Assessment of Anxiety and Local Anesthesia Experiences in Dental Students Using the Modified Dental Anxiety Scale (MDAS)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Acquisition
2.3. Statistical Analysis
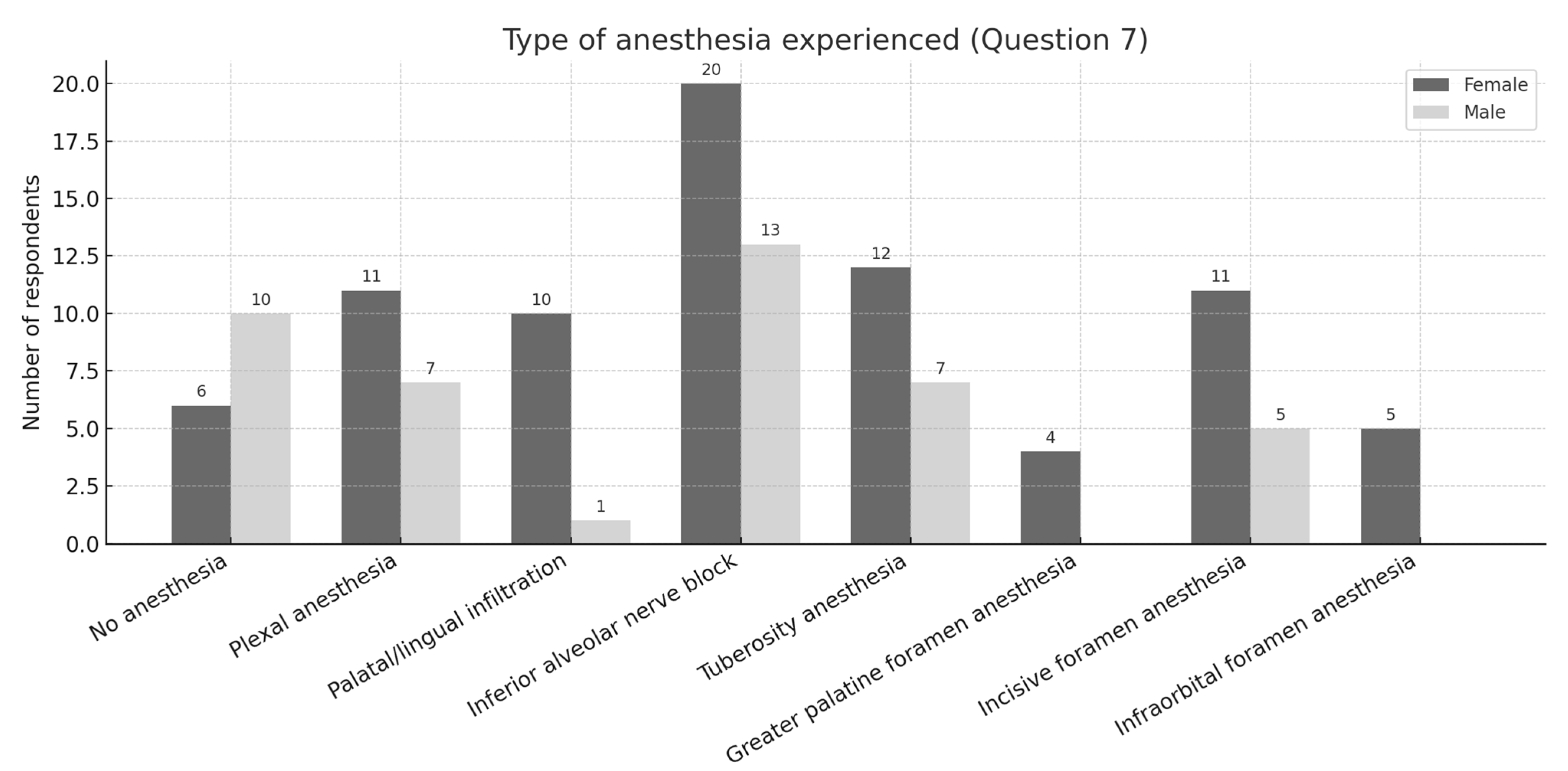
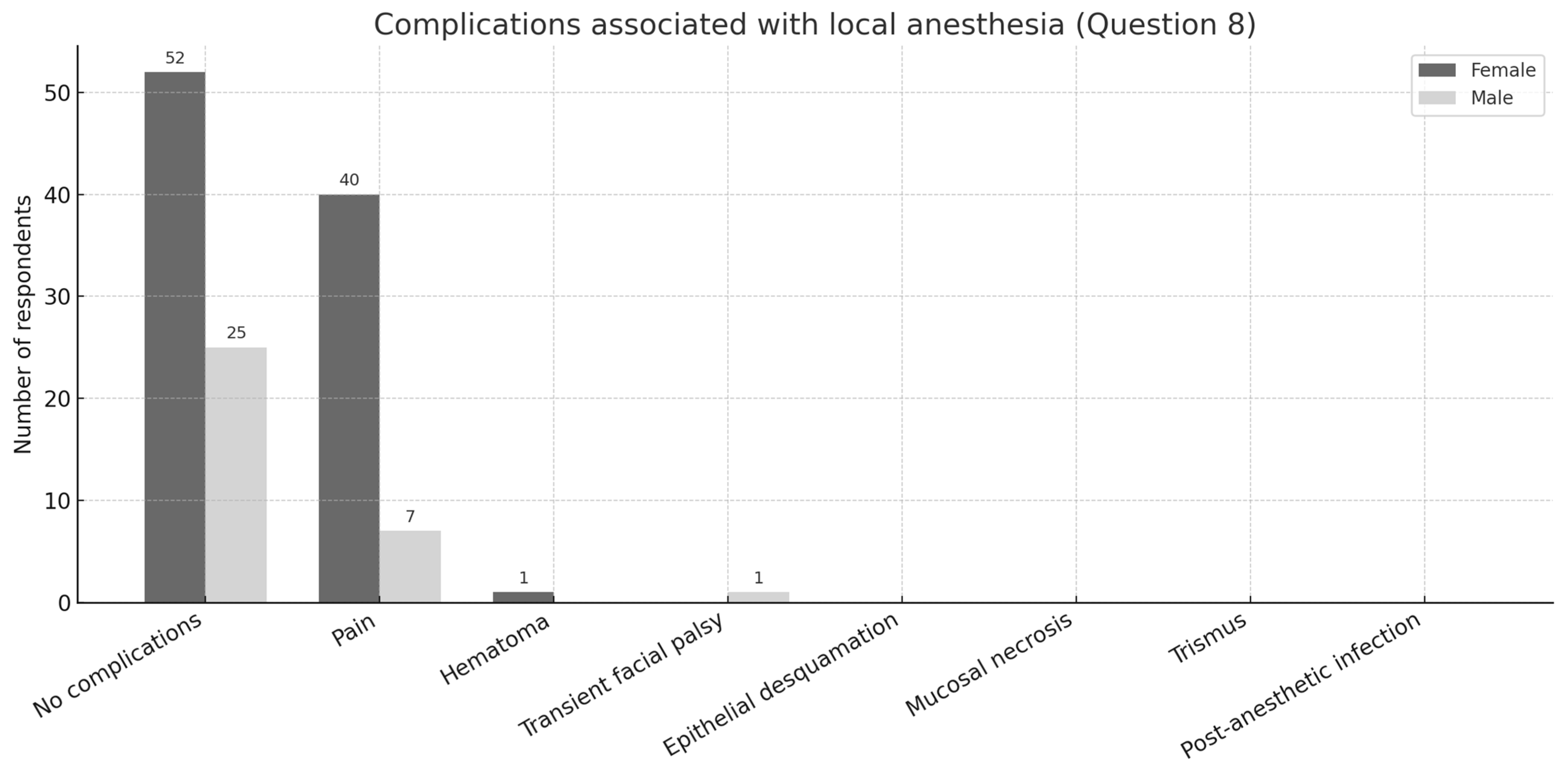
3. Results
4. Discussion
5. Conclusions
- The majority of dental students exhibit moderate levels of dental anxiety despite extensive exposure to local anesthesia, suggesting that the fear is largely anticipatory rather than based on adverse clinical outcomes.
- Local anesthetic injections represent the primary trigger of dental anxiety, surpassing other procedures such as scaling and drilling in terms of perceived distress.
- No statistically significant gender differences were identified regarding dental anxiety levels, implying that educational exposure may play a balancing role in emotional vulnerability.
- The Modified Dental Anxiety Scale (MDAS) can be recommended as a practical and validated tool for evaluating dental anxiety in academic populations. However, its limitations, including reliance on self-reported data and restriction to five items, should be acknowledged when interpreting results.
- The integration of structured anxiety management strategies into the dental curriculum is essential to enhance students’ well-being and improve the quality of patient care.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MDAS | Modified Dental Anxiety Scale |
| DAS | Dental Anxiety Scale |
| IDAF-4C+ | Index of Dental Anxiety and Fear |
| WHO | World Health Organization |
| SD | Standard Deviation |
| CI | Confidence Interval |
References
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Armfield, J.A.; Demarco, F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021, 108, 103632. [Google Scholar] [CrossRef]
- De Stefano, R. Psychological factors in dental patient care: Odontophobia. Medicina 2019, 55, 678. [Google Scholar] [CrossRef] [PubMed]
- Yakar, B.; Kaygusuz, T.Ö.; Pırınçcı, E. Evaluation of Dental Anxiety and Fear in Patients who Admitted to the Faculty of Dentistry: Which Patients are More Risky in terms of Dental Anxiety. Ethiop. J. Health Sci. 2019, 29, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Kassem El Hajj, H.; Fares, Y.; Abou-Abbas, L. Assessment of dental anxiety and dental phobia among adults in Lebanon. BMC Oral Health 2021, 21, 48. [Google Scholar] [CrossRef] [PubMed]
- AlRatroot, S.; Alotaibi, G.; AlBishi, F.; Khan, S.; Ashraf Nazir, M. Dental Anxiety Amongst Pregnant Women: Relationship with Dental Attendance and Sociodemographic Factors. Int. Dent. J. 2022, 72, 179–185. [Google Scholar] [CrossRef]
- Alkanan, S.A.M.; Alhaweri, H.S.; Khalifa, G.A.; Ata, S.M.S. Dental pain perception and emotional changes: On the relationship between dental anxiety and olfaction. BMC Oral Health 2023, 23, 175. [Google Scholar] [CrossRef]
- Ogawa, M.; Saito, A.; Karukivi, M.; Lahti, S. Associations of sensory sensitivity, pain catastrophizing, and alexithymia with dental anxiety. Eur. J. Oral Sci. 2024, 132, e12973. [Google Scholar] [CrossRef]
- Seligman, L.D.; Hovey, J.D.; Chacon, K.; Ollendick, T.H. Dental anxiety: An understudied problem in youth. Clin. Psychol. Rev. 2017, 55, 25–40. [Google Scholar] [CrossRef] [PubMed]
- Scandurra, C.; Gasparro, R.; Dolce, P.; Bochicchio, V.; Muzii, B.; Sammartino, G.; Marenzi, G.; Maldonato, N.M. The role of cognitive and non-cognitive factors in dental anxiety: A mediation model. Eur. J. Oral Sci. 2021, 129, e12793. [Google Scholar] [CrossRef] [PubMed]
- Ozlek, E.; Yıldırım, A.; Koc, A.; Boysan, M. Socio-demographic determinants of dental anxiety and fear among college students. East. J. Med. 2019, 24, 169–175. [Google Scholar] [CrossRef]
- Saba, Z.; Katirci, G. Relationship between dental anxiety levels and oral health among dental patients in Turkey: A cross-sectional study. BMC Oral Health 2023, 23, 328. [Google Scholar] [CrossRef]
- Wide, U.; Hakeberg, M. Treatment of dental anxiety and phobia—Diagnostic criteria and conceptual model of behavioural treatment. Dent. J. 2021, 9, 153. [Google Scholar] [CrossRef]
- Khan, S.D.A.A.; Alqannass, N.M.; Alwadei, M.M.; Alnajrani, M.D.; Alhareth, A.Y.A.; Alqahtani, K.M. Assessment of the Relationship between Dental Anxiety and Oral Health-Related Quality of Life. J. Pharm. Bioallied Sci. 2021, 13, S359–S362. [Google Scholar] [CrossRef]
- Begdache, L.; Ahmed, E.; Malik, S.; Karakaya, M.F. Dental Anxiety and Its Association with Dietary Intake and Food Groups: A Cross-Sectional Study. Dent. J. 2023, 11, 240. [Google Scholar] [CrossRef]
- Mueller, M.; Schorle, S.; Vach, K.; Hartmann, A.; Zeeck, A.; Schlueter, N. Relationship between dental experiences, oral hygiene education and self-reported oral hygiene behaviour. PLoS ONE 2022, 17, e0264306. [Google Scholar] [CrossRef]
- Stein Duker, L.I.; Grager, M.; Giffin, W.; Hikita, N.; Polido, J.C. The Relationship between Dental Fear and Anxiety, General Anxiety/Fear, Sensory Over-Responsivity and Oral Health Behaviors and Outcomes: A Conceptual Model. Int. J. Environ. Res. Public Health 2022, 19, 2380. [Google Scholar] [CrossRef]
- Chi, S.I. What is the gold standard of the dental anxiety scale? J. Dent. Anesth. Pain Med. 2023, 23, 193. [Google Scholar] [CrossRef] [PubMed]
- Bantel, D.; Chmielewski, W.X.; Brähler, E.; Stöbel-Richter, Y.; Zenger, M.; Weil, K.M.; Berth, H. The dental anxiety scale (DAS)—Psychometric properties and longitudinal findings among middle-aged adults. BMC Psychol. 2025, 13, 304. [Google Scholar] [CrossRef]
- Dadalti, M.T.S.; Cunha, A.J.L.; Souza, T.G.D.; Silva, B.A.; Luiz, R.R.; Risso, P.A. Anxiety about dental treatment—A gender issue. Acta Odontol. Latinoam. 2021, 34, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Mărginean, I.; Filimon, L. Modified Dental Anxiety Scale: A Validation Study on Communities From the West Part of Romania. Int. J. Educ. Psychol. Community 2012, 2, 102–114. [Google Scholar]
- Svensson, L.; Hakeberg, M.; Wide, U. Evaluating the validity of the Index of Dental Anxiety and Fear IDAF-4C in adults with severe dental anxiety. Eur. J. Oral Sci. 2020, 128, 423–428. [Google Scholar] [CrossRef]
- Done, A.E.; Preoteasa, E.; Preoteasa, C.T. Psychometric Assessment of the Romanian Version of the Index of Dental Anxiety and Fear (IDAF-4C+). Healthcare 2023, 11, 1420. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, C.R.; Khijmatgar, S.; Chowdhury, A.; Harding, S.; Lynch, E.; Gootveld, M. Dental anxiety in first- and final-year Indian dental students. BDJ Open 2019, 5, 15. [Google Scholar] [CrossRef]
- Gunjal, S.; Pateel, D.G.S.; Parkar, S. Dental Anxiety among Medical and Paramedical Undergraduate Students of Malaysia. Int. J. Dent. 2017, 2017, 4762576. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.X.D.; Soh, X.C.; Hartanto, A.; Goh, A.Y.H.; Majeed, N.M. Prevalence of anxiety in college and university students: An umbrella review. J. Affect. Disord. Rep. 2023, 14, 100658. [Google Scholar] [CrossRef]
- Korpela, I.; Vaununmaa, K.; Tolvanen, M.; Suominen, A.; Freeman, R.; Lahti, S. Dental students’ and patients’ perceived importance and knowledge of dental anxiety. Eur. J. Dent. Educ. 2019, 23, 515–521. [Google Scholar] [CrossRef]
- Humphris, G.M.; Newton, J.T. Is the Modified Dental Anxiety Scale (MDAS) a Single or Two Construct Measure? A Theoretical and Pragmatic Perspective. Dent. J. 2025, 13, 186. [Google Scholar] [CrossRef]
- Kritsidima, M.; Scambler, S.; Asimakopoulou, K. Exploring the Levels of Dental Anxiety in Greek Patients. Int. Dent. J. 2025, 75, 100826. [Google Scholar] [CrossRef]
- Winkler, C.H.; Bjelopavlovic, M.; Lehmann, K.M.; Petrowski, K.; Irmscher, L.; Berth, H. Impact of Dental Anxiety on Dental Care Routine and Oral-Health-Related Quality of Life in a German Adult Population—A Cross-Sectional Study. J. Clin. Med. 2023, 12, 5291. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, M.J.; Proença, L.; Cavacas, M.A. Anxiety levels of 1st and 5th-year dental students in Portugal—Cross-sectional study. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2024, 65, 129–135. [Google Scholar] [CrossRef]
- Muneer, M.U.; Ismail, F.; Munir, N.; Shakoor, A.; Das, G.; Ahmed, A.R.; Ahmed, M.A. Dental Anxiety and Influencing Factors in Adults. Healthcare 2022, 10, 1529. [Google Scholar] [CrossRef]
- Zhang, D.; Li, S.; Zhang, R. Effects of dental anxiety and anesthesia on vital signs during tooth extraction. BMC Oral Health 2024, 24, 583. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, B.; Erwood, K.; Ncomanzi, S.; Fischer, V.; O’Brien, D.; Lee, A. Management strategies for adult patients with dental anxiety in the dental clinic: A systematic review. Aust. Dent. J. 2022, 67, S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Martín, V.; Verdejo-Herrero, J.; Romero-del Rey, R.; Garcia-Gonzalez, J.; Requena-Mullor, M.D.M.; Alarcon-Rodriguez, R. The Effect of Immersive Virtual Reality on Dental Anxiety and Intraoperative Pain in Adults Undergoing Local Anesthesia: A Randomized Clinical Trial. Healthcare 2024, 12, 432. [Google Scholar] [CrossRef] [PubMed]
- Lahti, S.; Kajita, M.; Pohjola, V.; Suominen, A. Reliability and Validity of the Modified Dental Anxiety Scale Among Children Aged 9 to 12 Years. Dent. J. 2025, 13, 200. [Google Scholar] [CrossRef]
- Gazal, G.; Tola, A.W.; Fareed, W.M.; Alnazzawi, A.A.; Zafar, M.S. A randomized control trial comparing the visual and verbal communication methods for reducing fear and anxiety during tooth extraction. Saudi Dent. J. 2016, 28, 80–85. [Google Scholar] [CrossRef]
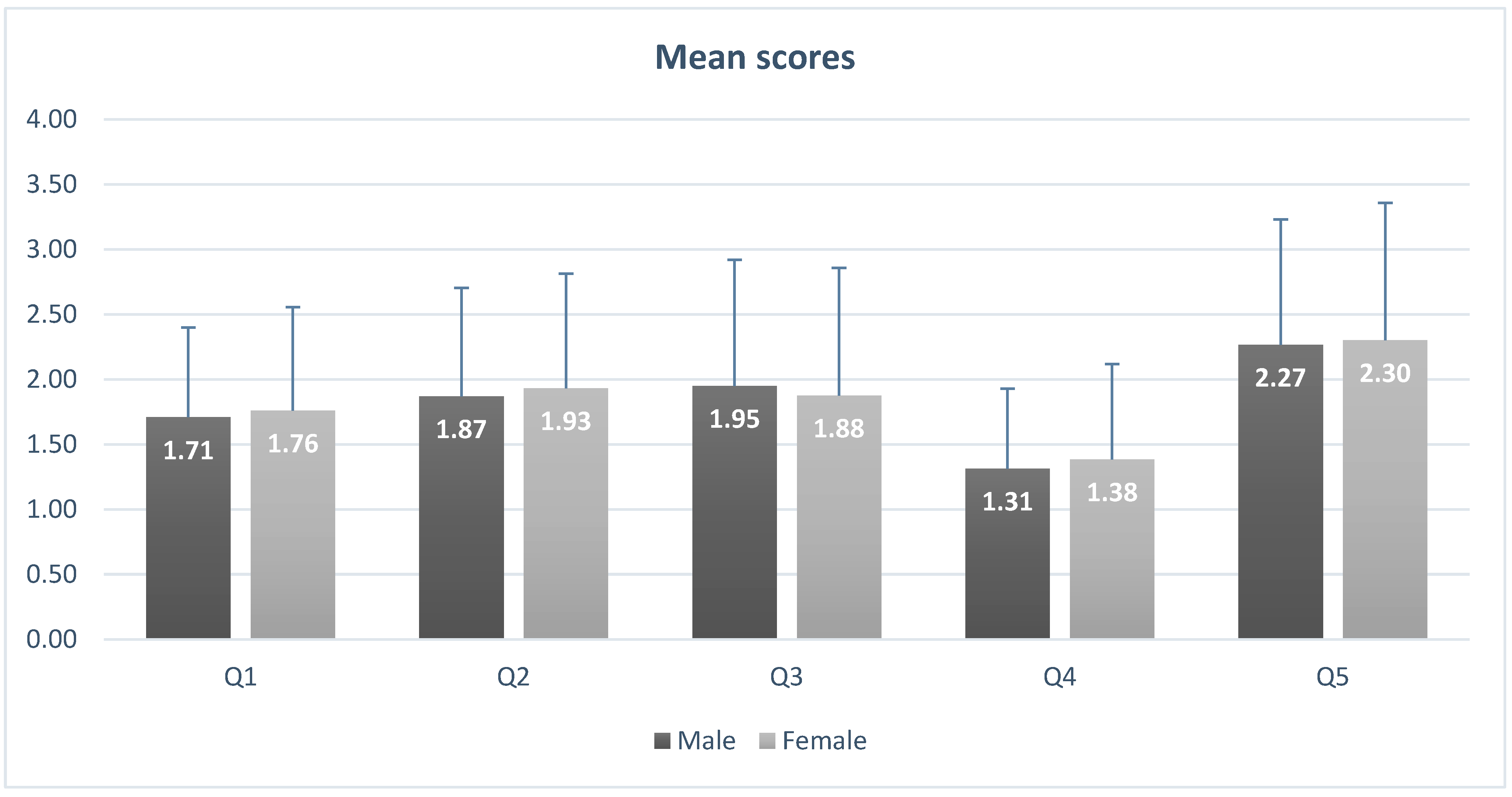
| Question no. | Gender | Not Anxious | Slightly Anxious | Fairly Anxious | Very Anxious | Extremely Anxious | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | ||
| 1 | Female | 30 | 24.6 | 42 | 34.4 | 6 | 4.9 | 0 | 0 | 1 | 0.8 |
| * 0.953 | Male | 17 | 13.9 | 20 | 16.4 | 5 | 4.1 | 0 | 0 | 1 | 0.8 |
| ** 0.813 | Total | 47 | 38.5 | 62 | 50.8 | 11 | 9 | 0 | 0 | 2 | 1.6 |
| 2 | Female | 21 | 17.2 | 45 | 36.9 | 11 | 9 | 1 | 0.8 | 1 | 0.8 |
| * 2.806 | Male | 14 | 11.5 | 19 | 15.6 | 7 | 5.7 | 2 | 1.6 | 1 | 0.8 |
| ** 0.591 | Total | 35 | 28.7 | 64 | 52.5 | 18 | 14.8 | 3 | 2.5 | 2 | 1.6 |
| 3 | Female | 31 | 25.4 | 39 | 32 | 7 | 5.7 | 1 | 0.8 | 1 | 0.8 |
| * 5.497 | Male | 18 | 14.8 | 14 | 11.5 | 8 | 6.6 | 1 | 0.8 | 2 | 1.6 |
| ** 0.240 | Total | 49 | 40.2 | 53 | 43.4 | 15 | 12.3 | 2 | 1.6 | 3 | 2.5 |
| 4 | Female | 48 | 39.3 | 24 | 19.7 | 4 | 3.3 | 2 | 1.6 | 1 | 0.8 |
| * 4.951 | Male | 32 | 26.2 | 6 | 4.9 | 3 | 2.5 | 2 | 1.6 | 0 | 0 |
| ** 0.292 | Total | 80 | 65.6 | 30 | 24.6 | 7 | 5.7 | 4 | 3.3 | 1 | 0.8 |
| 5 | Female | 17 | 13.9 | 32 | 26.2 | 24 | 19.7 | 4 | 3.3 | 2 | 1.6 |
| * 1.669 | Male | 9 | 7.4 | 18 | 14.8 | 10 | 8.2 | 4 | 3.3 | 2 | 1.6 |
| ** 0.796 | Total | 26 | 21.3 | 50 | 41 | 34 | 27.9 | 8 | 6.6 | 4 | 3.3 |
| Question 6 | Total | ||||
|---|---|---|---|---|---|
| No | Yes | p Value (t-Test) | |||
| Gender | Female | 6 | 73 | 79 | p < 0.001 |
| Male | 10 | 33 | 43 | ||
| Total | 16 | 106 | 122 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bologa, E.; Tărăboanță-Gamen, A.C.; Tărăboanță, I.; Boișteanu, O.; Platon, A.-L.; Stelea, Ș.-O.; Simionescu, A.-M.A.; Grădinariu, A.I.; Jehac, A.; Bologa, C.; et al. Assessment of Anxiety and Local Anesthesia Experiences in Dental Students Using the Modified Dental Anxiety Scale (MDAS). Dent. J. 2025, 13, 445. https://doi.org/10.3390/dj13100445
Bologa E, Tărăboanță-Gamen AC, Tărăboanță I, Boișteanu O, Platon A-L, Stelea Ș-O, Simionescu A-MA, Grădinariu AI, Jehac A, Bologa C, et al. Assessment of Anxiety and Local Anesthesia Experiences in Dental Students Using the Modified Dental Anxiety Scale (MDAS). Dentistry Journal. 2025; 13(10):445. https://doi.org/10.3390/dj13100445
Chicago/Turabian StyleBologa, Emilia, Andra Claudia Tărăboanță-Gamen, Ionuț Tărăboanță, Otilia Boișteanu, Alexandra-Lorina Platon, Șerban-Ovidiu Stelea, Ana-Maria Andreea Simionescu, Anca Irina Grădinariu, Alina Jehac, Cristina Bologa, and et al. 2025. "Assessment of Anxiety and Local Anesthesia Experiences in Dental Students Using the Modified Dental Anxiety Scale (MDAS)" Dentistry Journal 13, no. 10: 445. https://doi.org/10.3390/dj13100445
APA StyleBologa, E., Tărăboanță-Gamen, A. C., Tărăboanță, I., Boișteanu, O., Platon, A.-L., Stelea, Ș.-O., Simionescu, A.-M. A., Grădinariu, A. I., Jehac, A., Bologa, C., & Stelea, C. G. (2025). Assessment of Anxiety and Local Anesthesia Experiences in Dental Students Using the Modified Dental Anxiety Scale (MDAS). Dentistry Journal, 13(10), 445. https://doi.org/10.3390/dj13100445







