The Clinical Application of the ARi® Implant System in Severely Resorbed Anterior Alveolar Ridges: A Case Report
Abstract
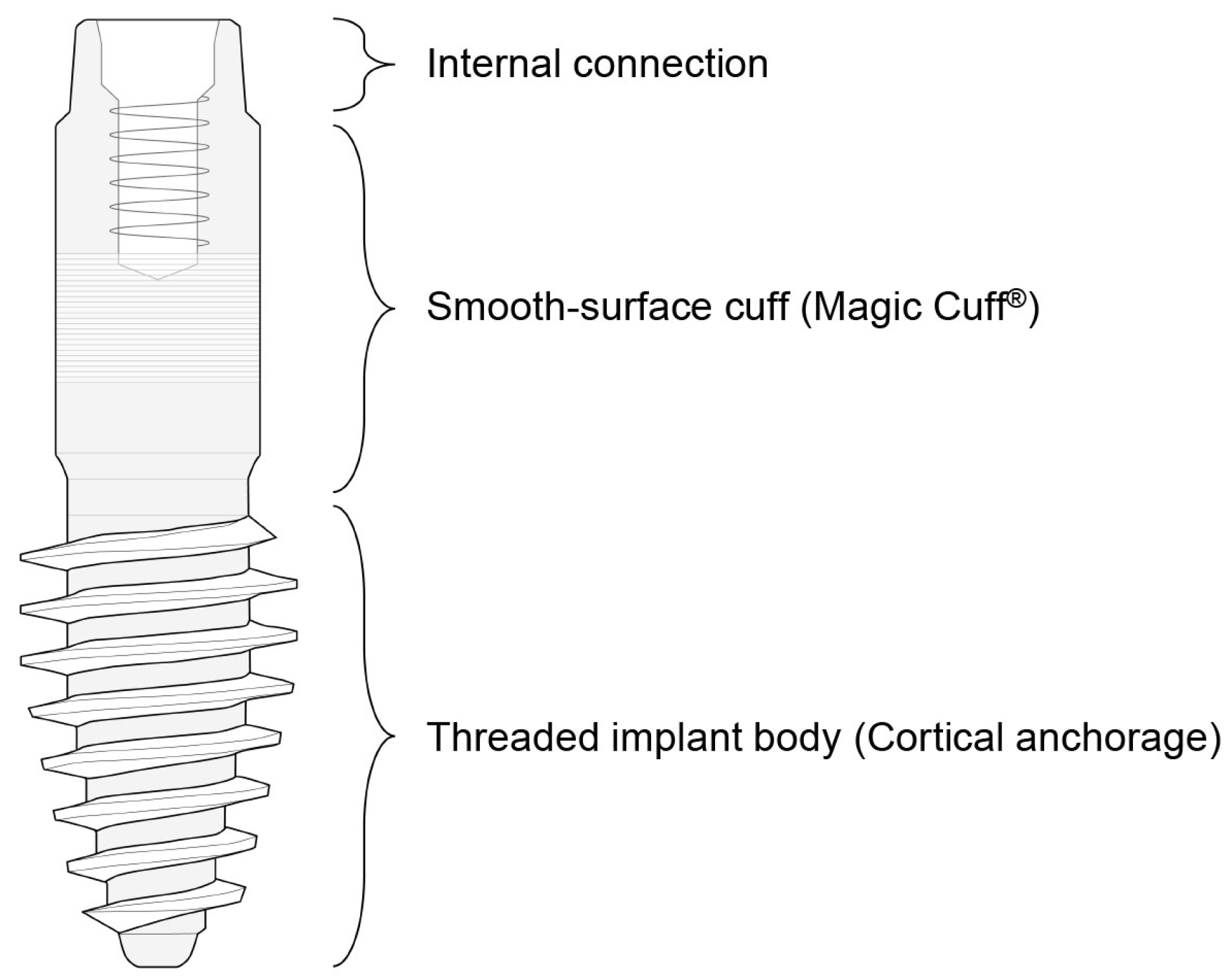
1. Introduction
2. Case Reports
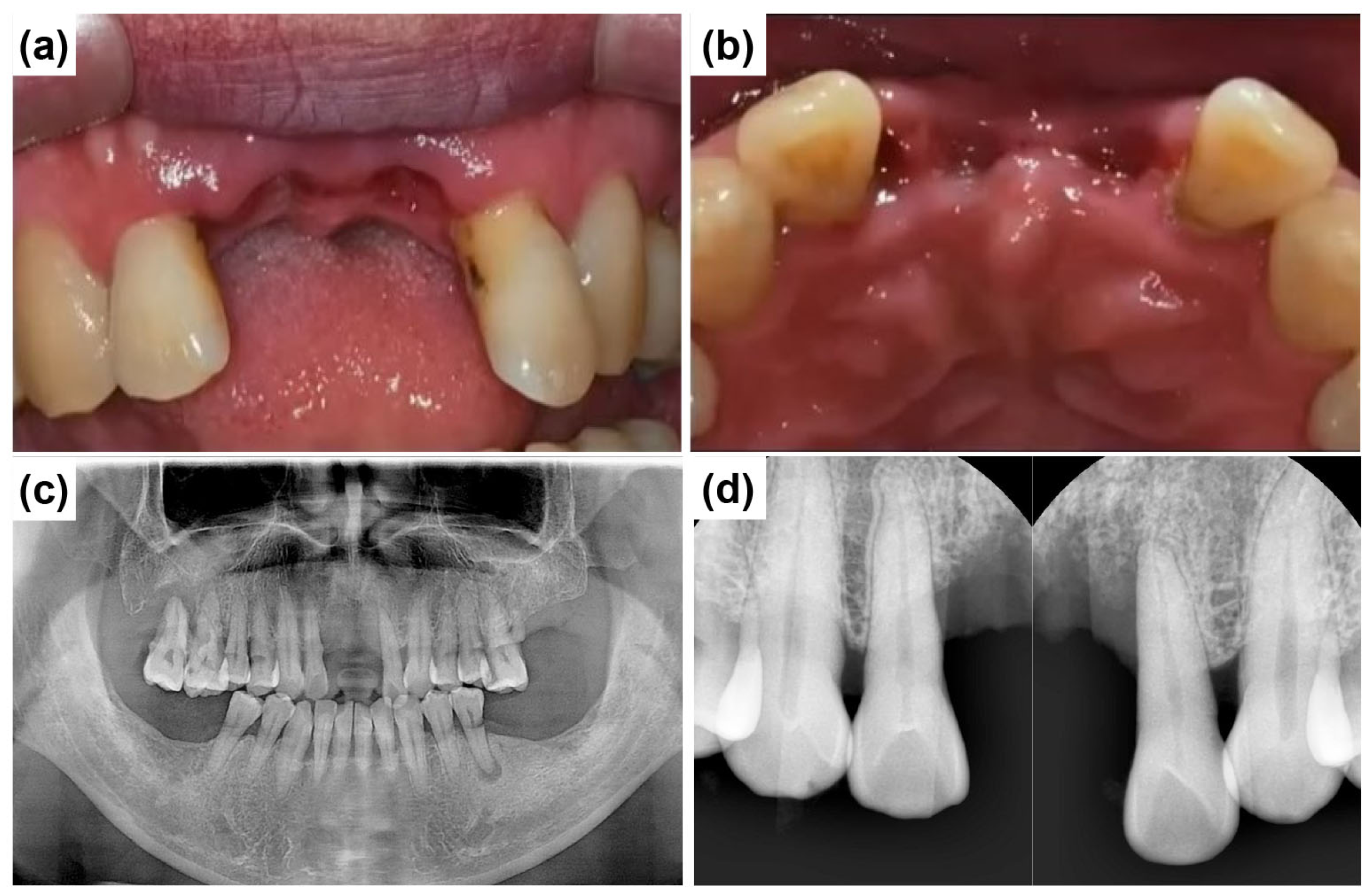
2.1. Case Report 1
2.2. Case Report 2
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, P.; Yu, S.; Zhu, G. The psychosocial impacts of implantation on the dental aesthetics of missing anterior teeth patients. Br. Dent. J. 2012, 213, E20. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.M.; Nascimento, C.C.; Barbosa, G.C.G.; Coqueiro, R.S. Do dental esthetics have any influence on finding a job? Am. J. Orthod. Dentofac. Orthop. 2014, 146, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Boardman, N.; Darby, I.; Chen, S. A retrospective evaluation of aesthetic outcomes for single-tooth implants in the anterior maxilla. Clin. Oral Implant. Res. 2016, 27, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Pathak, A.; Dhamande, M.M.; Gujjelwar, S.; Sonar, P.R.; Tawade, S.U.; Gupta, A. Basal implant placement in the anterior aesthetic zone: A case report. Cureus 2024, 16, e61782. [Google Scholar] [CrossRef]
- Patel, K.; Madan, S.; Mehta, D.; Shah, S.P.; Trivedi, V.; Seta, H. Basal implants: An asset for rehabilitation of atrophied resorbed maxillary and mandibular jaw—A prospective study. Ann. Maxillofac. Surg. 2021, 11, 64–69. [Google Scholar] [CrossRef]
- Chiapasco, M.; Casentini, P.; Zaniboni, M. Bone augmentation procedures in implant dentistry. Int. J. Oral Maxillofac. Implant. 2009, 24, 237–259. [Google Scholar] [PubMed]
- Titsinides, S.; Agrogiannis, G.; Karatzas, T. Bone grafting materials in dentoalveolar reconstruction: A comprehensive review. Jpn. Dent. Sci. Rev. 2019, 55, 26–32. [Google Scholar] [CrossRef]
- Buser, D.; Urban, I.; Monje, A.; Kunrath, M.F.; Dahlin, C. Guided bone regeneration in implant dentistry: Basic principle, progress over 35 years, and recent research activities. Periodontology 2000 2023, 93, 9–25. [Google Scholar] [CrossRef]
- Garg, R.; Mishra, N.; Alexander, M.; Gupta, S.K. Implant survival between endo-osseous dental implants in immediate loading, delayed loading, and basal immediate loading dental implants a 3-year follow-up. Ann. Maxillofac. Surg. 2017, 7, 237–244. [Google Scholar] [CrossRef]
- Roccuzzo, M.; Savoini, M.; Dalmasso, P.; Ramieri, G. Long-term outcomes of implants placed after vertical alveolar ridge augmentation in partially edentulous patients: A 10-year prospective clinical study. Clin. Oral Implant. Res. 2017, 28, 1204–1210. [Google Scholar] [CrossRef]
- Vishnu, V.A.; Sanyal, P.K.; Tewary, S.; Nilesh, K.; Prasad, R.M.S.; Pawashe, K. A split-mouth clinico-radiographic comparative study for evaluation of crestal bone and peri-implant soft tissues in immediately loaded implants with and without platelet-rich plasma bioactivation. J. Dent. Res. Dent. Clin. Dent. Prospect. 2019, 13, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Kumar, S.; Singh, R.; Vaibhav, V.; Kedia, N.B.; Singh, A.K. Basal implants-A new era of prosthodontic dentistry. IP Ann. Prosthodont. Restor. Dent. 2020, 6, 1–3. [Google Scholar] [CrossRef]
- Yang, K.R.; Hong, M.H. Improved biocompatibility and osseointegration of nanostructured calcium-incorporated titanium implant surface treatment (XPEED®). Materials 2024, 17, 2707. [Google Scholar] [CrossRef]
- Makary, C.; Menhall, A.; Lahoud, P.; Yang, K.R.; Park, K.B.; Razukevicius, D.; Traini, T. Bone-to-implant contact in implants with plasma-treated nanostructured calcium-incorporated surface (XPEEDActive) compared to non-plasma-treated implants (XPEED): A human histologic study at 4 weeks. Materials 2024, 17, 2331. [Google Scholar] [CrossRef]
- Makary, C.; Menhall, A.; Lahoud, P.; An, H.W.; Park, K.B.; Traini, T. Nanostructured calcium-incorporated surface compared to machined and SLA dental implants—A split-mouth randomized case/double-control histological human study. Nanomaterials 2023, 13, 357. [Google Scholar] [CrossRef]
- Cobo-Vázquez, C.M.; Molinero-Mourelle, P.; Romeo-Rubio, M.; Guisado-Moya, B.F.; Del Río-Highsmith, J.; López-Quiles, J. Prospective clinical-radiological study of the survival and behavior of short implants. J. Prosthet. Dent. 2025, 133, 796–804. [Google Scholar] [CrossRef]
- Esposito, M.; Barausse, C.; Pistilli, R.; Checchi, V.; Diazzi, M.; Gatto, M.R.; Felice, P. Posterior jaws rehabilitated with partial prostheses supported by 4.0 × 4.0 mm or by longer implants: Four-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 221–230. [Google Scholar] [PubMed]
- Priest, G.F. The esthetic challenge of adjacent implants. J. Oral Maxillofac. Surg. 2007, 65, 2–12. [Google Scholar] [CrossRef]
- Sanz-Sánchez, I.; Sanz-Martín, I.; Ortiz-Vigón, A.; Molina, A.; Sanz, M. Complications in bone-grafting procedures: Classification and management. Periodontology 2000 2022, 88, 86–102. [Google Scholar] [CrossRef]
- Buser, D.; Ingimarsson, S.; Dula, K.; Lussi, A.; Hirt, H.P.; Belser, U.C. Long-term stability of osseointegrated implants in augmented bone: A 5-year prospective study in partially edentulous patients. Int. J. Periodontics Restor. Dent. 2002, 22, 109–117. [Google Scholar] [PubMed]
- Simion, M.; Fontana, F.; Rasperini, G.; Maiorana, C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin. Oral Implant. Res. 2007, 18, 620–629. [Google Scholar] [CrossRef] [PubMed]
- Gosai, H.; Anchlia, S.; Patel, K.; Bhatt, U.; Chaudhari, P.; Garg, N. Versatility of basal cortical screw implants with immediate functional loading. Journal of Maxillofacial and Oral Surgery. J. Maxillofac. Oral Surg. 2022, 21, 824–832. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10 (Suppl. 2), S96–S101. [Google Scholar] [CrossRef]
- Roy, A.K.; Dixit, N.; Punde, P.; Sinha, K.T.; Jalaluddin, M.; Kumar, A. Stress distribution in cortical bone around the basal implant—A finite element analysis. J. Pharm. Bioallied. Sci. 2021, 13 (Suppl. 1), S633–S636. [Google Scholar] [CrossRef]
- Ali, S.M.; Othman, K.S.; Samad, A.A.; Mahmud, P.K. Comparison between basal and conventional implants as a treatment modality in atrophied ridges. J. Dent. Implant. Res. 2019, 38, 48–54. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone quality and quantity and dental implant failure: A systematic re-view and meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Beri, A.; Pisulkar, S.G.; Bansod, A.; Shrivastava, A.; Jain, R.; Deshmukh, S. Rapid smile restoration: Basal implants for the edentulous mandible with immediate loading. Cureus 2024, 16, e62655. [Google Scholar] [CrossRef]













Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, K.-B.; An, H.-W.; Park, K.-O.; Hong, M.-H. The Clinical Application of the ARi® Implant System in Severely Resorbed Anterior Alveolar Ridges: A Case Report. Dent. J. 2025, 13, 241. https://doi.org/10.3390/dj13060241
Park K-B, An H-W, Park K-O, Hong M-H. The Clinical Application of the ARi® Implant System in Severely Resorbed Anterior Alveolar Ridges: A Case Report. Dentistry Journal. 2025; 13(6):241. https://doi.org/10.3390/dj13060241
Chicago/Turabian StylePark, Kwang-Bum, Hyun-Wook An, Keun-Oh Park, and Min-Ho Hong. 2025. "The Clinical Application of the ARi® Implant System in Severely Resorbed Anterior Alveolar Ridges: A Case Report" Dentistry Journal 13, no. 6: 241. https://doi.org/10.3390/dj13060241
APA StylePark, K.-B., An, H.-W., Park, K.-O., & Hong, M.-H. (2025). The Clinical Application of the ARi® Implant System in Severely Resorbed Anterior Alveolar Ridges: A Case Report. Dentistry Journal, 13(6), 241. https://doi.org/10.3390/dj13060241





