Correlation Between Homogeneity of Different Composite Resins and Their Adhesion to Glass Fiber Posts: In Vitro Assessment
Abstract
1. Introduction
2. Materials and Methods
- I.
- Cores built up with a light-cured composite “bulk-filled” (One Bulk Fill Restorative, 3M ESPE, St. Paul, MN, USA).
- II.
- Cores built up with a dual-cured resin composite—dedicated for core build ups and GFP cementation (Dentocore body, Itena, Paris, France).
2.1. Glass Fiber Post Cementation and Core Build up
2.2. Sample Assessment
2.3. Data Analysis
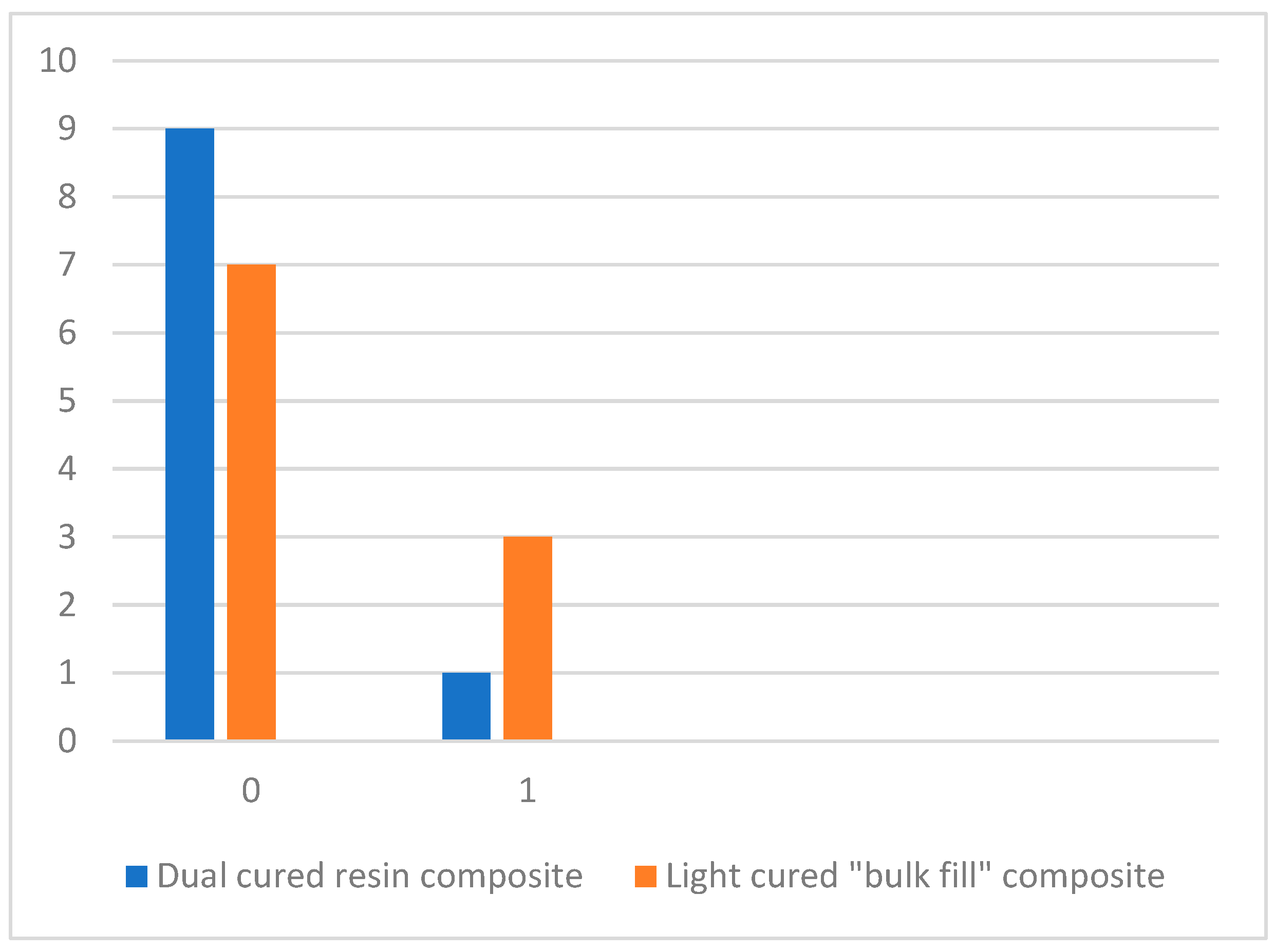
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GFP | Glass fiber post |
| SEM | Scanning electron microscope |
References
- Mergoni, G.; Ganim, M.; Lodi, G.; Figini, L.; Gagliani, M.; Manfredi, M. Single versus multiple visits for endodontic treatment of permanent teeth. Cochrane Database Syst. Rev. 2022, 2023, CD005296. [Google Scholar] [CrossRef]
- Fransson, H.; Dawson, V. Tooth survival after endodontic treatment. Int. Endod. J. 2022, 56, 140–153. [Google Scholar] [CrossRef]
- Alquria, T.A.; Acharya, A.; Tordik, P.; Griffin, I.; Martinho, F.C. Impact of root canal disinfection on the bacteriome present in primary endodontic infection: A next generation sequencing study. Int. Endod. J. 2024, 57, 1124–1135. [Google Scholar] [CrossRef]
- López-Valverde, I.; Vignoletti, F.; Vignoletti, G.; Martin, C.; Sanz, M. Long-term tooth survival and success following primary root canal treatment: A 5- to 37-year retrospective observation. Clin. Oral Investig. 2023, 27, 3233–3244. [Google Scholar] [CrossRef]
- Yan, W.; Jiang, H.; Deng, Z.; Paranjpe, A.; Zhang, H.; Arola, D. Shrinkage strains in the dentin of endodontically treated teeth with water loss. J. Endod. 2021, 47, 806–811. [Google Scholar] [CrossRef]
- Trushkowsky, R.D. Restoration of endodontically treated teeth: Criteria and technique considerations. Quintessence Int. 2014, 45, 557–567. [Google Scholar] [CrossRef]
- Aloqayli, S.; Alsalhi, H.; Alenezi, A. Clinical outcomes and complication rates of endodontically treated teeth with fixed dental prostheses: A retrospective study. Dent. J. 2025, 13, 42. [Google Scholar] [CrossRef]
- Podili, S.; Puthenkandathil, R.; Kulkarni, M.M.; Alobaid, M.A.; Valluri, B.P.; Shaik, Z.A. Fracture resistance of different post–core systems: An in vitro study. J. Pharm. Bioallied Sci. 2023, 15 (Suppl. S1), S239–S243. [Google Scholar] [CrossRef]
- Badami, V.; Ketineni, H.; Akarapu, S.; Mittapalli, S.P.; Khan, A. Comparative evaluation of different post materials on stress distribution in endodontically treated teeth using the Finite Element Analysis method: A systematic review. Cureus 2022, 14, e29753. [Google Scholar] [CrossRef]
- Jurema, A.L.; Filgueiras, A.T.; Santos, K.A.; Bresciani, E.; Caneppele, T.M. Effect of intraradicular fiber post on the fracture resistance of endodontically treated and restored anterior teeth: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 13–24. [Google Scholar] [CrossRef]
- Escobar, L.B.; Pereira da Silva, L.; Manarte-Monteiro, P. Fracture resistance of fiber-reinforced composite restorations: A systematic review and meta-analysis. Polymers 2023, 15, 3802. [Google Scholar] [CrossRef]
- Windle, C.B.; Hill, A.E.; Tantbirojn, D.; Versluis, A. Dual-cure dental composites: Can light curing interfere with conversion? J. Mech. Behav. Biomed. Mater. 2022, 132, 105289. [Google Scholar] [CrossRef]
- Fraga, M.A.; Correr-Sobrinho, L.; Sinhoreti, M.A.; Carletti, T.M.; Correr, A.B. Do dual-cure bulk-fill resin composites reduce gaps and improve depth of cure. Braz. Dent. J. 2021, 32, 77–86. [Google Scholar] [CrossRef]
- Pantiwat, P.; Salimee, P. Effect of different composite core materials on fracture resistance of endodontically treated teeth restored with FRC posts. J. Appl. Oral Sci. 2017, 25, 203–210. [Google Scholar] [CrossRef]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef]
- Lazari, P.; de Carvalho, M.; Del Bel Cury, A.; Magne, P. Survival of extensively damaged endodontically treated incisors restored with different types of posts-and-core foundation restoration material. J. Prosthet. Dent. 2018, 119, 769–776. [Google Scholar] [CrossRef]
- Tjan, A.H.; Bergh, B.H.; Lidner, C. Effect of various incremental techniques on the marginal adaptation of class II composite resin restorations. J. Prosthet. Dent. 1992, 67, 62–66. [Google Scholar] [CrossRef]
- Altassan, M.; Alsulimani, O.; Alzahrani, B.M.; Alghanemi, A.; Abukhudhayr, A.; Alharbi, S.; Munshi, N. Evaluation of the fracture resistance of different designs of all-resin post and core systems: An in vitro study. Cureus 2024, 16, e54137. [Google Scholar] [CrossRef]
- Grandini, S.; Balleri, P.; Ferrari, M. Scanning electron microscopic investigation of the surface of fiber posts after cutting. J. Endod. 2002, 28, 610–612. [Google Scholar] [CrossRef][Green Version]
- Monticelli, F. Micromorphology of the fiber post–resin core unit: A scanning electron microscopy evaluation. Dent. Mater. 2004, 20, 176–183. [Google Scholar] [CrossRef]
- Sarkis-Onofre, R.; Amaral Pinheiro, H.; Poletto-Neto, V.; Bergoli, C.D.; Cenci, M.S.; Pereira-Cenci, T. Randomized controlled trial comparing glass fiber posts and cast metal posts. J. Dent. 2020, 96, 103334. [Google Scholar] [CrossRef] [PubMed]
- Tsolomitis, P.; Diamantopoulou, S.; Papazoglou, E. Contemporary concepts of adhesive cementation of glass fiber posts: A narrative review. J. Clin. Med. 2024, 13, 3479. [Google Scholar] [CrossRef] [PubMed]
- Elfakhri, F.; Alkahtani, R.; Li, C.; Khaliq, J. Influence of filler characteristics on the performance of dental composites: A comprehensive review. Ceram. Int. 2022, 48, 27280–27294. [Google Scholar] [CrossRef]
- Ferrari, M.; Vichi, A.; Grandini, S. Efficacy of different adhesive techniques on bonding to root canal walls: An SEM investigation. Dent. Mater. 2001, 17, 422–429. [Google Scholar] [CrossRef]
- Yu, P.; Xu, Y.-X.; Liu, Y.-S. Polymerization shrinkage and shrinkage stress of bulk-fill and non-bulk-fill resin-based composites. J. Dent. Sci. 2022, 17, 1212–1216. [Google Scholar] [CrossRef]
- Dimitriadi, M.; Petropoulou, A.; Anagnostou, M.; Zafiropoulou, M.; Zinelis, S.; Eliades, G. Effect of curing mode on the conversion and IIT-derived mechanical properties of core build-up resin composites. J. Mech. Behav. Biomed. Mater. 2021, 123, 104757. [Google Scholar] [CrossRef]
- Sá, V.A.; Bittencourt, H.R.; Burnett Júnior, L.H.; Spohr, A.M. Preheated and injected bulk-fill resin composites: A micro-CT analysis of internal voids and marginal adaptation in class II restorations. Materials 2025, 18, 327. [Google Scholar] [CrossRef]



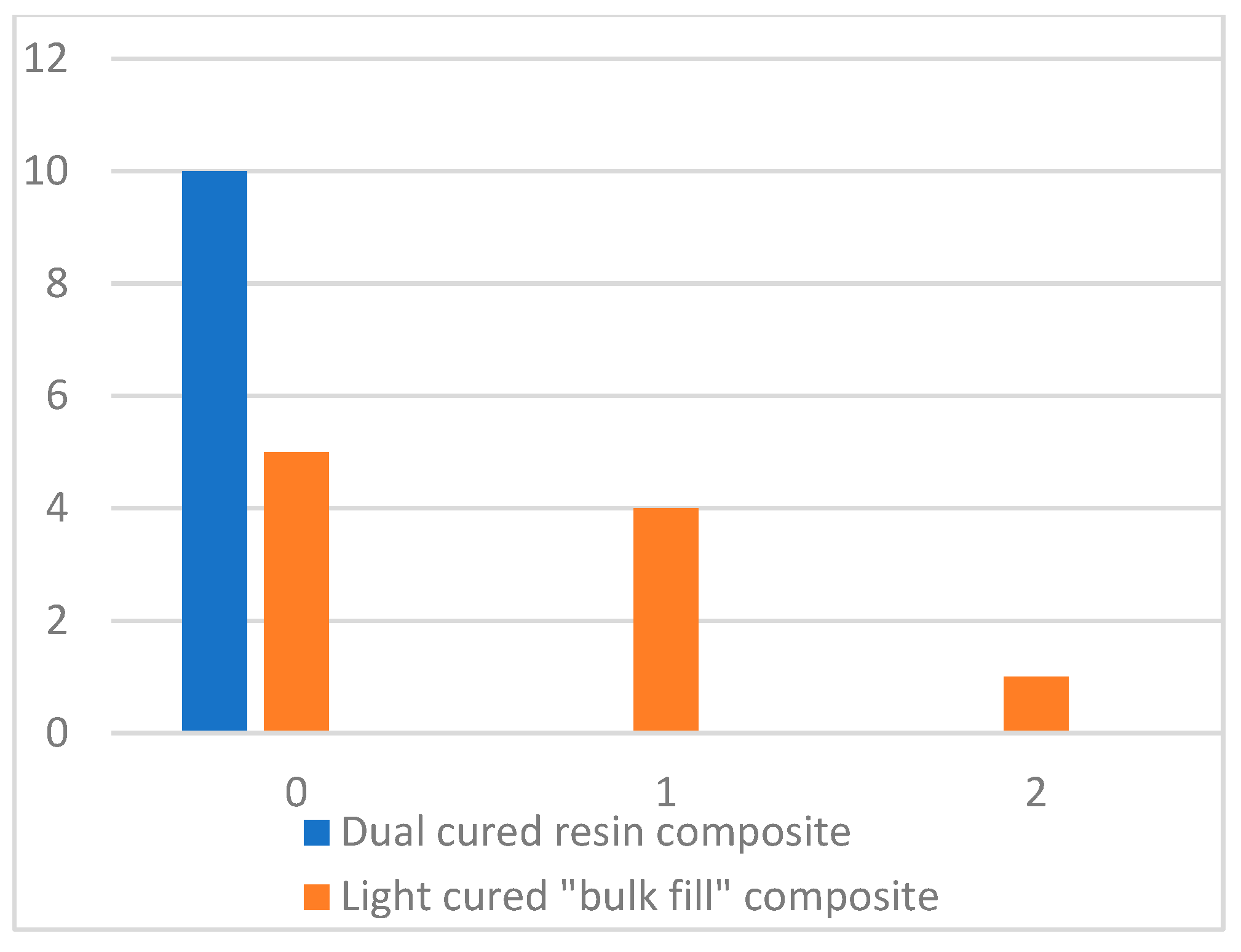
| Groups | Average Rank | Z | p | Mann–Whitney U Test |
|---|---|---|---|---|
| Dual-cured resin composite | 8.00 | −2.500 | 0.012 | 25.000 |
| Light-cured “bulk-filled” composite | 12.00 |
| Groups | Average Rank | Z | p | Mann–Whitney U Test |
|---|---|---|---|---|
| Dual-cured resin composite | 9.50 | −0.756 | 0.301 | 40.000 |
| Light-cured “bulk-filled” composite | 11.50 |
| Pores in Composite Material | Pores Around GFP | |||
|---|---|---|---|---|
| Spearman test | Pores in composite material | Correlation Coefficient | 1.000 | 0.330 |
| Sig. (2-tailed) | 0.156 | |||
| N | 20 | 20 | ||
| Pores around GFP | Correlation Coefficient | 0.330 | 1.000 | |
| Sig. (2-tailed) | 0.156 | |||
| N | 20 | 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oleinikaitė, Ž.; Skirbutis, G.; Rutkauskaitė, G. Correlation Between Homogeneity of Different Composite Resins and Their Adhesion to Glass Fiber Posts: In Vitro Assessment. Dent. J. 2025, 13, 290. https://doi.org/10.3390/dj13070290
Oleinikaitė Ž, Skirbutis G, Rutkauskaitė G. Correlation Between Homogeneity of Different Composite Resins and Their Adhesion to Glass Fiber Posts: In Vitro Assessment. Dentistry Journal. 2025; 13(7):290. https://doi.org/10.3390/dj13070290
Chicago/Turabian StyleOleinikaitė, Živilė, Gediminas Skirbutis, and Greta Rutkauskaitė. 2025. "Correlation Between Homogeneity of Different Composite Resins and Their Adhesion to Glass Fiber Posts: In Vitro Assessment" Dentistry Journal 13, no. 7: 290. https://doi.org/10.3390/dj13070290
APA StyleOleinikaitė, Ž., Skirbutis, G., & Rutkauskaitė, G. (2025). Correlation Between Homogeneity of Different Composite Resins and Their Adhesion to Glass Fiber Posts: In Vitro Assessment. Dentistry Journal, 13(7), 290. https://doi.org/10.3390/dj13070290




