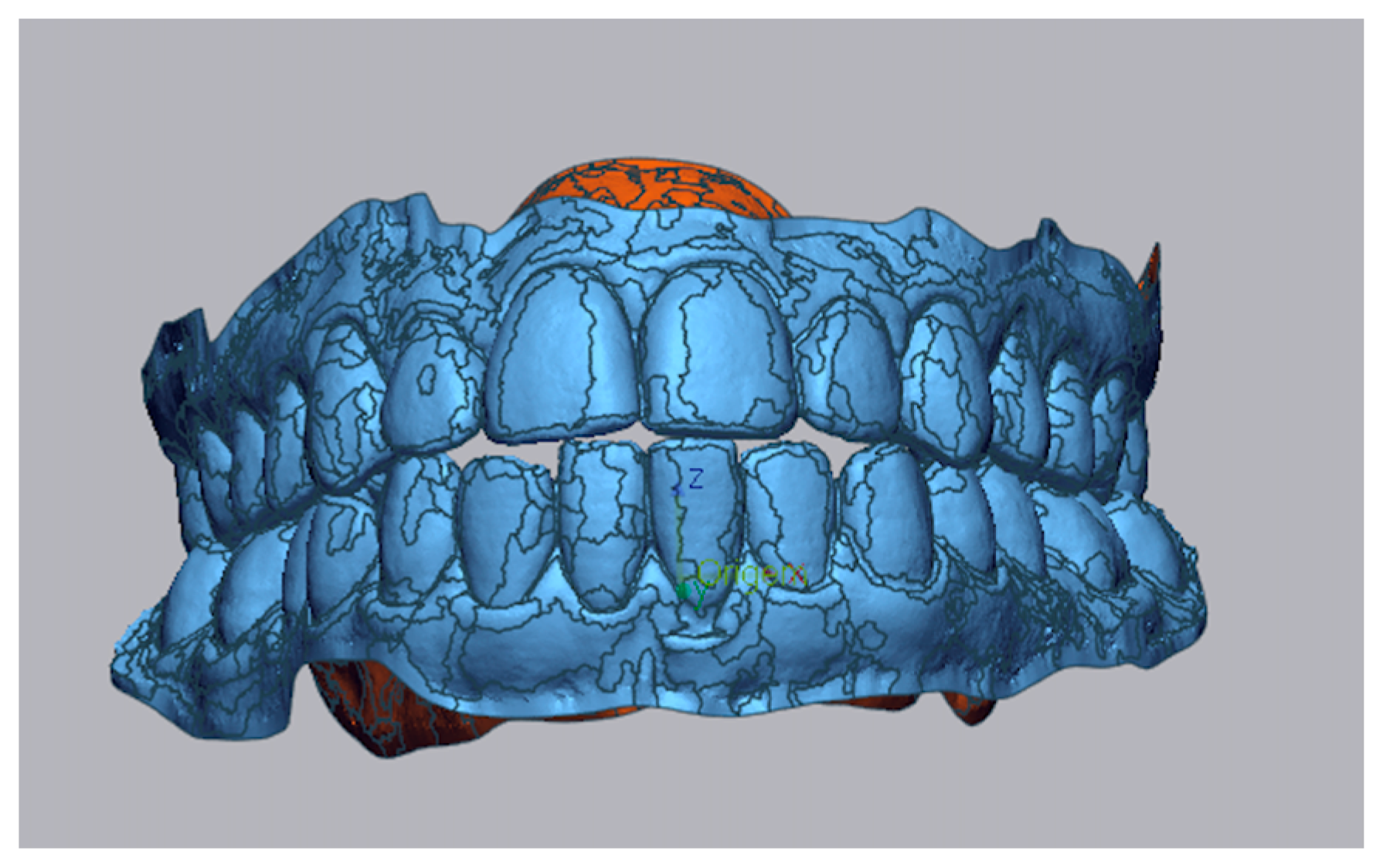
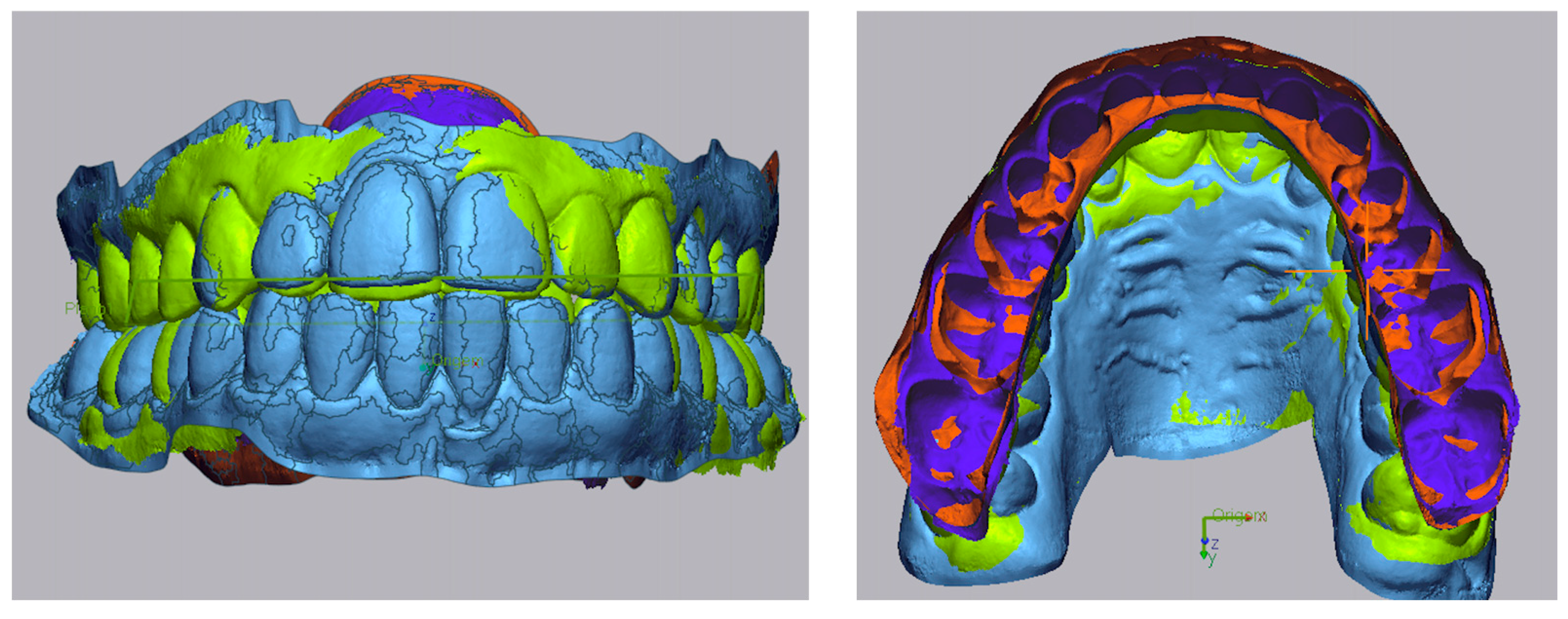
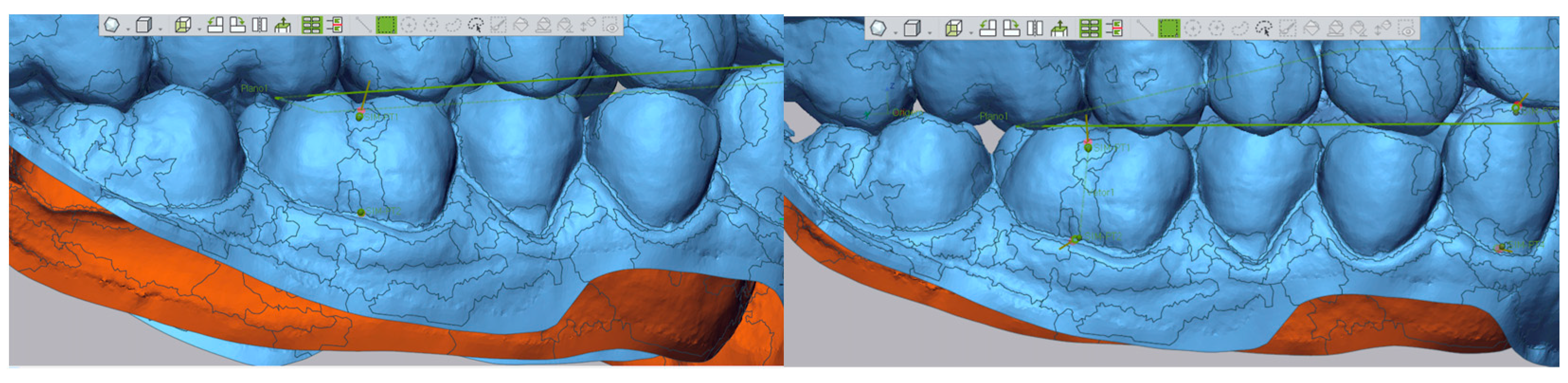
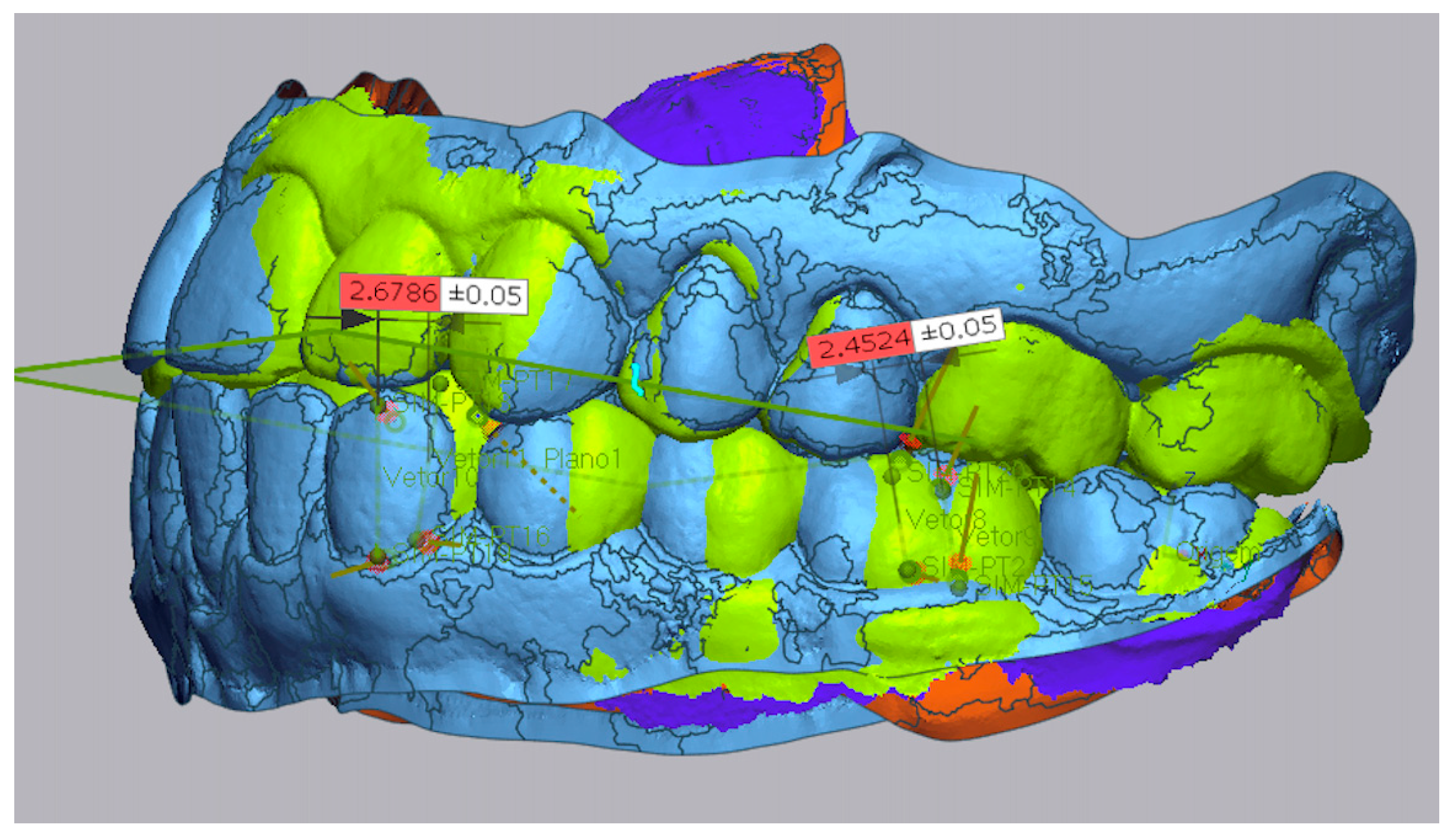
Advancements in 3D scanning technologies and analysis software, such as Geomagic
®, in addition to cephalometric evaluation techniques, have enabled more precise assessments of treatment predictability. Three-dimensional superimpositions enable detailed comparisons to be made between programmed and achieved movements, and cephalometry provides valuable insight into skeletal and dental change [
11].
Recent studies demonstrate that Invisalign
® can achieve maxillary molar distalization of approximately 2.0 mm, typically without significant vertical alterations, and often with discrepancies from planned movements of less than 0.5 mm [
12,
13]. Furthermore, the use of skeletal anchorage devices, such as
mini-screws, has been shown to enhance the predictability and stability of distal movements, especially in complex or asymmetric clinical scenarios [
1,
14].
Despite technological progress, individual anatomical characteristics, including arch length discrepancies, initial crowding, and
skeletal pattern, continue to influence the effectiveness of distalization [
3]. This underscores the necessity of personalized treatment planning. The
Peer Assessment Rating (PAR) index is a valuable tool for quantifying initial malocclusion complexity, although its predictive value regarding treatment outcomes remains to be fully clarified [
15,
16].
Considering the therapeutic potential of distalization in managing both Class II and Class III malocclusions, evaluating the predictability of digital planning tools is critical.
This retrospective study aimed to evaluate the accuracy and clinical outcomes of molar distalization with clear aligners and the impact of mini-screws, facial biotype, and skeletal pattern on treatment results. Planned and achieved tooth movements were assessed by comparing digital models and clinical records before and after treatment.
4. Discussion
Clear aligners represent a discreet and effective orthodontic modality for dental alignment, offering aesthetic advantages without compromising clinical outcomes [
7,
10]. However, their predictability in achieving complex movements such as molar and canine distalization remains under scrutiny [
3].
In this study, clinically relevant distalization was achieved in both arches, yet deviations between programmed and achieved movements consistently exceeded 1 mm. In the maxillary arch, mean deviations were 1.49 ± 1.28 mm for canines and 1.62 ± 1.36 mm for molars. In the mandibular arch, deviations were 1.05 ± 1.31 mm for canines and 1.38 ± 1.29 mm for molars. These results highlight the limited predictability of ClinCheck
® for distalization. Our results are in line with the studies conducted by Taffarel et al. and Li et al. [
19,
20].
The decision to use mini-screws was not based solely on the amount of distalization, but rather on biomechanical complexity and the absence of reciprocal anchorage [
1]. This was particularly relevant in Class III cases, where distalization was combined with retroclined lower incisors, resulting in all movements directed posteriorly, and in Class II cases with pronounced upper incisor proclination, where simultaneous anterior retraction and posterior distalization were required. In both situations, the lack of opposing forces increased unpredictability in movement, justifying the use of skeletal anchorage.
The results of this study indicate that skeletal anchorage with mini-screws significantly enhanced the amount of achieved distalization in the maxillary arch, particularly in both canines (p = 0.006) and molars (p = 0.031). The mean differences were clinically relevant (1.75 mm for canines and 1.74 mm for molars), and the confidence intervals did not include zero, reinforcing the significance of these findings. Planned distalization was also greater in the maxillary group with mini-screws, especially for molars (p = 0.029), suggesting that clinicians felt more confident in programming larger movements when skeletal anchorage was planned.
In contrast, mandibular distalization did not show statistically significant improvement with mini-screws, likely due to anatomical constraints (e.g., dense bone and limited space) [
21] and the fact that all cases involved Class III skeletal patterns. These patterns inherently limit the biological feasibility of extensive distalization.
Nonetheless, despite the lack of statistical significance, a clinically satisfactory outcome was achieved in the end, with the establishment of a Class I occlusion as assessed by the PAR index, indicating effective compensation for the underlying skeletal discrepancy.
Furthermore, when a substantial amount of distalization is required to correct sagittal discrepancies in Class III patients, orthognathic surgery should be considered instead of excessive orthodontic compensation. Attempting to manage these cases with distalization alone may exceed the biological limits of movement and compromise long-term stability [
1].
Notably, neither skeletal pattern, as measured by the ANB angle, nor facial biotype showed significant effects on distalization outcomes. This suggests that, when supported by individualized planning and biomechanical optimization, clear aligner therapy can deliver consistent and effective results across different craniofacial patterns.
The effectiveness of the treatment was objectively confirmed through the Peer Assessment Rating (PAR) index, with a substantial reduction in malocclusion severity observed [
16]. The maxillary distalization group achieved a mean PAR depletion of 86.76%, while the mandibular group achieved 97.16%; this difference was statistically significant (
p = 0.026). These results demonstrate that, despite the mechanical limitations of replicating the planned distalization, the clinical outcomes were highly successful in terms of both function and aesthetics.
It is important to note that the overall complexity of the case was also evaluated using the PAR index, which provides an objective assessment of occlusal irregularity. However, the indication for mini-screws was not guided by the PAR score, but rather by biomechanical considerations, specifically the degree of movement unpredictability and the absence of reciprocal anchorage. Therefore, the clinical complexity that justified skeletal anchorage was distinct from the occlusal complexity measured by the PAR.
Overall, the findings emphasize the importance of having realistic clinical expectations when planning distalization with aligners. To optimize outcomes, adjunctive strategies such as skeletal anchorage, close monitoring of treatment, and individualized staging are essential. Future prospective studies incorporating objective compliance monitoring and larger sample sizes are necessary to refine prediction models and optimize biomechanics for complex movements.
Although the sample size of 30 individuals was adequate for a preliminary analysis, it is relatively small and may limit the generalization of the results. Moreover, as all participants were recruited based on clinic visits, the sample should be considered a convenience sample. In this context of specific clinical issues, an a priori power analysis was not feasible and therefore was not conducted. Future studies with larger, more diverse samples and greater control of clinical variables are needed to confirm and expand these results.
5. Conclusions
Clear aligners can be used to distalize the molars and canines in moderate to complex Class II and Class III cases. However, the predictability of these movements is limited, as planned and achieved outcomes often differ by more than 1 mm.
Nevertheless, substantial clinical improvement was demonstrated through significant reductions in the PAR index, particularly in the mandibular group (97.16%), despite the lack of statistically significant skeletal anchorage effect in the lower arch.
Skeletal anchorage significantly improved the amount and predictability of distalization in the maxillary arch, especially for canines and molars, supporting its use in complex biomechanical cases with absent reciprocal anchorage.
Skeletal pattern and facial biotype had no significant influence on treatment outcomes, reinforcing the relevance of individualized digital planning and biomechanical control.
Adjunctive strategies, such as skeletal anchorage, customized staging, and realistic goals, remain essential to optimize distalization with aligners, especially in borderline cases.