Final-Year Dental Students’ Perceived Confidence: Competencies in General Dentistry
Abstract
1. Introduction
2. Materials and Methods
2.1. Background and Clinical Training Schedule
2.2. Survey 1: Data Collection and Analysis
2.3. Survey 2: Data Collection and Analysis
3. Results
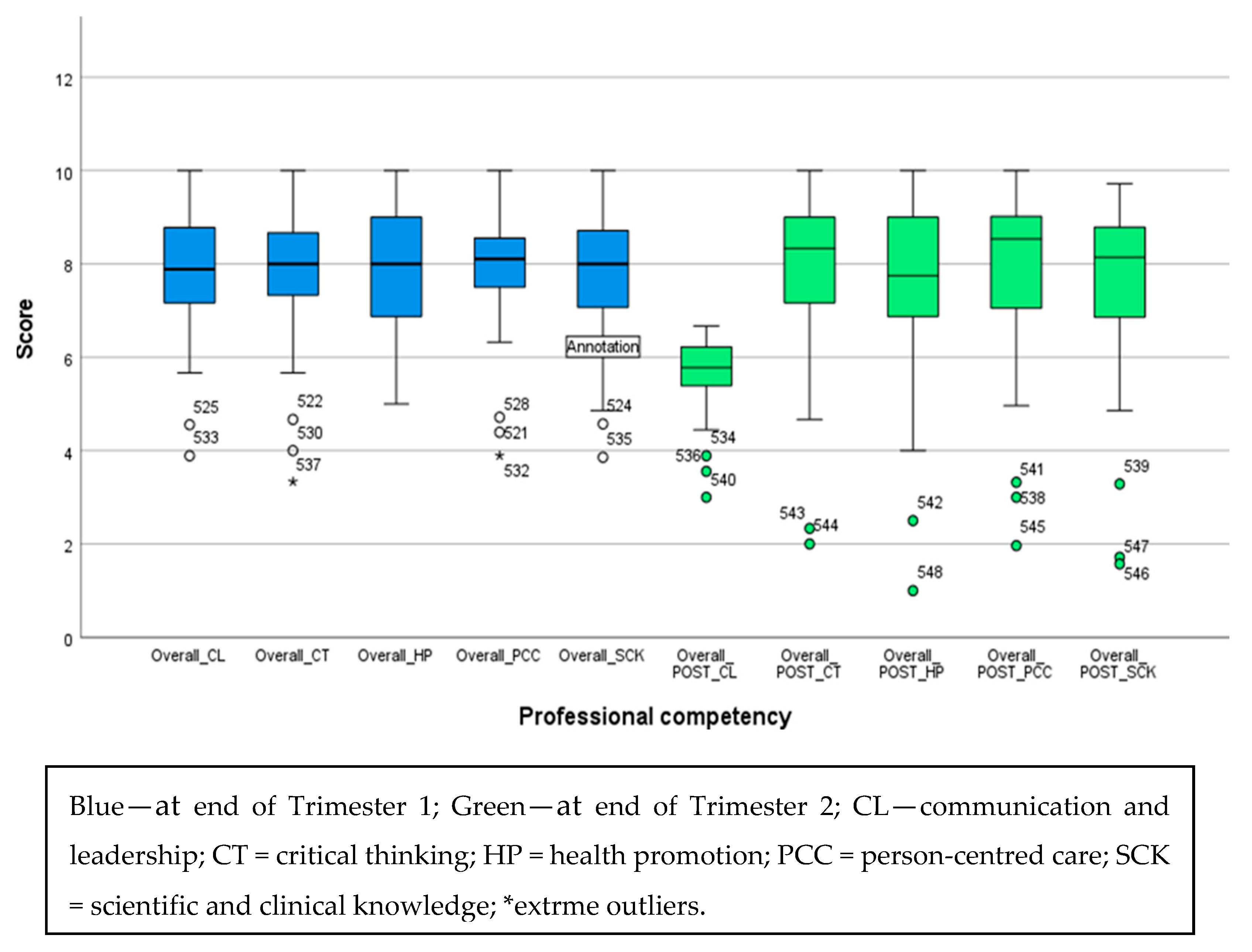
3.1. Survey 1
3.2. Survey 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADC | Australian Dental Council |
| CL | Communication and Leadership |
| CT | Critical Thinking |
| FYDSs | Final-Year Dental Students |
| HP | Health Promotion |
| PCC | ·Person-centred Care |
| SCK | Scientific and Clinical knowledge |
| SD | Standard Deviation |
| SRP | Social Responsibility and Professionalism |
| T1 | Trimester 1 |
| T2 | Trimester 2 |
Appendix A
- What is your gender?
- ○
- Female
- ○
- Male
- ○
- Non-binary
- ○
- Prefer not to say
- What is your age?
- ○
- 18–25 years
- ○
- 26–35 years
- ○
- 36–45 years
- ○
- 46–55 years
- ○
- Above 55 years
- What is your student status?
- ○
- Domestic student
- ○
- International student
- Have you completed a tertiary level degree before commencing the Bachelor of Dental Health Science?
- ○
- Yes
- ○
- No
- ○
- Unsure
- ○
- Prefer not to say
- Have you completed the final year in house training at Griffith University
- ○
- Yes
- ○
- No
- Have you completed the final year out placement training
- ○
- Yes
- ○
- No
| Statement | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 1. Communication and leadership | ||||||||||
| I can engage respectfully with the person receiving care, their families, carers, and communities in relation to oral health | ||||||||||
| I can present information in a manner that enables the person to understand the care and treatment options available, the risks and benefits, and to be involved in decision making about their care | ||||||||||
| I can engage in interprofessional collaborative practice to provide person-centred care | ||||||||||
| I can recognise, assess, and respond to domestic and family violence risk, prioritise safety, provide information, and refer as required | ||||||||||
| I can engage in mentor/mentee activities and leadership within a healthcare team | ||||||||||
| I can maintain one’s own health and wellbeing and support the health and wellbeing of colleagues and team member | ||||||||||
| I can utilise digital technologies and informatics to manage health information and inform person-centred care | ||||||||||
| I can apply the principles of open disclosure in incident management, review adverse events, and implement changes to reduce the risk of reoccurrence | ||||||||||
| I can identify opportunities for improvement in care delivery and advocate for improved oral health outcomes, including for groups or populations at increased risk of harm or poor oral health | ||||||||||
| 2. Critical thinking | ||||||||||
| I can locate, critically appraise and evaluate evidence in a scientific manner to support and deliver oral health care | ||||||||||
| I can apply clinical reasoning and judgement in a reflective practice approach to oral health care | ||||||||||
| I can demonstrate an understanding of research processes and the role of research in advancing knowledge and clinical practice | ||||||||||
| 3. Health promotion | ||||||||||
| I can understand the social determinants of health, risk factors and behaviours that influence health | ||||||||||
| I can understand the connection between health promotion and health policy development | ||||||||||
| I can apply the theories and principles of health promotion to improve oral and general health | ||||||||||
| I can design, implement and evaluate evidence-based health promotion strategies and programs | ||||||||||
| 4. Scientific and clinical knowledge | ||||||||||
| I can apply the social, cultural, biological, biomedical, physical and behavioural sciences in relation to oral health care provision and disease prevention | ||||||||||
| I can apply the theories and principles of population oral health | ||||||||||
| I can apply the scientific principles of infection prevention and control | ||||||||||
| I can understand the scientific basis, limitations, risks of dental materials and demonstrate their use | ||||||||||
| I can apply the principles of risk management and quality improvement | ||||||||||
| I can apply the principles of pharmacology, understanding the limitations and risks of using therapeutic agents, including polypharmacy and overuse, and the implication of the Prescribing Competencies Framework on dental practice | ||||||||||
| I can understand the scientific basis, risks, and demonstrate the safe use of ionising radiation | ||||||||||
| 5. Person centred care | ||||||||||
| 5.1 clinical information gathering | ||||||||||
| I can obtain and record a relevant history of the individual’s medical, social, dietary, and oral health status | ||||||||||
| I can perform an examination for health, disease and abnormalities of the dentition, mouth and associated structures | ||||||||||
| I can select necessary clinical, pathology and other diagnostic procedures and interpret results | ||||||||||
| I can maintain accurate, consistent, legible and contemporaneous records of patient management and protect patient privacy | ||||||||||
| I can evaluate individual patient risk factors for oral disease | ||||||||||
| I can request and/or take radiographs relevant to dental practice | ||||||||||
| 5.2 diagnosis and management planning | ||||||||||
| I can recognise health as it relates to the individual, taking into consideration medical, social and cultural contexts | ||||||||||
| I can diagnose disease or abnormalities of the dentition, mouth and associated structures and identify conditions which require management | ||||||||||
| I can determine the impact of risk factors, systemic disease and medications on oral health and treatment planning | ||||||||||
| I can determine when and how to refer to the appropriate health and or care professional | ||||||||||
| I can obtain and record informed consent and financial consent for treatment | ||||||||||
| I can formulate and record a comprehensive person centred, evidence-based oral health treatment plan | ||||||||||
| 5.3 clinical treatment and evaluation | ||||||||||
| I can apply the principles of disease and trauma prevention and early intervention in the management of the dentition, mouth and associated structures | ||||||||||
| I can ensure the principles of supported decision making and positive behaviour support are incorporated into the provision of person-centred care | ||||||||||
| I can evaluate and monitor the progress of treatment and oral health outcomes | ||||||||||
| I can manage dental emergencies | ||||||||||
| I can manage medical emergencies | ||||||||||
| I can manage diseases, pathology, and conditions associated with the dentition, orofacial complex, and associated structures | ||||||||||
| I can administer, apply and/or prescribe medicines | ||||||||||
| I can manage dental caries | ||||||||||
| I can manage diseases and conditions of the periodontium and supporting tissues of the teeth or their replacements | ||||||||||
| I can manage skeletal and dental occlusal discrepancies | ||||||||||
| I can manage the removal of teeth and oral surgical procedures | ||||||||||
| I can manage diseases and conditions of pulpal and periapical tissues | ||||||||||
| I can manage the loss of tooth structure by restoring the dentition with direct and indirect restorations | ||||||||||
| I can utilise removable prostheses to rehabilitate, restore appearance and function, prevent injury, and stabilise the occlusion | ||||||||||
| I can utilise fixed prostheses to rehabilitate, restore appearance and function and stabilise the occlusion | ||||||||||
| I can manage the individual’s anxiety and pain related to the dentition, mouth and associated structures | ||||||||||
Appendix B
- Start date
- Completion date
- What was your placement site?
- How was the accommodation?
- How did your supervisor assist your learning during your placement?
- What worked well and what did you like about your placement?
- What improvements could be made to the placement to add value to your degree and outcome?
- What aspects of the placement did you find most worthwhile?
- What aspects of the placement could be improved?
- Reflecting back on the placement is there anything else you would like to comment on?
| Statement | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| 1. | During my placement I was able to perform the required skills and learnt new skills. | ||||||||||
| 2. | During my placement I was provided feedback on my clinical performance when I requested it. | ||||||||||
| 3. | During my placement I received constructive feedback on my work from all clinical supervisors. | ||||||||||
| 4. | During my placement felt comfortable asking for support. | ||||||||||
| 5. | How would you rate the value of your placement overall? | ||||||||||
| 6. | Following the placement, I feel confident to work in industry. |
References
- Marino, R.; Delany, C.; Manton, D.J.; Reid, K.; Satur, J.; Crombie, F.; Wong, R.; McNally, C.; Adams, G.G.; Lopez, D. Preparedness for practice of newly qualified dental practitioners in the Australian context: An exploratory study. BMC Med. Educ. 2022, 22, 625. [Google Scholar] [CrossRef]
- Bokhari, S.A.H.; Rashed, H.T.; Al-Farhan, M.F. Evaluation of perceived competency of dental graduates of Saudi Arabia. Educ. Res. Int. 2022, 2022, 2600474. [Google Scholar] [CrossRef]
- Elmanaseer, W.R.; Al-Omoush, S.A.; Alamoush, R.A.; Abu Zaghlan, R.; Alsoleihat, F. Dental Students’ Perception and Self-Perceived Confidence Level in Key Dental Procedures for General Practice and the Impact of Competency Implementation on Their Confidence Level, Part I (Prosthodontics and Conservative Dentistry). Int. J. Dent. 2023, 2023, 2015331. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.; Holder, A. Dental undergraduate students’ perceptions about placements in primary dental care during the undergraduate dental curriculum: A qualitative evidence synthesis. Br. Dent. J. 2022, 233, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Australian Dental Council. Professional Competencies of the Newly Qualified Dental Practitioner; ADC: Melbourne, Australia, 2022. [Google Scholar]
- Gilmour, A.; Welply, A.; Cowpe, J.; Bullock, A.D.; Jones, R.J. The undergraduate preparation of dentists: Confidence levels of final year dental students at the School of Dentistry in Cardiff. Br. Dent. J. 2016, 221, 349–354. [Google Scholar] [CrossRef]
- Kulkarni, S.; Dagli, N.; Duraiswamy, P.; Desai, H.; Vyas, H.; Baroudi, K. Stress and professional burnout among newly graduated dentists. J. Int. Soc. Prev. Community Dent. 2016, 6, 535–541. [Google Scholar] [CrossRef]
- Ilic, J.; Radović, K.; Savić-Stanković, T.; Popovac, A.; Miletić, V.; Milić Lemić, A. The effect of COVID-19 pandemic on final year dental students’ self-confidence level in performing clinical procedures. PLoS ONE 2021, 16, e0257359. [Google Scholar] [CrossRef]
- Manakil, J.; George, R. Self-perceived work preparedness of the graduating dental students. Eur. J. Dent. Educ. 2013, 17, 101–105. [Google Scholar] [CrossRef]
- Mariño, R.; Hawthorne, L.; Morgan, M.; Ismail, M. Transcultural skills content in a dental curriculum: A comparative study. Eur. J. Dent. Educ. 2012, 16, e33–e40. [Google Scholar] [CrossRef]
- Manakil, J.; Rihani, S.; George, R. Preparedness and practice management skills of graduating dental students entering the work force. Educ. Res. Int. 2015, 2015, 976124. [Google Scholar] [CrossRef]
- Rajan, S.; Chen, H.Y.; Chen, J.J.; Chin-You, S.; Chee, S.; Chrun, R.; Byun, J.; Abuzar, M. Final year dental students’ self-assessed confidence in general dentistry. Eur. J. Dent. Educ. 2020, 24, 233–242. [Google Scholar] [CrossRef]
- Lalloo, R.; Evans, J.L.; Johnson, N.W. Dental care provision by students on a remote rural clinical placement. Aust. N. Z. J. Public Health 2013, 37, 47–51. [Google Scholar] [CrossRef]
- Meisha, D.E.; Al-dabbagh, R.A. Self-confidence as a predictor of senior dental student academic success. J. Dent. Educ. 2021, 85, 1497–1503. [Google Scholar] [CrossRef]
- Schmitz, C. LimeSurvey: An Open Source Survey Tool; LimeSurvey Project: Hamburg, Germany, 2012; Available online: http://www.limesurvey.org (accessed on 5 May 2025).
- Kelley, K.; Clark, B.; Brown, V.; Sitzia, J. Good practice in the conduct and reporting of survey research. Int. J. Qual. Health Care 2003, 15, 261–266. [Google Scholar] [CrossRef]
- Hazarika, D.; Konwar, G.; Deb, S.; Bora, D.J. Sentiment Analysis on Twitter by Using TextBlob for Natural Language Processing. ICRMAT 2020, 24, 63–67. [Google Scholar]
- Ghaemi-Amiri, M.; Mirzapour, A.; Gholinia, H.; Sistani, M.M.N. Self-assessment of professional competence and influential factors among dental students. J. Dent. Educ. 2024, 88, 1625–1633. [Google Scholar] [CrossRef]
- Sun, J.; Adegbosin, A.E.; Reher, V.; Rehbein, G.; Evans, J. Validity and reliability of a self-assessment scale for Dental and Oral Health student’s perception of transferable skills in Australia. Eur. J. Dent. Educ. 2020, 24, 42–52. [Google Scholar] [CrossRef]
- Bowers, A.D.; Peters, O.A.; Subar, P.; March, S.; Peters, C.I. Dental Student Community Clinic Placement in Australia and the United States: Systematic Review and Case Study. J. Calif. Dent. Assoc. 2022, 50, 49–61. [Google Scholar] [CrossRef]
- Aston-Mourney, K.; McLeod, J.; Rivera, L.R.; McNeill, B.A.; Baldi, D.L. Prior degree and academic performance in medical school: Evidence for prioritising health students and moving away from a bio-medical science-focused entry stream. BMC Med. Educ. 2022, 22, 700. [Google Scholar] [CrossRef]
- Arheiam, A.; Bankia, I.; Ingafou, M. Perceived competency towards preventive dentistry among dental graduates: The need for curriculum change. Libyan J. Med. 2015, 10, 26666. [Google Scholar] [CrossRef]
- Bracksley-O’Grady, S.; Anderson, K.; Dickson-Swift, V.; Masood, M. Curriculum mapping of health promotion competencies in dental and oral health training programmes in Australia. Health Promot. J. Aust. 2022, 33, 98–113. [Google Scholar] [CrossRef]
- Chi, M.T.; Glaser, R.; Farr, M.J. The Nature of Expertise; Psychology Press: Brighton and Hove, UK, 2014. [Google Scholar]
- Repo, S.; Lehtinen, T.; Rusanen, E.; Hyytinen, H. Prior education of Open University students contributes to their capability in critical thinking. J. Adult Contin. Educ. 2017, 23, 61–77. [Google Scholar] [CrossRef]
- Calvert, M.J.; Ross, N.M.; Freemantle, N.; Xu, Y.; Zvauya, R.; Parle, J.V. Examination performance of graduate entry medical students compared with mainstream students. J. R. Soc. Med. 2009, 102, 425–430. [Google Scholar] [CrossRef]
- Craig, P.L.; Gordon, J.; Clark, R.; Langendyk, V. Prior academic background and student performance in assessment in a graduate entry programme. BMC Med. Educ. 2004, 38, 1164–1168. [Google Scholar] [CrossRef]
- De Clercq, L.; Pearson, S.-A.; Rolfe, I.E. The relationship between previous tertiary education and course performance in first year medical students at Newcastle University, Australia. Educ. Health 2001, 14, 417–426. [Google Scholar] [CrossRef]
- Dodds, A.E.; Reid, K.J.; Conn, J.J.; Elliott, S.L.; McColl, G.J. Comparing the academic performance of graduate-and undergraduate-entry medical students. Med. Educ. 2010, 44, 197–204. [Google Scholar] [CrossRef]
- Ludin, S.M. Does good critical thinking equal effective decision-making among critical care nurses? A cross-sectional survey. Intensive Crit. Care Nurs. 2018, 44, 1–10. [Google Scholar] [CrossRef]
- Purvis, C.A. Factors That Influence the Development of Critical Thinking Skills in Associate Degree Nursing Students. Ph.D. Thesis, University of Georgia, Athens, GA, USA, 2009. [Google Scholar]
- Azizi-Fini, I.; Hajibagheri, A.; Adib-Hajbaghery, M. Critical thinking skills in nursing students: A comparison between freshmen and senior students. Nurs. Midwifery Stud. 2015, 4, e25721. [Google Scholar] [CrossRef]
- Hunter, S.; Pitt, V.; Croce, N.; Roche, J. Critical thinking skills of undergraduate nursing students: Description and demographic predictors. Nurse Educ. Today. 2014, 34, 809–814. [Google Scholar] [CrossRef]
- Mousazadeh, S.; Momennasab, M.; Bakhtiari, T.; Reisi, M. Nursing students’ disposition toward critical thinking and its relationship with their academic performance. Nursing 2016, 5, 61. [Google Scholar] [CrossRef]
- Abuzar, M.A.; Owen, J. A community engaged dental curriculum: A rural Indigenous outplacement programme. J. Public Health Res. 2016, 5, 668. [Google Scholar] [CrossRef]
| Characteristic | No of Students in T1 | (%) | No of Students in T2 | (%) |
|---|---|---|---|---|
| Age | ||||
| 18–25 years | 32 | 47.11 | 12 | 34.3 |
| 26–35 years | 29 | 42.6 | 18 | 51.4 |
| 36–45 years | 7 | 10.3 | 3 | 8.6 |
| Above 45 | 0 | 0 | 2 | 5.7 |
| Total | 68 | 100.0 | 35 | 100.0 |
| Gender | ||||
| Male | 33 | 48.5 | 12 | 34.3 |
| Female | 34 | 50.0 | 21 | 60.0 |
| Non-binary | 1 | 1.5 | 2 | 5.7 |
| Total | 68 | 100.0 | 35 | 100.0 |
| Student status | ||||
| Domestic | 47 | 69.1 | 25 | 71.4 |
| International | 21 | 30.9 | 10 | 28.6 |
| Total | 68 | 100.0 | 35 | 100.0 |
| Previous tertiary degree | ||||
| Completed | 37 | 54.4 | 23 | 65.7 |
| Not completed | 31 | 45.6 | 12 | 34.3 |
| Total | 68 | 100.0 | 35 | 100.0 |
| Placement | ||||
| In-house (university) | 26 | 38.2 | 20 | 57.1 |
| Outplacement | 42 | 61.8 | 15 | 42.9 |
| Total | 68 | 100.0 | 35 | 100.0 |
| Variables | Less than Median Level of Confidence N (%) | More than Median Level of Confidence N (%) | Fisher’s Exact Test Value | p-Value | |
|---|---|---|---|---|---|
| CT | Completed a previous degree | 11 (16.2) | 26 (38.2) | 5.537 | 0.019 |
| Did not complete a previous degree | 18 (25.6) | 13 (19.1) | |||
| Total | 29 (42.6) | 39 (57.4) | |||
| CL | Completed a previous degree | 12 (17.6) | 25 (36.8) | 5.663 | 0.017 |
| Did not complete a previous degree | 19 (27.9) | 12 (17.6) | |||
| Total | 31 (45.6) | 37 (54.4) | |||
| Variables | <Median Confidence | >Median Confidence | Fisher’s Exact Test Value | p-Value | |
|---|---|---|---|---|---|
| N (%) | N (%) | ||||
| HP | Completed a | 7 (20.0) | 16 (45.7) | 4.227 | 0.040 |
| previous degree | |||||
| Did not complete a previous degree | 8 (22.9) | 4 (11.4) | |||
| Total | 15 (42.9) | 20 (57.1) | |||
| SCK | Completed a previous degree | 7(20.0) | 16 (45.7) | 6.311 | 0.012 |
| Did not complete a previous degree | 9 (25.7) | 3 (8.6) | |||
| Total | 16 (45.7) | 19 (54.3) | |||
| SCK | 18–25 years | 9 (25.7) | 3 (8.6) | 6.547 | 0.040 |
| 26–35 years | 5 (14.3) | 13 (37.1) | |||
| 36 years and above | 2 (5.7) | 3 (8.6) | |||
| Total | 16 (45.7) | 19 (54.3) | |||
| CT | 18–25 years | 9 (25.7) | 3 (8.6) | 8.486 | 0.014 |
| 26–35 years | 4 (11.4) | 14 (40.0) | |||
| 36 years and above | 3 (8.6) | 2 (5.7) | |||
| Total | 16 (45.7) | 19 (54.3) | |||
| Variable | Group | <Median Confidence | >Median Confidence | Total N | Fisher’s Exact Test Value |
|---|---|---|---|---|---|
| PCC | T1 outplacement | 20 (47.6%) | 22 (52.4%) | 68 | 0.036 |
| PCC | T1 in-house | 13 (50.0%) | 13 (50.0%) | ||
| PCC | Total | 33 (48.5%) | 35 (51.5%) | ||
| SCK | T1 outplacement | 9 (45.2%) | 23 (54.8%) | 68 | 0.005 |
| SCK | T1 in-house | 12 (46.2%) | 14 (53.8%) | ||
| SCK | Total | 31 (45.6%) | 37 (54.4%) | ||
| HP | T1 outplacement | 16 (51.6%) | 26 (61.9%) | 68 | 2.486 |
| HP | T1 in-house | 15 (57.7%) | 11 (42.3%) | ||
| HP | Total | 31 (45.6%) | 37 (54.4%) | ||
| CT | T1 outplacement | 18 (42.9%) | 24 (57.1%) | 68 | 0.002 |
| CT | T1 in-house | 11 (42.3%) | 15 (57.7%) | ||
| CT | Total | 29 (42.6%) | 39 (57.4%) | ||
| CL | T1 outplacement | 19 (45.2%) | 23 (54.8%) | 68 | 0.005 |
| CL | T1 in-house | 12 (46.2%) | 14 (53.8%) | ||
| CL | Total | 31 (45.6%) | 37 (54.4%) | ||
| Overall confidence | T1 outplacement | 19 (45.2%) | 23 (54.8%) | 68 | 0.005 |
| Overall confidence | T1 in-house | 12 (46.2%) | 14 (53.8%) | 68 | |
| PCC | T2 in-house | 10 (50.0%) | 10 (50.0%) | 35 | 0.038 |
| PCC | T2 outplacement | 7 (46.7%) | 8 (53.3%) | ||
| PCC | Total | 17 (48.6%) | 18 (51.4%) | ||
| SCK | T2 in-house | 9 (45.0%) | 11 (55.0%) | 35 | 0.01 |
| SCK | T2 outplacement | 7 (46.7%) | 8 (53.3%) | ||
| SCK | Total | 16 (45.7%) | 19 (54.3%) | ||
| HP | T2 in-house | 6 (30.0%) | 14 (70.0%) | 35 | 3.15 |
| HP | T2 outplacement | 9 (60.0%) | 6 (40.0%) | ||
| HP | Total | 15 (42.9%) | 20 (57.1%) | ||
| CT | T2 in-house | 10 (50.0%) | 10 (50.0%) | 35 | 0.345 |
| CT | T2 outplacement | 6 (40.0%) | 9 (60.0%) | ||
| CT | Total | 16 (45.7%) | 19 (54.3%) | ||
| CL | T2 in-house | 8 (40.0%) | 12 (60.0%) | 35 | 0.614 |
| CL | T2 outplacement | 8 (53.7%) | 7 (46.7%) | ||
| CL | Total | 16 (45.7%) | 19 (54.3%) | ||
| Overall confidence | T2 in-house | 8 (40.0%) | 12 (60.0%) | 35 | 0.00 |
| Overall confidence | T2 outplacement | 6 (40.0%) | 9 (60.0%) | 35 |
| Item | Mean | Median | Standard Deviation | Skewness | Kurtosis | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| During my placement I was able to perform the required skills and learnt new skills | 8.4 | 8.0 | 1.45 | −0.47 | −0.40 | 5.0 | 10.0 |
| During my placement I was provided feedback on my clinical performance when requested | 8.9 | 10.0 | 1.43 | −1.25 | 0.47 | 5.0 | 10.0 |
| During my placement I received constructive feedback from all clinical supervisors | 8.5 | 9.0 | 1.66 | −1.02 | 0.23 | 4.0 | 10.0 |
| During my placement I felt comfortable asking for support | 9.2 | 10.0 | 1.23 | −1.30 | 0.23 | 6.0 | 10.0 |
| How would you rate the value of your placement overall | 8.6 | 9.0 | 1.79 | −1.65 | 2.28 | 3.0 | 10.0 |
| Following the placement, I feel confident to work in industry | 7.9 | 8.0 | 1.63 | −1.37 | 2.68 | 3.0 | 10.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yaparathna, N.; Udayamalee, I.; Gray, M.; He, C.; Wu, R.; Taing, C.; Abuzar, M. Final-Year Dental Students’ Perceived Confidence: Competencies in General Dentistry. Dent. J. 2025, 13, 268. https://doi.org/10.3390/dj13060268
Yaparathna N, Udayamalee I, Gray M, He C, Wu R, Taing C, Abuzar M. Final-Year Dental Students’ Perceived Confidence: Competencies in General Dentistry. Dentistry Journal. 2025; 13(6):268. https://doi.org/10.3390/dj13060268
Chicago/Turabian StyleYaparathna, Navodika, Iresha Udayamalee, Megan Gray, Cheree He, Rachel Wu, Chelsea Taing, and Menaka Abuzar. 2025. "Final-Year Dental Students’ Perceived Confidence: Competencies in General Dentistry" Dentistry Journal 13, no. 6: 268. https://doi.org/10.3390/dj13060268
APA StyleYaparathna, N., Udayamalee, I., Gray, M., He, C., Wu, R., Taing, C., & Abuzar, M. (2025). Final-Year Dental Students’ Perceived Confidence: Competencies in General Dentistry. Dentistry Journal, 13(6), 268. https://doi.org/10.3390/dj13060268







