Evaluation of the Surface Properties of Three CAD/CAM Ceramics: A Comparative In Vitro Study
Abstract
1. Introduction
- Therefore, this in vitro study aimed to:
- Evaluate and compare the surface morphology of zirconia-reinforced lithium silicate, feldspathic ceramic, and lithium disilicate CAD/CAM materials using scanning electron microscopy (SEM).
- Analyze the surface roughness parameters (Ra, Rq, Rsk) obtained through 3D profilometry.
- Assess surface wettability and free surface energy using contact angle measurements.
- Determine the elemental composition of each material through energy-dispersive X-ray spectroscopy (EDS).
2. Materials and Methods
2.1. Study Design and Setting
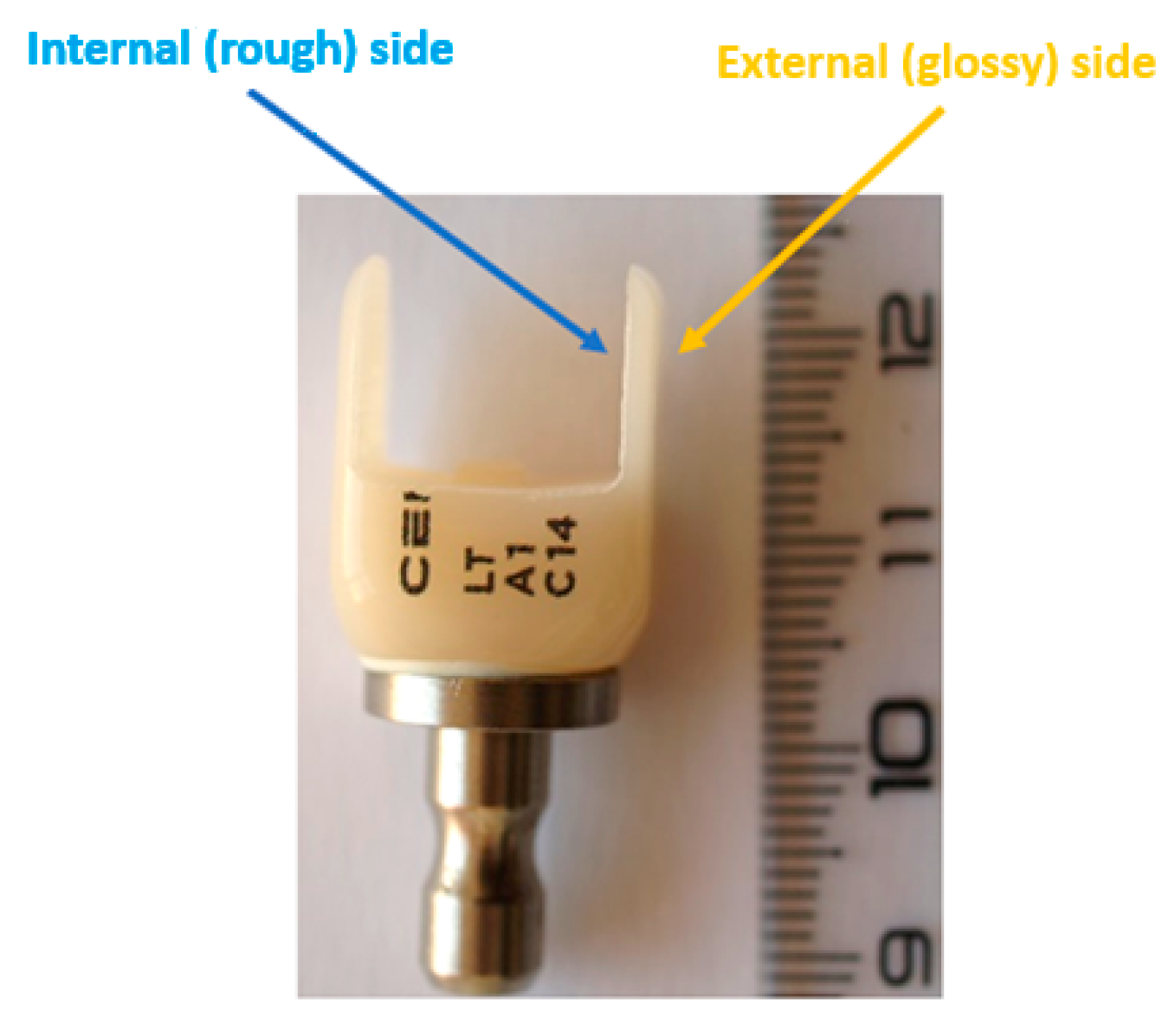
2.2. CAD/CAM Processing of the Ceramic Materials
2.3. Computed Tomography (CT) Analysis
2.4. Scanning Electron Microscopy (SEM) and Energy-Dispersive X-Ray Spectroscopy (EDS)
2.5. Surface Roughness Analysis
- Ra—arithmetic mean roughness;
- Rq—root mean square roughness;
- Rt—total height of the roughness profile.
2.6. Wettability Measurements
2.7. Investigators
2.8. Statistical Analysis
3. Results
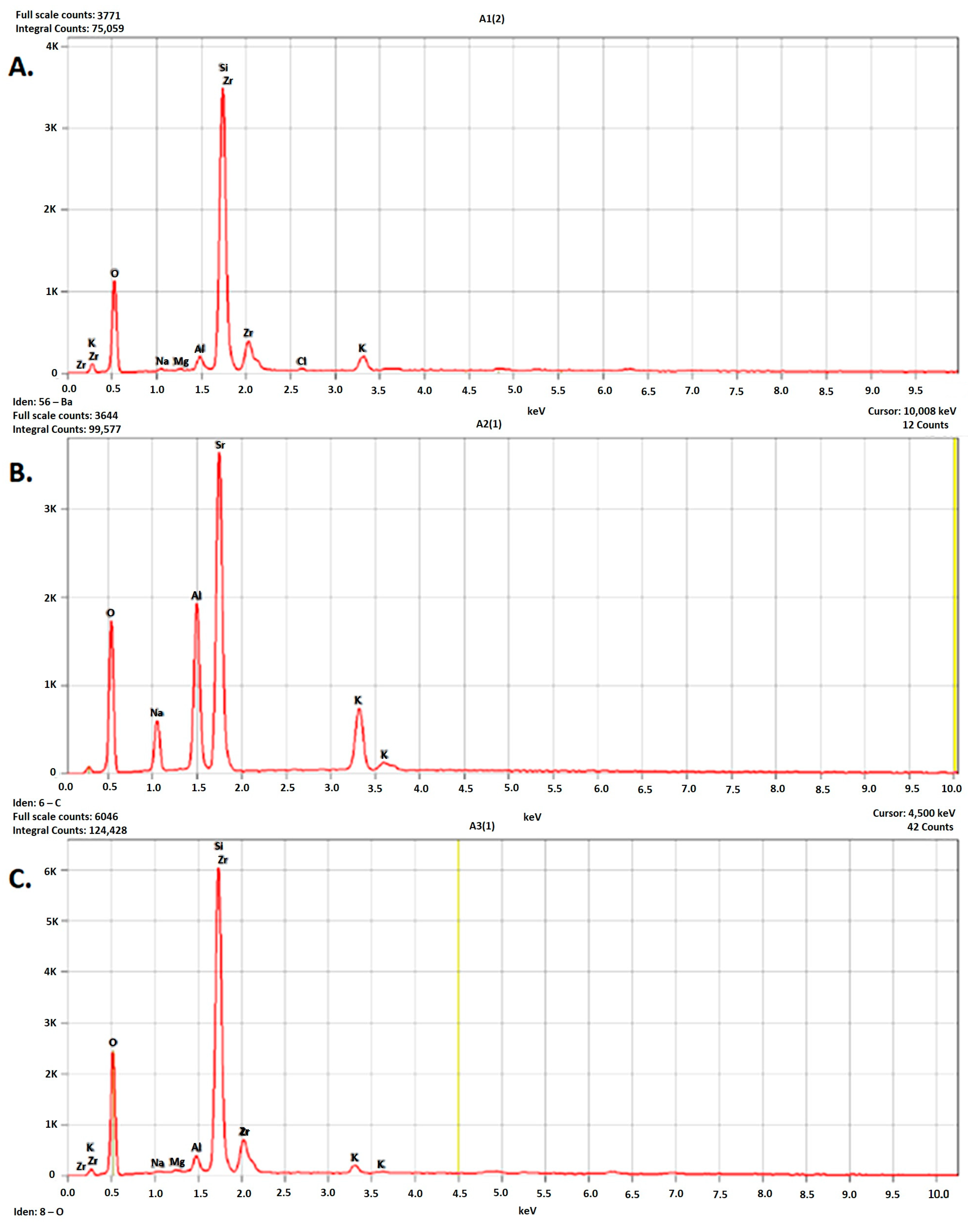
3.1. EDS
3.2. CT
3.3. SEM
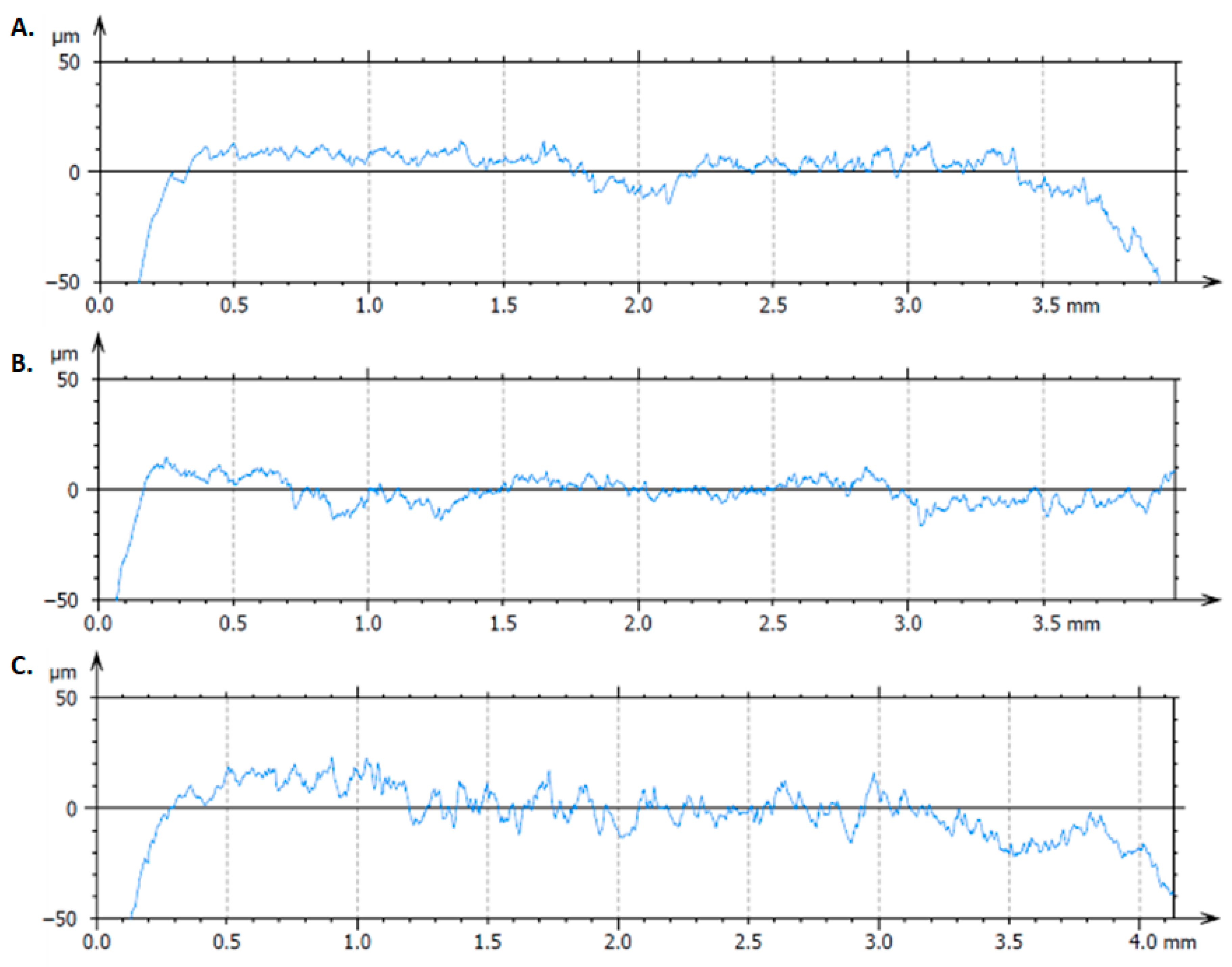
3.4. Surface Roughness
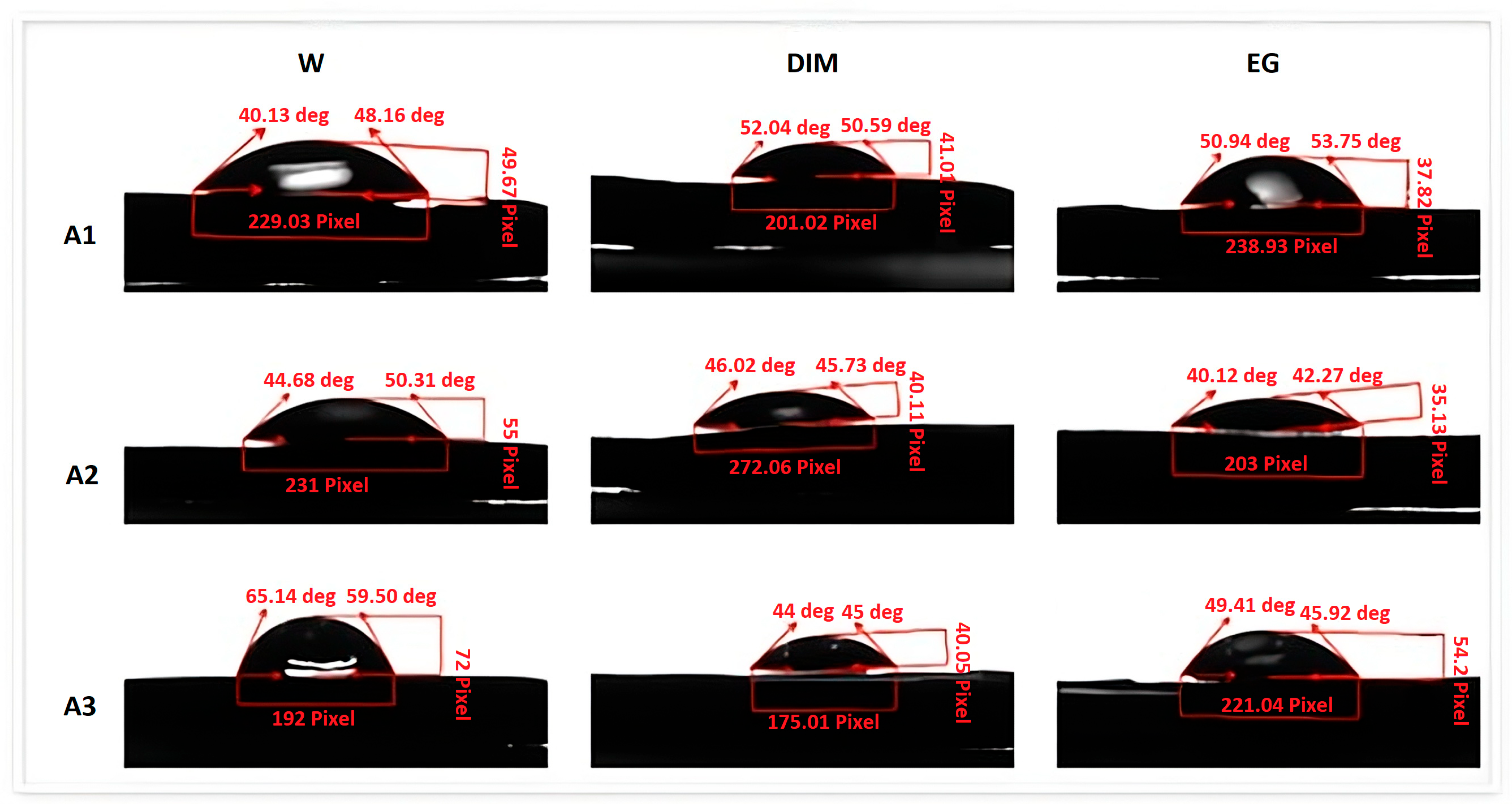
3.5. Contact Angle
3.6. Overall Inference
4. Discussion
4.1. General Findings
4.2. Surface Morphology and Roughness
4.3. Wettability and Surface Free Energy
4.4. Elemental Composition
4.5. Comparative Assessment and Clinical Significance
4.6. Clinical Implications
4.7. Strengths, Limitations, and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Georgeanu, V.A.; Gingu, O.; Antoniac, I.V.; Manolea, H.O. Current Options and Future Perspectives on Bone Graft and Biomaterials Substitutes for Bone Repair, from Clinical Needs to Advanced Biomaterials Research. Appl. Sci. 2023, 13, 8471. [Google Scholar] [CrossRef]
- Maiti, N.; Mahapatra, N.; Patel, D.; Chanchad, J.; Saurabhbhai Shah, A.; Mahboob Rahaman, S.K.; Surana, P. Application of CAD-CAM in Dentistry. Bioinformation 2024, 20, 547–550. [Google Scholar] [CrossRef]
- Marian, D.; Toro, G.; D’Amico, G.; Trotta, M.C.; D’Amico, M.; Petre, A.; Lile, I.; Hermenean, A.; Fratila, A. Challenges and Innovations in Alveolar Bone Regeneration: A Narrative Review on Materials, Techniques, Clinical Outcomes, and Future Directions. Medicina 2025, 61, 20. [Google Scholar] [CrossRef]
- Antoniac, I.; Valeanu, N.; Niculescu, M.; Antoniac, A.; Robu, A.; Popescu, L.; Manescu Paltanea, V.; Anusca, D.; Enachescu, C.I. Outcomes of Birmingham Hip Resurfacing Based on Clinical Aspects and Retrieval Analysis of Failed Prosthesis. Materials 2024, 17, 3965. [Google Scholar] [CrossRef]
- Ahmed, K.E. We’re Going Digital: The Current State of CAD/CAM Dentistry in Prosthodontics. Prim. Dent. J. 2018, 7, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Susic, I.; Travar, M.; Susic, M. The application of CAD/CAM technology in Dentistry. IOP Conf. Ser. Mater. Sci. Eng. 2017, 200, 012020. [Google Scholar] [CrossRef]
- Gunal, B.; Ulusoy, M.M. Optical Properties of Contemporary Monolithic CAD-CAM Restorative Materials at Different Thicknesses. J. Esthet. Restor. Dent. 2018, 30, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Fratila, A.E.; Elisei, A.M.; Constantin, I.; Stanciu, P.R.; Stanciu, D.; Iliescu, A.A.; Forna, N.C.; Grigorescu, C.C. The Efficiency of Custom Dental Implants in Managing Oral Complications of Crohn’s Disease. Rom. J. Oral Rehabil. 2024, 16, 567–578. [Google Scholar] [CrossRef]
- Aziz, A.; El-Mowafy, O. Six-Year Clinical Performance of Lithium Disilicate Glass-Ceramic CAD-CAM Versus Metal-Ceramic Crowns. J. Adv. Prosthodont. 2023, 15, 44–54. [Google Scholar] [CrossRef]
- Meirelles, L. Ceramic CAD/CAM Materials: An Overview of Clinical Uses and Considerations. ADA Prof. Prod. Rev. 2017, 12, 1–9. [Google Scholar]
- Oprea, M.; Pandele, A.M.; Nechifor, A.C.; Nicoara, A.I.; Antoniac, I.V.; Semenescu, A.; Voicu, S.I.; Enachescu, C.I.; Fratila, A.M. Improved Biomineralization Using Cellulose Acetate/Magnetic Nanoparticles Composite Membranes. Polymers 2025, 17, 209. [Google Scholar] [CrossRef] [PubMed]
- Daou, E.E. The Zirconia Ceramic: Strengths and Weaknesses. Open Dent. J. 2014, 8, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Bors, A.; Szekely, M.; Veres Bardocz, Z.; Corneschi, I.; Ciocoiu, R.; Antoniac, A.; Enachescu, C. Characterization of Innovative Dental Resin Reinforced with Zirconia Nanoparticles Obtained by 3D Printing. UPB Sci. Bull. Ser. B 2024, 86, 289–299. [Google Scholar]
- Nascimento, V.A.; Bento, V.A.A.; Cruz, K.H.; Silva, L.S.; Pesqueira, A.A.; Pellizzer, E.P. Color Stability and Surface Roughness of Resin-Ceramics with Different Surface Treatments: A Systematic Review and Meta-Analysis of In Vitro Studies. J. Prosthet. Dent. 2025, 134, 72–84. [Google Scholar] [CrossRef]
- Fu, L.; Engqvist, H.; Xia, W. Glass-Ceramics in Dentistry: A Review. Materials 2020, 13, 1049. [Google Scholar] [CrossRef]
- Kaczmarek, K.; Konieczny, B.; Siarkiewicz, P.; Leniart, A.; Lukomska-Szymanska, M.; Skrzypek, S.; Lapinska, B. Surface Characterization of Current Dental Ceramics Using Scanning Electron Microscopic and Atomic Force Microscopic Techniques. Coatings 2022, 12, 1122. [Google Scholar] [CrossRef]
- Nasrabadi Hassan Nasri, C.S.; Robu, A.; Stere, A.; Antoniac, I.; Valeanu, N.; Ciocoiu, R.; Enachescu, C.I. Comparative Analysis of Surface Properties of Ti6Al4V Femoral Stem Hip Prosthesis and Plate for Long Bone Fractures Used in Orthopedic Surgery. UPB Sci. Bull. Ser. B 2024, 86, 237–246. [Google Scholar]
- Cavalu, S.; Fritea, L.; Brocks, M.; Barbaro, K.; Murvai, G.; Costea, T.O.; Antoniac, I.; Verona, C.; Romani, M.; Latini, A.; et al. Novel Hybrid Composites Based on PVA/SeTiO2 Nanoparticles and Natural Hydroxyapatite for Orthopedic Applications: Correlations between Structural, Morphological and Biocompatibility Properties. Materials 2020, 13, 2077. [Google Scholar] [CrossRef]
- Kowalski, J.; Lapinska, B.; Nissan, J.; Lukomska-Szymanska, M. Factors Influencing Marginal Bone Loss Around Dental Implants: A Narrative Review. Coatings 2021, 11, 865. [Google Scholar] [CrossRef]
- Cavalu, S.; Antoniac, I.; Luminita, F.; Mates, I.; Milea, C.; Vasile, L.; Vicaş, S.; Mohan, A.G. Surface Modifications of the Titanium Mesh for Cranioplasty Using Selenium Nanoparticles Coating. J. Adhes. Sci. Technol. 2018, 32, 2509–2522. [Google Scholar] [CrossRef]
- Ruales-Carrera, E.; Dal Bó, M.; Fernandes das Neves, W.; Fredel, M.C.; Maziero Volpato, C.A.; Hotza, D. Chemical Tempering of Feldspathic Porcelain for Dentistry Applications: A Review. Open Ceram. 2022, 9, 100201. [Google Scholar] [CrossRef]
- Gonçalves, S.E.P.; Bresciani, E. 2—Reconstructions using alloys and ceramics. In Material-Tissue Interfacial Phenomena; Spencer, P., Misra, A., Eds.; Woodhead Publishing: Cambridge, UK, 2017; pp. 23–66. [Google Scholar]
- Streit, G.; Sykes, L. Overview of Lithium Disilicate as a Restorative Material in Dentistry. S. Afr. Dent. J. 2022, 77, 495–499. [Google Scholar] [CrossRef]
- Manziuc, M.; Kui, A.; Chisnoiu, A.; Labuneț, A.; Negucioiu, M.; Ispas, A.; Buduru, S. Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicina 2023, 59, 2135. [Google Scholar] [CrossRef] [PubMed]
- Nejatidanesh, F.; Amjadi, M.; Akouchekian, M.; Savabi, O. Clinical Performance of CEREC AC Bluecam Conservative Ceramic Restorations After Five Years—A Retrospective Study. J. Dent. 2015, 43, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Tatia, C.I.; Iancu, M.M.; Antoniac, A.; Necșulescu, A.; Robu, A.; Vasilescu, M.L.; Corneschi, I.; Fratila, A.M. Comparative Analysis of the Surface Properties of Different Dental Implants. UPB Sci. Bull. Ser. B 2024, 86, 245–256. [Google Scholar]
- Devlukia, S.; Hammond, L.; Malik, K. Is Surface Roughness of Direct Resin Composite Restorations Material and Polisher-Dependent? A Systematic Review. J. Esthet. Restor. Dent. 2023, 35, 947–967. [Google Scholar] [CrossRef]
- Lu, K.; Chen, Z.; Luo, Y.; Huang, P.; He, Q.; Xie, J.; Yin, L. Microgrinding of Lithium Metasilicate/Disilicate Glass-Ceramics. Ceram. Int. 2022, 48, 8548–8562. [Google Scholar] [CrossRef]
- Kreve, S.; Dos Reis, A.C. Effect of Surface Properties of Ceramic Materials on Bacterial Adhesion: A Systematic Review. J. Esthet. Restor. Dent. 2022, 34, 461–472. [Google Scholar] [CrossRef]
- Soares, E.J.; de Lima Oliveira, R.F.; Silame, F.D.J.; Tonani-Torrieri, R.; Franca, R.; Pires-de, F.P. Color Stability, Translucency, and Wettability of a Lithium Disilicate Dental Ceramics Submitted to Different Surface Treatments. Int. J. Prosthodont. Restor. Dent. 2021, 11, 4–8. [Google Scholar] [CrossRef]



| Code | Brand Name | Manufacturer | Composition/Type | LOT No. | Milling Machine | Software | Thermal/Sintering Process |
|---|---|---|---|---|---|---|---|
| A1 | Celtra Duo | Dentsply Sirona, Bensheim, Germany | Zirconia-reinforced lithium silicate glass-ceramic (ZLS) | - | CEREC MC XL (Dentsply Sirona, Bensheim, Germany) | CEREC Software (version 5.2.3, Dentsply Sirona) | Crystallized in the SpeedFire furnace at 840 °C for 10 min |
| A2 | CEREC Blocs | Dentsply Sirona, Bensheim, Germany | Feldspathic glass-ceramic (SiO2-Al2O3-K2O-Na2O) | - | CEREC MC XL (Dentsply Sirona, Bensheim, Germany) | CEREC Software (version 5.2.3, Dentsply Sirona) | No additional firing required |
| A3 | CEREC Tessera | Dentsply Sirona, Bensheim, Germany | Lithium disilicate glass-ceramic reinforced with virgilite crystals | - | CEREC MC XL (Dentsply Sirona, Bensheim, Germany) | CEREC Software (version 5.2.3, Dentsply Sirona) | Fired in the SpeedFire furnace at 760 °C for 4 min |
| Element | Weight % | Weight % Error | Atom % | Atom % Error |
|---|---|---|---|---|
| O | 53.84 | ±0.62 | 71.04 | ±0.81 |
| Na | 0.75 | ±0.07 | 0.69 | ±0.07 |
| Mg | 0.22 | ±0.06 | 0.19 | ±0.05 |
| Al | 1.59 | ±0.10 | 1.24 | ±0.08 |
| Si | 30.54 | ±0.22 | 22.96 | ±0.17 |
| Cl | 0.32 | ±0.04 | 0.19 | ±0.03 |
| K | 2.42 | ±0.06 | 1.31 | ±0.03 |
| Zr | 10.33 | ±1.30 | 2.39 | ±0.30 |
| Total | 100.00 | 100.00 |
| Element | Weight % | Weight % Error | Atom % | Atom % Error |
|---|---|---|---|---|
| O | 48.11 | ±0.45 | 61.68 | ±0.58 |
| Na | 7.30 | ±0.12 | 6.51 | ±0.11 |
| Al | 12.40 | ±0.14 | 9.43 | ±0.10 |
| Si | 26.70 | ±0.20 | 19.50 | ±0.14 |
| K | 5.49 | ±0.10 | 2.88 | ±0.05 |
| Total | 100.00 | 100.00 |
| Element | Weight % | Weight % Error | Atom % | Atom % Error |
|---|---|---|---|---|
| O | 58.52 | ±0.49 | 73.64 | ±0.61 |
| Na | 0.58 | ±0.10 | 0.51 | ±0.09 |
| Mg | 0.36 | ±0.05 | 0.30 | ±0.04 |
| Al | 1.73 | ±0.08 | 1.29 | ±0.06 |
| Si | 30.91 | ±0.19 | 22.16 | ±0.13 |
| K | 1.22 | ±0.04 | 0.63 | ±0.02 |
| Zr | 6.66 | ±0.80 | 1.47 | ±0.18 |
| Total | 100.00 | 100.00 |
| Set | Zona | Ra [µm] | Rq [µm] | Rsk | ΔRa % vs. Sample | ΔRq % vs. Sample | p-Value |
|---|---|---|---|---|---|---|---|
| A1 | Sample | 1.9715 | 2.7405 | −1.1601 | |||
| A1 | Internal side | 1.8038 | 2.2854 | −0.1891 | −8.51% | −16.61% | ns |
| A1 | External side | 0.2013 | 0.8079 | −11.9274 | −89.79% | −70.52% | p < 0.05 |
| A2 | Sample | 1.9148 | 2.8214 | −2.2669 | |||
| A2 | Internal side | 1.7077 | 2.1848 | −0.2938 | −10.82% | −22.56% | ns |
| A2 | External side | 0.4326 | 0.6799 | −1.8274 | −77.41% | −75.90% | p < 0.05 |
| A3 | Sample | 2.8647 | 4.3593 | −2.8007 | |||
| A3 | Internal side | 1.8304 | 2.3576 | −0.0663 | −36.11% | −45.92% | ns |
| A3 | External side | 0.0766 | 0.1940 | −10.4699 | −97.33% | −95.55% | p < 0.05 |
| Sample | Side | W (°) Mean ± SD | DIM (°) Mean ± SD | EG (°) Mean ± SD | γs^d (mN/m) | γs^p (mN/m) | γs (mN/m) |
|---|---|---|---|---|---|---|---|
| A1 | External side | 43.29 ± 7.08 | 50.23 ± 8.03 | 50.23 ± 5.44 | 34.1 | 24.9 | 59.0 |
| A2 | External side | 46.30 ± 4.82 | 45.14 ± 4.84 | 42.31 ± 7.17 | 36.9 | 21.6 | 58.5 |
| A3 | External side | 64.74 ± 4.19 | 45.35 ± 2.59 | 45.65 ± 4.91 | 36.8 | 10.9 | 47.7 |
| A1 | Internal side | 42.49 ± 4.97 | 35.68 ± 5.74 | 39.10 ± 10.52 | 41.7 | 21.5 | 63.2 |
| A2 | Internal side | 38.31 ± 4.37 | 37.06 ± 3.46 | 23.75 ± 7.98 | 41.1 | 24.1 | 65.1 |
| A3 | Internal side | 31.41 ± 4.48 | 37.49 ± 3.21 | 23.25 ± 3.22 | 40.8 | 27.8 | 68.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boanca, C.; Earar, K.; Focsaneanu, S.C.; Cocoș, D.I.; Budacu, C.C. Evaluation of the Surface Properties of Three CAD/CAM Ceramics: A Comparative In Vitro Study. Dent. J. 2025, 13, 550. https://doi.org/10.3390/dj13120550
Boanca C, Earar K, Focsaneanu SC, Cocoș DI, Budacu CC. Evaluation of the Surface Properties of Three CAD/CAM Ceramics: A Comparative In Vitro Study. Dentistry Journal. 2025; 13(12):550. https://doi.org/10.3390/dj13120550
Chicago/Turabian StyleBoanca, Cristian, Kamel Earar, Sergiu Ciprian Focsaneanu, Dorin Ioan Cocoș, and Cristian Constantin Budacu. 2025. "Evaluation of the Surface Properties of Three CAD/CAM Ceramics: A Comparative In Vitro Study" Dentistry Journal 13, no. 12: 550. https://doi.org/10.3390/dj13120550
APA StyleBoanca, C., Earar, K., Focsaneanu, S. C., Cocoș, D. I., & Budacu, C. C. (2025). Evaluation of the Surface Properties of Three CAD/CAM Ceramics: A Comparative In Vitro Study. Dentistry Journal, 13(12), 550. https://doi.org/10.3390/dj13120550






