Three-Dimensional Surgical Guides in Orthodontics: The Present and the Future
Abstract
1. Introduction
2. Surgical Guides-Characteristics
2.1. History
2.2. Classification of Surgical Guides
- 1.
- Type of Mini-Implant: Guides can be tailored for specific types of mini-implants, such as threaded or plate-type implants.
- 2.
- Design Configuration: They can vary in design, including full-arch guides, segmental guides, or individualized guides that consider patient-specific anatomy.
- 3.
- Guiding Mechanism: Some guides use specific drilling protocols to ensure accurate placement, which can include stop mechanisms to control depth.
- 4.
2.2.1. Manufacturing
- 1.
- CAD/CAM Technology: Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) allow for precise design and production of guides based on digital models. Subcategories of the CAD/CAM techniques include:
- 2.
2.2.2. Materials
- 1.
- Photopolymer Resins: These are often used in stereolithography (SLA) 3D printing, providing high precision and detail.
- 2.
- Thermoplastic Polyurethane (TPU): Known for its flexibility and durability, TPU is suitable for guides that may require some adaptability during the surgical procedure.
- 3.
- Acrylic Resins: These materials are frequently used in various 3D printing methods and provide good mechanical properties along with biocompatibility.
- 4.
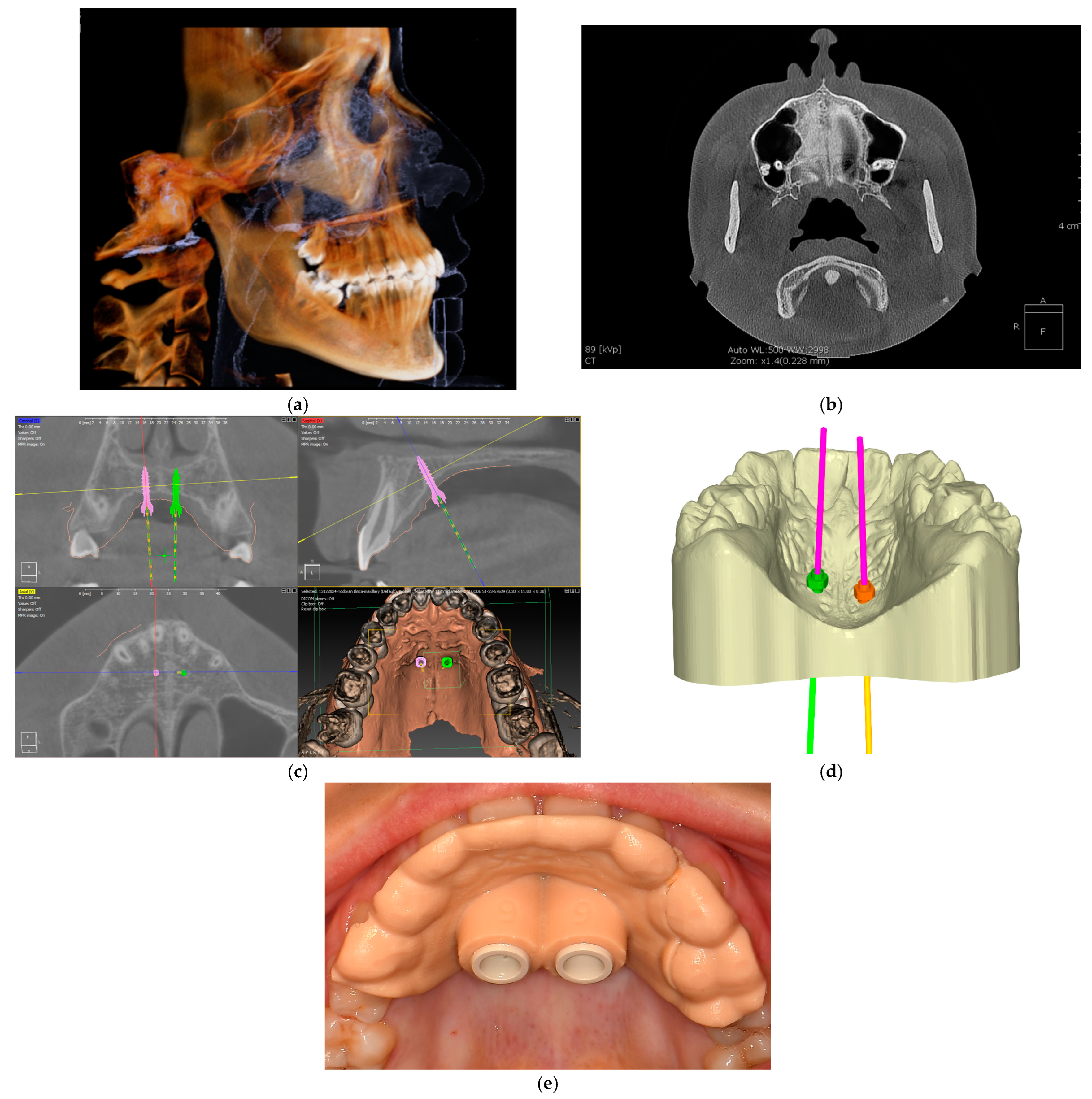
2.3. Steps in Guide Fabrication
- 1.
- Patient Assessment and Imaging: Obtain detailed imaging data, usually through cone beam computed tomography (CBCT) and digital scans, to assess the patient’s anatomy and treatment needs.
- 2.
- Digital Model Creation: Using specialized software, create a 3D digital model of the patient’s dental structures based on imaging data.
- 3.
- Guide Design: Design the surgical guide in CAD software, ensuring it accommodates the specific surgical protocol and the type of mini-implants to be used. This design will include features for accurate drill alignment and depth control.
- 4.
- 3D Printing: Print the surgical guide using suitable 3D printing technology, such as SLA or FDM, ensuring that the material used is biocompatible and suitable for surgical applications.
- 5.
- Post-Processing: After printing, the guide may require cleaning, curing (if applicable), and sterilization to ensure it is safe for clinical use.
- 6.
- Clinical Verification: Prior to the surgical procedure, the guide should be verified in the patient’s mouth to ensure proper fit and alignment [19].
2.4. Advantages and Disadvantages of the Surgical Guides
2.4.1. Advantages
2.4.2. Disadvantages
2.5. Mechanical Properties of Surgical Guides
- 1.
- Strength and Durability.
- 2.
- Rigidity and Flexibility.
- 3.
- Precision and Fit.
- 4.
- Stability.
2.6. Biocompatibility and Sterilization
2.7. Clinical Considerations
2.8. Future of the Surgical Guides
- 1.
- AI and Machine Learning Integration: Recent developments have seen the integration of artificial intelligence and machine learning algorithms in the design and planning phase of surgical guides. These technologies help in predicting optimal outcomes and refining treatment plans based on large datasets of previous cases, thus enhancing the customization and accuracy of guides [57].
- 2.
- Advanced 3D Printing Materials: Innovations in 3D printing materials have led to the development of more durable and biocompatible options. Materials such as resin composites and advanced polymers are being used to create guides that are not only strong and accurate but also safe for prolonged use in the oral environment [58].
- 3.
- Augmented Reality (AR) Applications: Augmented reality is being explored as a tool to enhance the planning and execution of orthodontic procedures. By overlaying digital information on the real-world view, AR can assist orthodontists in visualizing guide placement and ensuring precise alignment during surgery [57].
- 4.
- Cloud-Based Digital Workflows: The adoption of cloud-based platforms allows for seamless collaboration between orthodontists, dental technicians, and patients. These systems enable real-time sharing of digital models and treatment plans, facilitating more efficient and coordinated care [56].
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cousley, R.R. Introducing 3D printing in your orthodontic practice. J. Orthod. 2020, 47, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.M. 3D Imaging Advancements and New Technologies in Clinical and Scientific Dental and Orthodontic Fields. J. Clin. Med. 2022, 11, 2200. [Google Scholar] [CrossRef] [PubMed]
- Graber, T.M.; Vanarsdall, R.L. Orthodontics-Current Principles and Techniques; Mosby, Inc.: Maryland Heights, MO, USA, 2000; pp. 1005–1010. [Google Scholar]
- Chung, K.R.; Kim, S.H.; Kook, Y.A. C-orthodontic microimplant as a unique skeletal anchorage. J. Clin. Orthod. 2004, 38, 478–486. [Google Scholar]
- Chen, L.; Liang, X.; Shen, C.; Jiang, S.; Wang, J. Synthetic CT generation from CBCT images via deep learning. Med. Phys. 2020, 47, 1115–1125. [Google Scholar] [CrossRef]
- Martinez, A.C.; Schiaffino, E.M.; Aranzola, A.P.; Fernandez, C.A.; Seol, M.L.; Sherrard, C.G.; Jones, J.; Huddleston, W.H.; Dornbusch, D.A.; Sreenivasan, S.T.; et al. Multiprocess 3D printing of sodium-ion batteries via vat photopolymerization and direct ink writing. J. Phys. Energy 2023, 5, 045010. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, S.M.; Park, J.H.; Yang, S.; Kim, J.W. Effectiveness of individualized 3D titanium-printed Orthognathic osteotomy guides and custom plates. BMC Oral Health 2023, 23, 255. [Google Scholar] [CrossRef]
- Morea, C.; Dominguez, G.C.; Wuo, A.V.; Tortamano, A. Surgical guide for optimal positioning of mini-implants. J. Clin. Orthod. 2005, 39, 317–321. [Google Scholar] [PubMed]
- Kim, S.H.; Choi, Y.S.; Hwang, E.H.; Chung, K.R.; Kook, Y.A.; Nelson, G. Surgical positioning of orthodontic mini-implants with guides fabricated on models replicated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S82–S89. [Google Scholar] [CrossRef] [PubMed]
- Fortin, T.; Isidori, M.; Blanchet, E.; Perriat, M.; Bouchet, H.; Coudert, J.L.J.L. An image-guided system-drilled surgical template and trephine guide pin to make treatment of completely edentulous patients easier: A clinical report on immediate loading. Clin. Implant Dent. Relat. Res. 2004, 6, 111–119. [Google Scholar] [CrossRef]
- Sießegger, M.; Schneider, B.T.; Mischkowski, R.A.; Lazar, F.; Krug, B.; Klesper, B.; Zöller, J.E. Use of an image-guided navigation system in dental implant surgery in anatomically complex operation sites. J. Craniomaxillofac. Surg. 2001, 29, 276–281. [Google Scholar] [CrossRef]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.; Huang, G.J. Orthodontics: Current Principles and Techniques, 5th ed.Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- McNamara, J.A.; Lione, R.; Franchi, L.; Angelieri, F.; Cevidanes, L.H.; Darendeliler, M.A.; Cozza, P. The role of rapid maxillary expansion in the promotion of oral and general health. Prog. Orthod. 2015, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Zhang, J.; He, J.; Li, Y.; Li, C.; Lin, Z.; Wu, H.; Zhou, L. The application of 3D printing in dentistry: A bibliometric analysis from 2012 to 2023. J. Prosthet. Dent. 2024, in press. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. BioMed Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef] [PubMed]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef] [PubMed]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent develompents for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Gallo, S.; Pascadopoli, M.; Canzi, P.; Marconi, S.; Montasser, M.A.; Bressani, D.; Gandini, P.; Sfondrini, M.F. Properties of CAD/CAM 3D Printing Dental Materials and Their Clinical Applications in Orthodontics: Where Are We Now? Appl. Sci. 2022, 12, 551. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Almeh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthod. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Fleming, P.S.; Marinho, V.; Johal, A. Orthodontic measurements on digital study models compared with plaster models: A systematic review. Orthod. Craniofac. Res. 2011, 14, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Al Mortadi, N.; Eggbeer, D.; Lewis, J.; Williams, R.J. CAD/CAM/AM applications in the manufacture of dental appliances. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Vidakis, N.; Petousis, M.; Maniadi, A.; Koudoumas, E.; Kenanakis, G.; Romanitan, C.; Tutunaru, O.; Suchea, M.; Kechagias, J. The Mechanical and Physical Properties of 3D-Printed Materials Composed of ABS-ZnO Nanocomposites and ABS-ZnO Microcomposites. Micromachines 2020, 11, 615. [Google Scholar] [CrossRef] [PubMed]
- Skorski, M.; Esenther, J.; Ahmed, Z.; Miller, A.; Hartings, M. The chemical, mechanical, and physical properties of 3D printed materials composed of TiO2 -ABS nanocomposites. Sci. Technol. Adv. Mater. 2016, 17, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Pop, S.I.; Dudescu, M.; Mihali, S.G.; Păcurar, M.; Bratu, D.C. Effects of disinfection and steam sterilization on the mechanical properties of 3D SLA-and DLP-printed surgical guides for orthodontic implant placement. Polymers 2022, 14, 2107. [Google Scholar] [CrossRef] [PubMed]
- Liaw, C.Y.; Guvendiren, M. Current and emerging applications of 3D printing in medicine. Biofabrication 2017, 9, 024102. [Google Scholar] [CrossRef]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [PubMed]
- Alhnan, M.A.; Okwuosa, T.C.; Sadia, M.; Wan, K.W.; Ahmed, W.; Arafat, B. Emergence of 3D Printed Dosage Forms: Opportunities and Challenges. Pharm. Res. 2016, 33, 1817–1832. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Tappa, K.; Jammalamadaka, U. Novel biomaterials used in medical 3D printing techniques. J. Funct. Biomater. 2018, 9, 17. [Google Scholar] [CrossRef]
- Chia, H.N.; Wu, B.M. Recent advances in 3D printing of biomaterials. J. Biol. Eng. 2015, 9, 4. [Google Scholar] [CrossRef]
- Liu, Q.; Leu, M.C.; Schmitt, S.M. Rapid prototyping in dentistry: Technology and application. Int. J. Adv. Manuf. Technol. 2005, 29, 317–335. [Google Scholar] [CrossRef]
- ASTM D638-14; Standard Test Method for Tensile Properties of Plastics. ASTM International: West Conshohocken, PA, USA, 2014. [CrossRef]
- ASTM D790-03; Standard Test Methods for Flexural Properties of Unreinforced and Reinforced Plastics and Electrical Insulating Materials. ASTM International: West Conshohocken, PA, USA, 2003. [CrossRef]
- Quintana, R.; Choi, J.-W.; Puebla, K.; Wicker, R. Effects of build orientation on tensile strength for stereolithography-manufactured ASTM D-638 type I specimens. Int. J. Adv. Manuf. Technol. 2010, 46, 201–215. [Google Scholar] [CrossRef]
- Kazemi, M.; Rahimi, A.R. Supports effect on tensile strength of the stereolithography parts. Rapid Prototyp. J. 2015, 21, 79–88. [Google Scholar] [CrossRef]
- Arefin, A.M.E.; Khatri, N.R.; Kulkarni, N.; Egan, P.F. Polymer 3D Printing Review: Materials, Process, and Design Strategies for Medical Applications. Polymers 2021, 13, 1499. [Google Scholar] [CrossRef]
- Taormina, G.; Sciancalepore, C.; Bondioli, F.; Messori, M. Special resins for stereolithography: In situ generation of silver nanoparticles. Polymers 2018, 10, 212. [Google Scholar] [CrossRef]
- Pohlmann, A.R.; Fonseca, F.N.; Paese, K.; Detoni, C.B.; Coradini, K.; Beck, R.C.; Guterres, S.S. Poly(-caprolactone) microcapsule and nanocapsules in drug delivery. Expert Opin. Drug Deliv. 2013, 10, 623–638. [Google Scholar] [CrossRef] [PubMed]
- Tofail, S.A.M.; Koumoulos, E.P.; Bandyopadhyay, A.; Bose, S.; O’Donoghue, L.; Charitidis, C. Additive manufacturing: Scientific and technological challenges, market uptake and opportunities. Mater. Today 2018, 21, 22–37. [Google Scholar] [CrossRef]
- Miedzińska, D.; Gieleta, R.; Popławski, A. Experimental Study on Influence of Curing Time on Strength Behavior of SLA-Printed Samples Loaded with Different Strain Rates. Materials 2020, 13, 5825. [Google Scholar] [CrossRef]
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Mangano, F.G.; Hauschild, U.; Admakin, O. Full in-office guided surgery with open selective tooth-supported templates: A prospective clinical study on 20 patients. Int. J. Environ. Res. Public Health 2018, 15, 2361. [Google Scholar] [CrossRef] [PubMed]
- Al-Harbi, S.A.; Sun, A.Y. Implant placement accuracy when using stereolithographic template as a surgical guide: Preliminary results. Implant. Dent. 2009, 18, 46–56. [Google Scholar] [CrossRef]
- Burbano, F.M.; Pasick, C.; Torina, P.J.; Harmaty, M.; Taub, P.J. Away rotations in plastic and reconstructive surgery: A survey of program directors. Plast. Reconstr. Surg. 2020, 145, 235e–236e. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Wang, J.; Ma, C.; Shen, J.; Dong, X.; Lin, D. A systematic review of the accuracy of digital surgical guides for dental implantation. Int. J. Implant Dent. 2023, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Guttridge, C.; Shannon, A.; O’Sullivan, A.; O’Sullivan, K.J.; O’Sullivan, L.W. Biocompatible 3D printing resins for medical applications: A review of marketed intended use, biocompatibility certification, and post-processing guidance. Ann. 3D Print. Med. 2022, 5, 100044. [Google Scholar] [CrossRef]
- ISO 11139:2018; Sterilization of Health Care Products—Vocabulary of Terms Used in Sterilization and Related Equipment and Process Standards. The International Organisation for Standardization: Geneva, Switzerland, 2018. Available online: https://www.iso.org/standard/66262.html (accessed on 1 February 2022).
- ISO 17664:2017; Processing of Health Care Products—Information to Be Provided by the Medical Device Manufacturer for the Processing of Medical Devices. The International Organisation for Standardization: Geneva, Switzerland, 2017. Available online: https://www.iso.org/standard/62952.html (accessed on 1 February 2022).
- The Official Journal of European Union: The European Medical Device Regulations L117. 2017. Available online: https://eurlex.europa.eu/legal-content/EN/TXT/PDF/?uri=OJ:L:2017:117:FULL&from=EN (accessed on 1 February 2022).
- Rutala, W.A.; Gergen, M.F.; Weber, D.J. Comparative evaluation of the sporicidal activity of new low-temperature sterilization technologies: Ethylene oxide, 2 plasma sterilization systems, and liquid peracetic acid. Am. J. Infect. Control. 1998, 26, 393–398. [Google Scholar] [CrossRef]
- Smith, P.N.; Palenik, C.J.; Blanchard, S.B. Microbial contamination and the sterilization/disinfection of surgical guides used in the placement of endosteal implant. Int. J. Oral Maxillofac. Implants 2011, 26, 274–281. [Google Scholar] [PubMed]
- Marquez Bautista, N.; Meniz-García, C.; López-Carriches, C.; Sánchez-Labrador, L.; Cortés-Bretón Brinkmann, J.; Madrigal Martínez-Pereda, C. Accuracy of Different Systems of Guided Implant Surgery and Methods for Quantification: A Systematic Review. Appl. Sci. 2024, 14, 11479. [Google Scholar] [CrossRef]
- Zhao, D.; Xie, W.; Li, T.; Wang, A.; Wu, L.; Kang, W.; Wang, L.; Guo, S.; Tang, X.; Xie, S. New-designed 3D printed surgical guide promotes the accuracy of endodontic microsurgery: A study of 14 upper anterior teeth. Sci. Rep. 2023, 13, 15512. [Google Scholar] [CrossRef] [PubMed]
- Török, G.; Gombocz, P.; Bognár, E.; Nagy, P.; Dinya, E.; Kispélyi, B.; Hermann, P. Effects of disinfection and sterilization on the dimensional changes and mechanical properties of 3D printed surgical guides for implant therapy—Pilot study. BMC Oral Health 2020, 20, 19. [Google Scholar] [CrossRef]
- Guni, A.; Varma, P.; Zhang, J.; Fehervari, M.; Ashrafian, H. Artificial intelligence in surgery: The future is now. Eur. Surg. Res. 2024, 65, 22–39. [Google Scholar] [CrossRef]
- Mangano, F.G.; Yang, K.R.; Lerner, H.; Admakin, O.; Mangano, C. Artificial intelligence and mixed reality for dental implant planning: A technical note. Clin. Implant Dent. Relat. Res. 2024, 26, 942–953. [Google Scholar] [CrossRef]
- Elgarba, B.M.; Fontenele, R.C.; Tarce, M.; Jacobs, R. Artificial intelligence serving pre-surgical digital implant planning: A scoping review. J. Dent. 2024, 143, 104862. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Oh, J.H.; Kim, S.G. Virtual surgical plan with custom surgical guide for orthognathic surgery: Systematic review and meta-analysis. Maxillofac. Plast. Reconstr. Surg. 2024, 46, 39. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Kim, S.G. Redefining precision and efficiency in orthognathic surgery through virtual surgical planning and 3D printing: A narrative review. Maxillofac. Plast. Reconstr. Surg. 2023, 45, 42. [Google Scholar] [CrossRef]
- Altalhi, A.M.; Alharbi, F.S.; Alhodaithy, M.A.; Almarshedy, B.S.; Al-Saaib, M.Y.; Al Jfshar, R.M.; Aljohani, A.S.; Alshareef, A.H.; Muhayya, M.; Al-Harbi, N.H. The Impact of Artificial Intelligence on Dental Implantology: A Narrative Review. Cureus 2023, 15, e47941. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Macrì, M.; D’Albis, V.; D’Albis, G.; Forte, M.; Capodiferro, S.; Favia, G.; Alrashadah, A.O.; García, V.D.-F.; Festa, F. The Role and Applications of Artificial Intelligence in Dental Implant Planning: A Systematic Review. Bioengineering 2024, 11, 778. [Google Scholar] [CrossRef] [PubMed]
- Satapathy, S.K.; Kunam, A.; Rashme, R.; Sudarsanam, P.P.; Gupta, A.; Kumar, H.S.K. AI-Assisted Treatment Planning for Dental Implant Placement: Clinical vs AI-Generated Plans. J. Pharm. Bioallied. Sci. 2024, 16, S939–S941. [Google Scholar] [CrossRef] [PubMed]
- Balhaddad, A.A.; Garcia, I.M.; Mokeem, L.; Alsahafi, R.; Majeed-Saidan, A.; Albagami, H.H.; Khan, A.S.; Ahmad, S.; Collares, F.M.; Della Bona, A.; et al. Three-dimensional (3D) printing in dental practice: Applications, areas of interest, and level of evidence. Clin. Oral Investig. 2023, 27, 2465–2481. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pop, S.I.; Bud, E.; Jánosi, K.M.; Bud, A.; Kerekes-Máthé, B. Three-Dimensional Surgical Guides in Orthodontics: The Present and the Future. Dent. J. 2025, 13, 74. https://doi.org/10.3390/dj13020074
Pop SI, Bud E, Jánosi KM, Bud A, Kerekes-Máthé B. Three-Dimensional Surgical Guides in Orthodontics: The Present and the Future. Dentistry Journal. 2025; 13(2):74. https://doi.org/10.3390/dj13020074
Chicago/Turabian StylePop, Silvia Izabella, Eugen Bud, Kinga Mária Jánosi, Anamaria Bud, and Bernadette Kerekes-Máthé. 2025. "Three-Dimensional Surgical Guides in Orthodontics: The Present and the Future" Dentistry Journal 13, no. 2: 74. https://doi.org/10.3390/dj13020074
APA StylePop, S. I., Bud, E., Jánosi, K. M., Bud, A., & Kerekes-Máthé, B. (2025). Three-Dimensional Surgical Guides in Orthodontics: The Present and the Future. Dentistry Journal, 13(2), 74. https://doi.org/10.3390/dj13020074






